A Case of Lumbar Spinal Epidural Abscess and Facet Joint Septic Arthritis Caused by Haemophilus influenzae in an Immunocompetent Host
Abstract
1. Introduction
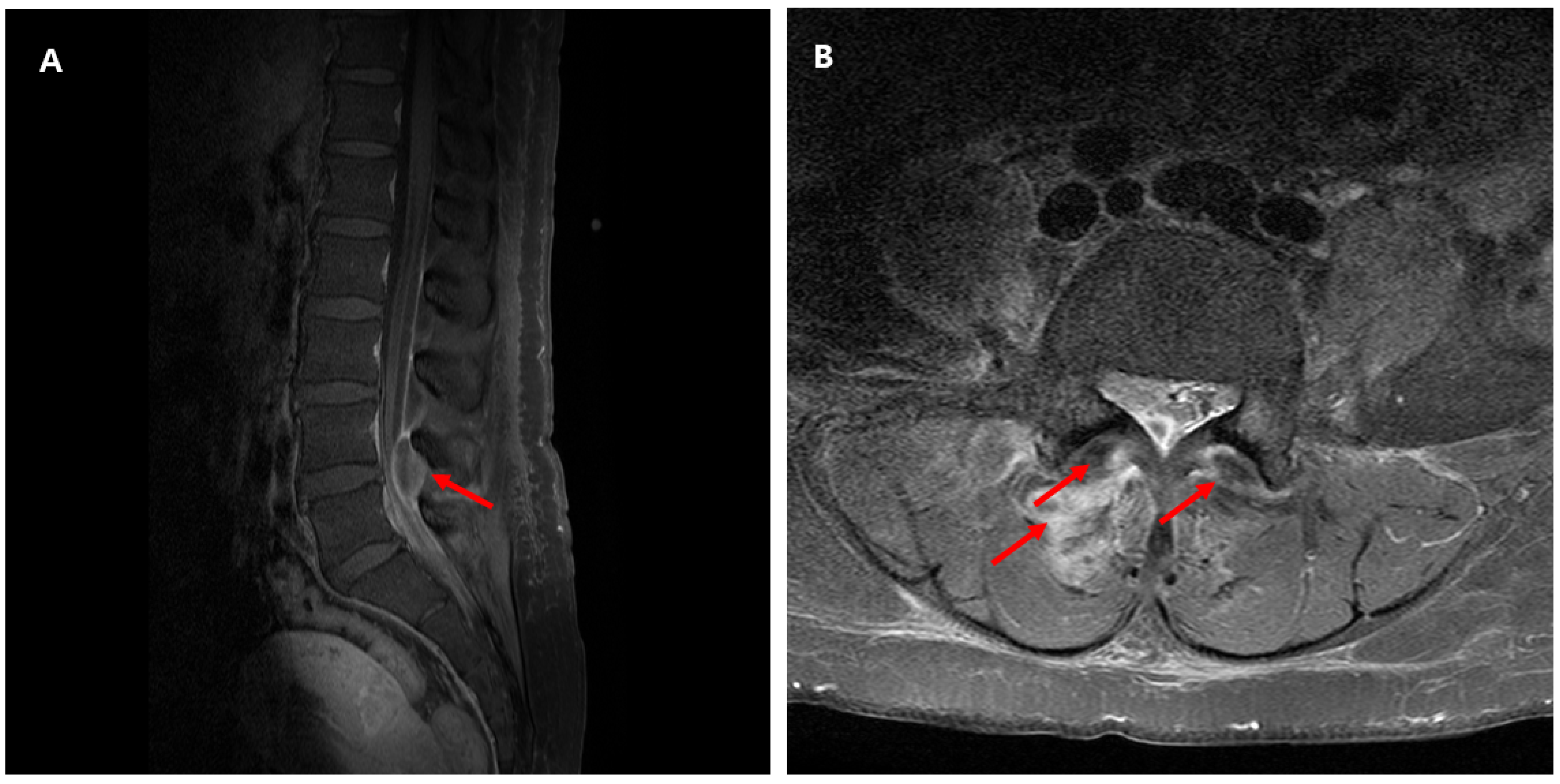
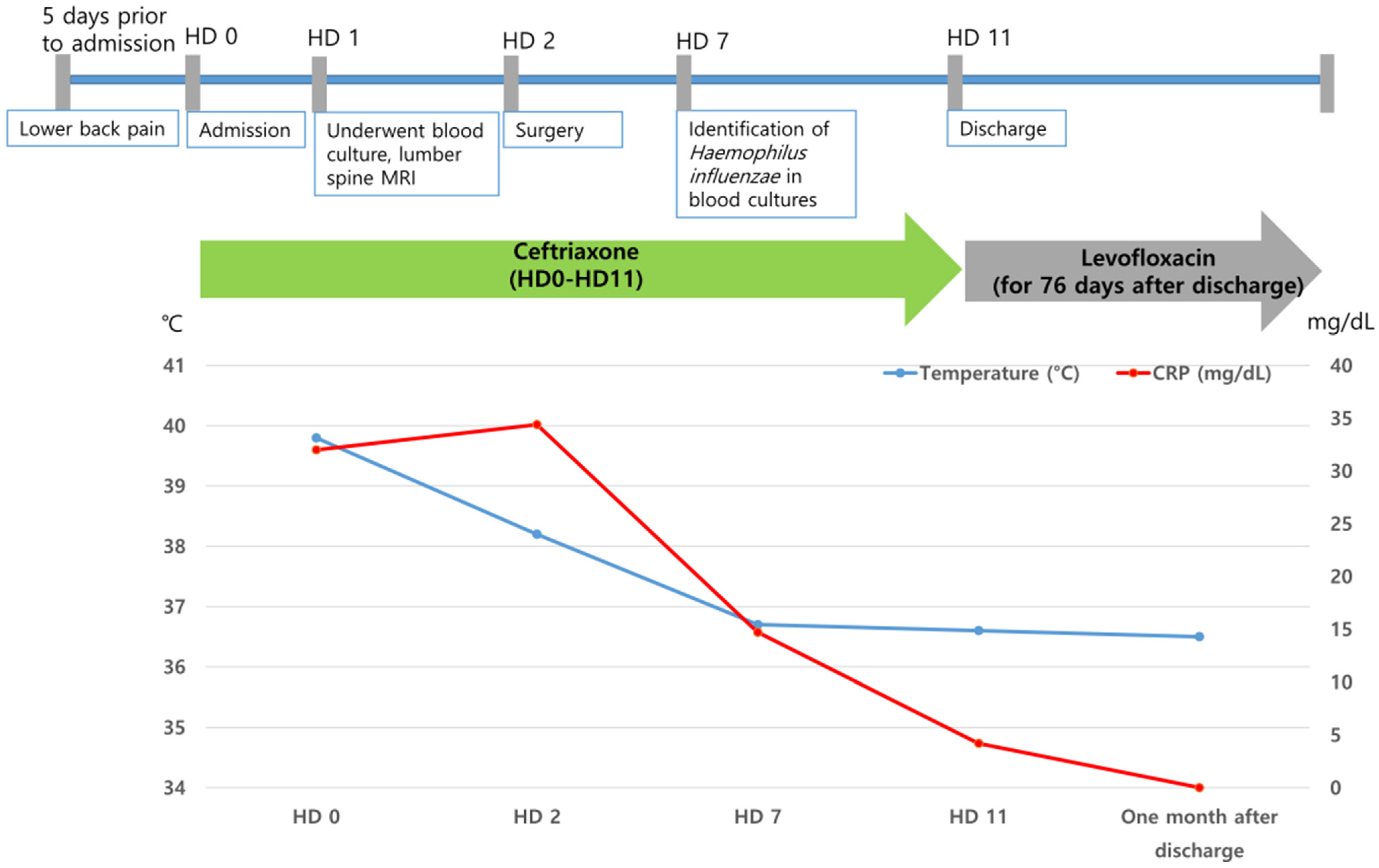
2. Case Presentation
3. Discussion
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peltola, H. Worldwide Haemophilus influenzae Type b Disease at the Beginning of the 21st Century: Global Analysis of the Disease Burden 25 Years after the Use of the Polysaccharide Vaccine and a Decade after the Advent of Conjugates. Clin. Microbiol. Rev. 2000, 13, 302–317. [Google Scholar] [CrossRef]
- Ladhani, S.; Slack, M.P.; Heath, P.T.; von Gottberg, A.; Chandra, M.; Ramsay, M.E. Invasive haemophilus influenzae disease, europe, 1996–2006. Emerg. Infect. Dis. 2010, 16, 455–463. [Google Scholar] [CrossRef]
- Bertran, M.; D’Aeth, J.C.; Hani, E.; Amin-Chowdhury, Z.; Fry, N.K.; Ramsay, M.E.; Litt, D.J.; Ladhani, S.N. Trends in invasive haemophilus influenzae serotype a disease in england from 2008–09 to 2021–22: A prospective national surveillance study. Lancet. Infect. Dis. 2023, 23, 1197–1206. [Google Scholar] [CrossRef] [PubMed]
- Langereis, J.D.; de Jonge, M.I. Invasive disease caused by nontypeable haemophilus influenzae. Emerg. Infect. Dis. 2015, 21, 1711–1718. [Google Scholar] [CrossRef] [PubMed]
- Abdi, A.M.; Yehualaw, D.D.; Kebede, T.S.; Darod, Z.A. A Global Review of Invasive Haemophilus Influenzae Disease from 2000–2023: Current Status, Challenges and Future Perspectives. 2024. Available online: https://www.preprints.org/manuscript/202306.0948 (accessed on 7 November 2025).
