Impact of Papillary Morphology and Diverticular Type on Needle-Knife Papillotomy in Patients with Periampullary Diverticulum with Difficult Biliary Cannulation
Abstract
1. Introduction
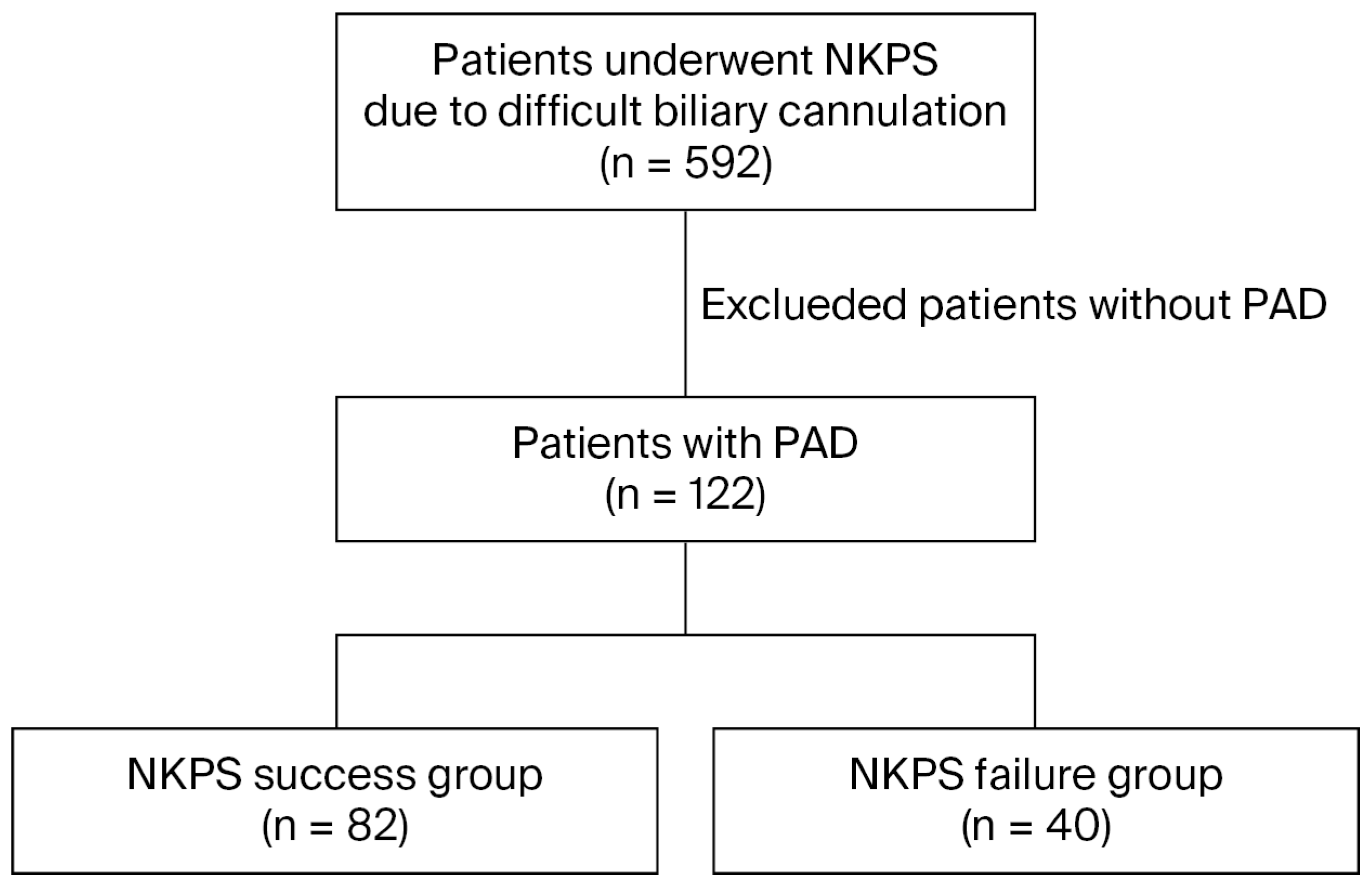
2. Patients and Methods
2.1. ERCP and NKP Procedures
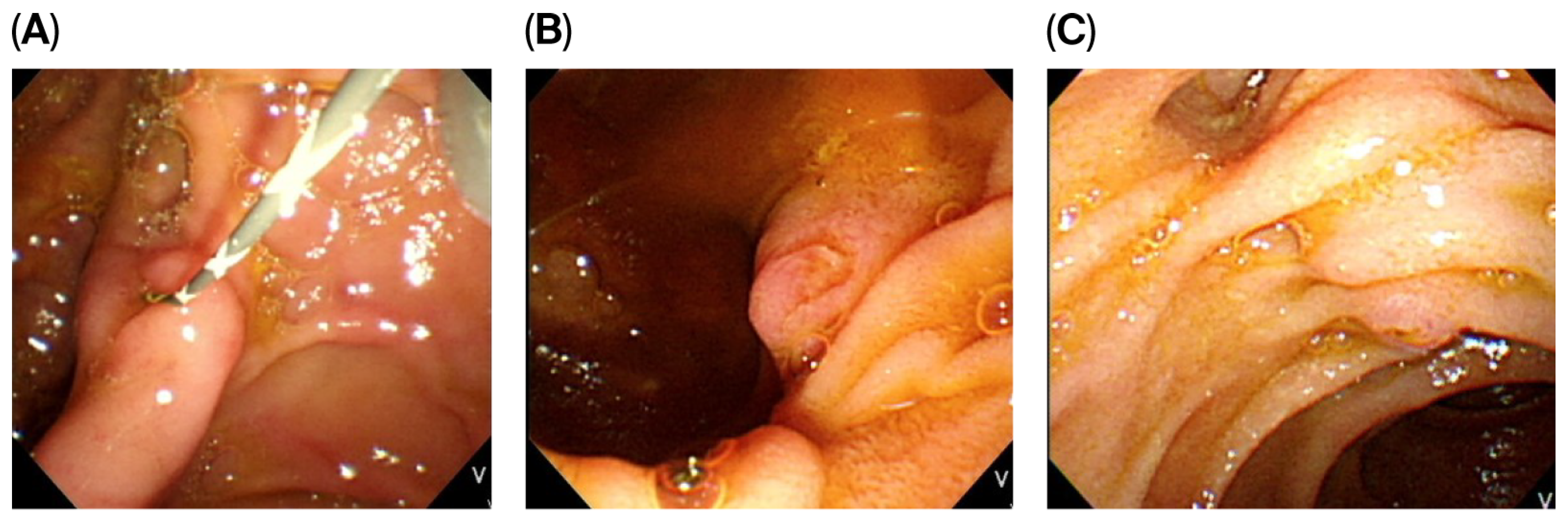
2.2. Classification of Periampullary Diverticulum
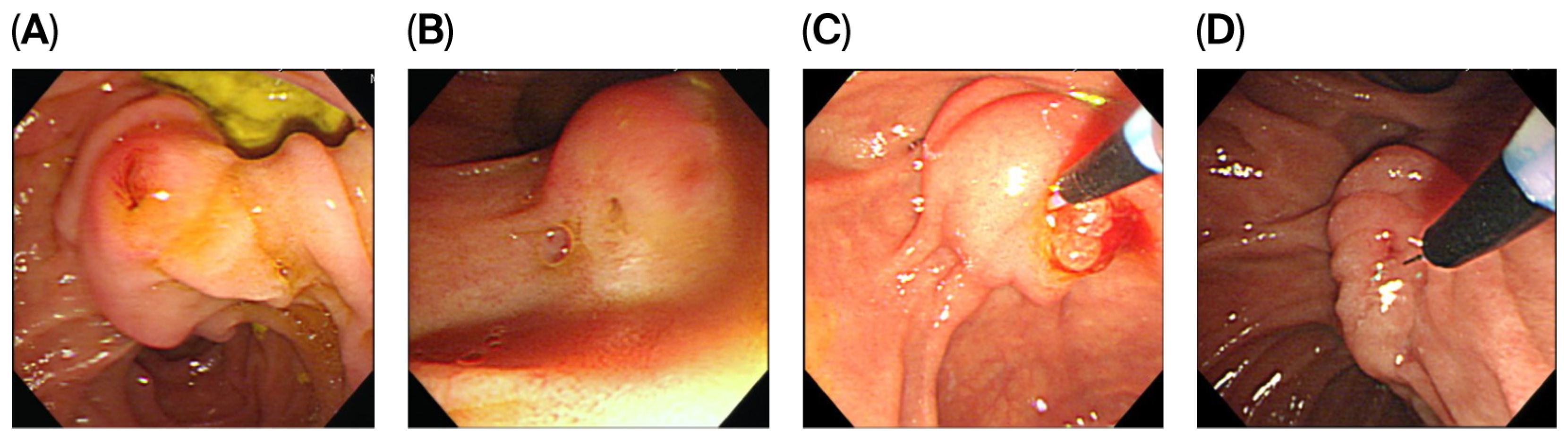
2.3. Morphology of the Major Duodenum Papilla
2.4. Statistical Analysis
3. Results
3.1. Result Comparisons Between the NKP Success and Failure Groups
3.2. Results Based on Diverticular Type
3.3. Results Based on Papillary Morphology
3.4. Factors Associated with NKP Outcomes
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PAD | periampullary diverticulum |
| ERCP | endoscopic retrograde cholangiopancreatography |
| NKP | needle-knife papillotomy |
| MDP | major duodenal papilla |
| SBC | selective biliary cannulation |
| NKPS | needle-knife precut sphincterotomy |
| CBD | common bile duct |
| NSAIDs | nonsteroidal anti-inflammatory drugs |
References
- Cennamo, V.; Fuccio, L.; Zagari, R.M.; Eusebi, L.H.; Ceroni, L.; Laterza, L.; Fabbri, C.; Bazzoli, F. Can early precut implementation reduce endoscopic retrograde cholangiopancreatography-related complication risk? Meta-analysis of randomized controlled trials. Endoscopy 2010, 42, 381–388. [Google Scholar] [CrossRef]
- Jayaraj, M.; Mohan, B.P.; Dhindsa, B.S.; Mashiana, H.S.; Radhakrishnan, G.; Dhir, V.; Trindade, A.J.; Adler, D.G. Periampullary Diverticula and ERCP Outcomes: A Systematic Review and Meta-Analysis. Dig. Dis. Sci. 2019, 64, 1364–1376. [Google Scholar] [CrossRef]
- Tyagi, P.; Sharma, P.; Sharma, B.C.; Puri, A.S. Periampullary diverticula and technical success of endoscopic retrograde cholangiopancreatography. Surg. Endosc. 2009, 23, 1342–1345. [Google Scholar] [CrossRef]
- Mohammad Alizadeh, A.H.; Afzali, E.S.; Shahnazi, A.; Mousavi, M.; Doagoo, S.Z.; Mirsattari, D.; Zali, M.R. ERCP features and outcome in patients with periampullary duodenal diverticulum. ISRN Gastroenterol. 2013, 2013, 217261. [Google Scholar] [CrossRef]
