Association Between the Blood Urea Nitrogen-to-Creatinine Ratio Trajectories and Clinical Outcomes in Critically Ill Hemorrhagic Stroke Patients: Insights from MIMIC-IV Database
Abstract
1. Introduction
2. Methods
2.1. Acknowledgements Statement
2.2. Patients and Data Collection
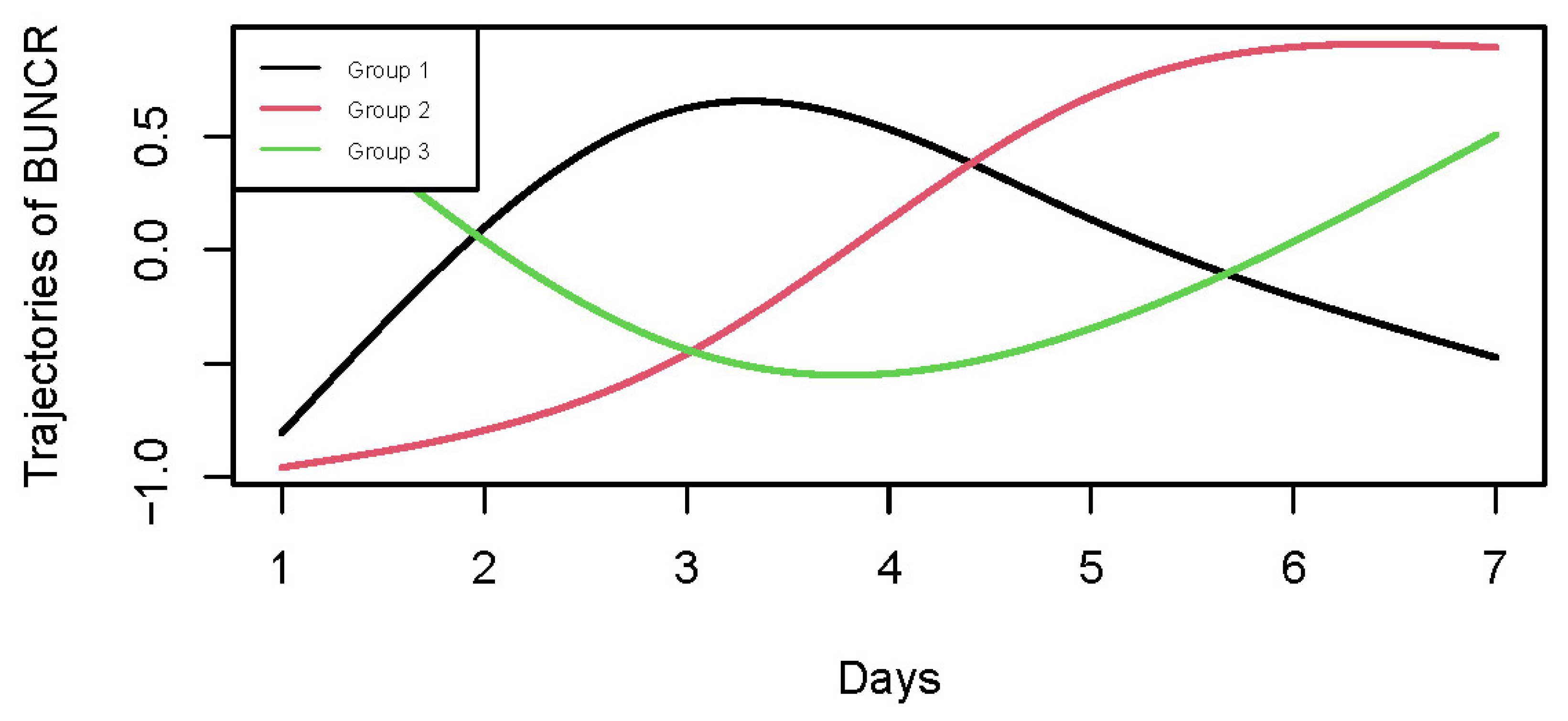
2.3. Group-Based Trajectory Models
2.4. Clinical Outcomes
2.5. Statistical Analysis
3. Results
3.1. BUNCR Trajectories and Baseline Characteristics
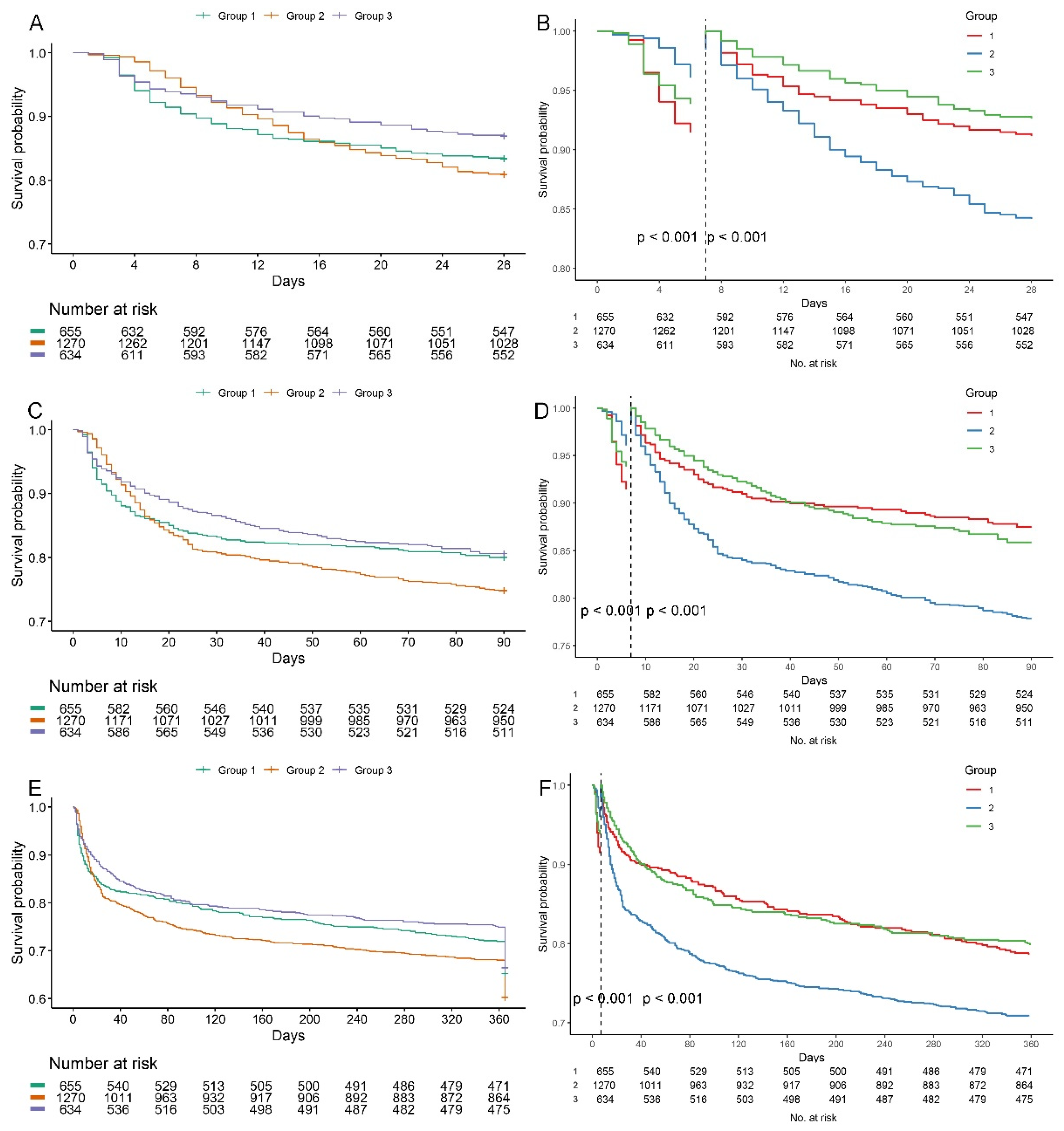
3.2. Association Between BUNCR Trajectories and Clinical Outcomes
3.3. Subgroup Analysis and Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HS | Hemorrhagic stroke |
| ICU | Intensive care unit |
| BUNCR | Blood urea nitrogen-to-creatinine ratio |
| GBTM | Group-based Trajectory Modeling |
| MIMIC-IV | Medical Information Mart for Intensive Care-IV |
| ACM | All-cause mortality |
| ICH | Intracerebral hemorrhage |
| TyG-i | Triglyceride-glucose index |
| HRR | Hemoglobin-to-red cell distribution width ratio |
| BUN | Blood urea nitrogen |
| ICD | International Classification of Diseases |
| SQL | Structured Query Language (SQL) |
| DBP | Diastolic blood pressure |
| MBP | Mean blood pressure (MBP) |
| SpO2 | Oxygen saturation measured via pulse oximetry |
| SOFA | Sequential Organ Failure Assessment |
| APS-III | Acute Physiology III score |
| SIRS | Systemic Inflammatory Response Syndrome |
| SAPS | Simplified Acute Physiology Score |
| OASIS | Oxford Acute Severity of Illness Score |
| GCS | Glasgow Coma Scale |
| Hb | Hemoglobin |
| RBC | Red blood cell count |
| WBC | White blood cell count |
| PLT | Platelet count |
| APTT | Activated partial thromboplastin time |
| PT | Prothrombin time |
| CCI | Charlson Comorbidity Index |
| PVD | Peripheral vascular disease |
| IVH | Intraventricular hemorrhage |
| CKD | Chronic-kidney disease |
| T2DM | Type 2 diabetes mellitus |
| T1DM | Type 1 diabetes mellitus |
| CHD | Coronary heart disease |
| COPD | Chronic obstructive pulmonary disease |
| MV | Mechanical ventilation |
| G1 | Group 1 |
| G2 | Group 2 |
| G3 | Group 3 |
| BIC | Bayesian Information Criterion |