- Oliver, S.E.; Rubis, A.B.; Soeters, H.M.; Reingold, A.; Barnes, M.; Petit, S.; Farley, M.M.; Harrison, L.H.; Como-Sabetti, K.; Khanlian, S.A.; et al. Epidemiology of invasive nontypeable haemophilus influenzae disease—United states, 2008–2019. Clin. Infect. Dis. 2023, 76, 1889–1895. [Google Scholar] [CrossRef] [PubMed]
- Van Eldere, J.; Slack, M.P.; Ladhani, S.; Cripps, A.W. Non-typeable haemophilus influenzae, an under-recognised pathogen. Lancet. Infect. Dis. 2014, 14, 1281–1292. [Google Scholar] [CrossRef]
- Slack, M.; Esposito, S.; Haas, H.; Mihalyi, A.; Nissen, M.; Mukherjee, P.; Harrington, L. Haemophilus influenzae type b disease in the era of conjugate vaccines: Critical factors for successful eradication. Expert Rev. Vaccines 2020, 19, 903–917. [Google Scholar] [CrossRef]
- Tristram, S.; Jacobs, M.R.; Appelbaum, P.C. Antimicrobial resistance in haemophilus influenzae. Clin. Microbiol. Rev. 2007, 20, 368–389. [Google Scholar] [CrossRef]
- Gutmann, L.; Williamson, R.; Collatz, E.; Acar, J.F. Mechanisms of beta-lactam resistance in haemophilus influenzae. Eur. J. Clin. Microbiol. Infect. Dis. 1988, 7, 610–615. [Google Scholar] [CrossRef]
- Qiao, L.; Choi, A.; Jung, J. Cervical spinal epidural abscess from haemophilus influenzae in an adult: A case report. Cureus 2024, 16, e74946. [Google Scholar] [CrossRef]
- Sermet, K.; Demaeght, F.; Alcaraz, I.; Viget, N.; Dauenhauer, J.; Senneville, E.; Robineau, O. A rare case of invasive non-typeable haemophilus influenzae spondylodiscitis and periprosthetic joint infection. J. Bone Jt. Infect. 2021, 6, 207–209. [Google Scholar] [CrossRef] [PubMed]
- Howard, A.J. Nosocomial spread of haemophilus influenzae. J. Hosp. Infect. 1991, 19, 1–3. [Google Scholar] [CrossRef]
- Briere, E.C.; Rubin, L.; Moro, P.L.; Cohn, A.; Clark, T.; Messonnier, N. Prevention and control of haemophilus influenzae type b disease: Recommendations of the advisory committee on immunization practices (acip). MMWR. Recomm. Rep. 2014, 63, 1–14. [Google Scholar]
- Winkelstein, J.A.; Moxon, E.R. The role of complement in the host’s defense against haemophilus influenzae. J. Infect. Dis. 1992, 165, S62–S65. [Google Scholar] [CrossRef]
- Auten, G.M.; Levy, C.S.; Smith, M.A. Haemophilus parainfluenzae as a rare cause of epidural abscess: Case report and review. Rev. Infect. Dis. 1991, 13, 609–612. [Google Scholar] [CrossRef]
- Scerpella, E.G.; Wu, S.; Oefinger, P.E. Case report of spinal epidural abscess caused by haemophilus paraphrophilus. J. Clin. Microbiol. 1994, 32, 563–564. [Google Scholar] [CrossRef]
- McCann, N.; Barakat, M.F.; Schafer, F. An aggressive form of haemophilus parainfluenzae infective endocarditis presenting with limb weakness. BMJ Case Rep. 2018, 2018, bcr-2017. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.J.; Ard, K.L. Septic arthritis of the spinal facet joint: Review of 117 cases. Open Forum Infect. Dis. 2024, 11, ofae091. [Google Scholar] [CrossRef]
- Borenstein, D.G.; Simon, G.L. Hemophilus influenzae septic arthritis in adults: A report of four cases and a review of the literature. Medicine 1986, 65, 191. [Google Scholar] [CrossRef] [PubMed]
- Ho Jr, G.; Gadbaw Jr, J.J.; Glickstein, S.L. Hemophilus Influenzae Septic Arthritis in Adults; Seminars in Arthritis and Rheumatism; Elsevier: Amsterdam, The Netherlands, 1983; pp. 314–321. [Google Scholar]