- Tabak, F.; Ji, G.Z.; Miao, L. Impact of periampullary diverticulum on biliary cannulation and ERCP outcomes: A single-center experience. Surg. Endosc. 2021, 35, 5953–5961. [Google Scholar] [CrossRef]
- Yue, P.; Zhu, K.X.; Wang, H.P.; Meng, W.B.; Liu, J.K.; Zhang, L.; Zhu, X.L.; Zhang, H.; Miao, L.; Wang, Z.F.; et al. Clinical significance of different periampullary diverticulum classifications for endoscopic retrograde cholangiopancreatography cannulation. World J. Gastroenterol. 2020, 26, 2403–2415. [Google Scholar] [CrossRef]
- Lobo, D.N.; Balfour, T.W.; Iftikhar, S.Y. Periampullary diverticula: Consequences of failed ERCP. Ann. R. Coll. Surg. Engl. 1998, 80, 326–331. [Google Scholar]
- Boix, J.; Lorenzo-Zúñiga, V.; Añaños, F.; Domènech, E.; Morillas, R.M.; Gassull, M.A. Impact of periampullary duodenal diverticula at endoscopic retrograde cholangiopancreatography: A proposed classification of periampullary duodenal diverticula. Surg. Laparosc. Endosc. Percutan. Tech. 2006, 16, 208–211. [Google Scholar] [CrossRef] [PubMed]
- Testoni, P.A.; Mariani, A.; Aabakken, L.; Arvanitakis, M.; Bories, E.; Costamagna, G.; Devière, J.; Dinis-Ribeiro, M.; Dumonceau, J.M.; Giovannini, M.; et al. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016, 48, 657–683. [Google Scholar] [CrossRef] [PubMed]
- Tsou, Y.K.; Pan, K.T.; Lee, M.H.; Lin, C.H. Endoscopic salvage therapy after failed biliary cannulation using advanced techniques: A concise review. World J. Gastroenterol. 2022, 28, 3803–3813. [Google Scholar] [CrossRef] [PubMed]
- Lo, M.-H.; Lin, C.-H.; Wu, C.-H.; Tsou, Y.-K.; Lee, M.-H.; Sung, K.-F.; Liu, N.-J. Management of biliary diseases after the failure of initial needle knife precut sphincterotomy for biliary cannulation. Sci. Rep. 2021, 11, 14968. [Google Scholar] [CrossRef]
- Lee, M.-H.; Huang, S.-W.; Lin, C.-H.; Tsou, Y.-K.; Sung, K.-F.; Wu, C.-H.; Liu, N.-J. Predictive factors of needle-knife pre-cut papillotomy failure in patients with difficult biliary cannulation. Sci. Rep. 2022, 12, 4942. [Google Scholar] [CrossRef]
