Simultaneous Endovascular Abdominal Aortic Aneurysm Repair and Open Repair of Common Femoral Artery Aneurysm: Short Case Series and Current Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
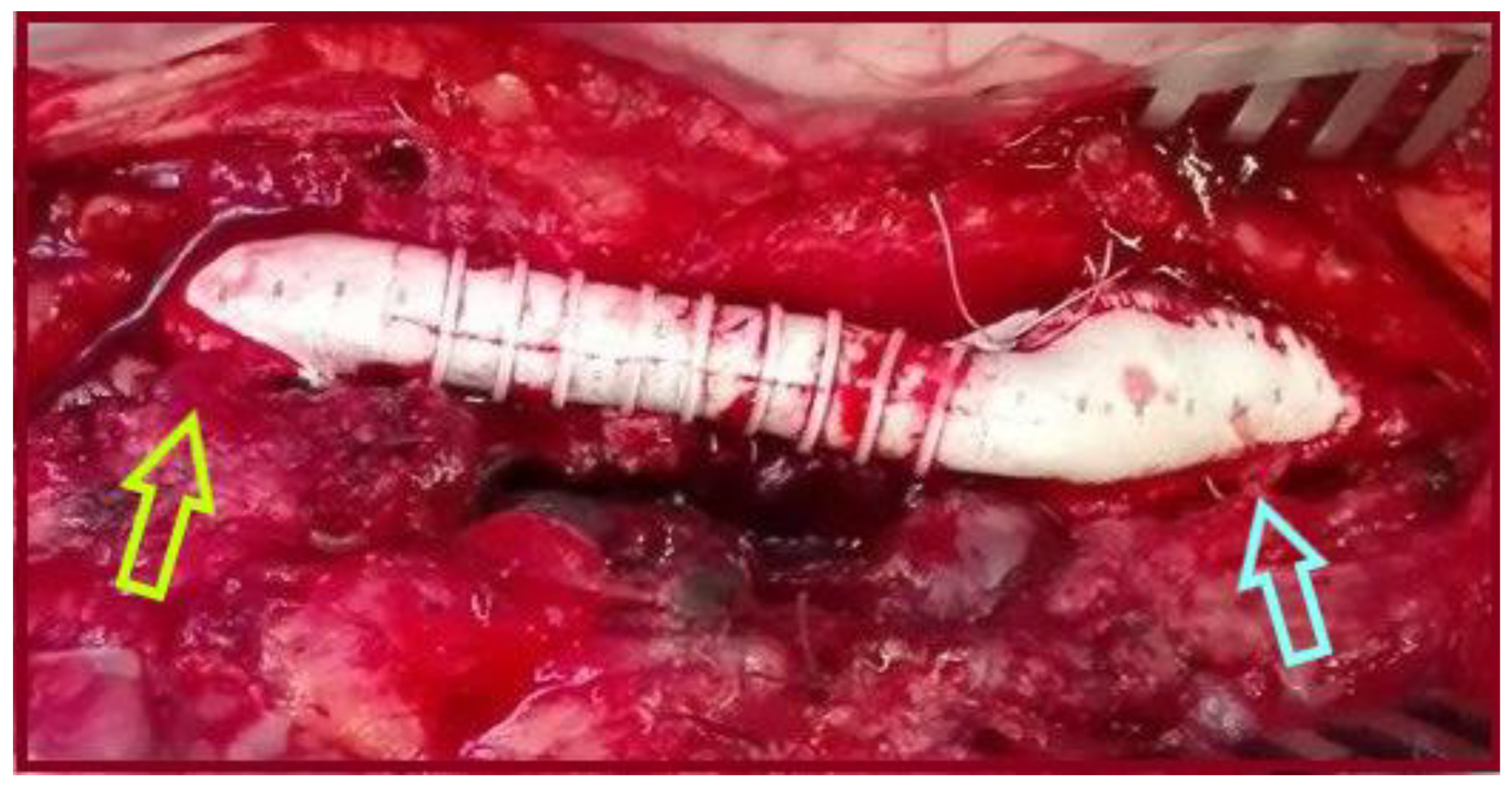
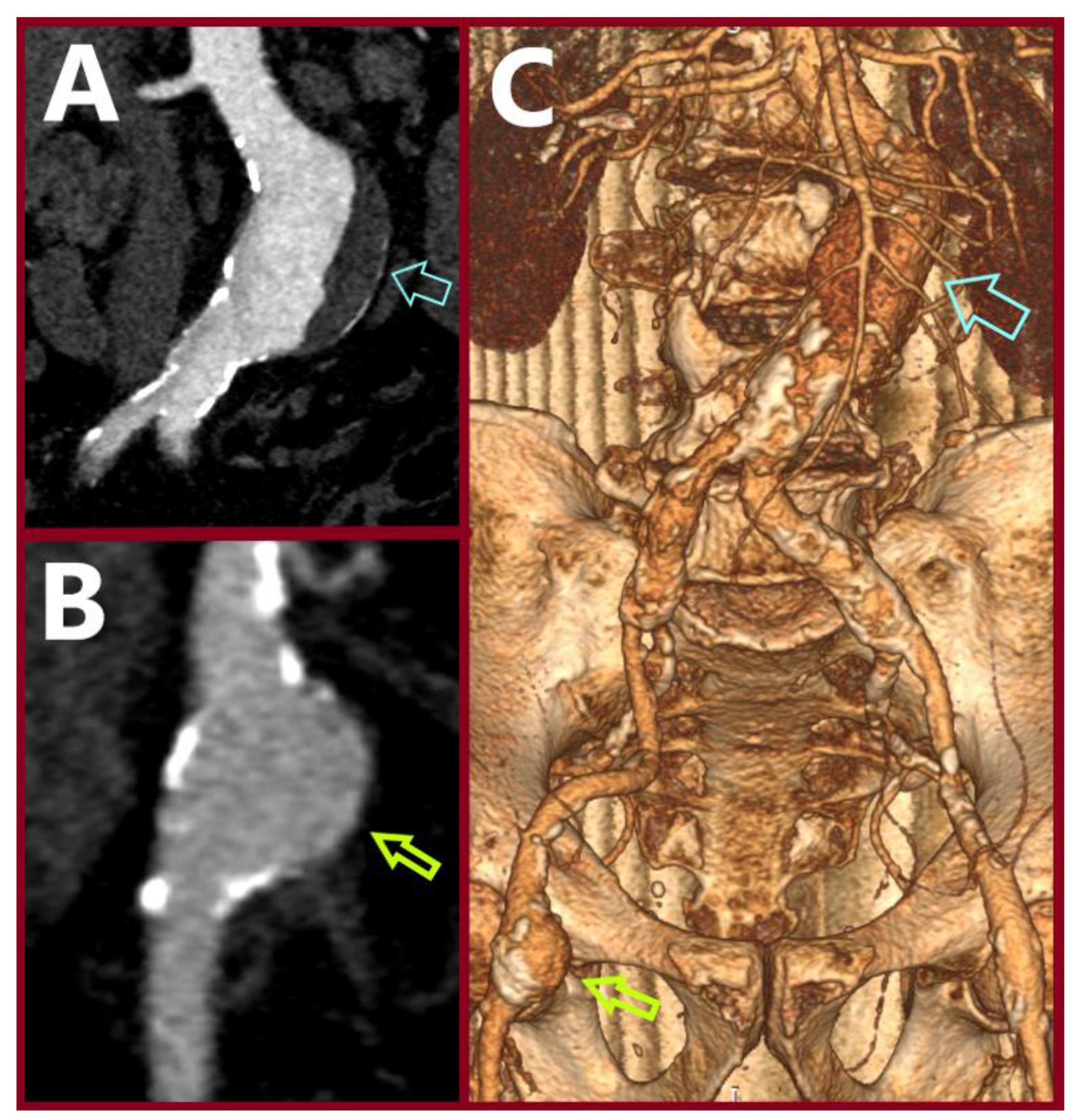
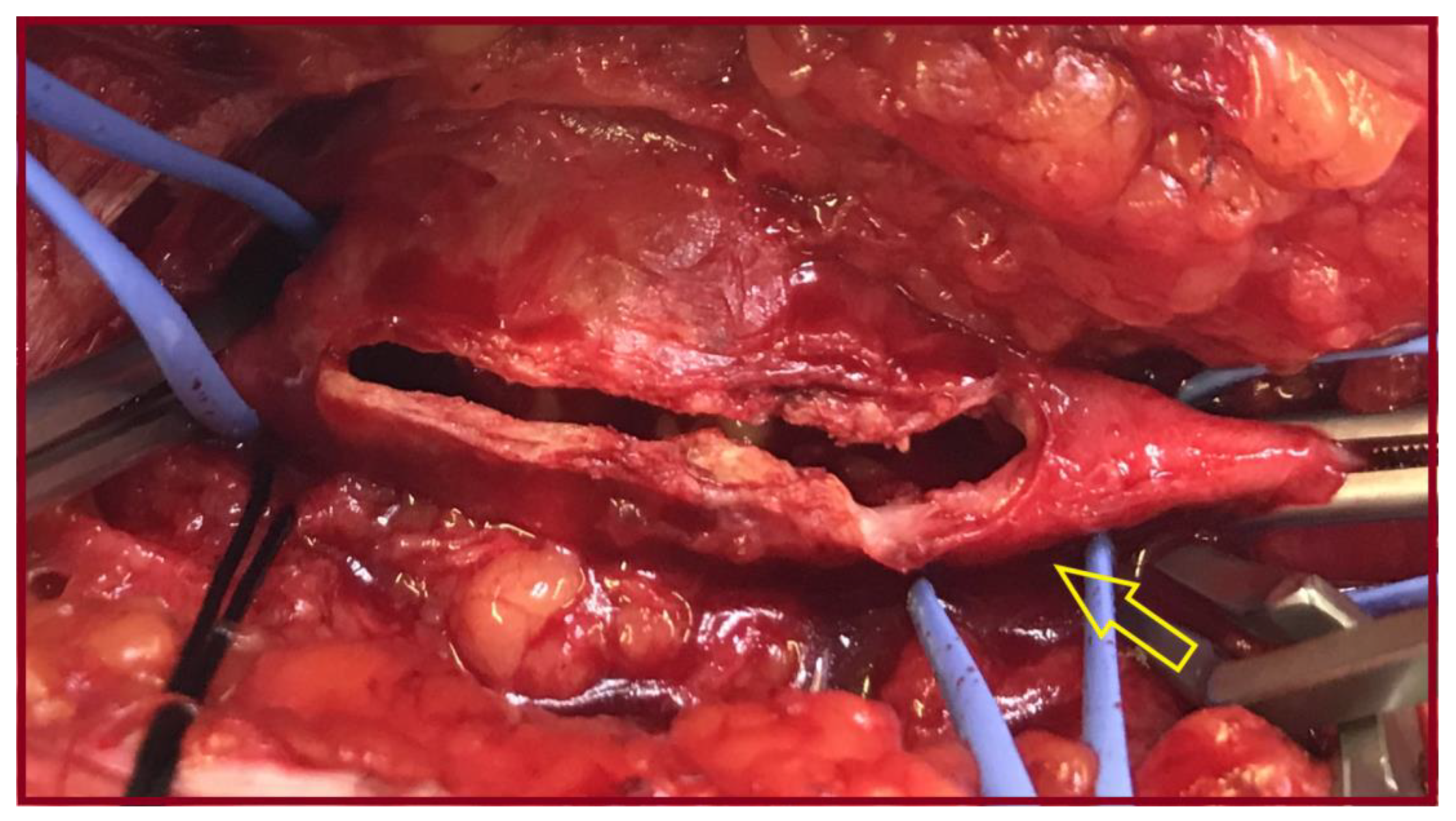
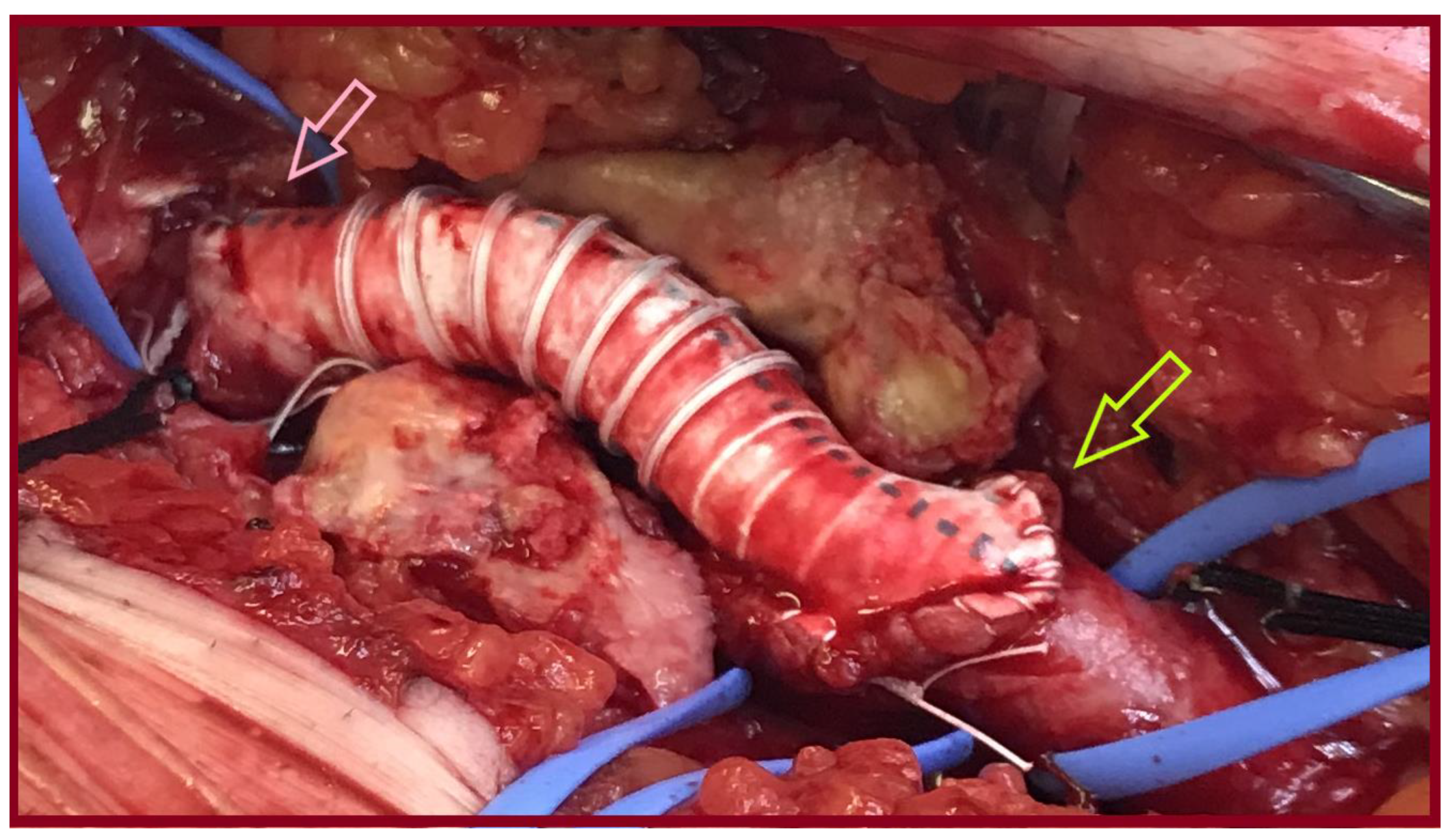
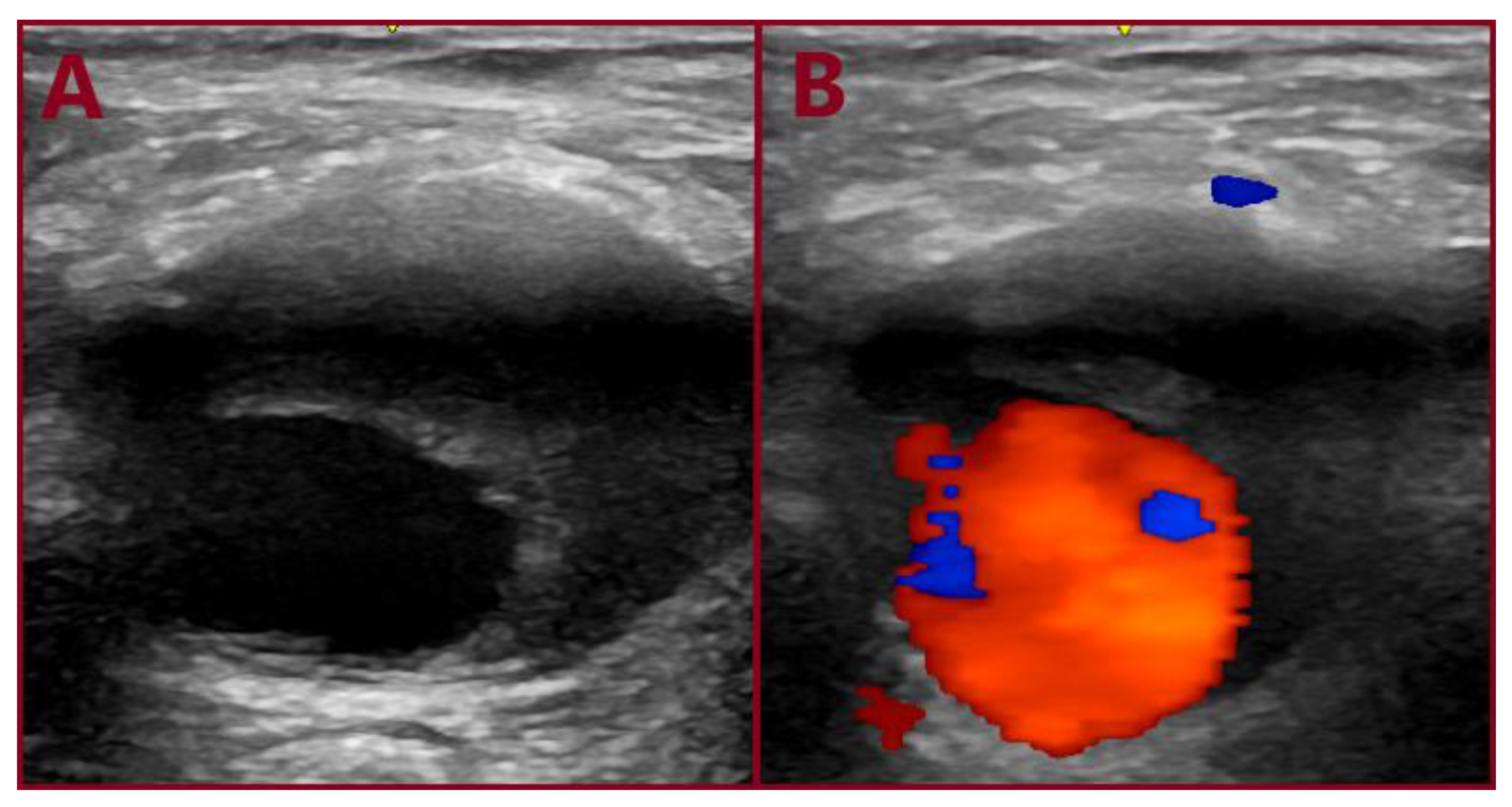
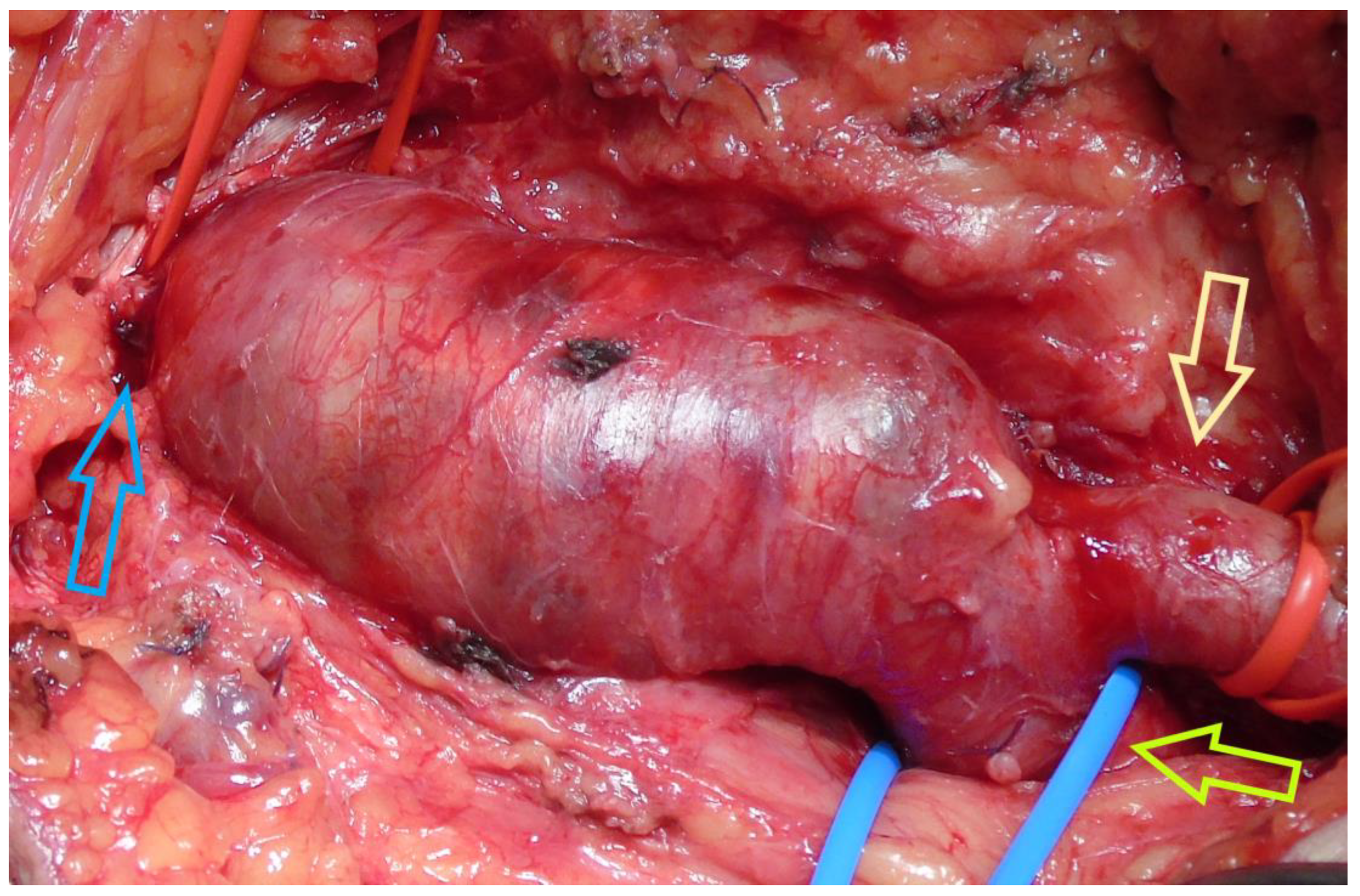
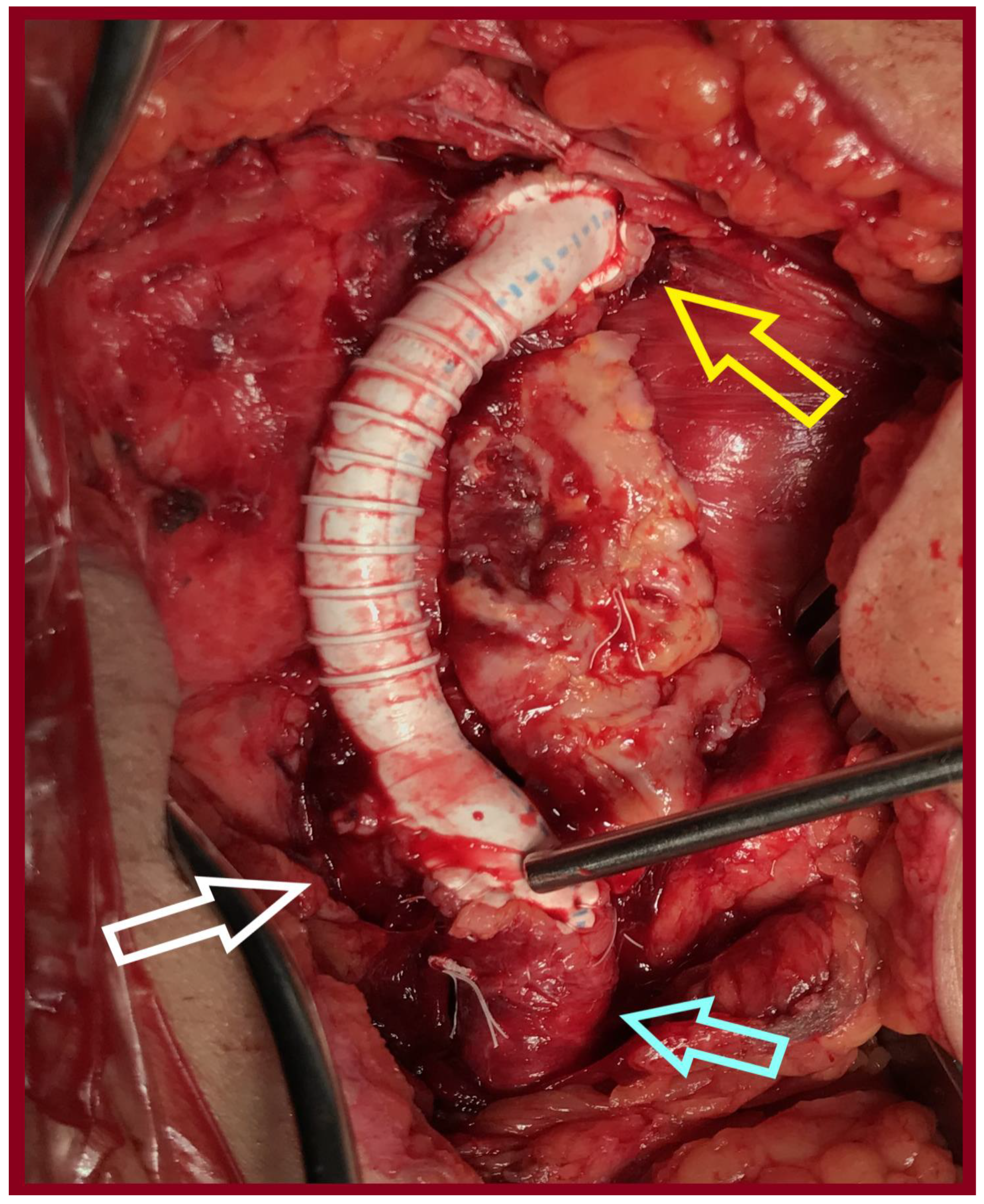
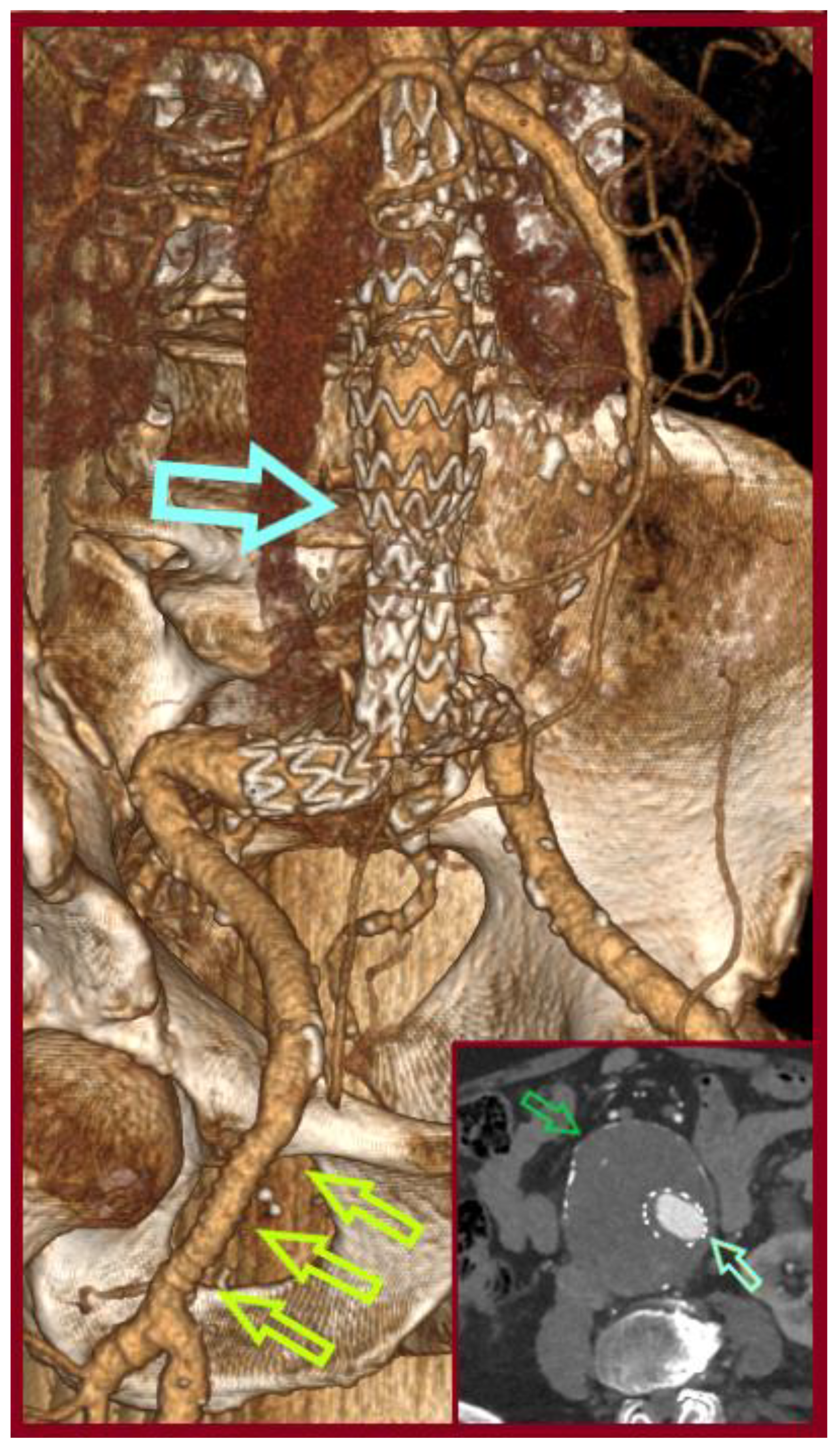
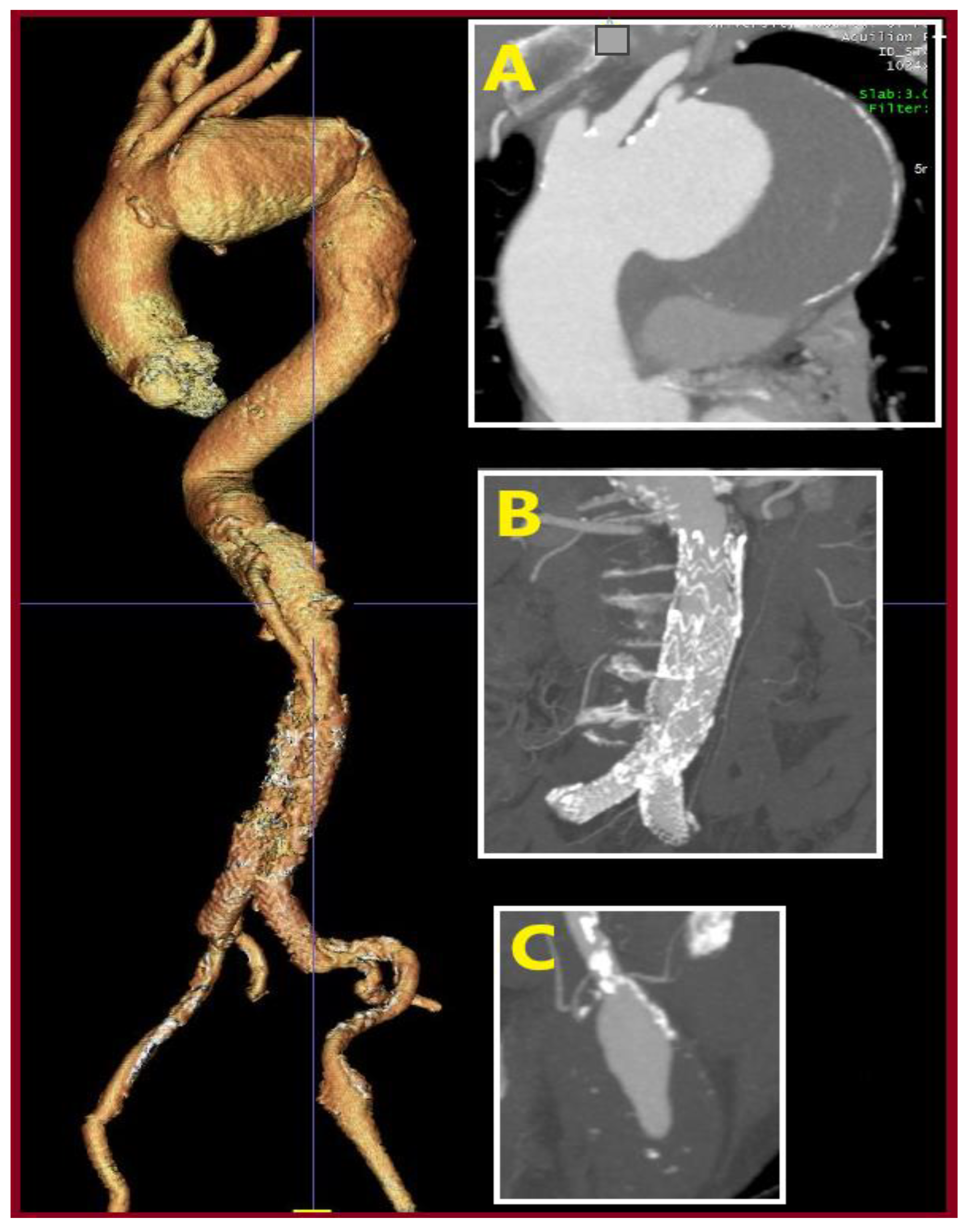
3.1. Case 1
3.2. Case 2
3.3. Case 3
4. Discussion and Literature Review
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sidawy, A.N.; Perler, B.A. Rutherford’s Vascular Surgery and Endovascular Therapy, 2-Volume Set, 10th ed.; Elsevier: Amsterdam, The Netherlands, 2022. [Google Scholar]
- Papageorgopoulou, C.; Nikolakopoulos, K.; Ntouvas, I.; Papadoulas, S.; Kritikos, N. A rare combination of tibial artery aneurysm and traumatic arteriovenous fistula: A case report. Pan Afr. Med. J. 2022, 42, 122. [Google Scholar] [CrossRef] [PubMed]
