Comparisons of Clinical and Functional Characteristics of Patients with Epiretinal Membrane, Macular Pseudohole, Epiretinal Membrane Foveoschisis, and Lamellar Macular Hole
Abstract
1. Introduction
2. Methods
2.1. Patient Selection and Classification
2.2. Visual Assessment
2.3. Surgical Procedures
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hubschman, J.P.; Govetto, A.; Spaide, R.F.; Schumann, R.; Steel, D.; Figueroa, M.S.; Sebag, J.; Gaudric, A.; Staurenghi, G.; Haritoglou, C.; et al. Optical coherence tomography-based consensus definition for lamellar macular hole. Br. J. Ophthalmol. 2020, 104, 1741–1747. [Google Scholar] [CrossRef] [PubMed]
- dell’Omo, R.; Filippelli, M.; De Turris, S.; Cimino, L.; Steel, D.H.; Pavesio, C.E.; Govetto, A.; Chehaibou, I.; Parmeggiani, F.; Romano, M.R.; et al. Fluorescein Angiography Findings in Eyes with Lamellar Macular Hole and Epiretinal Membrane Foveoschisis. Investig. Ophthalmol. Vis. Sci. 2021, 62, 34. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nakamura, K.; Inoue, T.; Nagura, K.; Tanaka, Y.; Arasaki, R.; Asaoka, R.; Yanagi, Y.; Maruyama-Inoue, M.; Kadonosono, K. Foveal microstructure and visual function in patients with lamellar macular hole, epiretinal membrane foveoschisis or macular pseudohole. Eye 2022, 36, 2247–2252. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hetzel, A.; Neubauer, J.; Gelisken, F. Clinical characteristics of patients with epiretinal membrane-Foveoschisis. Graefes Arch. Clin. Exp. Ophthalmol. 2023, 261, 1579–1585. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Omoto, T.; Asahina, Y.; Zhou, H.P.; Fujino, R.; Takao, M.; Obata, R.; Inoue, T.; Asaoka, R.; Maruyama-Inoue, M.; Yanagi, Y.; et al. Visual outcomes and prognostic factors of vitrectomy for lamellar macular holes and epiretinal membrane foveoschisis. PLoS ONE 2021, 16, e0247509. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Photcharapongsakul, C.; Chokesuwattanaskul, S.; Choovuthayakorn, J.; Chaikitmongkol, V.; Kunavisarut, P.; Watanachai, N.; Patikulsila, D. Visual acuity and anatomical changes following vitrectomy for epiretinal membrane foveoschisis: A case series. BMC Ophthalmol. 2021, 21, 433. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lam, M.; Philippakis, E.; Gaudric, A.; Tadayoni, R.; Couturier, A. Postoperative outcomes of idiopathic epiretinal membrane associated with foveoschisis. Br. J. Ophthalmol. 2022, 106, 1000–1005. [Google Scholar] [CrossRef] [PubMed]