- Canena, J.; Lopes, L.; Fernandes, J.; Costa, P.; Arvanitakis, M.; Koch, A.D.; Poley, J.W.; Jimenez, J.; Dominguez-Munõz, E.; Familiari, P.; et al. Influence of a novel classification of the papilla of Vater on the outcome of needle-knife fistulotomy for biliary cannulation. BMC Gastroenterol. 2021, 21, 147. [Google Scholar] [CrossRef] [PubMed]
- Haraldsson, E.; Lundell, L.; Swahn, F.; Enochsson, L.; Löhr, J.M.; Arnelo, U.; Scandinavian Association for Digestive Endoscopy (SADE) Study Group of Endoscopic Retrograde Cholangio-Pancreaticography. Endoscopic classification of the papilla of Vater. Results of an inter- and intraobserver agreement study. United Eur. Gastroenterol. J. 2017, 5, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, R.; Lethebe, B.C.; Gonzalez-Moreno, E.; Kayal, A.; Bass, S.; Cole, M.; Turbide, C.; Chau, M.; Koury, H.F.; Brenner, D.R. Morphology of the major papilla predicts ERCP procedural outcomes and adverse events. Surg. Endosc. 2021, 35, 6455–6465. [Google Scholar] [CrossRef] [PubMed]
- Cotton, P.B.; Eisen, G.M.; Aabakken, L.; Baron, T.H.; Hutter, M.M.; Jacobson, B.C.; Mergener, K.; Nemcek, A., Jr.; Petersen, B.T.; Petrini, J.L.; et al. A lexicon for endoscopic adverse events: Report of an ASGE workshop. Gastrointest. Endosc. 2010, 71, 446–454. [Google Scholar] [CrossRef]
- Buxbaum, J.L.; Freeman, M.; Amateau, S.K.; Chalhoub, J.M.; Chowdhury, A.; Coelho-Prabhu, N.; Das, R.; Desai, M.; Elhanafi, S.E.; Forbes, N.; et al. American Society for Gastrointestinal Endoscopy guideline on post-ERCP pancreatitis prevention strategies: Methodology and review of evidence. Gastrointest. Endosc. 2023, 97, 163–183.e40. [Google Scholar] [CrossRef]
- Fernandes, J.; Canena, J.; Moreira, M.; Alexandrino, G.; Figueiredo, L.; Araújo, T.; Lourenço, L.; Horta, D.; Lopes, L. Needle knife fistulotomy in flat and diverticular papillae: Is it time for redemption? Hepatobiliary Pancreat. Dis. Int. 2022, 21, 175–181. [Google Scholar] [CrossRef]
- Park, C.S.; Park, C.H.; Koh, H.R.; Jun, C.H.; Ki, H.S.; Park, S.Y.; Kim, H.S.; Choi, S.K.; Rew, J.S. Needle-knife fistulotomy in patients with periampullary diverticula and difficult bile duct cannulation. J. Gastroenterol. Hepatol. 2012, 27, 1480–1483. [Google Scholar] [CrossRef]