- Al Laham, O.; Shahrour, A.; Yahya, O.; Hamzeh, H. Successful surgical repair of an eminently rare case of an incidental idiopathic Common Femoral Artery Pseudoaneurysm in a 6-year-old female child—A Case Report. Int. J. Surg. Case Rep. 2022, 96, 107362. [Google Scholar] [CrossRef] [PubMed]
- Kakkos, S.K.; Tyllianakis, M.; Panagopoulos, A.; Kokkalis, Z.; Lianou, I.; Koletsis, E.; Tsolakis, I.; Papadoulas, S.; Gliatis, J.; Maroulis, I.; et al. Outcome Predictors in Civilian and Iatrogenic Arterial Trauma. World J. Surg. 2020, 45, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Dousdampanis, P.; Trigka, K.; Ntouvas, I.; Assimakopoulos, S.F.; Musso, C.G.; Papadoulas, S. Cramps during Hemodialysis: Are They Always Innocent? Saudi J. Kidney Dis. Transplant. 2019, 30, 985–988. [Google Scholar] [CrossRef]
- Hatrick, A.; Malcolm, P.; Burnand, K.; Irvine, A. A superficial femoral artery aneurysm in a patient with Marfan’s syndrome. Eur. J. Vasc. Endovasc. Surg. 1998, 15, 459–460. [Google Scholar] [CrossRef]
- Willems, S.A.; Buntinx, M.; Gelinck, L.B.; van Schaik, J.; Eefting, D. Ruptured Aneurysm of the Common Iliac Artery Caused by Brucella melitensis: A Case Report. EJVES Vasc. Forum 2021, 52, 26–29. [Google Scholar] [CrossRef]
