Timing Matters? Impact of Early Sperm Processing on Motile Sperm Recovery, Fertilization, Blastocyst Rate, and Pregnancy Outcomes in IUI and IVF †
Abstract
1. Introduction
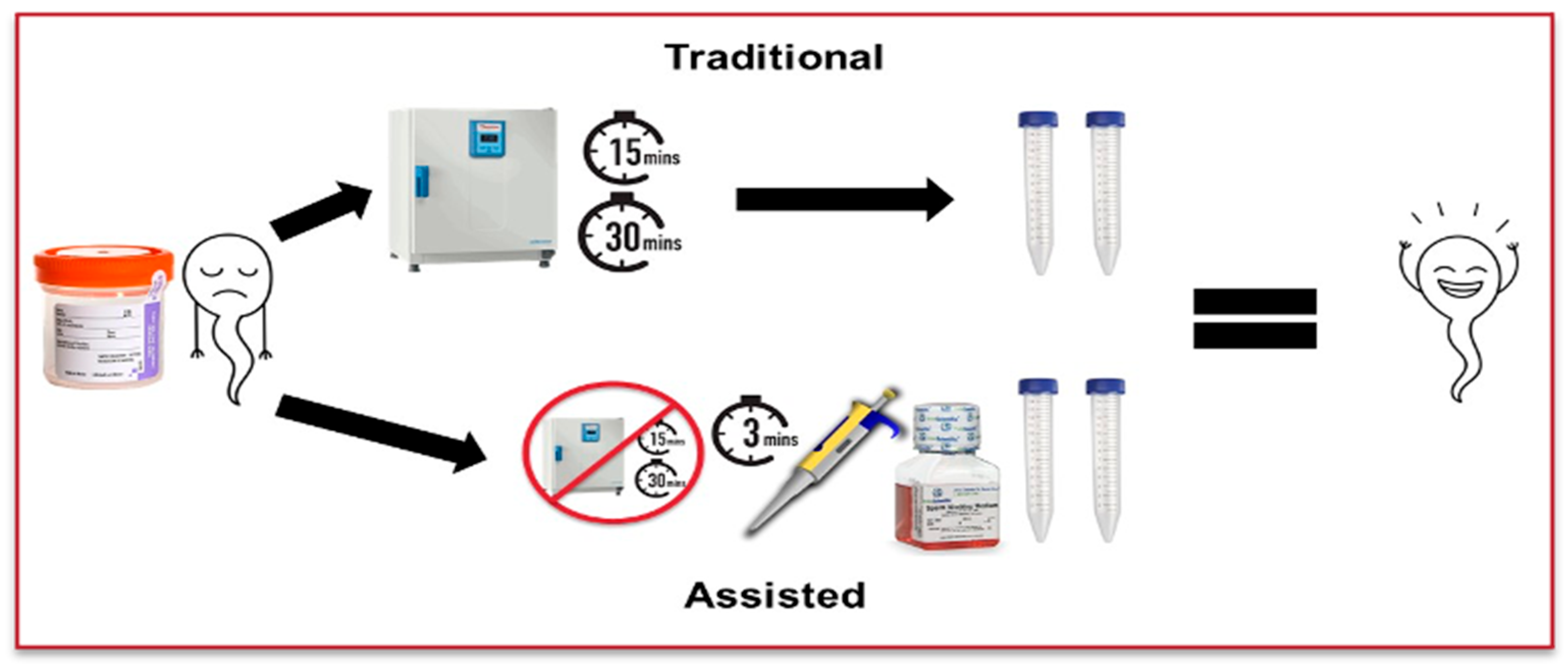
2. Materials and Methods
2.1. Pilot Study
2.2. Retrospective Study
3. Results
3.1. Pilot Study: Assessment of Motile Sperm Recovery
3.2. Retrospective Study: Comparison of Fertilization and Blastocyst Rates in IVF Cycles
3.3. Retrospective Study: Comparison of Pregnancy Outcomes in IVF and IUI Cycles
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sunderam, S.; Kissin, D.M.; Zhang, Y.; Folger, S.G.; Boulet, S.L.; Warner, L.; Callaghan, W.M.; Barfield, W.D. Assisted Reproductive Technology Surveillance—United States, 2016. MMWR Surveill. Summ. 2019, 68, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Dcunha, R.; Hussein, R.S.; Ananda, H.; Kumari, S.; Adiga, S.K.; Kannan, N.; Zhao, Y.; Kalthur, G. Current Insights and Latest Updates in Sperm Motility and Associated Applications in Assisted Reproduction. Reprod. Sci. 2022, 29, 7–25. [Google Scholar] [CrossRef] [PubMed]
- Fainberg, J.; Kashanian, J.A. Recent Advances in Understanding and Managing Male Infertility. F1000Research 2019, 8, F1000-aculty. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Singh, A.K. Trends of Male Factor Infertility, an Important Cause of Infertility: A Review of Literature. J. Hum. Reprod. Sci. 2015, 8, 191–196. [Google Scholar] [CrossRef]
- World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen, 6th ed.; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Liu, S.; Wu, G.; Wang, L.; Zhao, Y.; Lv, Y.; Dang, N.; Yao, Y. The Influence of Preincubation Time of Prepared Sperm before IVF on Fertilization, Embryo Developmental Competence and the Reproductive Outcomes. Ginekol. Pol. 2023, 94, 107–112. [Google Scholar] [CrossRef]
- Jeong, M.; Kim, S.K.; Kim, H.; Lee, J.R.; Jee, B.C.; Kim, S.H. Predictive Value of Sperm Motility before and after Preparation for the Pregnancy Outcomes of Intrauterine Insemination. Clin. Exp. Reprod. Med. 2021, 48, 255–261. [Google Scholar] [CrossRef]
- Zhou, J.; Chen, L.; Li, J.; Li, H.; Hong, Z.; Xie, M.; Chen, S.; Yao, B. The Semen pH Affects Sperm Motility and Capacitation. PLoS ONE 2015, 10, e0132974. [Google Scholar] [CrossRef]
- Raad, G.; Bakos, H.W.; Bazzi, M.; Mourad, Y.; Fakih, F.; Shayya, S.; Mchantaf, L.; Fakih, C. Differential Impact of Four Sperm Preparation Techniques on Sperm Motility, Morphology, DNA Fragmentation, Acrosome Status, Oxidative Stress, and Mitochondrial Activity: A Prospective Study. Andrology 2021, 9, 1549–1559. [Google Scholar] [CrossRef]
- Hoa, N.T.; Son, N.K.; Hoa, T.P.; Giang, M.T.; Dung, L.N.; Duc, N.M.; Ha, N.M. The Effectiveness of Sperm Preparation Using Density Mini-Gradient and Single-Layer Centrifugation for Oligospermia Samples. Acta Inform. Med. 2022, 30, 100–104. [Google Scholar] [CrossRef]
- Nagy, Z.P.; Varghese, A.C.; Agarwal, A. (Eds.) Clinical Embryology: A Practical Guide; Springer: London, UK, 2013; pp. 13–24. [Google Scholar]