- Arabpour, E.; Sadeghi, A.; Rashtchian, A.; Rastegar, R.; Abdehagh, M.; Zali, M.R. Impact of periampullary diverticulum and relevant cannulation techniques on the outcomes of endoscopic retrograde cholangiopancreatography: A retrospective study. BMC Gastroenterol. 2025, 25, 665. [Google Scholar] [CrossRef]
- Kim, H.W.; Kang, D.H.; Choi, C.W.; Park, J.H.; Lee, J.H.; Kim, M.D.; Kim, I.D.; Yoon, K.T.; Cho, M.; Jeon, U.B.; et al. Limited endoscopic sphincterotomy plus large balloon dilation for choledocholithiasis with periampullary diverticula. World J. Gastroenterol. 2010, 16, 4335–4340. [Google Scholar] [CrossRef]
- Kim, C.W.; Chang, J.H.; Kim, J.H.; Kim, T.H.; Lee, I.S.; Han, S.W. Size and type of periampullary duodenal diverticula are associated with bile duct diameter and recurrence of bile duct stones. J. Gastroenterol. Hepatol. 2013, 28, 893–898. [Google Scholar] [CrossRef]
- Haraldsson, E.; Kylänpää, L.; Grönroos, J.; Saarela, A.; Toth, E.; Qvigstad, G.; Hult, M.; Lindström, O.; Laine, S.; Karjula, H.; et al. Macroscopic appearance of the major duodenal papilla influences bile duct cannulation: A prospective multicenter study by the Scandinavian Association for Digestive Endoscopy Study Group for ERCP. Gastrointest. Endosc. 2019, 90, 957–963. [Google Scholar] [CrossRef]
- Angsuwatcharakon, P.; Thongsuwan, C.; Ridtitid, W.; Piyachaturawat, P.; Kulpatcharapong, S.; Kongkam, P.; Rerknimitr, R. Morphology of the major duodenal papilla for the selection of advanced cannulation techniques in difficult biliary cannulation. Surg. Endosc. 2023, 37, 5807–5815. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.S.; Xu, J.H.; Dong, Z.Q.; Gao, P.; Shen, Y.C. Success and Safety of Needle Knife Papillotomy and Fistulotomy Based on Papillary Anatomy: A Prospective Controlled Trial. Dig. Dis. Sci. 2022, 67, 1901–1909. [Google Scholar] [CrossRef] [PubMed]
- Horiuchi, A.; Nakayama, Y.; Kajiyama, M.; Tanaka, N. Effect of precut sphincterotomy on biliary cannulation based on the characteristics of the major duodenal papilla. Clin. Gastroenterol. Hepatol. 2007, 5, 1113–1118. [Google Scholar] [CrossRef]
- Lyu, Y.; Ye, S.; Wang, B. Impact of duodenal papilla anatomy on needle knife papillotomy safety and efficacy in patients with difficult biliary canulation. BMC Surg. 2024, 24, 61. [Google Scholar] [CrossRef] [PubMed]