| K-M | Kaplan–Meier |
| HR | Hazard ratio |
| CI | Confidence interval |
| GFR | Glomerular filtration rate |
| RAAS | Renin–angiotensin–aldosterone system |
| SCr | Serum creatinine |
References
- GBD 2021 Stroke Risk Factor Collaborators. Global, Regional, and National Burden of Stroke and Its Risk Factors, 1990–2021: A Systematic Analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 2024, 23, 973–1003. [Google Scholar] [CrossRef]
- Ali, M.; van Etten, E.S.; Akoudad, S.; Schaafsma, J.D.; Visser, M.C.; Ali, M.; Cordonnier, C.; Sandset, E.C.; Klijn, C.J.M.; Ruigrok, Y.M.; et al. Haemorrhagic Stroke and Brain Vascular Malformations in Women: Risk Factors and Clinical Features. Lancet Neurol. 2024, 23, 625–635. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Jiang, Y.; Cai, J.; Fan, H.Y.; Liang, J.; Yuan, R.; Wu, H.; Wang, Y.; Cheng, S.; Zhang, Y. Prediction of Prognosis in Patients with Nontraumatic Intracranial Hemorrhage Using Blood Urea Nitrogen-to-Creatinine Ratio on Admission: A Retrospective Cohort Study Based on Data from the Medical Information Mart for Intensive Care-IV Database. Front. Neurol. 2024, 14, 1267815. [Google Scholar] [CrossRef]
- Huang, Y.; Li, Z.; Yin, X. Triglyceride-Glucose Index: A Novel Evaluation Tool for All-Cause Mortality in Critically Ill Hemorrhagic Stroke Patients-a Retrospective Analysis of the MIMIC-IV Database. Cardiovasc. Diabetol. 2024, 23, 100. [Google Scholar] [CrossRef]
- Liu, J.; Wang, J. Association between Hemoglobin-to-Red Blood Cell Distribution Width Ratio and Hospital Mortality in Patients with Non-Traumatic Subarachnoid Hemorrhage. Front. Neurol. 2023, 14, 1180912. [Google Scholar] [CrossRef]
- Shahbaz, H.; Rout, P.; Gupta, M. Creatinine Clearance. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Gunst, J.; Kashani, K.B.; Hermans, G. The Urea-Creatinine Ratio as a Novel Biomarker of Critical Illness-Associated Catabolism. Intensive Care Med. 2019, 45, 1813–1815. [Google Scholar] [CrossRef]
- Haines, R.W.; Zolfaghari, P.; Wan, Y.; Pearse, R.M.; Puthucheary, Z.; Prowle, J.R. Elevated Urea-to-Creatinine Ratio Provides a Biochemical Signature of Muscle Catabolism and Persistent Critical Illness after Major Trauma. Intensive Care Med. 2019, 45, 1718–1731. [Google Scholar] [CrossRef]
