Ultrasound-Guided Supraclavicular Nerves Block for Acute Pain Management in Clavicular Fractures—A Pragmatic Randomized Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics
2.2. Randomization
2.3. Sample Size
2.4. Ultrasound-Guided Supraclavicular Nerves Block
2.5. Pain Medication Protocols
2.6. Outcome Measures and Data Collection
2.7. Statistical Analysis
3. Results
3.1. Recruitment, Randomization, and Patient Characteristics
3.2. Block Performance
3.3. Pain Relief
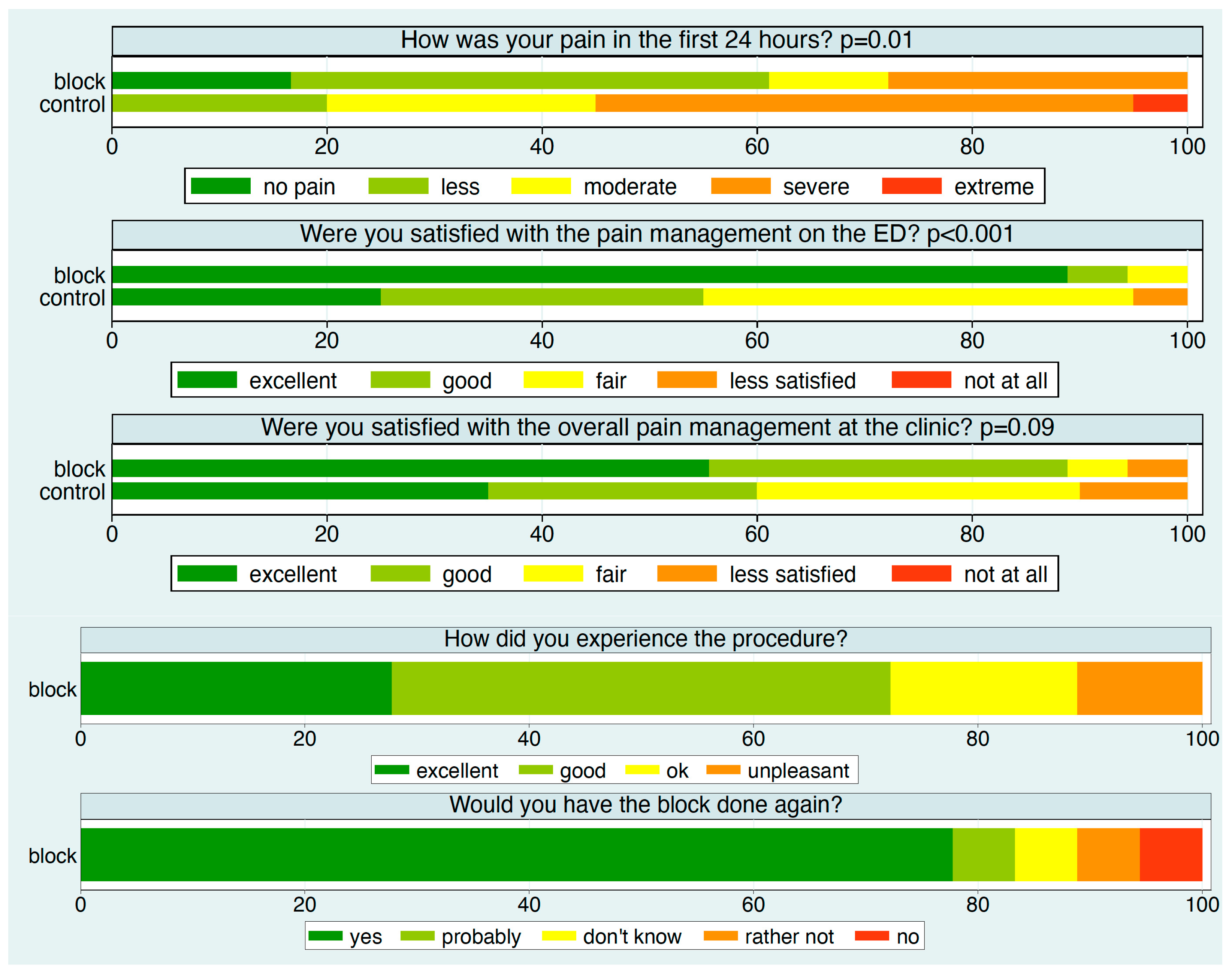
3.4. Patient Experience
3.5. Pain Medication
3.6. Adverse Reactions and Adverse Events
3.7. Impact on Patient Management
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| RA | Regional anesthesia |
| SCLN | Supraclavicular nerve |
| PN | Phrenic nerve |
| GAN | Great auricular nerve |
| TCN | Transverse cervical nerve |
| LON | Lesser occipital nerve |
| SCM | Sternocleidomastoid muscle |
| SCF | Superficial cervical fascia |
| PVF | Prevertebral fascia |
| mSM | Middle scalene muscle |
| aSM | anterior scalene muscle |
| minSM | Scalenus minimus muscle |
| RvC5 | Ventral ramus of the 5th spinal nerve |
| CF | Clavicle fracture |
| ED | Emergency department |
| NRS | Numeric rating scale |
| ASA | American Society of Anesthesiologists |
References
- Ullah, K.; Khan, S.; Wang, Y.; Zhao, Z.; Cheng, P.; Sapkota, B.; Ren, L.; Khan, S.; Rehman, M.U.; Xue, Y. Bilaterally Threaded, Minimal Invasive, Elastic Locking Intramedullary Nailing (ELIN) for the Treatment of Clavicle Fractures. Orthop. Surg. 2020, 12, 321–332. [Google Scholar] [CrossRef] [PubMed]
- Rupp, M.; Walter, N.; Pfeifer, C.; Lang, S.; Kerschbaum, M.; Krutsch, W.; Baumann, F.; Alt, V. The incidence of fractures among the adult population of Germany. Dtsch. Ärzteblatt Int. 2021, 118, 665–669. [Google Scholar] [CrossRef] [PubMed]
- Lindsey, M.H.; Grisdela, P.; Lu, L.; Zhang, D.; Earp, B. What Are the Functional Outcomes and Pain Scores after Medial Clavicle Fracture Treatment? Clin. Orthop. Relat. Res. 2021, 479, 2400–2407. [Google Scholar] [CrossRef]
- Kim, D.-W.; Kim, D.-H.; Kim, B.-S.; Cho, C.-H. Current Concepts for Classification and Treatment of Distal Clavicle Fractures. Clin. Orthop. Surg. 2020, 12, 135. [Google Scholar] [CrossRef]
- Yoo, J.-S.; Heo, K.; Kwon, S.-M.; Lee, D.-H.; Seo, J.-B. Effect of Surgical-Site, Multimodal Drug Injection on Pain and Stress Biomarkers in Patients Undergoing Plate Fixation for Clavicular Fractures. Clin. Orthop. Surg. 2018, 10, 455. [Google Scholar] [CrossRef]
- Joshi, G.P. Multimodal Analgesia Techniques and Postoperative Rehabilitation. Anesthesiol. Clin. N. Am. 2005, 23, 185–202. [Google Scholar] [CrossRef]
- Phillips, D.M. JCAHO Pain Management Standards Are Unveiled. JAMA 2000, 284, 428. [Google Scholar] [CrossRef]