- Sekine, R.; Kogo, J.; Jujo, T.; Sato, K.; Arizono, I.; Kawagoe, T.; Tokuda, N.; Kitaoka, Y.; Takagi, H. Efficacy of Fovea-Sparing Internal Limiting Membrane Peeling for Epiretinal Membrane Foveoschisis. Ophthalmic Res. 2022, 65, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, T.; Matsui, Y.; Kato, K.; Chujo, S.; Maeda, S.; Ozaki, A.; Ikesugi, K.; Sugimoto, M.; Matsubara, H.; Kondo, M. Comparisons of Clinical Characteristics and Surgical Outcomes of Epiretinal Membrane Foveoschisis to Typical Epiretinal Membrane. J. Clin. Med. 2023, 12, 4009. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Matoba, R.; Kanzaki, Y.; Morita, T.; Masuda, Y.; Kimura, S.; Hosokawa, M.M.; Shiode, Y.; Morizane, Y. Mixed Pathophysiologies of Lamellar Macular Holes and Related Diseases: A Multimodal Optical Coherence Tomography-Based Study. Retina 2024, 44, 1785–1792. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, T.; Matsuyama, K. Nippon Medical School’s Ethical Review Processes for Studies Involving Human Subjects. J. Nippon Med. Sch. 2024, 91, 136–139. [Google Scholar] [CrossRef] [PubMed]
- da Silva, R.A.; Roda, V.M.P.; Matsuda, M.; Siqueira, P.V.; Lustoza-Costa, G.J.; Wu, D.C.; Hamassaki, D.E. Cellular components of the idiopathic epiretinal membrane. Graefes Arch. Clin. Exp. Ophthalmol. 2022, 260, 1435–1444. [Google Scholar] [CrossRef] [PubMed]
- Parolini, B.; Schumann, R.G.; Cereda, M.G.; Haritoglou, C.; Pertile, G. Lamellar macular hole: A clinicopathologic correlation of surgically excised epiretinal membranes. Investig. Ophthalmol. Vis. Sci. 2011, 52, 9074–9083. [Google Scholar] [CrossRef] [PubMed]