- Fakhoury, E.; Oh, K.; Koudoumas, D.; Harris, L.M.; Dosluoglu, H.H.; Curl, R. Successful treatment of a ruptured profunda femoris artery aneurysm in association with fibromuscular dysplasia. J. Vasc. Surg. Cases Innov. Tech. 2019, 5, 485–487. [Google Scholar] [CrossRef]
- Bayram, M.; Duman, Z.M.; Devecioglu, E.G.; Timur, B. Giant Femoral Aneurysm in Giant Cell Arteritis. Indian J. Vasc. Endovasc. Surg. 2022, 9, 418–420. [Google Scholar] [CrossRef]
- Adityawati, A.A.D.; Kurnianingsih, N.; Satrijo, B.; Prasetya, I. Common Femoral Artery Aneurysm: A Challenging Diagnostic And Treatment Of A Rare Case. Hear. Sci. J. 2021, 2, 31–33. [Google Scholar] [CrossRef]
- Mazzolai, L.; Teixido-Tura, G.; Lanzi, S.; Boc, V.; Bossone, E.; Brodmann, M.; Bura-Rivière, A.; De Backer, J.; Deglise, S.; Della Corte, A.; et al. 2024 ESC Guidelines for the management of peripheral arterial and aortic diseases. Eur. Heart J. 2025, 26, 1e–169e. [Google Scholar] [CrossRef]
- Yahya, O.; Obaisy, M.M.; Al Laham, O.; Ghannam, M.; Mohammad, A. Arteriomegaly with synchronous true aneurysms; Management of Common Femoral Artery and Profunda Femoris Artery aneurysms in a 70-year-old male—A case report. Int. J. Surg. Case Rep. 2022, 94, 107161. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, T.; Kurosaka, M.; Sugimoto, T. A true aneurysm of the femoral artery in acromegaly. Clin. Imaging 2001, 25, 126–129. