Effect of Mandibular Advancement Device Treatment on the Site-Specific Degree of Upper Airway Collapse During Drug-Induced Sleep Endoscopy †
Abstract
1. Introduction
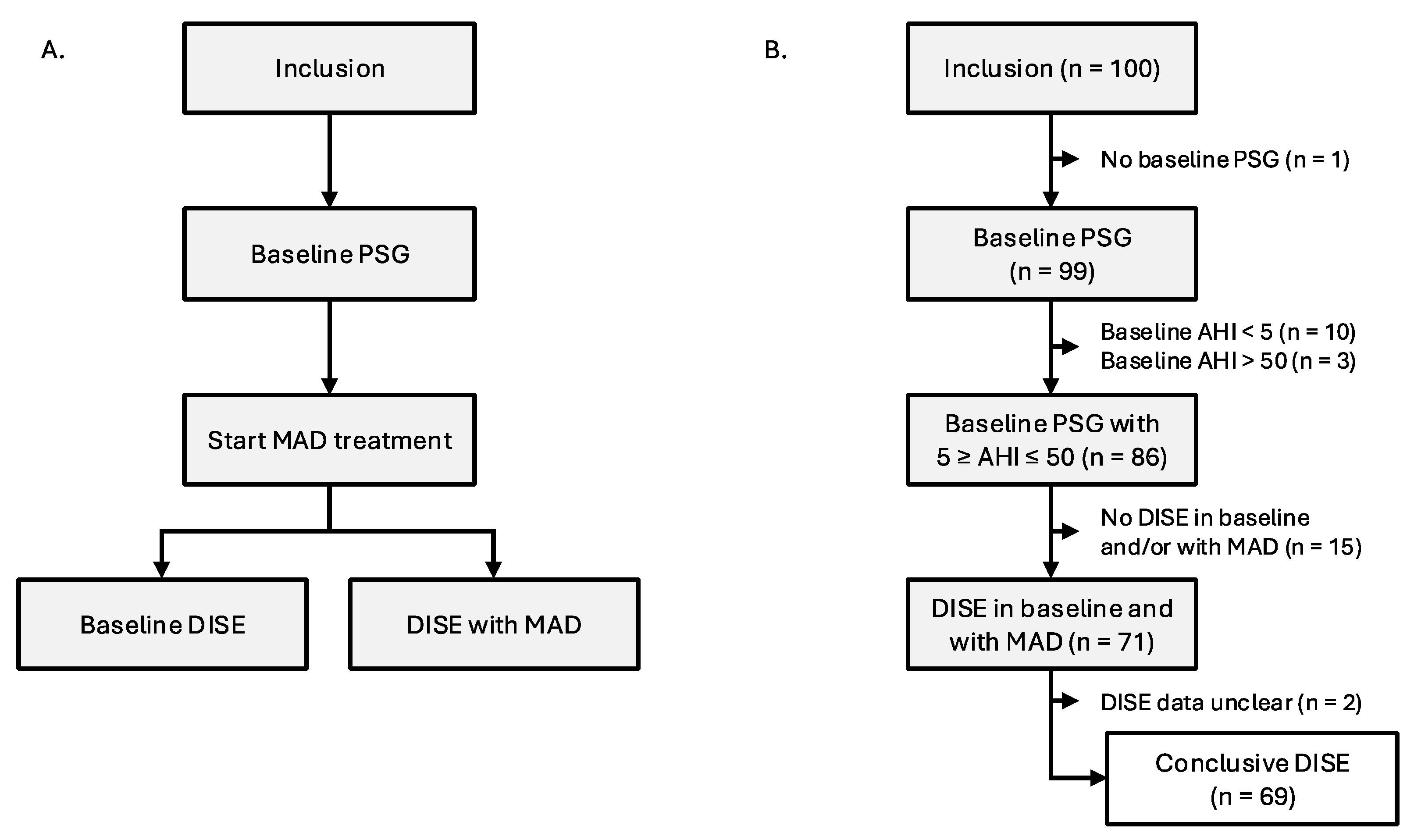
2. Materials and Methods
2.1. Drug-Induced Sleep Endoscopy
2.2. Statistical Analyses
- with treatment = 0 at baseline; treatment = 1 with MAD; and
- with j = boundaries for the three categories (1 = none vs. partial collapse; 2 = partial vs. complete collapse).