- Compera, D.; Entchev, E.; Haritoglou, C.; Scheler, R.; Mayer, W.J.; Wolf, A.; Kampik, A.; Schumann, R.G. Lamellar Hole-Associated Epiretinal Proliferation in Comparison to Epiretinal Membranes of Macular Pseudoholes. Am. J. Ophthalmol. 2015, 160, 373–384.e1. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.S.; Lee, J.S.; Son, G.; Sohn, J. Epiretinal Proliferation Associated with Lamellar Hole or Macular Hole: Origin and Surgical Prognosis. Korean J. Ophthalmol. 2019, 33, 142–149. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Goldman, D. Müller glial cell reprogramming and retina regeneration. Nat. Rev. Neurosci. 2014, 15, 431–442. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Frisina, R.; Gius, I.; Palmieri, M.; Finzi, A.; Tozzi, L.; Parolini, B. Myopic Traction Maculopathy: Diagnostic and Management Strategies. Clin. Ophthalmol. 2020, 14, 3699–3708. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pertile, G.; Iacovello, D.; Maraone, G.; Bottega, E.; Guerriero, M.; Maggio, E. Lamellar macular defects: Are degenerative lamellar macular holes truly degenerative? Front. Med. 2023, 10, 1156410. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mohammed, T.K.; Thompson, J.T. Outcomes of Pars Plana Vitrectomy With Membrane Peel for Lamellar Macular Holes and Related Conditions Using a New Optical Coherence Tomography Consensus Definition. J. Vitreoretin. Dis. 2023, 8, 125–130. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Okamoto, F. Changes in Metamorphopsia in Patients Undergoing Treatment for Vitreoretinal Disorders. J. Nippon Med. Sch. 2024, 91, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, S.; Okamoto, F.; Yuasa, M.; Kunikata, T.; Okamoto, Y.; Hiraoka, T.; Oshika, T. Vision-related quality of life and visual function in patients undergoing vitrectomy, gas tamponade and cataract surgery for macular hole. Br. J. Ophthalmol. 2009, 93, 1595–1599. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, F.; Okamoto, Y.; Hiraoka, T.; Oshika, T. Effect of vitrectomy for epiretinal membrane on visual function and vision-related quality of life. Am. J. Ophthalmol. 2009, 147, 869–874.e1. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, F.; Okamoto, Y.; Fukuda, S.; Hiraoka, T.; Oshika, T. Vision-related quality of life and visual function after vitrectomy for various vitreoretinal disorders. Investig. Ophthalmol. Vis. Sci. 2010, 51, 744–751. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudzadeh, R.; Israilevich, R.; Salabati, M.; Hsu, J.; Garg, S.J.; Regillo, C.D.; Ho, A.C.; Khan, M.A. Pars Plana Vitrectomy for Idiopathic Epiretinal Membrane: OCT Biomarkers of Visual Outcomes in 322 Eyes. Ophthalmol. Retina. 2022, 6, 308–317. [Google Scholar] [CrossRef] [PubMed]
- Chatzistergiou, V.; Papasavvas, I.; Ambresin, A.; Pournaras, J.C. Prediction of Postoperative Visual Outcome in Patients with Idiopathic Epiretinal Membrane. Ophthalmologica 2021, 244, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Minami, S.; Shinoda, H.; Shigeno, Y.; Nagai, N.; Kurihara, T.; Watanabe, K.; Sonobe, H.; Takagi, H.; Tsubota, K.; Ozawa, Y. Effect of axial length and age on the visual outcome of patients with idiopathic epiretinal membrane after pars plana vitrectomy. Sci. Rep. 2019, 9, 19056. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Scheerlinck, L.M.; van der Valk, R.; van Leeuwen, R. Predictive factors for postoperative visual acuity in idiopathic epiretinal membrane: A systematic review. Acta Ophthalmol. 2015, 93, 203–212. [Google Scholar] [CrossRef] [PubMed]
| ERM | MPH | ERM-FS | LMH | |
|---|---|---|---|---|
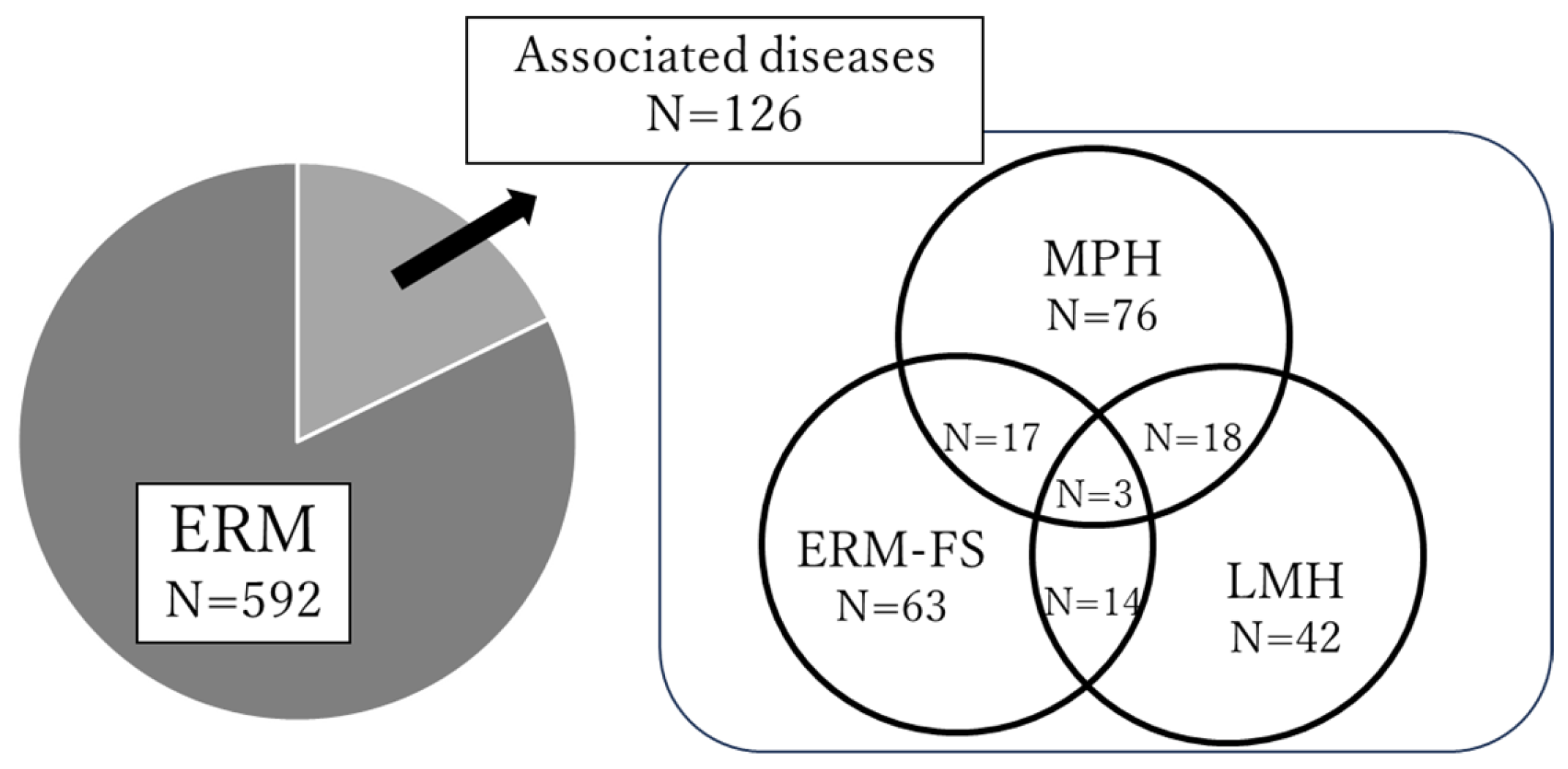
| Number of eyes | 592 | 76 | 63 | 42 |
| Age, mean ± SD, years | 71.7 ± 8.2 | 71.1 ± 7.8 | 69.6 ± 8.8 | 71.3 ± 8.2 |
| Gender, Men/Women | 315/277 | 37/39 | 28/35 | 21/21 |
| Prevalences of glaucoma (%) | 60 (10.1%) | 8 (10.5%) | 8 (12.7%) | 6 (14.3%) |
| AL, mm | 24.0 ± 1.38 | 24.8 ± 2.01 * | 24.8 ± 2.00 * | 24.9 ±1.88 * |
| SE, diopter | −0.94 ± 3.02 | −2.41 ± 4.87 | −2.32 ± 4.93 | −2.59 ± 4.57 |
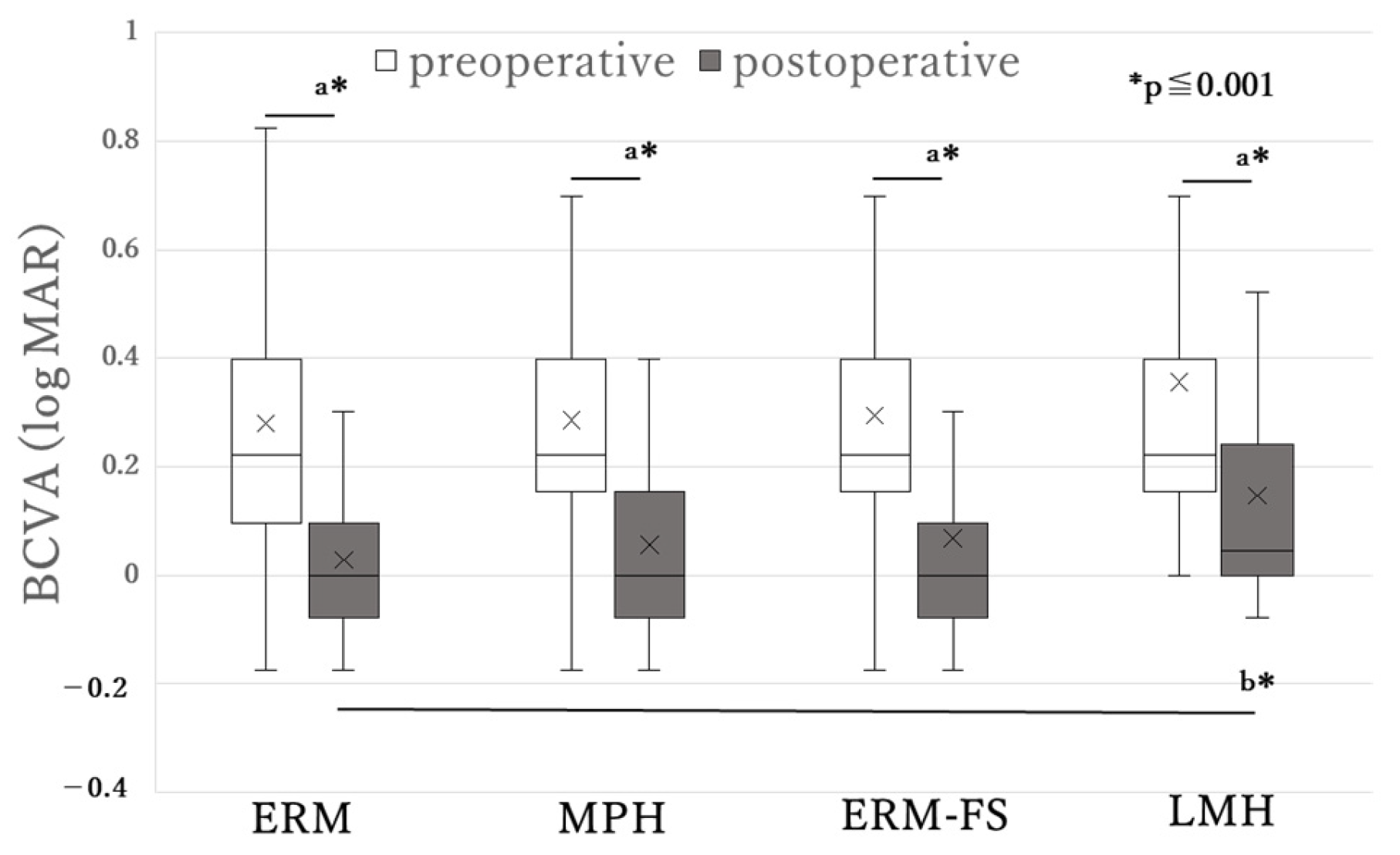
| Preoperative BCVA | 0.29 ± 0.26 | 0.29 ± 0.25 | 0.29 ± 0.30 | 0.36 ± 0.33 |
| Postoperative BCVA | 0.03 ± 0.19 | 0.06 ± 0.17 | 0.07 ± 0.24 | 0.15 ± 0.26 † |
| Preoperative metamorphopsia score | 0.52 ± 0.51 * | 0.34 ± 0.29 * | 0.36 ± 0.30 | 0.46 ± 0.38 |
| ERM | MPH | ERM-FS | LMH | |||||
|---|---|---|---|---|---|---|---|---|
| r | p Value | r | p Value | r | p Value | r | p Value | |
| Age | 0.113 | <0.01 * | 0.211 | 0.071 | −0.159 | 0.212 | −0.198 | 0.208 |