- Boomsma, C.M.; Cohlen, B.J.; Farquhar, C. Semen Preparation Techniques for Intrauterine Insemination. Cochrane Database Syst. Rev. 2019, 10, CD004507. [Google Scholar] [CrossRef]
- Feyzioglu, B.S.; Avul, Z. Effects of Sperm Separation Methods before Intrauterine Insemination on Pregnancy Outcomes and Live Birth Rates: Differences between the Swim-Up and Microfluidic Chip Techniques. Medicine 2023, 102, e36042. [Google Scholar] [CrossRef]
- Gualtieri, R.; Kalthur, G.; Barbato, V.; Longobardi, S.; Di Rella, F.; Adiga, S.K.; Talevi, R. Sperm Oxidative Stress during In Vitro Manipulation and Its Effects on Sperm Function and Embryo Development. Antioxidants 2021, 10, 1025. [Google Scholar] [CrossRef]
- Pujol, A.; García-Peiró, A.; Ribas-Maynou, J.; Lafuente, R.; Mataró, D.; Vassena, R. A Microfluidic Sperm-Sorting Device Reduces the Proportion of Sperm with Double-Stranded DNA Fragmentation. Zygote 2022, 30, 200–205. [Google Scholar] [CrossRef]
- Adolfsson, E.; Ingberg, J.; Igersten, E.; Bohlin, T. Clinical Validation and Experiences of the Microfluidics Sperm Selection Device ZyMōt™ for Standard IVF. JBRA Assist Reprod. 2025, 29, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Gavriil, E.; Desli, A.; Geladaris, V.; Kachpani, E.; Neofytou, E.; Tatsi, P.; Dovas, D. Embryology Outcomes of a Device-Based Sperm Separation Technique Compared to Density Gradient Centrifugation Using Thawed Spermatozoa-a Sibling Donor Oocyte Study. J. Assist. Reprod. Genet. 2025, 42, 97–105. [Google Scholar] [CrossRef]
- Hsu, C.T.; Lee, C.I.; Lin, F.S.; Wang, F.Z.; Chang, H.C.; Wang, T.E.; Huang, C.C.; Tsao, H.M.; Lee, M.S.; Agarwal, A. Live motile sperm sorting device for enhanced sperm-fertilization competency: Comparative analysis with density-gradient centrifugation and microfluidic sperm sorting. J. Assist. Reprod. Genet. 2023, 40, 1855–1864. [Google Scholar] [CrossRef]
- Balasuriya, A.; Serhal, P.; Doshi, A.; Harper, J.C. Processes Involved in Assisted Reproduction Technologies Significantly Increase Sperm DNA Fragmentation and Phosphatidylserine Translocation. Andrologia 2014, 46, 86–97. [Google Scholar] [CrossRef]
- Haering, C.; Manvelyan, E.; Coyne, K.; Hyams, L.A.; Hamrick, J.; Findley, J.; Weinerman, R.; Flyckt, R.; Kim, S.T. The Pre-Catching Sperm Technique Increases the Efficiency of the Intracytoplasmic Sperm Injection Method by Improving Fertilization and Blastocyst Formation Rates. J. Clin. Med. 2025, 14, 4872. [Google Scholar] [CrossRef] [PubMed]
- Fasano, C.; D’Andolfi, G.; Di Matteo, L.; Forte, C.; Dale, B.; Tosti, E. Comparison of Sperm Preparation Methods to Improve the Recovery of Mature Spermatozoa in Sub-Fertile Males. Zygote 2022, 30, 664–673. [Google Scholar] [CrossRef]
- Volpes, A.; Sammartano, F.; Rizzari, S.; Gullo, S.; Marino, A.; Allegra, A. The Pellet Swim-Up Is the Best Technique for Sperm Preparation during In Vitro Fertilization Procedures. J. Assist. Reprod. Genet. 2016, 33, 765–770. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.T.; Sofaly, K.; Mason, I.; Weinerman, R.; Flyckt, R. Timing is Critical: Post-Collection Sperm DNA Integrity and Motility. N. Am. Proc. Gynecol. Obstet. Suppl. 2025. [Google Scholar] [CrossRef]