3. Results
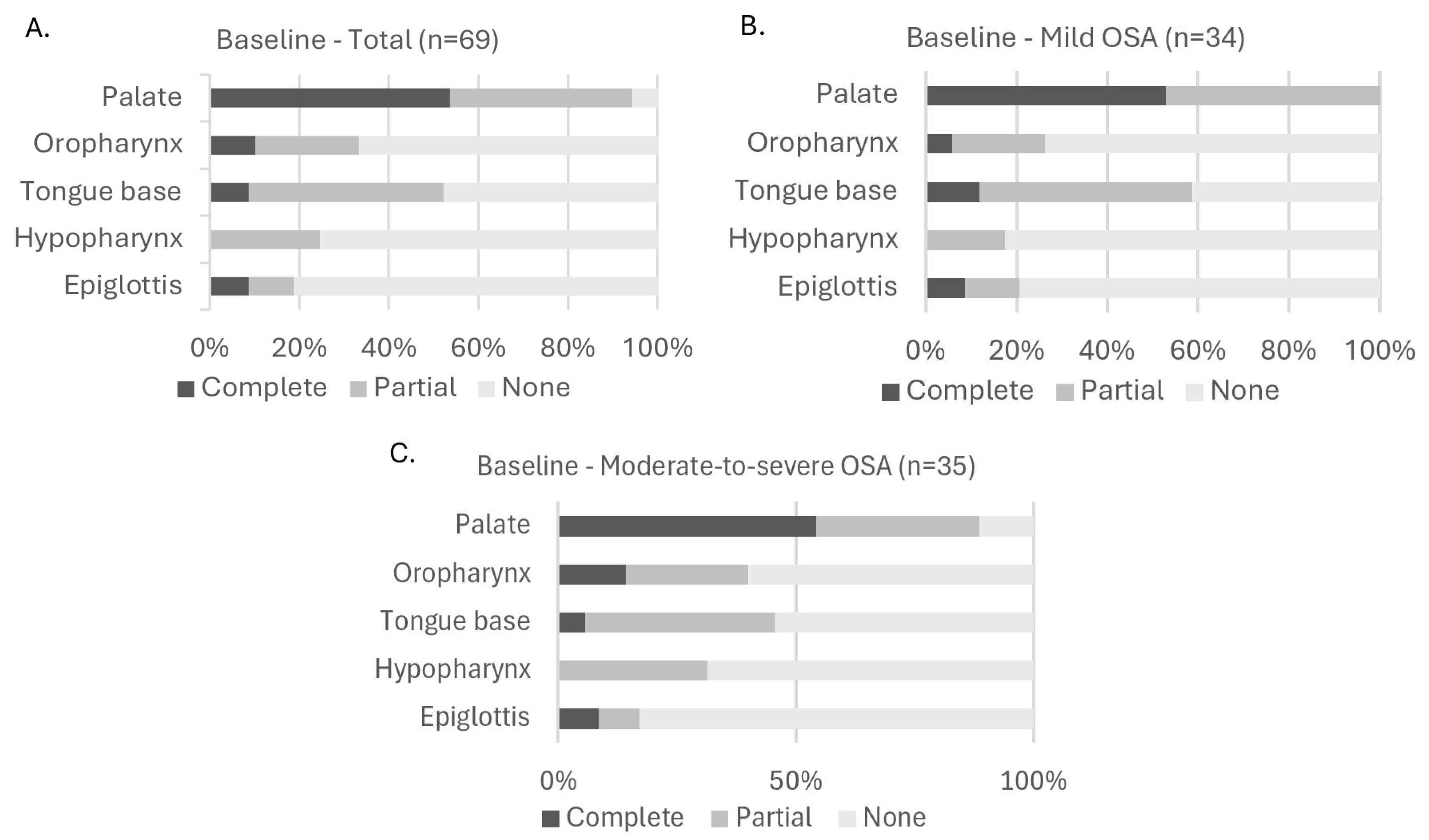
3.1. Population Characteristics at Baseline
3.2. Population Characteristics During MAD Therapy
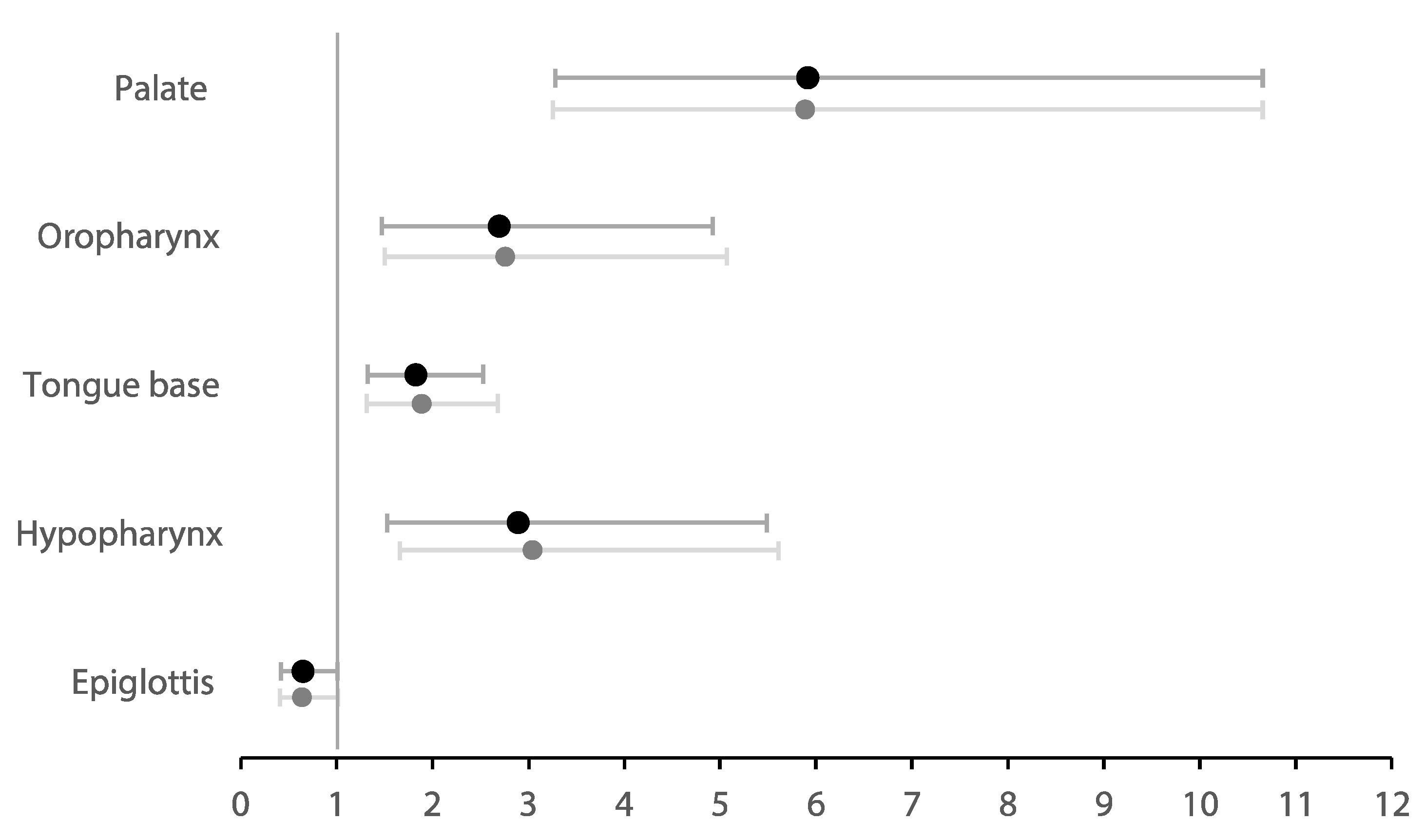
3.3. Regression Analysis
3.4. Exploratory Analyses
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AHI | Apnea–hypopnea index |
| BIS | Bispectral index |
| BMI | Body mass index |
| CCC | Complete concentric collapse |
| CPAP | Continuous positive airway pressure |
| DISE | Drug-induced sleep endoscopy |
| ENT | Ear, nose, and throat |
| ESS | Epworth sleepiness scale |
| MAD | Mandibular advancement device |
| ODI | Oxygen desaturation index |
| OR | Odds ratio |
| OSA | Obstructive sleep apnea |
| PSG | Polysomnography |
| SD | Standard deviation |
| SaO2 | Oxygen saturation |
| VAS | Visual analog scale for snoring |
References
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef]
- Marin, J.M.; Carrizo, S.J.; Vicente, E.; Agusti, A.G.N. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: An observational study. Lancet 2005, 365, 1046–1053. [Google Scholar] [CrossRef]
- Dodds, S.; Williams, L.J.; Roguski, A.; Vennelle, M.; Douglas, N.J.; Kotoulas, S.-C.; Riha, R.L. Mortality and morbidity in obstructive sleep apnoea–hypopnoea syndrome: Results from a 30-year prospective cohort study. ERJ Open Res. 2020, 6, 00057–02020. [Google Scholar] [CrossRef] [PubMed]
- Ayas, N.T.; Taylor, C.M.; Laher, I. Cardiovascular consequences of obstructive sleep apnea. Curr. Opin. Cardiol. 2016, 31, 599–605. [Google Scholar] [CrossRef]
- Marshall, N.S.; Wong, K.K.H.; Cullen, S.R.J.; Knuiman, M.W.; Grunstein, R.R. Sleep Apnea and 20-Year Follow-Up for All-Cause Mortality, Stroke, and Cancer Incidence and Mortality in the Busselton Health Study Cohort. J. Clin. Sleep Med. 2014, 10, 355–362. [Google Scholar] [CrossRef]
- Wang, X.; Ouyang, Y.; Wang, Z.; Zhao, G.; Liu, L.; Bi, Y. Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: A meta-analysis of prospective cohort studies. Int. J. Cardiol. 2013, 169, 207–214. [Google Scholar] [CrossRef]
- Sullivan, C.; Berthon-Jones, M.; Issa, F.; Eves, L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet 1981, 317, 862–865. [Google Scholar] [CrossRef]