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.Y.; Min, S.K.; Kim, K.I.; Kim, H.Y. Intimal angiosarcoma presenting with common femoral artery aneurysm. J. Vasc. Surg. 2012, 56, 819–821. [Google Scholar] [CrossRef]
- Yanar, F.; Öner, G.; Yüksel, S.; Salduz, A.; Azamat, I.F.; Özçınar, B.; Bilgic, B.; Cömert, R.G.; Kozanoğlu, E.; Kurtoğlu, M. Femoral artery aneurysm developed on intimal sarcoma: Case report. Turk. J. Surg. 2022, 38, 306–311. [Google Scholar] [CrossRef]
- Sapienza, P. Femoral artery aneurysms: Long-term follow-up and results of surgical treatment. Cardiovasc. Surg. 1996, 4, 181–184. [Google Scholar] [CrossRef]
- Diaz, J.; Baeza, C.; González, A.; Torres, P.; Arribas, A.; Aparicio, C. Open Surgical Repair of Femoral Artery Aneurysm: Case Report. Clin Surg. 2020, 5, 2993. [Google Scholar]
- Wanhainen, A.; Van Herzeele, I.; Goncalves, F.B.; Montoya, S.B.; Berard, X.; Boyle, J.R.; D’oRia, M.; Prendes, C.F.; Karkos, C.D.; Kazimierczak, A.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2024 Clinical Practice Guidelines on the Management of Abdominal Aorto-Iliac Artery Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2024, 67, 192–331. [Google Scholar] [CrossRef]