- Leurcharusmee, P.; Maikong, N.; Kantakam, P.; Navic, P.; Mahakkanukrauh, P.; Tran, D.Q. Innervation of the clavicle: A cadaveric investigation. Reg. Anesth. Pain Med. 2021, 46, 1076–1079. [Google Scholar] [CrossRef]
- Tran, D.Q.H.; Tiyaprasertkul, W.; González, A.P. Analgesia for Clavicular Fracture and Surgery: A Call for Evidence. Reg. Anesth. Pain Med. 2013, 38, 539–543. [Google Scholar] [CrossRef]
- Abdelghany, M.S.; Ahmed, S.A.; Afandy, M.E. Superficial cervical plexus block alone or combined with interscalene brachial plexus block in surgery for clavicle fractures: A randomized clinical trial. Minerva Anestesiol. 2021, 87, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Reverdy, F. Combined interscalene-superficial cervical plexus block for clavicle surgery: An easy technique to avoid general anesthesia. BJA Br. J. Anaesth. 2015, 115. [Google Scholar] [CrossRef]
- Lee, C.C.M.; Beh, Z.Y.; Lua, C.B.; Peng, K.; Fathil, S.M.; Hou, J.-D.; Lin, J.-A. Regional Anesthetic and Analgesic Techniques for Clavicle Fractures and Clavicle Surgeries: Part 1—A Scoping Review. Healthcare 2022, 10, 1487. [Google Scholar] [CrossRef]
- Tran, D.Q.H.; Elgueta, M.F.; Aliste, J.; Finlayson, R.J. Diaphragm-Sparing Nerve Blocks for Shoulder Surgery. Reg. Anesth. Pain Med. 2017, 42, 32–38. [Google Scholar] [CrossRef]
- Litz, R.; Avila Gonzalez, C.; Feigl, G. Cervical Plexus Block. In Musculoskeletal Ultrasound for Regional Anaesthesia and Pain Medicine, 2nd ed.; Karmakar, M.J., Ed.; Department of Anaesthesia and Intensive Care: Hong Kong, China, 2016; pp. 253–265. [Google Scholar]
- Schulz, K.F.; Altman, D.G.; Moher, D.; CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomized trials. Ann. Intern. Med. 2010, 152, 726–732. [Google Scholar] [CrossRef] [PubMed]
- Erlacher, W.; Schuschnig, C.; Koinig, H.; Marhofer, P.; Melischek, M.; Mayer, N.; Kapral, S. Clonidine as adjuvant for mepivacaine, ropivacaine and bupivacaine in axillary, perivascular brachial plexus block. Can. J. Anesth. 2001, 48, 522–525. [Google Scholar] [CrossRef] [PubMed]
- Allman, F.L. Fractures and ligamentous injuries of the clavicle and its articulation. J. Bone Jt. Surg. Am. 1967, 49, 774–784. [Google Scholar] [CrossRef]
- O’Neill, B.J.; Hirpara, K.M.; O’Briain, D.; McGarr, C.; Kaar, T.K. Clavicle fractures: A comparison of five classification systems and their relationship to treatment outcomes. Int. Orthop. (SICOT) 2011, 35, 909–914. [Google Scholar] [CrossRef]
- Herring, A.A.; Stone, M.B.; Frenkel, O.; Chipman, A.; Nagdev, A.D. The ultrasound-guided superficial cervical plexus block for anesthesia and analgesia in emergency care settings. Am. J. Emerg. Med. 2012, 30, 1263–1267. [Google Scholar] [CrossRef]
- Divella, M.; Vetrugno, L. Regional blocks for clavicle fractures: Keep Hippocrates in mind. Minerva Anestesiol. 2021, 87, 499–501. [Google Scholar] [CrossRef]
