3D-Printed Arch Supports Combined with Toe Spreaders Modulate Phase-Specific Ankle Alignment and Muscle Activity in Young Adults with Functional Flat Foot
Abstract
1. Introduction
2. Materials and Methods
2.1. Subject Information
2.2. Identification of Functional Flat Foot
2.3. 3D-Printed Arch Support Insoles and Toe Spreaders
2.4. Experimental Procedures
2.5. Outcome Measurement
2.5.1. Gait Pattern Analysis
2.5.2. Center of Force Analysis
2.5.3. Ankle Alignment Analysis
2.5.4. Electromyographic Recording
2.6. Statistical Analyses
3. Results
3.1. Gait Pattern
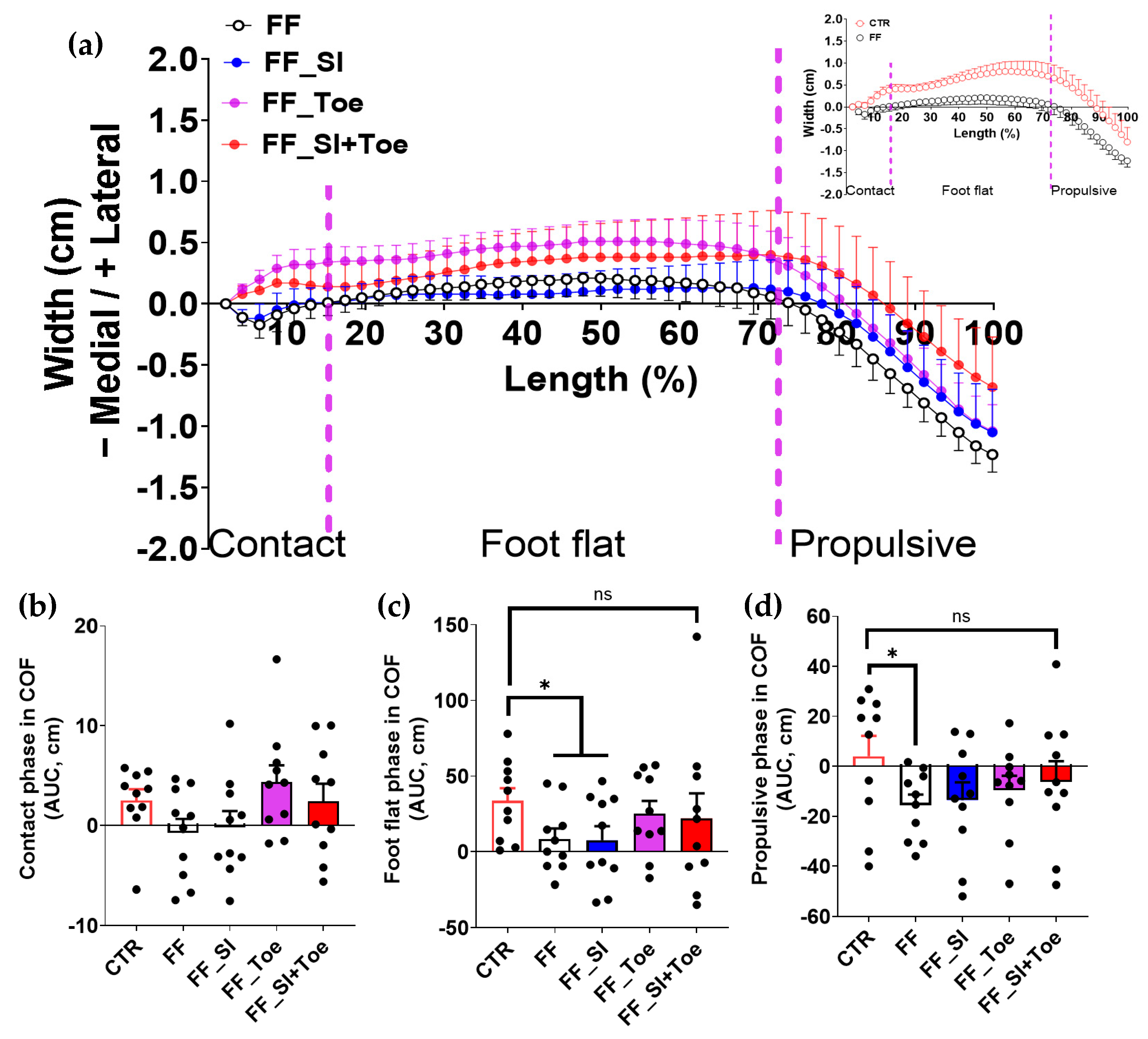
3.2. Center of Force
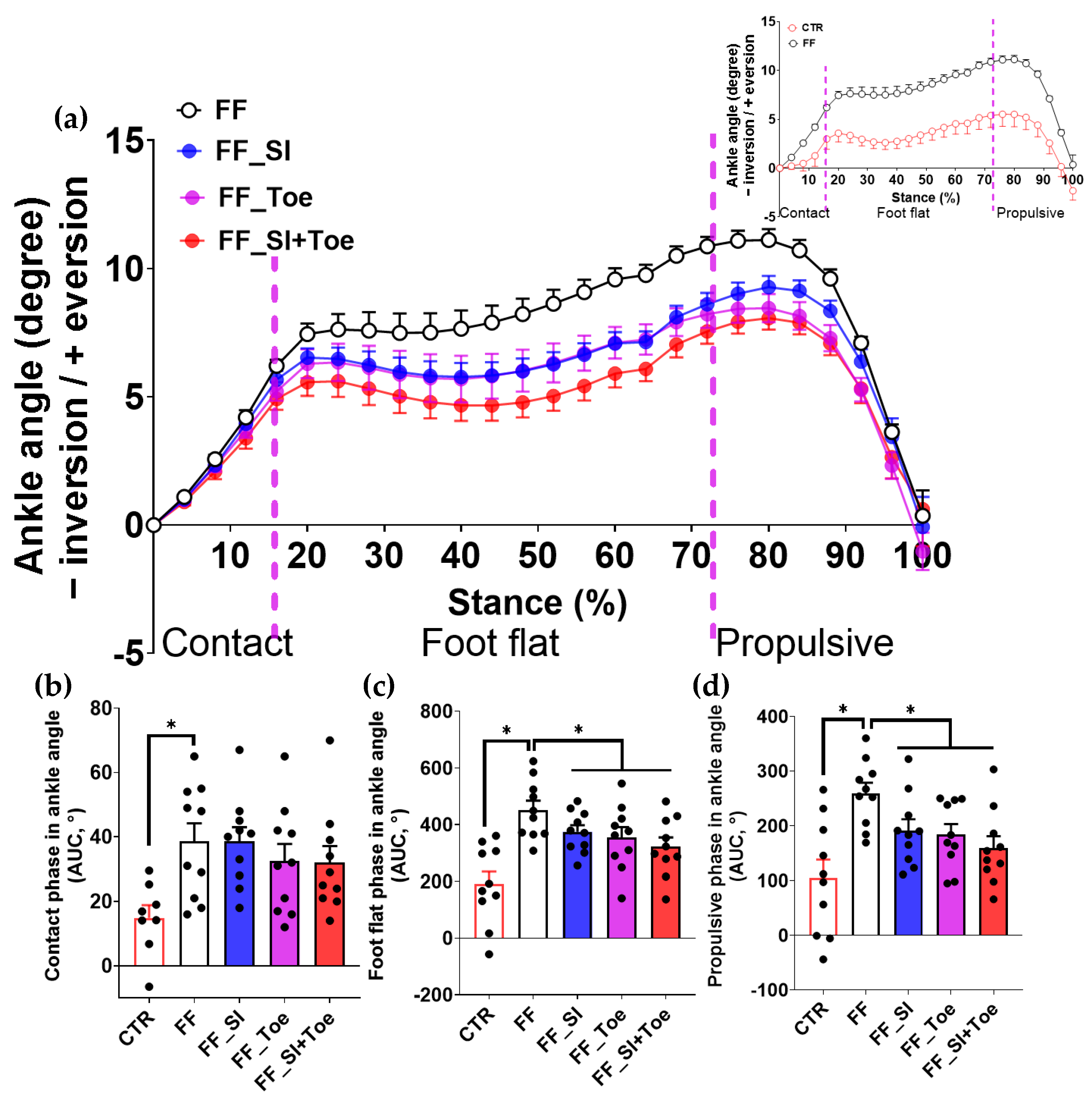
3.3. Ankle Alignment
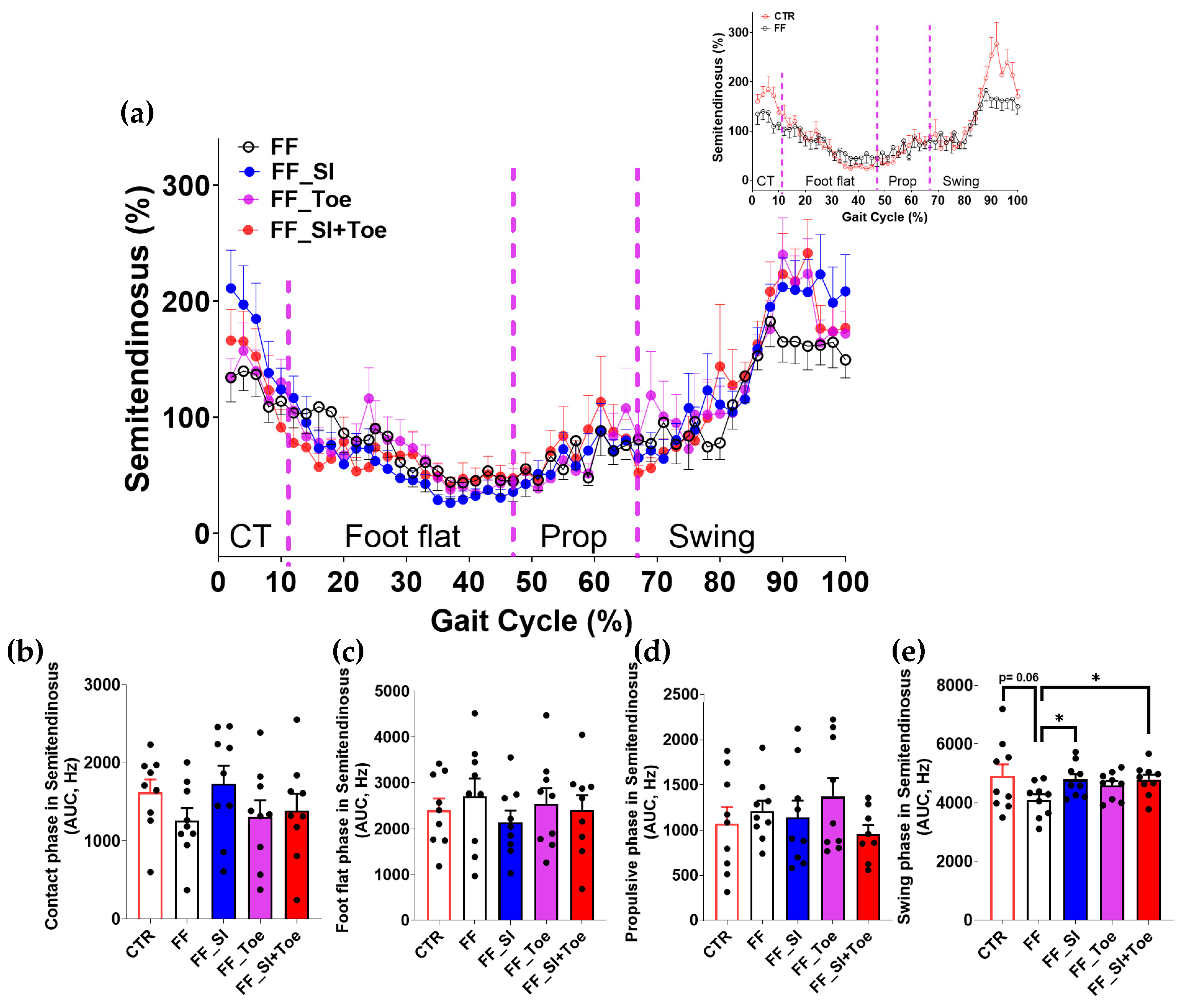
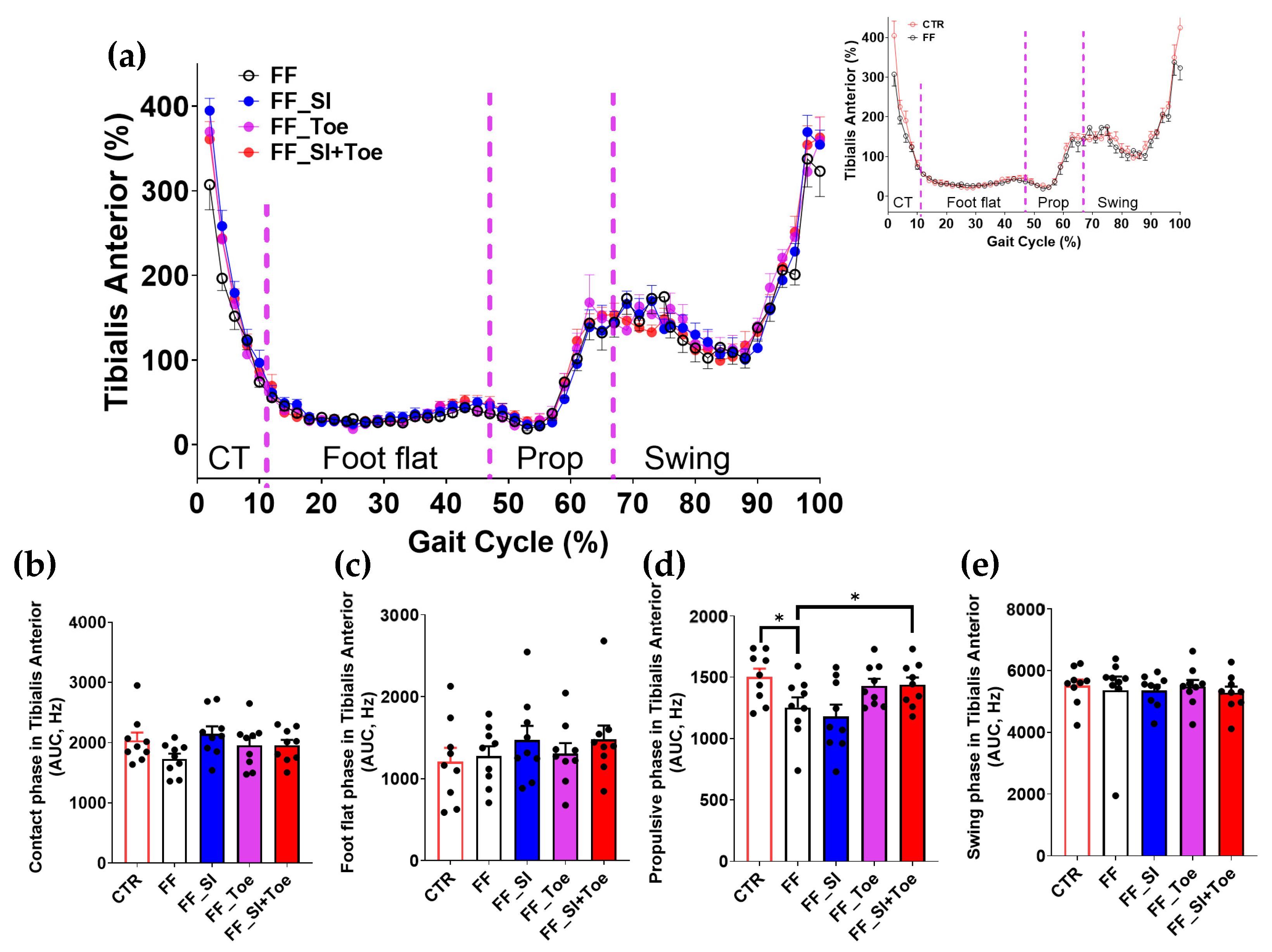
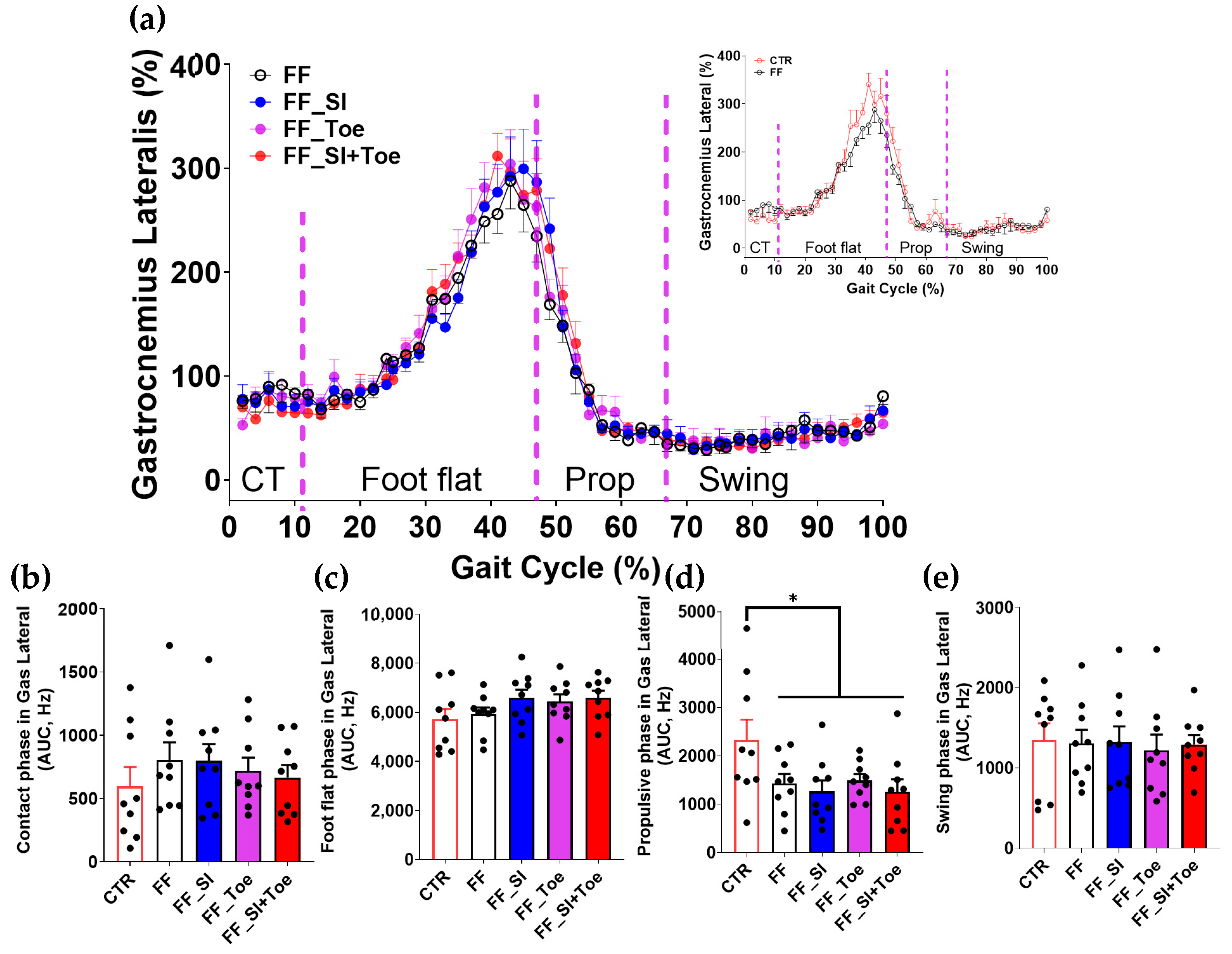
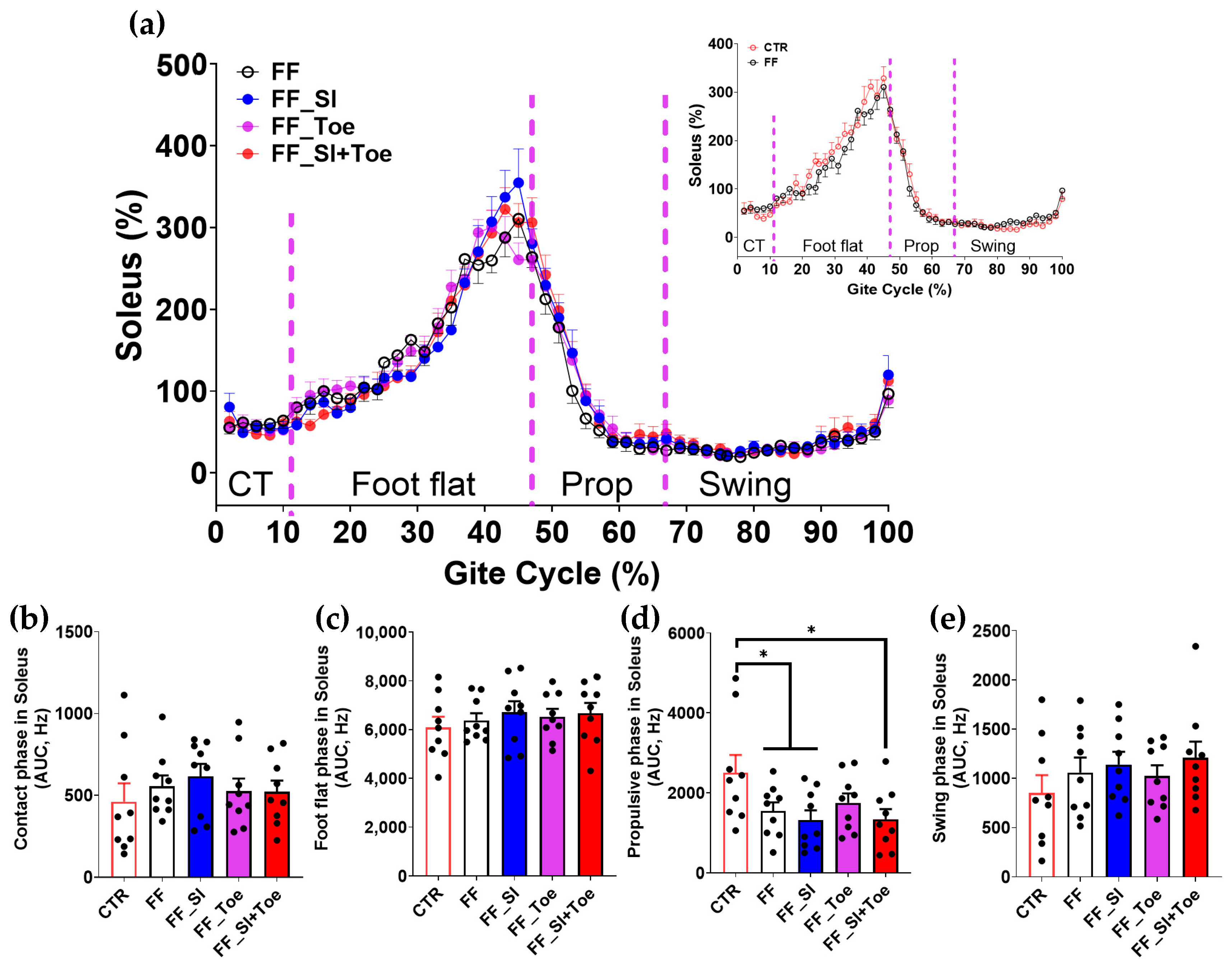
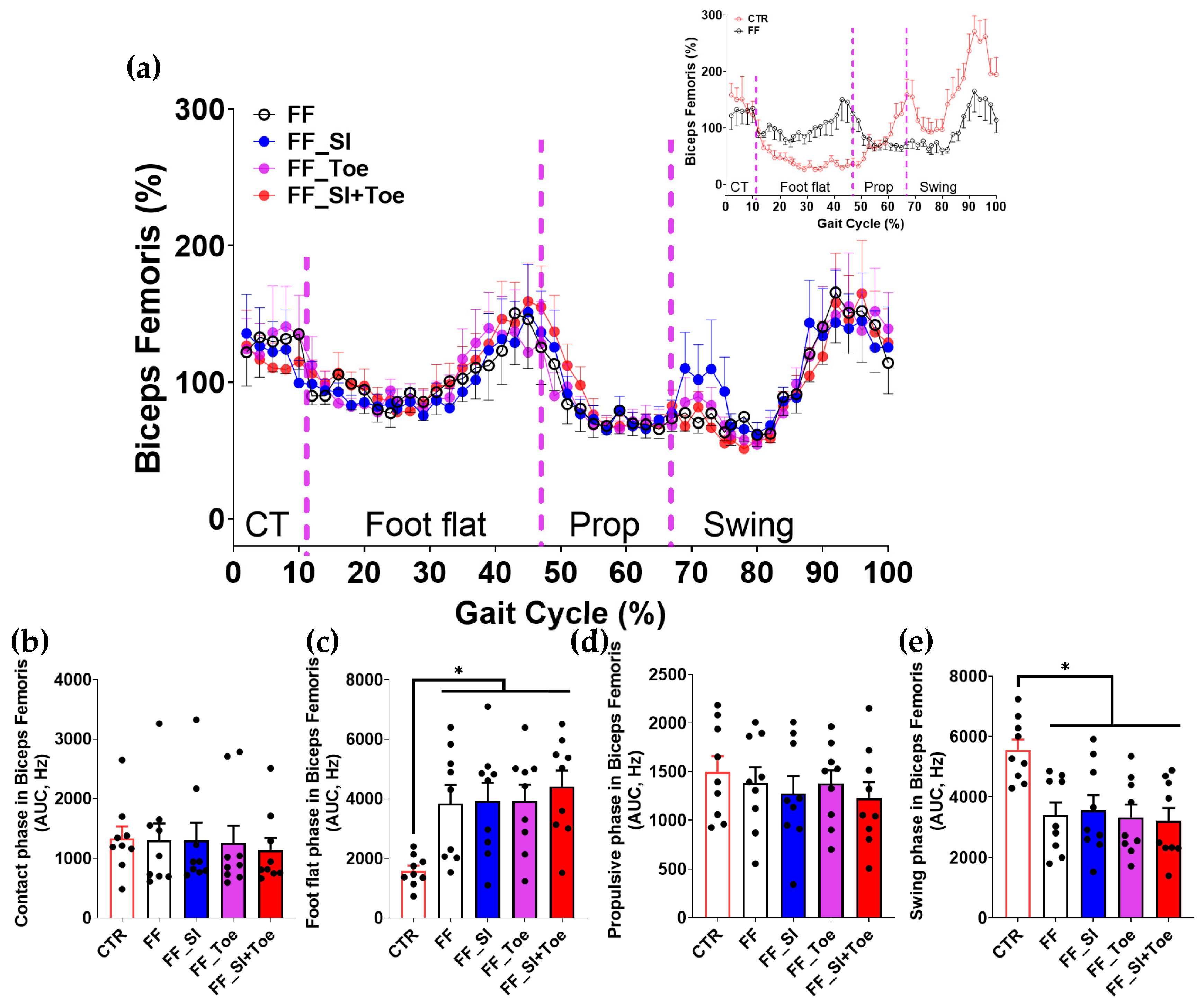
3.4. Muscle Activity
4. Discussion
4.1. Modification of COF Trajectory
4.2. Reduction in Ankle Eversion
4.3. Phase-Specific Changes in Muscle Activation
4.4. Residual and Unexpected Effects
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bednarczyk, E.; Sikora, S.; Kossobudzka-Górska, A.; Jankowski, K.; Hernandez-Rodriguez, Y. Understanding flat feet: An in-depth analysis of orthotic solutions. J. Orthop. Rep. 2024, 3, 100250. [Google Scholar] [CrossRef]
- Tareco, J.M.; Miller, N.H.; MacWilliams, B.A.; Michelson, J.D. Defining flatfoot. Foot Ankle Int. 1999, 20, 456–460. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-C.; Wang, L.-Y.; Wang, H.-C.; Chang, K.-L.; Leong, C.-P. The Relationship between the Flexible Flatfoot and Plantar Fasciitis: Ultrasonographic Evaluation. Chang Gung Med. J. 2004, 27, 443–451. [Google Scholar] [PubMed]