- Diwan, A.; Sarkar, R.; Stanley, J.C.; Zelenock, G.B.; Wakefield, T.W. Incidence of femoral and popliteal artery aneurysms in patients with abdominal aortic aneurysms. J. Vasc. Surg. 2000, 31, 863–869. [Google Scholar] [CrossRef]
- Hotonu, S.A.; Johnson, C.H.N.; Kansal, N.; Bhattacharya, V. Common femoral artery aneurysm repair using bifurcated graft. BMJ Case Rep. 2018, 2018. [Google Scholar] [CrossRef]
- Saleem, T.; D’Cruz, J.R.; Baril, D.T. Femoral Aneurysm Repair. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 14 July 2023. [Google Scholar]
- Kennedy, R.E.; Hamilton, C.; Rahimi, S.; Ady, J. Simultaneous hybrid repair of symptomatic femoral, iliac, and abdominal aortic aneurysms. Vascular 2023, 32, 537–540. [Google Scholar] [CrossRef] [PubMed]
- Tsolakis, I.A.; Kakkos, S.K.; Papageorgopoulou, C.P.; Papadoulas, S.; Lampropoulos, G.; Fligou, F.; Nikolakopoulos, K.M.; Ntouvas, I.; Kouri, A. Predictors of Operative Mortality of 928 Intact Aortoiliac Aneurysms. Ann. Vasc. Surg. 2020, 71, 370–380. [Google Scholar] [CrossRef] [PubMed]