- Verbraecken, J.; Dieltjens, M.; Op de Beeck, S.; Vroegop, A.; Braem, M.; Vanderveken, O.; Randerath, W. Non-CPAP therapy for obstructive sleep apnoea. Breathe 2022, 18, 220164. [Google Scholar] [CrossRef] [PubMed]
- Randerath, W.; Verbraecken, J.; de Raaff, C.A.L.; Hedner, J.; Herkenrath, S.; Hohenhorst, W.; Jakob, T.; Marrone, O.; Marklund, M.; McNicholas, W.T.; et al. European Respiratory Society guideline on non-CPAP therapies for obstructive sleep apnoea. Eur. Respir. Rev. 2021, 30, 210200. [Google Scholar] [CrossRef] [PubMed]
- Randerath, W.J.; Verbraecken, J.; Andreas, S.; Bettega, G.; Boudewyns, A.; Hamans, E.; Jalbert, F.; Paoli, J.R.; Sanner, B.; Smith, I.; et al. Non-CPAP therapies in obstructive sleep apnoea. Eur. Respir. J. 2011, 37, 1000–1028. [Google Scholar] [CrossRef]
- Kim, H.K.; Kim, M.E. Treatment Outcomes of Mandibular Advancement Devices in Mild, Moderate, and Severe Obstructive Sleep Apnea: A Preliminary Study. JOMP 2023, 48, 96–105. [Google Scholar] [CrossRef]
- Phillips, C.L.; Grunstein, R.R.; Darendeliler, M.A.; Mihailidou, A.S.; Srinivasan, V.K.; Yee, B.J.; Marks, G.B.; Cistulli, P.A. Health Outcomes of Continuous Positive Airway Pressure versus Oral Appliance Treatment for Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2013, 187, 879–887. [Google Scholar] [CrossRef]
- Chan, A.S.L.; Sutherland, K.; Schwab, R.J.; Zeng, B.; Petocz, P.; Lee, R.W.W.; Darendeliler, M.A.; Cistulli, P.A. The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax 2010, 65, 726–732. [Google Scholar] [CrossRef]
- Sangalli, L.; Yanez-Regonesi, F.; Moreno-Hay, I. Evolution of adherence and self-reported symptoms over 36 months with mandibular advancement device therapy for obstructive sleep apnea: A retrospective study. J. Clin. Sleep Med. 2024, 20, 487–496. [Google Scholar] [CrossRef]
- Durán-Cantolla, J.; Crovetto-Martínez, R.; Alkhraisat, M.H.; Crovetto, M.; Municio, A.; Kutz, R.; Aizpuru, F.; Miranda, E.; Anitua, E. Efficacy of mandibular advancement device in the treatment of obstructive sleep apnea syndrome: A randomized controlled crossover clinical trial. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e605–e615. [Google Scholar] [CrossRef]
- Liao, J.; Shi, Y.; Gao, X.; Zhang, B.; Li, Y.; Xu, W.; Han, D. Efficacy of Oral Appliance for Mild, Moderate, and Severe Obstructive Sleep Apnea: A Meta-analysis. Otolaryngol.–Head Neck Surg. 2024, 170, 1270–1279. [Google Scholar] [CrossRef]