- Michelson, J.D.; Durant, D.M.; McFarland, E. The injury risk associated with pes planus in athletes. Foot Ankle Int. 2002, 23, 629–633. [Google Scholar] [CrossRef] [PubMed]
- Kirmizi, M.; Sengul, Y.S.; Angin, S. The effects of calf muscles fatigue on dynamic plantar pressure distribution in normal foot posture and flexible flatfoot: A case-control study. J. Back Musculoskelet. Rehabil. 2022, 35, 649–657. [Google Scholar] [CrossRef]
- Murley, G.S.; Menz, H.B.; Landorf, K.B. Foot posture influences the electromyographic activity of selected lower limb muscles during gait. J. Foot Ankle Res. 2009, 2, 35. [Google Scholar] [CrossRef]
- Yates, B.; White, S. The incidence and risk factors in the development of medial tibial stress syndrome among naval recruits. Am. J. Sports Med. 2004, 32, 772–780. [Google Scholar] [CrossRef]
- Hunt, A.E.; Smith, R.M. Mechanics and control of the flat versus normal foot during the stance phase of walking. Clin. Biomech. 2004, 19, 391–397. [Google Scholar] [CrossRef]
- Simkin, A.; Leichter, I.; Giladi, M.; Stein, M.; Milgrom, C. Combined effect of foot arch structure and an orthotic device on stress fractures. Foot Ankle 1989, 10, 25–29. [Google Scholar] [CrossRef]
- Milgrom, C.; Radeva-Petrova, D.R.; Finestone, A.; Nyska, M.; Mendelson, S.; Benjuya, N.; Simkin, A.; Burr, D. The effect of muscle fatigue on in vivo tibial strains. J. Biomech. 2007, 40, 845–850. [Google Scholar] [CrossRef]