| AL | −0.033 | 0.455 | 0.086 | 0.481 | 0.281 | <0.05 * | 0.069 | 0.68 |
| SE | −0.042 | 0.318 | −0.134 | 0.254 | −0.146 | 0.253 | 0.05 | 0.755 |
| Metamorphopsia score | 0.012 | 0.848 | −0.353 | <0.05 * | 0.145 | 0.437 | 0.279 | 0.197 |
| ERM | MPH | ERM-FS | LMH | |||||
|---|---|---|---|---|---|---|---|---|
| r | p Value | r | p Value | r | p Value | r | p Value | |
| Preoperative BCVA | 0.423 | <0.001 * | 0.412 | <0.001 * | 0.339 | 0.006 * | 0.522 | <0.001 * |
| Age | 0.31 | <0.001 * | 0.452 | <0.001 * | 0.256 | <0.05 * | 0.218 | 0.171 |
| AL | −0.142 | 0.001 * | −0.096 | 0.427 | 0.136 | 0.311 | −0.282 | 0.091 |
| SE | 0.079 | 0.055 | 0.023 | 0.849 | −0.003 | 0.980 | 0.188 | 0.238 |
| Metamorphopsia score | −0.089 | 0.145 | 0.05 | 0.774 | 0.09 | 0.631 | 0.085 | 0.699 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kubota, N.; Miyata, K.; Mori, Y.; Nakano, Y.; Goto, H.; Okamoto, F. Comparisons of Clinical and Functional Characteristics of Patients with Epiretinal Membrane, Macular Pseudohole, Epiretinal Membrane Foveoschisis, and Lamellar Macular Hole. J. Clin. Med. 2025, 14, 7991. https://doi.org/10.3390/jcm14227991
Kubota N, Miyata K, Mori Y, Nakano Y, Goto H, Okamoto F. Comparisons of Clinical and Functional Characteristics of Patients with Epiretinal Membrane, Macular Pseudohole, Epiretinal Membrane Foveoschisis, and Lamellar Macular Hole. Journal of Clinical Medicine. 2025; 14(22):7991. https://doi.org/10.3390/jcm14227991
Chicago/Turabian StyleKubota, Noriko, Kazunori Miyata, Yosai Mori, Yuji Nakano, Hitoshi Goto, and Fumiki Okamoto. 2025. "Comparisons of Clinical and Functional Characteristics of Patients with Epiretinal Membrane, Macular Pseudohole, Epiretinal Membrane Foveoschisis, and Lamellar Macular Hole" Journal of Clinical Medicine 14, no. 22: 7991. https://doi.org/10.3390/jcm14227991
APA StyleKubota, N., Miyata, K., Mori, Y., Nakano, Y., Goto, H., & Okamoto, F. (2025). Comparisons of Clinical and Functional Characteristics of Patients with Epiretinal Membrane, Macular Pseudohole, Epiretinal Membrane Foveoschisis, and Lamellar Macular Hole. Journal of Clinical Medicine, 14(22), 7991. https://doi.org/10.3390/jcm14227991