- Leibovitz, S.; Levi, S.; Hanut, A.; Yanko, R.; Sharav, Y.; Haviv, Y. Evaluating the effectiveness of mandibular advancement devices in treating very severe obstructive sleep apnea: A retrospective cohort study. Sleep Breath. 2025, 29, 84. [Google Scholar] [CrossRef]
- Guimarães, M.d.L.R.; Hermont, A.P.; Guimarães, T.M.; Dal-Fabbro, C.; Bittencourt, L.; Chaves Junior, C.M. Severe obstructive sleep apnea treatment with mandibular advancement device: A case report. Sleep Sci. 2018, 11, 118–122. [Google Scholar] [CrossRef]
- Colpani, J.T.; Ou, Y.-H.; Kosasih, A.M.; Lee, F.K.F.; Chan, S.-P.; Tan, H.H.; Wong, R.C.W.; Chin, C.W.; Cistulli, P.A.; Lee, C.-H. Mandibular Advancement Device Versus CPAP in Severe Obstructive Sleep Apnea. J. Dent. Res. 2025; Online ahead of print. [Google Scholar] [CrossRef]
- Cunha, T.C.A.; GuimarÃEs, T.d.M.; Schultz, T.C.B.; Almeida, F.R.d.; Cunha, T.M.; Simamoto Junior, P.C.; Bittencourt, L.R.A. Predictors of success for mandibular repositioning appliance in obstructive sleep apnea syndrome. Braz. Oral Res. 2017, 31, e37. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, K.A.; Cartwright, R.; Rogers, R.; Schmidt-Nowara, W. Oral Appliances for Snoring and Obstructive Sleep Apnea: A Review. Sleep 2006, 29, 244–262. [Google Scholar] [CrossRef] [PubMed]
- Zinchuk, A.V.; Gentry, M.J.; Concato, J.; Yaggi, H.K. Phenotypes in obstructive sleep apnea: A definition, examples and evolution of approaches. Sleep Med. Rev. 2017, 35, 113–123. [Google Scholar] [CrossRef]
- Jordan, A.S.; McSharry, D.G.; Malhotra, A. Adult obstructive sleep apnoea. Lancet 2014, 383, 736–747. [Google Scholar] [CrossRef]
- Eckert, D.J.; Malhotra, A. Pathophysiology of Adult Obstructive Sleep Apnea. Proc. Am. Thorac. Soc. 2008, 5, 144–153. [Google Scholar] [CrossRef]
- Eckert, D.J.; White, D.P.; Jordan, A.S.; Malhotra, A.; Wellman, A. Defining Phenotypic Causes of Obstructive Sleep Apnea. Identification of Novel Therapeutic Targets. Am. J. Respir. Crit. Care Med. 2013, 188, 996–1004. [Google Scholar] [CrossRef]