- Murley, G.S.; Landorf, K.B.; Menz, H.B.; Bird, A.R. Effect of foot posture, foot orthoses and footwear on lower limb muscle activity during walking and running: A systematic review. Gait Posture 2009, 29, 172–187. [Google Scholar] [CrossRef]
- Telfer, S.; Woodburn, J. The use of 3D surface scanning for the measurement and assessment of the human foot. J. Foot Ankle Res. 2010, 3, 19. [Google Scholar] [CrossRef]
- Lin, K.-W.; Chou, L.-W.; Su, Y.-T.; Wei, S.-H.; Chen, C.-S. Biomechanical Effect of 3D-Printed Foot Orthoses in Patients with Knee Osteoarthritis. Appl. Sci. 2021, 11, 4200. [Google Scholar] [CrossRef]
- Hsu, C.Y.; Wang, C.S.; Lin, K.W.; Chien, M.J.; Wei, S.H.; Chen, C.S. Biomechanical Analysis of the FlatFoot with Different 3D-Printed Insoles on the Lower Extremities. Bioengineering 2022, 9, 563. [Google Scholar] [CrossRef]
- Ho, M.; Nguyen, J.; Heales, L.; Stanton, R.; Kong, P.W.; Kean, C. The biomechanical effects of 3D printed and traditionally made foot orthoses in individuals with unilateral plantar fasciopathy and flat feet. Gait Posture 2022, 96, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Tehraninasr, A.; Saeedi, H.; Forogh, B.; Bahramizadeh, M.; Keyhani, M.R. Effects of insole with toe-separator and night splint on patients with painful hallux valgus: A comparative study. Prosthet. Orthot. Int. 2008, 32, 79–83. [Google Scholar] [CrossRef]
- Moulodi, N.; Kamyab, M.; Farzadi, M. A comparison of the hallux valgus angle, range of motion, and patient satisfaction after use of dynamic and static orthoses. Foot 2019, 41, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Fuller, E.A. The windlass mechanism of the foot: A mechanical model to explain pathology. J. Am. Podiatr. Med. Assoc. 2000, 90, 35–46. [Google Scholar] [CrossRef]