- Zhang, Z.; Ho, K.M.; Gu, H.; Hong, Y.; Yu, Y. Defining Persistent Critical Illness Based on Growth Trajectories in Patients with Sepsis. Crit. Care 2020, 24, 57. [Google Scholar] [CrossRef]
- Puthucheary, Z.A.; Rawal, J.; McPhail, M.; Connolly, B.; Ratnayake, G.; Chan, P.; Hopkinson, N.S.; Phadke, R.; Dew, T.; Sidhu, P.S.; et al. Acute Skeletal Muscle Wasting in Critical Illness. JAMA 2013, 310, 1591–1600. [Google Scholar] [CrossRef]
- Paulus, M.C.; Melchers, M.; van Es, A.; Kouw, I.W.K.; van Zanten, A.R.H. The Urea-to-Creatinine Ratio as an Emerging Biomarker in Critical Care: A Scoping Review and Meta-Analysis. Crit. Care 2025, 29, 175. [Google Scholar] [CrossRef]
- Murata, A.; Kasai, T.; Matsue, Y.; Matsumoto, H.; Yatsu, S.; Kato, T.; Suda, S.; Hiki, M.; Takagi, A.; Daida, H. Relationship between Blood Urea Nitrogen-to-Creatinine Ratio at Hospital Admission and Long-Term Mortality in Patients with Acute Decompensated Heart Failure. Heart Vessel. 2018, 33, 877–885. [Google Scholar] [CrossRef] [PubMed]
- Statlender, L.; Shochat, T.; Robinson, E.; Fishman, G.; Hellerman-Itzhaki, M.; Bendavid, I.; Singer, P.; Kagan, I. Urea to Creatinine Ratio as a Predictor of Persistent Critical Illness. J. Crit. Care 2024, 83, 154834. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.E.W.; Bulgarelli, L.; Shen, L.; Gayles, A.; Shammout, A.; Horng, S.; Pollard, T.J.; Hao, S.; Moody, B.; Gow, B.; et al. MIMIC-IV, a Freely Accessible Electronic Health Record Dataset. Sci. Data 2023, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Gunst, J.; Vanhorebeek, I.; Casaer, M.P.; Hermans, G.; Wouters, P.J.; Dubois, J.; Claes, K.; Schetz, M.; Van den Berghe, G. Impact of Early Parenteral Nutrition on Metabolism and Kidney Injury. J. Am. Soc. Nephrol. 2013, 24, 995–1005. [Google Scholar] [CrossRef]
- Gunst, J.; Vanhorebeek, I.; Thiessen, S.E.; Van den Berghe, G. Amino Acid Supplements in Critically Ill Patients. Pharmacol. Res. 2018, 130, 127–131. [Google Scholar] [CrossRef]