- Kim, H.Y.; Soh, E.Y.; Lee, J.; Kwon, S.H.; Hur, M.; Min, S.-K.; Kim, J.-S. Incidence of hemi-diaphragmatic paresis after ultrasound-guided intermediate cervical plexus block: A prospective observational study. J. Anesth. 2020, 34, 483–490. [Google Scholar] [CrossRef]
- Opperer, M.; Kaufmann, R.; Meissnitzer, M.; Enzmann, F.K.; Dinges, C.; Hitzl, W.; Nawratil, J.; Koköfer, A. Depth of cervical plexus block and phrenic nerve blockade: A randomized trial. Reg. Anesth. Pain Med. 2022, 47, 205–211. [Google Scholar] [CrossRef]
- Arjun, B.K.; Vinod, C.N.; Puneeth, J.; Narendrababu, M.C. Ultrasound-guided interscalene block combined with intermediate or superficial cervical plexus block for clavicle surgery: A randomised double blind study. Eur. J. Anaesthesiol. 2020, 37, 979–983. [Google Scholar] [CrossRef] [PubMed]
- Petrucci, E. Intermediate Cervical Plexus Block in theManagement of Persistent Postoperative PainPost Carotid Endarterectomy: A Prospective, Randomized, Controlled, Clinical Trial. Pain Phys. 2020, 23, 237–244. [Google Scholar] [CrossRef]
- Eichenberger, U.; Stöckli, S.; Marhofer, P.; Huber, G.; Willimann, P.; Kettner, S.C.; Pleiner, J.; Curatolo, M.; Kapral, S. Minimal Local Anesthetic Volume for Peripheral Nerve Block: A New Ultrasound-Guided, Nerve Dimension-Based Method. Reg. Anesth. Pain Med. 2009, 34, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Ali, Q.; Manjunatha, L.; Amir, S.; Jamil, S.; Quadir, A. Efficacy of clonidine as an adjuvant to ropivacaine in supraclavicular brachial plexus block: A prospective study. Indian J. Anaesth. 2014, 58, 709. [Google Scholar] [CrossRef]
- Patil, K.; Singh, N. Clonidine as an adjuvant to ropivacaine-induced supraclavicular brachial plexus block for upper limb surgeries. J. Anaesthesiol. Clin. Pharmacol. 2015, 31, 365. [Google Scholar] [CrossRef]
- Bhatia, R.; Payal, Y.; Khurana, G. Addition of clonidine or lignocaine to ropivacaine for supraclavicular brachial plexus block: A comparative study. Singap. Med J. 2014, 55, 229–232. [Google Scholar] [CrossRef]
- Beaussier, M.; Weickmans, H.; Abdelhalim, Z.; Lienhart, A. Inguinal Herniorrhaphy Under Monitored Anesthesia Care with Ilioinguinal-Iliohypogastric Block: The Impact of Adding Clonidine to Ropivacaine. Anesth. Analg. 2005, 101, 1659–1662. [Google Scholar] [CrossRef]
- Helayel, P.E.; Kroth, L.; Boos, G.L.; Jahns, M.T.; Oliveira Filho, G.R.D. Efeitos da clonidina por via muscular e perineural no bloqueio do nervo isquiático com ropivacaína a 0,5%. Rev. Bras. Anestesiol. 2005, 55, 483–490. [Google Scholar] [CrossRef]


| Block (n = 19) | Control (n = 21) | p-Value | |
|---|---|---|---|
| Age (years) | 40 (18–70) | 43 (18–67) | 0.56 |
| Female/male | 1 (5%)/18 (94.7%) | 2 (9.5%)/19 (90.5%) | 1.00 |
| ASA | 1.5 (1–3) | 1.5 (1–3) | 1.00 |
| BMI | 24.2 (19.4–30.4) | 24.3 (19.5–33.9) | 1.00 |
| Type of accident | 0.42 | ||
| Bicycle | 14 (73.7%) | 14 (66.7%) | |