- Tong, J.W.K.; Kong, P.W. Association between foot type and lower extremity injuries: Systematic literature review with meta-analysis. J. Orthop. Sports Phys. Ther. 2013, 43, 700–714. [Google Scholar] [CrossRef]
- Yang, Z.; Liu, F.; Cui, L.; Liu, H.; Zuo, J.; Liu, L.; Li, S. Adult rigid flatfoot. Medicine 2020, 99, e18826. [Google Scholar] [CrossRef]
- Schmitt, A.P.L.; Liebau, K.H.; Hamm, A.; Hacke, C.; Mittelmeier, W.; Schulze, C. Comparison of the influence of supportive and sensorimotor insoles in the muscle activity of tibialis anterior and peroneus longus in combat boots. Foot 2022, 52, 101910. [Google Scholar] [CrossRef]
- Huang, Y.P.; Peng, H.T.; Wang, X.; Chen, Z.R.; Song, C.Y. The arch support insoles show benefits to people with flatfoot on stance time, cadence, plantar pressure and contact area. PLoS ONE 2020, 15, e0237382. [Google Scholar] [CrossRef]
- Peng, Y.; Wong, D.W.C.; Wang, Y.; Chen, T.L.W.; Tan, Q.; Chen, Z.; Jin, Z.; Zhang, M. Immediate Effects of Medially Posted Insoles on Lower Limb Joint Contact Forces in Adult Acquired Flatfoot: A Pilot Study. Int. J. Environ. Res. Public Health 2020, 17, 2226. [Google Scholar] [CrossRef]
- De Saca, L.R.; Catlin, P.A.; Segal, R.L. Immediate Effects of the Toe Spreader on the Tonic Toe Flexion Reflex. Phys. Ther. 1994, 74, 561–570. [Google Scholar] [CrossRef]
- Lee, K.S.; Ko, E.; Lee, S.Y. Immediate Effect of the Toe Spreader on Tibialis Anterior and Peroneus Longus Muscle Activities: A Pilot Study. J. Phys. Ther. Sci. 2013, 25, 293–295. [Google Scholar] [CrossRef]