- Luo, H.; Yang, X.; Chen, K.; Lan, S.; Liao, G.; Xu, J. Blood Creatinine and Urea Nitrogen at ICU Admission and the Risk of In-Hospital Death and 1-Year Mortality in Patients with Intracranial Hemorrhage. Front. Cardiovasc. Med. 2022, 9, 967614. [Google Scholar] [CrossRef]
- Prowle, J.R.; Kolic, I.; Purdell-Lewis, J.; Taylor, R.; Pearse, R.M.; Kirwan, C.J. Serum Creatinine Changes Associated with Critical Illness and Detection of Persistent Renal Dysfunction after AKI. Clin. J. Am. Soc. Nephrol. 2014, 9, 1015. [Google Scholar] [CrossRef]
- Van den Berghe, G. On the Neuroendocrinopathy of Critical Illness. Perspectives for Feeding and Novel Treatments. Am. J. Respir. Crit. Care Med 2016, 194, 1337–1348. [Google Scholar] [CrossRef]
- Nusshag, C.; Weigand, M.A.; Zeier, M.; Morath, C.; Brenner, T. Issues of Acute Kidney Injury Staging and Management in Sepsis and Critical Illness: A Narrative Review. Int. J. Mol. Sci. 2017, 18, 1387. [Google Scholar] [CrossRef]
- Conte, G.; Dal Canton, A.; Terribile, M.; Cianciaruso, B.; Di Minno, G.; Pannain, M.; Russo, D.; Andreucci, V.E. Renal Handling of Urea in Subjects with Persistent Azotemia and Normal Renal Function. Kidney Int. 1987, 32, 721–727. [Google Scholar] [CrossRef]
- Dossetor, J.B. Creatininemia versus Uremia. The Relative Significance of Blood Urea Nitrogen and Serum Creatinine Concentrations in Azotemia. Ann. Intern. Med. 1966, 65, 1287–1299. [Google Scholar] [CrossRef]
- Keller, W.J.; Mullaj, E. Antidiuretic Hormone Release Associated with Increased Intracranial Pressure Independent of Plasma Osmolality. Brain Behav. 2018, 8, e01005. [Google Scholar] [CrossRef] [PubMed]
- Baum, N.; Dichoso, C.C.; Carlton, C.E. Blood Urea Nitrogen and Serum Creatinine: Physiology and Interpretations. Urology 1975, 5, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Beier, K.; Eppanapally, S.; Bazick, H.S.; Chang, D.; Mahadevappa, K.; Gibbons, F.K.; Christopher, K.B. Elevation of Blood Urea Nitrogen Is Predictive of Long-Term Mortality in Critically Ill Patients Independent of “Normal” Creatinine. Crit. Care Med. 2011, 39, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Lin, S.; Xie, Y.; Mo, S.; Huang, Q.; Ge, H.; Shi, Z.; Li, S.; Zhou, D. Association between BUN/Creatinine Ratio and the Risk of in-Hospital Mortality in Patients with Trauma-Related Acute Respiratory Distress Syndrome: A Single-Centre Retrospective Cohort from the MIMIC Database. BMJ Open 2023, 13, e069345. [Google Scholar] [CrossRef]