- Fogel, E.L.; Sherman, S.; Lehman, G.A. Increased selective biliary cannulation rates in the setting of periampullary diverticula: Main pancreatic duct stent placement followed by pre-cut biliary sphincterotomy. Gastrointest. Endosc. 1998, 47, 396–400. [Google Scholar] [CrossRef]
| Overall (n = 122) | NKPS Success Group (n = 82) | NKPS Failure Group (n = 40) | p-Value | |
|---|---|---|---|---|
| Age, years (range) | 75 (35–94) | 75 (35–94) | 76 (51–92) | 0.654 |
| Male, n | 60 (49.2%) | 42 (51.2%) | 18 (45%) | 0.519 |
| Indication of ERCP, n | ||||
| Choledocholithiasis | 105 (86.1%) | 70 (85.3%) | 35 (87.5%) | 0.585 |
| Malignant stricture | 11 (9%) | 7 (8.5%) | 4 (10.0%) | 0.235 |
| Benign stricture | 3 (2.5%) | 2 (2.4%) | 1 (2.5%) | 0158 |
| Bile leakage | 3 (2.5%) | 3 (8.5%) | 0 (0.0%) | 0.244 |
| CBD diameter, cm | 1.1 (0.3–3.0) | 1.1 (0.3–2.7) | 1.0 (0.4–3.0) | 0.336 |
| Type of diverticulum, n | ||||
| Type I | 8 (6.6%) | 4 (4.9%) | 4 (10.0%) | 0.179 |
| Type II | 86 (70.5%) | 57 (69.5%) | 29 (72.5%) | 0.078 |
| Type III | 28 (23.0%) | 21 (25.6%) | 7 (17.5%) | 0.123 |
| Diverticulum diameter, cm | 0.8 (0.2–2) | 0.8 (0.2–2) | 1.0 (0.3–1.9) | 0.001 |
| Morphology of papilla, n | ||||
| Type I | 57 (46.7%) | 42 (51.2%) | 15 (37.5%) | 0.154 |
| Type II | 34 (27.9%) | 13 (15.9%) | 21 (52.5%) | <0.001 |
| Type III | 14 (11.5%) | 13 (15.9%) | 1 (2.5%) | 0.030 |
| Type IV | 17 (13.9%) | 14 (17.1%) | 3 (7.5%) | 0.158 |
| Bleeding during NKPS, n | 28 (22.9%) | 10 (12.2%) | 18 (45.0%) | <0.001 |
| Pancreatic stent | 32 (26.2%) | 23 (28.0%) | 9 (22.5%) | 0.662 |
| Surgically altered anatomy, n | 5 | 4 | 1 | 0.736 |
| B-II anastomosis | 4 (3.3%) | 3 (3.7%) | 1 (2.5%) | 0.689 |
| Roux-en-Y anastomosis | 1 (0.8%) | 1 (1.2%) | 0 | 0.998 |
| Adverse events of ERCP, n | ||||
| Overall | 20 (16.4%) | 13 (15.9%) | 7 (17.5%) | 0.485 |
| Pancreatitis | 8 (6.6%) | 4 (4.9%) | 4 (10.0%) | 0.283 |
| Delayed bleeding | 7 (5.7%) | 5 (6.1%) | 2 (5.0%) | 0.807 |
| Cholangitis | 5 (4.1%) | 4 (4.9%) | 1 (2.5%) | 0.534 |
| Perforation | 0 | 0 | 0 | 0.999 |