- Bojsen-Moller, F. Calcaneocuboid joint and stability of the longitudinal arch of the foot at high and low gear push off. J. Anat. 1979, 129, 165. [Google Scholar] [PubMed]
- Tang, S.F.; Chen, C.P.; Pan, J.L.; Chen, J.L.; Leong, C.P.; Chu, N.K. The effects of a new foot-toe orthosis in treating painful hallux valgus. Arch. Phys. Med. Rehabil. 2002, 83, 1792–1795. [Google Scholar] [CrossRef]
- Dingenen, B.; Peeraer, L.; Deschamps, K.; Fieuws, S.; Janssens, L.; Staes, F. Muscle-Activation Onset Times with Shoes and Foot Orthoses in Participants with Chronic Ankle Instability. J. Athl. Train. 2015, 50, 688. [Google Scholar] [CrossRef] [PubMed]
- Iskandar, M.N.S.; Loh, R.B.C.; Ho, M.Y.M.; Pan, J.W.; Kong, P.W. Crossover gait in running and measuring foot inversion angle at initial foot strike: A front-view video analysis approach. Front. Bioeng. Biotechnol. 2023, 11, 1210049. [Google Scholar] [CrossRef]
- Burden, A. How should we normalize electromyograms obtained from healthy participants? What we have learned from over 25 years of research. J. Electromyogr. Kinesiol. 2010, 20, 1023–1035. [Google Scholar] [CrossRef] [PubMed]
- Konrad, P. The ABC of EMG; Noraxon Inc.: Scottsdale, AZ, USA, 2005; ISBN 0977162214. [Google Scholar]
- Shi, L.; Ye, X.; Han, D.; Yang, C.; Tu, Y. Acute Effects of Back Squat Combined with Different Elastic Band Resistance on Vertical Jump Performance in Collegiate Basketball Players. J. Sports Sci. Med. 2023, 22, 502. [Google Scholar] [CrossRef]