- Inaguma, D.; Koide, S.; Ito, E.; Takahashi, K.; Hayashi, H.; Hasegawa, M.; Yuzawa, Y.; AICOPP Group. Ratio of Blood Urea Nitrogen to Serum Creatinine at Initiation of Dialysis Is Associated with Mortality: A Multicenter Prospective Cohort Study. Clin. Exp. Nephrol. 2018, 22, 353–364. [Google Scholar] [CrossRef]
- Janatpour, Z.C.; Korotcov, A.; Bosomtwi, A.; Dardzinski, B.J.; Symes, A.J. Subcutaneous Administration of Angiotensin-(1-7) Improves Recovery after Traumatic Brain Injury in Mice. J. Neurotrauma. 2019, 36, 3115–3131. [Google Scholar] [CrossRef]
- van Veldhuisen, D.J.; Ruilope, L.M.; Maisel, A.S.; Damman, K. Biomarkers of Renal Injury and Function: Diagnostic, Prognostic and Therapeutic Implications in Heart Failure. Eur. Heart J. 2015, 37, 2577–2585. [Google Scholar] [CrossRef]
- Schrier, R.W. Blood Urea Nitrogen and Serum Creatinine: Not Married in Heart Failure. Circ. Heart Fail. 2008, 1, 2–5. [Google Scholar] [CrossRef]
- Kazory, A. Emergence of Blood Urea Nitrogen as a Biomarker of Neurohormonal Activation in Heart Failure. Am. J. Cardiol. 2010, 106, 694–700. [Google Scholar] [CrossRef]
- Casaer, M.P.; Mesotten, D.; Schetz, M.R.C. Bench-to-Bedside Review: Metabolism and Nutrition. Crit. Care 2008, 12, 222. [Google Scholar] [CrossRef]
- Oshima, T.; Deutz, N.E.; Doig, G.; Wischmeyer, P.E.; Pichard, C. Protein-Energy Nutrition in the ICU Is the Power Couple: A Hypothesis Forming Analysis. Clin. Nutr. 2016, 35, 968–974. [Google Scholar] [CrossRef]
- Smilde, T.D.J.; van Veldhuisen, D.J.; Navis, G.; Voors, A.A.; Hillege, H.L. Drawbacks and Prognostic Value of Formulas Estimating Renal Function in Patients with Chronic Heart Failure and Systolic Dysfunction. Circulation 2006, 114, 1572–1580. [Google Scholar] [CrossRef]