- Papadoulas, S.; Pitros, C.; Tsimpoukis, A.; Papageorgopoulou, C.; Prentza, S.; Leivaditis, V.; Antzoulas, A.; Mulita, F.; Moulakakis, K.G. Late post-EVAR abdominal aortic aneurysm rupture: A meta-analysis study. Arch. Med Sci. Atheroscler. Dis. 2024, 9, 152–164. [Google Scholar] [CrossRef] [PubMed]
- Corriere, M.A.; Guzman, R.J. True and False Aneurysms of the Femoral Artery. Semin. Vasc. Surg. 2005, 18, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Calligaro, K.D.; Balraj, P.; Moudgill, N.; Rao, A.; Dougherty, M.J.; Eisenberg, J. Results of polytetrafluoroethylene-covered nitinol stents crossing the inguinal ligament. J. Vasc. Surg. 2013, 57, 421–426. [Google Scholar] [CrossRef]
- Chaikof, E.L.; Dalman, R.L.; Eskandari, M.K.; Jackson, B.M.; Lee, W.A.; Mansour, M.A.; Mastracci, T.M.; Mell, M.; Murad, M.H.; Nguyen, L.L.; et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J. Vasc. Surg. 2018, 67, 2–77.e2. [Google Scholar] [CrossRef]
- Barmparessos, E.; Georgiou, P.; Tsimpoukis, A.; Pitros, C.; Papadoulas, S. Ruptured Degenerative Common Femoral Artery An-eurysm. Hell. J. Vasc. Endovasc. Surg. 2024, 6. [Google Scholar]
- Levi, N.; Schroeder, T. Arteriosclerotic femoral artery aneurysms. A short review. J. Cardiovasc. Surg. 1997, 38, 335–338. [Google Scholar]