- Longo, G.; Denaro, V.; Ribeiro, A.P.; Maria, S.; João, A. The Effect of Short and Long-Term Therapeutic Treatment with Insoles and Shoes on Pain, Function, and Plantar Load Parameters of Women with Plantar Fasciitis: A Randomized Controlled Trial. Medicina 2022, 58, 1546. [Google Scholar] [CrossRef]
- Chadchavalpanichaya, N.; Prakotmongkol, V.; Polhan, N.; Rayothee, P.; Seng-Iad, S. Effectiveness of the custom-mold room temperature vulcanizing silicone toe separator on hallux valgus: A prospective, randomized single-blinded controlled trial. Prosthet. Orthot. Int. 2018, 42, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Kosashvili, Y.; Fridman, T.; Backstein, D.; Safir, O.; Ziv, Y.B. The correlation between pes planus and anterior knee or intermittent low back pain. Foot Ankle Int. 2008, 29, 910–913. [Google Scholar] [CrossRef]
- Farokhmanesh, K.; Shirzadian, T.; Mahboubi, M.; Shahri, M.N. Effect of Foot Hyperpronation on Lumbar Lordosis and Thoracic Kyphosis in Standing Position Using 3-Dimensional Ultrasound-Based Motion Analysis System. Glob. J. Health Sci. 2014, 6, 254. [Google Scholar] [CrossRef]
- Sung, P.S.; Zipple, J.T.; Andraka, J.M.; Danial, P. The kinetic and kinematic stability measures in healthy adult subjects with and without flat foot. Foot 2017, 30, 21–26. [Google Scholar] [CrossRef]
- Monajati, A.; Larumbe-Zabala, E.; Goss-Sampson, M.; Naclerio, F. Surface Electromyography Analysis of Three Squat Exercises. J. Hum. Kinet. 2019, 67, 73–83. [Google Scholar] [CrossRef]