| Sports | 2 (10.5%) | 6 (28.6%) | |
| Fall of other cause | 2 (10.5%) | 1 (4.8%) | |
| Direct blow | 1 (5.3%) | 0 (0.0%) | |
| Fracture location | 0.33 | ||
| Lateral third | 5 (26.3%) | 3 (14.3%) | |
| Middle third | 13 (68.4%) | 18 (85.7%) | |
| Medial third | 1 (5.3%) | 0 (0.0%) | |
| Dislocation | 1.00 | ||
| <5 mm | 1 (5.3%) | 2 (9.5%) | |
| >5 mm | 18 (94.7%) | 19 (90.5%) |
| Type of Block | |
|---|---|
| Supraclavicular Nerve block | 17 (89.5%) |
| Intermediate cervical plexus block | 2 (10.5%) |
| Local anesthetic | |
| Bupivacain 0.5% + Clonidin | 17 (89.5%) |
| Ropivacain 1% + Clonidin | 1 (5.3%) |
| Ropivacain 0.75% | 1 (5.3%) |
| Dose of local anesthetic | |
| 3 mL | 5 (26.3%) |
| 3.5 mL | 1 (5.3%) |
| 4 mL | 12 (63.2%) |
| 5 mL | 1 (5.3%) |
| Block | Control | |
|---|---|---|
| Sample size, n | 19 | 21 |
| Metamizole—iv | ||
| given | 2 (10.5%) | 5 (23.8%) |
| dose (mg) | 1750 (500–3000) | 2214 (1000–4000) |
| Ketorolac—iv | ||
| given | 0 (0.0%) | 3 (14.3%) |
| dose (mg) | 0 (0.0) | 30 (30–30) |
| Paracetamol—iv | ||
| given | 3 (15.8%) | 3 (14.3%) |
| dose (mg) | 1333 (1000–2000) | 2000 (1000–4000) |
| Ibuprofen—per os | ||
| given | 12 (63.2%) | 18 (85.7%) |
| dose (mg) | 633 (400–2000) | 1156 (400–2200) |
| Metamizole—per os | ||
| given | 4 (21.1%) | 15 (71.4%) |
| dose (mg) | 2000 (1000–3000) | 2607 (500–5000) |
| Paracetamol—per os | ||
| given | 1 (5.3%) | 3 (14.3%) |
| dose (mg) | 1000 (1000–1000) | 1500 (1000–2000) |
| Oxycodone—per os | ||
| given | 7 (36.8%) | 6 (28.6%) |
| dose (mg) | 18 (7–35) | 22 (7–40) |
| Fentanyl—iv | ||
| given | 4 (21.1%) | 6 (28.6%) |
| dose (µg) | 162 (50–300) | 200 (50–350) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schöll, E.; Gerbershagen, M.U.; Vach, W.; Rösli, M.; Litz, R.J. Ultrasound-Guided Supraclavicular Nerves Block for Acute Pain Management in Clavicular Fractures—A Pragmatic Randomized Trial. J. Clin. Med. 2025, 14, 8249. https://doi.org/10.3390/jcm14228249
Schöll E, Gerbershagen MU, Vach W, Rösli M, Litz RJ. Ultrasound-Guided Supraclavicular Nerves Block for Acute Pain Management in Clavicular Fractures—A Pragmatic Randomized Trial. Journal of Clinical Medicine. 2025; 14(22):8249. https://doi.org/10.3390/jcm14228249
Chicago/Turabian StyleSchöll, Eckehart, Mark Ulrich Gerbershagen, Werner Vach, Maria Rösli, and Rainer Jürgen Litz. 2025. "Ultrasound-Guided Supraclavicular Nerves Block for Acute Pain Management in Clavicular Fractures—A Pragmatic Randomized Trial" Journal of Clinical Medicine 14, no. 22: 8249. https://doi.org/10.3390/jcm14228249
APA StyleSchöll, E., Gerbershagen, M. U., Vach, W., Rösli, M., & Litz, R. J. (2025). Ultrasound-Guided Supraclavicular Nerves Block for Acute Pain Management in Clavicular Fractures—A Pragmatic Randomized Trial. Journal of Clinical Medicine, 14(22), 8249. https://doi.org/10.3390/jcm14228249