- Carrasco-Llatas, M.; Matarredona-Quiles, S.; De Vito, A.; Chong, K.B.; Vicini, C. Drug-Induced Sleep Endoscopy: Technique, Indications, Tips and Pitfalls. Healthcare 2019, 7, 93. [Google Scholar] [CrossRef] [PubMed]
- De Vito, A.; Carrasco Llatas, M.; Ravesloot, M.J.; Kotecha, B.; De Vries, N.; Hamans, E.; Maurer, J.; Bosi, M.; Blumen, M.; Heiser, C.; et al. European position paper on drug-induced sleep endoscopy: 2017 Update. Clin. Otolaryngol. 2018, 43, 1541–1552. [Google Scholar] [CrossRef] [PubMed]
- De Corso, E.; Bastanza, G.; Della Marca, G.; Grippaudo, C.; Rizzotto, G.; Marchese, M.R.; Fiorita, A.; Sergi, B.; Meucci, D.; Di Nardo, W.; et al. Drug-induced sleep endoscopy as a selection tool for mandibular advancement therapy by oral device in patients with mild to moderate obstructive sleep apnoea. Acta Otorhinolaryngol. Ital. 2015, 35, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Huntley, C.; Cooper, J.; Stiles, M.; Grewal, R.; Boon, M. Predicting Success of Oral Appliance Therapy in Treating Obstructive Sleep Apnea Using Drug-Induced Sleep Endoscopy. J. Clin. Sleep Med. 2018, 14, 1333–1337. [Google Scholar] [CrossRef]
- Johal, A.; Hector, M.P.; Battagel, J.M.; Kotecha, B.T. Impact of sleep nasendoscopy on the outcome of mandibular advancement splint therapy in subjects with sleep-related breathing disorders. J. Laryngol. Otol. 2007, 121, 668–675. [Google Scholar] [CrossRef]
- Verbruggen, A.; Vroegop, A.; Dieltjens, M.; Wouters, K.; Kastoer, C.; De Backer, J.; Verbraecken, J.; Willemen, M.; Van de Heyning, P.; Braem, M.; et al. Predicting Therapeutic Outcome of Mandibular Advancement Device Treatment in Obstructive Sleep Apnoea (PROMAD): Study Design and Baseline Characteristics. J. Dent. Sleep Med. 2016, 3, 119–138. [Google Scholar] [CrossRef]
- Collop, N.A.; Anderson, W.M.; Boehlecke, B.; Claman, D.; Goldberg, R.; Gottlieb, D.J.; Hudgel, D.; Sateia, M.; Schwab, R. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2007, 3, 737–747. [Google Scholar]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2017, 13, 479–504. [Google Scholar] [CrossRef]
- Iber, C.; Ancoli-Israel, S.; Chesson, A.L.; Quan, S. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology, and Technical Specification. 2007. Available online: https://pulmo-ua.com/wp-content/uploads/2021/12/AASM-sleep-scoring-2017.pdf (accessed on 2 May 2025).