- Dolapoglu, A.; Ertugay, S.; Posacioglu, H. Staged approach for surgical management of a true femoral artery aneurysm combined with bilateral iliac artery aneurysms. SAGE Open Med Case Rep. 2017, 5. [Google Scholar] [CrossRef]
- Lawrence, P.F.; Harlander-Locke, M.P.; Oderich, G.S.; Humphries, M.D.; Landry, G.J.; Ballard, J.L.; Abularrage, C.J. The current management of isolated degenerative femoral artery aneurysms is too aggressive for their natural history. J. Vasc. Surg. 2014, 59, 343–349. [Google Scholar] [CrossRef]
- Rancic, Z.; Pecoraro, F.; Pfammatter, T.; Mayer, D.; Veith, F.; Lachat, M. Less Invasive (Common) Femoral Artery Aneurysm Repair Using Endografts and Limited Dissection. Eur. J. Vasc. Endovasc. Surg. 2013, 45, 481–487. [Google Scholar] [CrossRef]
- Piffaretti, G.; Mariscalco, G.; Tozzi, M.; Rivolta, N.; Annoni, M.; Castelli, P. Twenty-year experience of femoral artery aneurysms. J. Vasc. Surg. 2011, 53, 1230–1236. [Google Scholar] [CrossRef] [PubMed]
- Papadoulas, S.; Ntouvas, I.; Nikolakopoulos, K.M.; Katsanos, K.; Kakkos, S.K. True aneurysm of profunda femoris artery. Chirurgia 2020, 32, 361. [Google Scholar] [CrossRef]
- Cutler, B.S.; Darling, R.C. Surgical management of arteriosclerotic femoral aneurysms. Surgery 1973, 74, 764–773. [Google Scholar] [PubMed]