- Kim, J.H.; Muto, C.A.; Pasculle, A.W.; Vergis, E.N. Invasive polyarticular septic arthritis caused by nontypeable haemophilus influenzae in a young adult: A case report and literature review. J. Clin. Rheumatol. 2011, 17, 380–382. [Google Scholar] [CrossRef]
- Arko, L.t.; Quach, E.; Nguyen, V.; Chang, D.; Sukul, V.; Kim, B.S. Medical and surgical management of spinal epidural abscess: A systematic review. Neurosurg. Focus 2014, 37, E4. [Google Scholar] [CrossRef] [PubMed]
- Stratton, A.; Gustafson, K.; Thomas, K.; James, M.T. Incidence and risk factors for failed medical management of spinal epidural abscess: A systematic review and meta-analysis. J. Neurosurg. Spine 2017, 26, 81–89. [Google Scholar] [CrossRef]
- Lee, Y.M.; Cho, O.H.; Park, S.Y.; Moon, C.; Chong, Y.P.; Kim, S.H.; Lee, S.O.; Choi, S.H.; Lee, M.S.; Bae, I.G.; et al. Factors associated with sequelae after treatment of hematogenous pyogenic vertebral osteomyelitis. Diagn. Microbiol. Infect. Dis. 2019, 94, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Berndsen, M.R.; Erlendsdóttir, H.; Gottfredsson, M. Evolving epidemiology of invasive haemophilus infections in the post-vaccination era: Results from a long-term population-based study. Clin. Microbiol. Infect. 2012, 18, 918–923. [Google Scholar] [CrossRef] [PubMed]
| Case | Age/ Sex | Underlying Conditions | Symptom | Implant | Involved Site | Combined Infection | Co-Pathogen | Neurologic Deficit | Surgery | Antibiotic Therapy | Outcome | Neurologic Sequelae | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F/79 | Diabetes, hypertension, atrial fibrillation, history of right hip fracture (10 years ago) | Right hip pain Fever | Hip prosthesis | L4-5 Hip prosthesis | None | None | No | Yes | Cefotaxime (12 weeks) → Ciprofloxacin (21 days) | Survived | No | [12] |
| 2 | F/74 | Diabetes, hypertension, disc at cervical spine | Neck pain Headache | No | C1-C2 | None | None | No | Yes | Ceftriaxone (6 weeks) | Survived | No | [11] |
| 3 | F/53 | Lumbar spine disc herniation | Right lower back pain with radiating pain in the right thigh Fever | No | L4-5 | None | None | No | Yes (HD 2) | Ceftriaxone (11 days) → levofloxacin (76 days) | Survived | No | This case |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-M. A Case of Lumbar Spinal Epidural Abscess and Facet Joint Septic Arthritis Caused by Haemophilus influenzae in an Immunocompetent Host. J. Clin. Med. 2025, 14, 8006. https://doi.org/10.3390/jcm14228006
Lee Y-M. A Case of Lumbar Spinal Epidural Abscess and Facet Joint Septic Arthritis Caused by Haemophilus influenzae in an Immunocompetent Host. Journal of Clinical Medicine. 2025; 14(22):8006. https://doi.org/10.3390/jcm14228006
Chicago/Turabian StyleLee, Yu-Mi. 2025. "A Case of Lumbar Spinal Epidural Abscess and Facet Joint Septic Arthritis Caused by Haemophilus influenzae in an Immunocompetent Host" Journal of Clinical Medicine 14, no. 22: 8006. https://doi.org/10.3390/jcm14228006
APA StyleLee, Y.-M. (2025). A Case of Lumbar Spinal Epidural Abscess and Facet Joint Septic Arthritis Caused by Haemophilus influenzae in an Immunocompetent Host. Journal of Clinical Medicine, 14(22), 8006. https://doi.org/10.3390/jcm14228006