- Op de Beeck, S.; Dieltjens, M.; Azarbarzin, A.; Willemen, M.; Verbraecken, J.; Braem, M.J.; Wellman, A.; Sands, S.A.; Vanderveken, O.M. Mandibular Advancement Device Treatment Efficacy Is Associated with Polysomnographic Endotypes. Ann. Am. Thorac. Soc. 2021, 18, 511–518. [Google Scholar] [CrossRef]
- Babar-Craig, H.; Rajani, N.K.; Bailey, P.; Kotecha, B.T. Validation of sleep nasendoscopy for assessment of snoring with bispectral index monitoring. Eur. Arch. Oto-Rhino-Laryngol. 2012, 269, 1277–1279. [Google Scholar] [CrossRef] [PubMed]
- Kezirian, E.J.; Hohenhorst, W.; de Vries, N. Drug-induced sleep endoscopy: The VOTE classification. Eur. Arch. Oto-Rhino-Laryngol. 2011, 268, 1233–1236. [Google Scholar] [CrossRef] [PubMed]
- Op de Beeck, S.; Dieltjens, M.; Verbruggen, A.E.; Vroegop, A.V.; Wouters, K.; Hamans, E.; Willemen, M.; Verbraecken, J.; De Backer, W.A.; Van de Heyning, P.H.; et al. Phenotypic Labelling Using Drug-Induced Sleep Endoscopy Improves Patient Selection for Mandibular Advancement Device Outcome: A Prospective Study. J. Clin. Sleep Med. 2019, 15, 1089–1099. [Google Scholar] [CrossRef] [PubMed]
- Buyse, B.; Nguyen, P.A.H.; Leemans, J.; Verhaeghe, V.; Peters, M.; Strobbe, S.; Valckenborgh, I.V.; Belge, C.; Testelmans, D. Short-term positive effects of a mandibular advancement device in a selected phenotype of patients with moderate obstructive sleep apnea: A prospective study. J. Clin. Sleep Med. 2023, 19, 5–16. [Google Scholar] [CrossRef]
- Kim, H.-Y.; Sung, C.-M.; Jang, H.-B.; Kim, H.C.; Lim, S.C.; Yang, H.C. Patients with epiglottic collapse showed less severe obstructive sleep apnea and good response to treatment other than continuous positive airway pressure: A case-control study of 224 patients. J. Clin. Sleep Med. 2021, 17, 413–419. [Google Scholar] [CrossRef]
- Van de Perck, E.; Dieltjens, M.; Vroegop, A.V.; Verbraecken, J.; Braem, M.; Vanderveken, O.M. Mandibular advancement device therapy in patients with epiglottic collapse. Sleep Breath. 2022, 26, 1915–1920. [Google Scholar] [CrossRef]
- Fernández-Sanjuán, P.; Alcaraz, M.; Bosco, G.; Pérez-Martín, N.; Morato, M.; Lugo, R.; Arrieta, J.J.; Sanabria, J.; Ríos-Lago, M.; Plaza, G. Modifications in Upper Airway Collapsibility during Sleep Endoscopy with a Mandibular Positioner: Study in Snorers and Obstructive Sleep Apnea Patients. J. Clin. Med. 2024, 13, 1184. [Google Scholar] [CrossRef]
- Sanchez-Azofra, A.; Malhotra, A.; Owens, R.L.; Healy, W.J. Obstructive Sleep Apnea: Pathophysiology and Endotypes. ATS Sch. 2023, 4, 567–568. [Google Scholar] [CrossRef]
- Van den Bossche, K.; Op de Beeck, S.; Dieltjens, M.; Verbruggen, A.E.; Vroegop, A.V.; Verbraecken, J.A.; Van de Heyning, P.H.; Braem, M.J.; Vanderveken, O.M. Multimodal phenotypic labelling using drug-induced sleep endoscopy, awake nasendoscopy and computational fluid dynamics for the prediction of mandibular advancement device treatment outcome: A prospective study. J. Sleep Res. 2022, 31, e13673. [Google Scholar] [CrossRef]