- Romkes, J.; Rudmann, C.; Brunner, R. Changes in gait and EMG when walking with the Masai Barefoot Technique. Clin. Biomech. 2006, 21, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Murley, G.S.; Landorf, K.B.; Menz, H.B. Do foot orthoses change lower limb muscle activity in flat-arched feet towards a pattern observed in normal-arched feet? Clin. Biomech. 2010, 25, 728–736. [Google Scholar] [CrossRef]
- Harms-Ringdahl, K.; Ekholm, J.; Schüldt, K.; Linder, J.; Ericson, M.O. Assessment of jet pilots’ upper trapezius load calibrated to maximal voluntary contraction and a standardized load. J. Electromyogr. Kinesiol. 1996, 6, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Murley, G.S.; Bird, A.R. The effect of three levels of foot orthotic wedging on the surface electromyographic activity of selected lower limb muscles during gait. Clin. Biomech. 2006, 21, 1074–1080. [Google Scholar] [CrossRef]
- Marouvo, J.; Sousa, F.; Fernandes, O.; Castro, M.A.; Paszkiel, S. Gait Kinematics Analysis of Flatfoot Adults. Appl. Sci. 2021, 11, 7077. [Google Scholar] [CrossRef]
- Lee, K.K.W.; Ling, S.K.K.; Yung, P.S.H. Controlled trial to compare the Achilles tendon load during running in flatfeet participants using a customized arch support orthoses vs an orthotic heel lift. BMC Musculoskelet. Disord. 2019, 20, 535. [Google Scholar] [CrossRef]
- Park, S.; Jung, J.-H.; Lei, S.; Jung, E.-Y.; Cho, H.-Y. 3D-Printed Customized Arch-Support Insoles Improve Gait Mechanics and Ankle Alignment in Young Adults with Functional Flat Foot During Uphill Walking. Medicina 2025, 61, 281. [Google Scholar] [CrossRef] [PubMed]