- Bonilla, D.A.; Kreider, R.B.; Stout, J.R.; Forero, D.A.; Kerksick, C.M.; Roberts, M.D.; Rawson, E.S. Metabolic Basis of Creatine in Health and Disease: A Bioinformatics-Assisted Review. Nutrients 2021, 13, 1238. [Google Scholar] [CrossRef]

| Variables | Overall (n = 2559) | G1 (n = 655) | G2 (n = 1270) | G3 (n = 634) | a p |
|---|---|---|---|---|---|
| Age | 65.36 ± 15.61 | 65.6 ± 15.51 | 66.27 ± 15.54 | 63.3 ± 15.68 | <0.01 |
| Gender (n, %) | |||||
| Female | 1216 (47.52) | 300 (45.80) | 601 (47.32) | 315 (49.68) | 0.37 |
| Male | 1343 (52.48) | 355 (54.20) | 669 (52.68) | 319 (50.32) | |
| Race (n, %) | |||||
| White | 249 (9.73) | 57 (8.70) | 128 (10.08) | 64 (10.09) | 0.05 |
| Black | 100 (3.91) | 31 (4.73) | 46 (3.62) | 23 (3.63) | |
| Mexican American | 755 (29.50) | 170 (25.95) | 409 (32.20) | 176 (27.76) | |
| Other | 1455 (56.86) | 397 (60.61) | 687 (54.09) | 371 (58.52) | |
| Marital status (n, %) | |||||
| Divorced | 172 (6.72) | 39 (5.95) | 85 (6.69) | 48 (7.57) | 0.15 |
| Married | 1504 (58.77) | 378 (57.71) | 763 (60.08) | 363 (57.26) | |
| Single | 639 (24.97) | 174 (26.56) | 291 (22.91) | 174 (27.44) | |
| Widowed | 244 (9.53) | 64 (9.77) | 131 (10.31) | 49 (7.73) | |
| Vital signs | |||||
| Heart rate (beats/min) | 82.88 ± 17.54 | 83.05 ± 16.96 | 82.6 ± 17.49 | 83.25 ± 18.23 | 0.71 |
| SBP | 133.26 ± 22.53 | 133.06 ± 20.77 | 134.9 ± 23.16 | 130.17 ± 22.71 | <0.01 |
| DBP | 74.93 ± 17.9 | 74.39 ± 16.99 | 75.65 ± 18.76 | 74.03 ± 16.98 | 0.12 |
| MBP | 90.04 ± 17.72 | 89.96 ± 17.23 | 90.78 ± 18.39 | 88.61 ± 16.78 | 0.04 |
| Respiratory rate (times/min) | 18.65 ± 5.47 | 18.73 ± 5.68 | 18.62 ± 5.4 | 18.62 ± 5.4 | 0.91 |
| SpO2 | 97.4 ± 3.65 | 97.24 ± 2.77 | 97.54 ± 4.24 | 97.29 ± 3.12 | 0.15 |
| Temperature (°C) | 98.34 ± 1.8 | 98.43 ± 1 | 98.35 ± 1.63 | 98.25 ± 2.59 | 0.23 |
| Severity | |||||
| SOFA | 3.52 ± 2.81 | 3.2 ± 2.55 | 3.61 ± 2.69 | 3.68 ± 3.25 | <0.01 |
| APS-III | 38.22 ± 17.8 | 35.73 ± 16.29 | 38.65 ± 17.59 | 39.95 ± 19.4 | <0.01 |
| SIRS | 2.39 ± 0.98 | 2.33 ± 0.99 | 2.47 ± 0.97 | 2.3 ± 0.98 | <0.01 |
| SAPS-II | 32.95 ± 12.05 | 31.93 ± 11.81 | 33.83 ± 11.73 | 32.25 ± 12.81 | <0.01 |
| OASIS | 31.18 ± 7.93 | 29.97 ± 7.81 | 32.23 ± 7.7 | 30.32 ± 8.22 | <0.01 |
| GCS | 12.65 ± 3.06 | 12.98 ± 2.75 | 12.39 ± 3.25 | 12.85 ± 2.94 | <0.01 |