| Type I (n = 8) | Type II (n = 86) | Type III (n = 28) | p-Value | |
|---|---|---|---|---|
| Age, years | 69.5 (69–74.8) | 77 (66–84) | 72 (62–79) | 0.188 |
| Male, n (%) | 7 (87.5%) | 39 (45.3%) | 14 (50%) | 0.074 |
| Indication of ERCP, n | ||||
| Choledocholithiasis | 1 (12.5%) | 76 (88.4%) | 22 (78.6%) | 0.088 |
| Malignant stricture | 6 (75.0%) | 7 (8.1%) | 3 (10.7%) | 0.136 |
| Benign stricture | 1 (12.5%) | 1 (1.2%) | 2 (7.1%) | 0.255 |
| Bile leakage | 0 | 2 (2.4%) | 1 (3.6%) | 0.263 |
| CBD diameter, cm | 1.4 (0.5–2.8) | 1.1 (0.3–3.0) | 1.0 (0.6–8.0) | 0.859 |
| Diverticulum diameter, cm | 1.2 (0.5–1.9) | 0.9 (0.3–2.0) | 0.5 (0.2–1.9) | <0.001 |
| NKPS success, n | 4 (50%) | 57 (66.3%) | 21 (75%) | 0.3910 |
| Adverse events, n | ||||
| Overall | 1 (12.5%) | 15 (17.4%) | 6 (21.5%) | 0.385 |
| Pancreatitis | 0 | 7 (8.1%) | 1 (3.6%) | 0.164 |
| Delayed bleeding | 1 (12.5%) | 7 (8.1%) | 1 (3.6%) | 0.225 |
| Cholangitis | 0 | 1 (1.2%) | 4 (14.3%) | 0.365 |
| Type I (n = 57) | Type II (n = 34) | Type III (n = 14) | Type IV (n = 17) | p-Value | |
|---|---|---|---|---|---|
| Bleeding during NKPS | 11 (19.3%) | 9 (26.5%) | 3 (21.4%) | 5 (29.4%) | 0.290 |
| NKPS success, n | 42 (73.7%) | 13 (38.2%) | 13 (92.9%) | 14 (82.4%) | 0.059 |
| Adverse events, n | |||||
| Overall | 9 (15.8%) | 4 (11.7%) | 3 (21.4%) | 4 (23.5%) | 0.884 |
| Pancreatitis | 4 (7.0%) | 1 (2.9%) | 0 | 3 (17.6%) | 0.162 |
| Delayed bleeding | 3 (5.3%) | 1 (2.9%) | 2 (14.3%) | 1 (5.9%) | 0.492 |
| Cholangitis | 2 (3.5%) | 2 (5.9%) | 1 (7.1%) | 0 | 0.710 |
| Variables | Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | ||
| Age | >70 y | 1.071 (0.486–2.361) | 0.864 | ||
| ≤70 y | Referent | ||||
| Gender | Male | 1.283 (0.601–2.740) | 0.519 | ||
| Female | Referent | ||||
| Choledocholithiasis | Yes | 0.500 (0.054–4.626) | 0.570 | ||
| No | Referent | ||||
| Malignant biliary stricture | Yes | 0.840 (0.231–3.055) | 0.791 | ||
| No | Referent | ||||
| CBD diameter (cm) | >6 mm | 1.029 (0.327–3.239) | 0.962 | ||
| ≤6 mm | Referent | ||||
| Morphology of papilla | Type II | 0.221 (0.089–0.549) | 0.001 | 0.331 (0.123–0.887) | 0.028 |
| Type III | 4.643 (0.559–38.590) | 0.155 | 9.122 (0.886–93.924) | 0.063 | |