- Buldt, A.K.; Murley, G.S.; Butterworth, P.; Levinger, P.; Menz, H.B.; Landorf, K.B. The relationship between foot posture and lower limb kinematics during walking: A systematic review. Gait Posture 2013, 38, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Levinger, P.; Murley, G.S.; Barton, C.J.; Cotchett, M.P.; McSweeney, S.R.; Menz, H.B. A comparison of foot kinematics in people with normal- and flat-arched feet using the Oxford Foot Model. Gait Posture 2010, 32, 519–523. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, E.-Y.; Lei, S.; Jeong, Y.; Cho, H.-Y.; Park, S. 3D-Printed Arch Supports Combined with Toe Spreaders Modulate Phase-Specific Ankle Alignment and Muscle Activity in Young Adults with Functional Flat Foot. J. Clin. Med. 2025, 14, 8017. https://doi.org/10.3390/jcm14228017
Jung E-Y, Lei S, Jeong Y, Cho H-Y, Park S. 3D-Printed Arch Supports Combined with Toe Spreaders Modulate Phase-Specific Ankle Alignment and Muscle Activity in Young Adults with Functional Flat Foot. Journal of Clinical Medicine. 2025; 14(22):8017. https://doi.org/10.3390/jcm14228017
Chicago/Turabian StyleJung, Eui-Young, Shi Lei, Yujin Jeong, Hwi-Young Cho, and Sanghee Park. 2025. "3D-Printed Arch Supports Combined with Toe Spreaders Modulate Phase-Specific Ankle Alignment and Muscle Activity in Young Adults with Functional Flat Foot" Journal of Clinical Medicine 14, no. 22: 8017. https://doi.org/10.3390/jcm14228017
APA StyleJung, E.-Y., Lei, S., Jeong, Y., Cho, H.-Y., & Park, S. (2025). 3D-Printed Arch Supports Combined with Toe Spreaders Modulate Phase-Specific Ankle Alignment and Muscle Activity in Young Adults with Functional Flat Foot. Journal of Clinical Medicine, 14(22), 8017. https://doi.org/10.3390/jcm14228017