- Dieltjens, M.; Vanderveken, O.M.; Van de Heyning, P.H.; Braem, M.J. Current opinions and clinical practice in the titration of oral appliances in the treatment of sleep-disordered breathing. Sleep Med. Rev. 2012, 16, 177–185. [Google Scholar] [CrossRef]
- Kezirian, E.J.; White, D.P.; Malhotra, A.; Ma, W.; McCulloch, C.E.; Goldberg, A.N. Interrater Reliability of Drug-Induced Sleep Endoscopy. Arch. Otolaryngol.–Head Neck Surg. 2010, 136, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Koo, S.K.; Lee, S.H.; Koh, T.K.; Kim, Y.J.; Moon, J.S.; Lee, H.B.; Park, G.H. Inter-rater reliability between experienced and inexperienced otolaryngologists using Koo’s drug-induced sleep endoscopy classification system. Eur. Arch. Oto-Rhino-Laryngol. 2019, 276, 1525–1531. [Google Scholar] [CrossRef] [PubMed]
- Vroegop, A.V.; Vanderveken, O.M.; Boudewyns, A.N.; Scholman, J.; Saldien, V.; Wouters, K.; Braem, M.J.; Van de Heyning, P.H.; Hamans, E. Drug-induced sleep endoscopy in sleep-disordered breathing: Report on 1249 cases. Laryngoscope 2014, 124, 797–802. [Google Scholar] [CrossRef]
- Vanderveken, O.M.; Maurer, J.T.; Hohenhorst, W.; Hamans, E.; Lin, H.-S.; Vroegop, A.V.; Anders, C.; Vries, N.d.; Heyning, P.H.V.d. Evaluation of Drug-Induced Sleep Endoscopy as a Patient Selection Tool for Implanted Upper Airway Stimulation for Obstructive Sleep Apnea. J. Clin. Sleep Med. 2013, 09, 433–438. [Google Scholar] [CrossRef]
- Ravesloot, M.J.L.; de Vries, N. One hundred consecutive patients undergoing drug-induced sleep endoscopy: Results and evaluation. Laryngoscope 2011, 121, 2710–2716. [Google Scholar] [CrossRef] [PubMed]
- Tukanov, E.; Op De Beeck, S.; Vroegop, A.; Braem, M.; Verbraecken, J.; Dieltjens, M.; Vanderveken, O.M. Effect of mandibular advancement device treatment on the degree of upper airway collapse during drug-induced sleep endoscopy. Chest 2024, 166, A6164–A6166. [Google Scholar] [CrossRef]

| Inclusion Criteria |
|
| Exclusion criteria |
|
| Total (n = 69) | Mild OSA: AHI < 15 (n = 34) | Moderate-to-Severe OSA: 15 ≥ AHI < 50 (n = 35) | p-Value | |
|---|---|---|---|---|
| Sex (male/female; n) | 59/10 | 28/6 | 31/4 | 0.513 a |
| Age (years) | 48.4 ± 9.5 | 48.7 ± 11.1 | 48.1 ± 7.9 | 0.780 b |
| BMI (kg/m2) | 27.5 ± 3.1 | 26.7 ± 3.3 | 28.3 ± 2.6 | 0.025 b |
| VAS (0–10) snoring | 6.0 (5.0–9.0) | 6.0 (5.0–9.0) | 7.0 (6.0–9.0) | 0.432 c |
| ESS (0–24) | 7.0 (5.0–13.5) | 7.5 (4.0–11.0) | 7.0 (5.0–15.0) | 0.318 c |
| AHI (events/h) | 16.5 (11.1–23.5) | 11.1 (7.3–12.8) | 23.3 (19.2–29.0) | <0.001 c |
| Supine AHI (events/h) | 29.4 (18.3–52.5) | 20.7 (12.3–36.0) | 40.4 (28.8–54.6) | 0.002 c |
| Non-supine AHI (events/h) | 8.9 (4.2–16.5) | 5.9 (3.0–8.7) | 15.7 (9.9–20.9) | <0.001 c |
| ODI (events/h) | 4.4 (2.4–10.9) | 2.6 (1.2–4.5) | 10.1 (3.8–15.5) | <0.001 c |
| Mean SaO2 (%) | 95.1 (94.1–96.1) | 95.5 (94.4–96.4) | 94.6 (93.6–95.7) | 0.026 c |
| Minimal SaO2 (%) | 87.0 (84.0–90.0) | 89.0 (84.6–91.0) | 86.0 (83.0–88.3) | 0.047 c |
| Total (n = 69) | ||||
|---|---|---|---|---|
| Site of Collapse | Ordinal Logistic Regression | + BMI + AHI | ||