| Laboratory parameters | |||||
| Hb (g/L) | 11.92 ± 1.99 | 12.06 ± 2.02 | 11.97 ± 1.93 | 11.66 ± 2.05 | <0.01 |
| RBC (109/L) | 3.97 ± 0.68 | 4.04 ± 0.69 | 3.99 ± 0.66 | 3.88 ± 0.71 | <0.01 |
| WBC (109/L) | 11.8 ± 8.37 | 12.23 ± 11.14 | 11.89 ± 8.19 | 11.17 ± 4.45 | 0.06 |
| PLT (109/L) | 218.39 ± 82.88 | 221.64 ± 85.05 | 217.66 ± 81.46 | 216.48 ± 83.47 | 0.49 |
| APTT (s) | 31.48 ± 11.98 | 31.77 ± 13.45 | 30.88 ± 10.68 | 32.39 ± 12.75 | 0.03 |
| PT (s) | 1.22 ± 0.3 | 1.23 ± 0.3 | 1.21 ± 0.26 | 1.23 ± 0.35 | 0.15 |
| Serum creatinine | 1.1 ± 1.14 | 1.03 ± 0.82 | 1.09 ± 1.16 | 1.21 ± 1.36 | 0.01 |
| BUN | 19.18 ± 14.73 | 18.8 ± 14.1 | 17.46 ± 12.09 | 23.01 ± 18.91 | <0.01 |
| BUNCR | 18.92 ± 7.95 | 18.94 ± 7.52 | 17.56 ± 6.98 | 21.6 ± 9.4 | <0.01 |
| Comorbidities (n, %) | |||||
| CCI | 5.45 ± 2.86 | 5.36 ± 2.89 | 5.66 ± 2.81 | 5.11 ± 2.88 | <0.01 |
| Sepsis | 173 (6.76) | 39 (5.95) | 73 (5.75) | 61 (9.62) | <0.01 |
| PVD | 26 (1.02) | 4 (0.61) | 14 (1.10) | 8 (1.26) | 0.46 |
| IVH | 350 (13.68) | 86 (13.13) | 193 (15.20) | 71 (11.20) | 0.05 |
| Hypertension | 1480 (57.84) | 387 (59.08) | 770 (60.63) | 323 (50.95) | <0.01 |
| Liver cirrhosis | 87 (3.40) | 31 (4.73) | 28 (2.20) | 28 (4.42) | <0.01 |
| CKD | 283 (11.06) | 62 (9.47) | 130 (10.24) | 91 (14.35) | 0.01 |
| Malignant tumors | 335 (13.09) | 95 (14.50) | 168 (13.23) | 72 (11.36) | 0.24 |
| T2DM | 567 (22.16) | 138 (21.07) | 298 (23.46) | 131 (20.66) | 0.28 |
| T1DM | 28 (1.09) | 9 (1.37) | 10 (0.79) | 9 (1.42) | 0.33 |
| Heart failure | 346 (13.52) | 88 (13.44) | 174 (13.70) | 84 (13.25) | 0.96 |
| CHD | 482 (18.84) | 129 (19.69) | 235 (18.50) | 118 (18.61) | 0.81 |
| COPD | 211 (8.25) | 51 (7.79) | 113 (8.90) | 47 (7.41) | 0.48 |
| Treatment (n, %) | |||||
| MT | 1981 (77.41) | 476 (72.67) | 1064 (83.78) | 441 (69.56) | <0.01 |
| Vasopressor | 205 (8.01) | 31 (4.73) | 123 (9.69) | 51 (8.04) | 0.10 |
| Outcomes (n, %) | |||||
| in-hospital ACM | 360 (14.07) | 85 (12.98) | 199 (15.67) | 76 (11.99) | 0.06 |
| ICU ACM | 260 (10.16) | 68 (10.38) | 132 (10.39) | 60 (9.46) | 0.80 |
| 28-day ACM | 435 (17.00) | 109 (16.64) | 243 (19.13) | 83 (13.09) | <0.01 |