| Assisted Liquefaction (n = 20) | Average of Difference | Range of Difference | p Value |
|---|---|---|---|
| Total Motility | 4% | −1 to 32% | p = 0.252 |
| Progressive Motility | 4% | −1 to 34% | p = 0.227 |
| Total Motile Sperm | 1.75 × 106 | −1.2 × 106 to 13.5 × 106 | p = 0.252 |
| AL | TL | p Value | |
|---|---|---|---|
| # of IVF cycles | 216 | 263 | |
| Average age of female (years) | 35.6 | 35.2 | p = 0.384 |
| Average * BMI of female (kg/m2) | 27.2 | 26.5 | p = 0.226 |
| Average ** AMH of female (ng/mL) | 3.75 | 3.03 | p = 0.055 |
| AL | TL | p Value | |
|---|---|---|---|
| # of IVF cycles | 216 | 263 | |
| Average number of oocytes | 13.9 | 12.7 | p = 0.079 |
| Fertilization Rate (%) | 80.0 | 81.9 | p = 0.297 |
| Abnormal Fertilization Rate (%) | 1.6 | 1.3 | p = 0.484 |
| Blastocyst Rate (%) | 48.2 | 48.1 | p = 0.595 |
| AL | TL | p Value | |
|---|---|---|---|
| # of Fresh ET | 44 | 76 | |
| Average age of female (years) | 34.6 | 35.5 | p = 0.287 |
| Average endometrial thickness (mm) | 9.5 | 10.2 | p = 0.091 |
| Positive Pregnancy Rate (%) | 70.5 | 75.0 | p = 0.667 |
| Clinical Pregnancy Rate (%) | 65.9 | 68.4 | p = 0.841 |
| Live Birth Rate (%) | 52.3 | 51.3 | p = 0.831 |
| AL | TL | p Value | |
|---|---|---|---|
| # of IUI cycles | 512 | 560 | |
| Average age of female (years) | 34.7 | 34.8 | p = 0.886 |
| Positive Pregnancy Rate (%) | 14.5 | 13.6 | p = 0.669 |
| Clinical Pregnancy Rate (%) | 11.9 | 12.9 | p = 0.841 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loo, K.; Mason, I.; Chung, R.; Sechler, S.; Coyne, K.; Findley, J.; Weinerman, R.; Flyckt, R.; Kim, S.T. Timing Matters? Impact of Early Sperm Processing on Motile Sperm Recovery, Fertilization, Blastocyst Rate, and Pregnancy Outcomes in IUI and IVF. J. Clin. Med. 2025, 14, 8094. https://doi.org/10.3390/jcm14228094
Loo K, Mason I, Chung R, Sechler S, Coyne K, Findley J, Weinerman R, Flyckt R, Kim ST. Timing Matters? Impact of Early Sperm Processing on Motile Sperm Recovery, Fertilization, Blastocyst Rate, and Pregnancy Outcomes in IUI and IVF. Journal of Clinical Medicine. 2025; 14(22):8094. https://doi.org/10.3390/jcm14228094
Chicago/Turabian StyleLoo, Kiana, Isabelle Mason, Rebecca Chung, Samantha Sechler, Kathryn Coyne, Joseph Findley, Rachel Weinerman, Rebecca Flyckt, and Sung Tae Kim. 2025. "Timing Matters? Impact of Early Sperm Processing on Motile Sperm Recovery, Fertilization, Blastocyst Rate, and Pregnancy Outcomes in IUI and IVF" Journal of Clinical Medicine 14, no. 22: 8094. https://doi.org/10.3390/jcm14228094
APA StyleLoo, K., Mason, I., Chung, R., Sechler, S., Coyne, K., Findley, J., Weinerman, R., Flyckt, R., & Kim, S. T. (2025). Timing Matters? Impact of Early Sperm Processing on Motile Sperm Recovery, Fertilization, Blastocyst Rate, and Pregnancy Outcomes in IUI and IVF. Journal of Clinical Medicine, 14(22), 8094. https://doi.org/10.3390/jcm14228094