| p | OR (95% CI) | p | OR (95% CI) | |
| Palate | <0.001 | 5.91 (3.28; 10.66) | <0.001 | 5.96 (3.29; 10.80) |
| Oropharynx | 0.001 | 2.70 (1.48; 4.92) | <0.001 | 2.81 (1.52; 5.18) |
| Tongue base | <0.001 | 1.83 (1.32; 2.53) | <0.001 | 1.90 (1.33; 2.70) |
| Hypopharynx | 0.001 | 2.90 (1.53; 5.48) | <0.001 | 3.17 (1.71; 5.88) |
| Epiglottis | 0.058 | 0.65 (0.42; 1.02) | 0.069 | 0.66 (0.42; 1.03) |
| Mild OSA: AHI < 15 (n = 34) | ||||
| Site of Collapse | Ordinal Logistic Regression | + BMI + AHI | ||
| p | OR (95% CI) | p | OR (95% CI) | |
| Palate | <0.001 | 7.70 (3.18; 18.64) | <0.001 | 7.78 (3.18; 19.06) |
| Oropharynx | 0.035 | 3.63 (1.09; 12.05) | 0.035 | 3.64 (1.09; 12.11) |
| Tongue base | 0.034 | 1.56 (1.03; 2.37) | 0.035 | 1.69 (1.04; 2.75) |
| Hypopharynx | 0.038 | 7.07 (1.11; 44.89) | 0.044 | 7.25 (1.06; 49.65) |
| Epiglottis | 0.664 | 0.89 (0.52; 1.52) | 0.755 | 0.92 (0.52; 1.60) |
| Moderate-to-Severe OSA: 15 ≥ AHI < 50 (n = 35) | ||||
| Site of Collapse | Ordinal Logistic Regression | + BMI + AHI | ||
| p | OR (95% CI) | p | OR (95% CI) | |
| Palate | <0.001 | 4.82 (22; 10.47) | <0.001 | 4.88 (2.25; 10.61) |
| Oropharynx | 0.014 | 2.43 (1.20; 4.94) | 0.007 | 2.64 (1.30; 5.36) |
| Tongue base | 0.003 | 2.24 (1.32; 3.79) | 0.003 | 2.24 (1.32; 3.80) |
| Hypopharynx | 0.019 | 2.22 (1.14; 4.30) | 0.006 | 2.90 (1.35; 6.19) |
| Epiglottis | 0.043 | 0.49 (0.23; 0.98) | 0.042 | 0.49 (0.24; 0.98) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tukanov, E.; Dieltjens, M.; Verbruggen, A.E.; Vroegop, A.V.; Verbraecken, J.A.; Van de Heyning, P.H.; Braem, M.J.; Op de Beeck, S.; Vanderveken, O.M. Effect of Mandibular Advancement Device Treatment on the Site-Specific Degree of Upper Airway Collapse During Drug-Induced Sleep Endoscopy. J. Clin. Med. 2025, 14, 8142. https://doi.org/10.3390/jcm14228142
Tukanov E, Dieltjens M, Verbruggen AE, Vroegop AV, Verbraecken JA, Van de Heyning PH, Braem MJ, Op de Beeck S, Vanderveken OM. Effect of Mandibular Advancement Device Treatment on the Site-Specific Degree of Upper Airway Collapse During Drug-Induced Sleep Endoscopy. Journal of Clinical Medicine. 2025; 14(22):8142. https://doi.org/10.3390/jcm14228142
Chicago/Turabian StyleTukanov, Eldar, Marijke Dieltjens, Annelies E. Verbruggen, Anneclaire V. Vroegop, Johan A. Verbraecken, Paul H. Van de Heyning, Marc J. Braem, Sara Op de Beeck, and Olivier M. Vanderveken. 2025. "Effect of Mandibular Advancement Device Treatment on the Site-Specific Degree of Upper Airway Collapse During Drug-Induced Sleep Endoscopy" Journal of Clinical Medicine 14, no. 22: 8142. https://doi.org/10.3390/jcm14228142
APA StyleTukanov, E., Dieltjens, M., Verbruggen, A. E., Vroegop, A. V., Verbraecken, J. A., Van de Heyning, P. H., Braem, M. J., Op de Beeck, S., & Vanderveken, O. M. (2025). Effect of Mandibular Advancement Device Treatment on the Site-Specific Degree of Upper Airway Collapse During Drug-Induced Sleep Endoscopy. Journal of Clinical Medicine, 14(22), 8142. https://doi.org/10.3390/jcm14228142