| 90-day ACM | 574 (22.43) | 131 (20.00) | 320 (25.20) | 123 (19.40) | <0.01 |
| 1-year ACM | 946 (36.97) | 228 (34.81) | 505 (39.76) | 213 (33.60) | 0.01 |
| Categories | HR | 95% CI | p |
|---|---|---|---|
| 28-day ACM | |||
| Group 2 | Reference | - | - |
| Group 1 | 0.91 | (0.72, 1.14) | 0.421 |
| Group 3 | 0.73 | (0.57, 0.94) | 0.014 |
| 90-day ACM | |||
| Group 2 | Reference | - | - |
| Group 1 | 0.80 | (0.65, 0.99) | 0.037 |
| Group 3 | 0.80 | (0.64, 0.99) | 0.038 |
| 1-year ACM | |||
| Group 2 | Reference | - | - |
| Group 1 | 0.83 | (0.71, 0.97) | 0.021 |
| Group 3 | 0.84 | (0.72, 0.99) | 0.037 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, X.; Luo, H.; Deng, H.; Wu, Y.; Wang, M.; Xiao, L.; Shi, X.; Pan, W.; Gao, Y.; Wang, W. Association Between the Blood Urea Nitrogen-to-Creatinine Ratio Trajectories and Clinical Outcomes in Critically Ill Hemorrhagic Stroke Patients: Insights from MIMIC-IV Database. J. Clin. Med. 2025, 14, 8141. https://doi.org/10.3390/jcm14228141
Huang X, Luo H, Deng H, Wu Y, Wang M, Xiao L, Shi X, Pan W, Gao Y, Wang W. Association Between the Blood Urea Nitrogen-to-Creatinine Ratio Trajectories and Clinical Outcomes in Critically Ill Hemorrhagic Stroke Patients: Insights from MIMIC-IV Database. Journal of Clinical Medicine. 2025; 14(22):8141. https://doi.org/10.3390/jcm14228141
Chicago/Turabian StyleHuang, Xinyuejia, Huixuan Luo, Hao Deng, Yang Wu, Mengqi Wang, Linglong Xiao, Xiaoman Shi, Wei Pan, Yuan Gao, and Wei Wang. 2025. "Association Between the Blood Urea Nitrogen-to-Creatinine Ratio Trajectories and Clinical Outcomes in Critically Ill Hemorrhagic Stroke Patients: Insights from MIMIC-IV Database" Journal of Clinical Medicine 14, no. 22: 8141. https://doi.org/10.3390/jcm14228141
APA StyleHuang, X., Luo, H., Deng, H., Wu, Y., Wang, M., Xiao, L., Shi, X., Pan, W., Gao, Y., & Wang, W. (2025). Association Between the Blood Urea Nitrogen-to-Creatinine Ratio Trajectories and Clinical Outcomes in Critically Ill Hemorrhagic Stroke Patients: Insights from MIMIC-IV Database. Journal of Clinical Medicine, 14(22), 8141. https://doi.org/10.3390/jcm14228141