| Type IV | 1.667 (0.420–6.620) | 0.468 | 2.66 (0.572–12.373) | 0.212 | |
| Type I | Referent | Referent | |||
| Type of diverticulum | Type I | 0.333 (0.065–1.699) | 0.402 | ||
| Type II | 0.655 (0.250–1.720) | 0.502 | |||
| Type III | Referent | ||||
| Diverticulum diameter | Every 1 cm increase | 0.213 (0.082–0.555) | 0.002 | 0.408 (0.252–1.121) | 0.202 |
| Surgically altered anatomy | Yes | 1.481 | 0.737 | ||
| No | Referent | Referent | |||
| Bleeding during NKPS | Yes | 0.170 (0.068–0.421) | <0.001 | 0.117 (0.039–0.351) | <0.001 |
| No | Referent | Referent | |||
| Endoscopist | B + C + D + E | 0.898 | 0.688 | ||
| A | Referent | ||||
| Pancreatic stent | Yes | 1.343 (0.554–3.253) | 0.514 | ||
| no | Referent | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, K.-T.; Wang, S.-F.; Wu, C.-H.; Lee, M.-H.; Tsou, Y.-K.; Lin, C.-H.; Sung, K.-F.; Liu, N.-J. Impact of Papillary Morphology and Diverticular Type on Needle-Knife Papillotomy in Patients with Periampullary Diverticulum with Difficult Biliary Cannulation. J. Clin. Med. 2025, 14, 8208. https://doi.org/10.3390/jcm14228208
Liu K-T, Wang S-F, Wu C-H, Lee M-H, Tsou Y-K, Lin C-H, Sung K-F, Liu N-J. Impact of Papillary Morphology and Diverticular Type on Needle-Knife Papillotomy in Patients with Periampullary Diverticulum with Difficult Biliary Cannulation. Journal of Clinical Medicine. 2025; 14(22):8208. https://doi.org/10.3390/jcm14228208
Chicago/Turabian StyleLiu, Kuan-Ting, Sheng-Fu Wang, Chi-Huan Wu, Mu-Hsien Lee, Yung-Kuan Tsou, Cheng-Hui Lin, Kai-Feng Sung, and Nai-Jen Liu. 2025. "Impact of Papillary Morphology and Diverticular Type on Needle-Knife Papillotomy in Patients with Periampullary Diverticulum with Difficult Biliary Cannulation" Journal of Clinical Medicine 14, no. 22: 8208. https://doi.org/10.3390/jcm14228208
APA StyleLiu, K.-T., Wang, S.-F., Wu, C.-H., Lee, M.-H., Tsou, Y.-K., Lin, C.-H., Sung, K.-F., & Liu, N.-J. (2025). Impact of Papillary Morphology and Diverticular Type on Needle-Knife Papillotomy in Patients with Periampullary Diverticulum with Difficult Biliary Cannulation. Journal of Clinical Medicine, 14(22), 8208. https://doi.org/10.3390/jcm14228208