- Vijayakumar, V.; Beeman, B. Endovascular repair of infrarenal abdominal aortic aneurysm combined with aneurysmectomy and interposition bypass for left common femoral artery aneurysm. BMJ Case Rep. 2024, 17, e261526. [Google Scholar] [CrossRef] [PubMed]
- Al-Faham, F.S.M.; Al-Hakkak, S.M.M.; Akpinar, M.B. Trauma-induced large true superficial femoral artery aneurysm: A case report. Ann. Med. Surg. 2020, 55, 234–237. [Google Scholar] [CrossRef]
- Graham, L.M.; Zelenock, G.B.; Whitehouse, W.M.; Erlandson, E.E.; Dent, T.L.; Lindenauer, S.M.; Stanley, J.C. Clinical Significance of Arteriosclerotic Femoral Artery Aneurysms. Arch. Surg. 1980, 115, 502–507. [Google Scholar] [CrossRef]
- Zenunaj, G.; Baldazzi, G.; Acciarri, P.; Gasbarro, V.; Cosacco, A.; Serra, R.; Traina, L. Treatment of true superficial femoral artery aneurysms: The 15-year experience of a single centre. Ind. Mark. Manag. 2024, 106, 425–431. [Google Scholar] [CrossRef]
- Tetsuya, N.; Satoshi, U.; Haruka, K. Ruptured common femoral artery aneurysm or abdominal aortic aneurysm? Case Rep. Surg. 2013. [Google Scholar] [CrossRef]
- Dávila, B.O.; Fresilli, M.; Fabio, M.O.; Diotallevi, N.; Marchetti, A.A.; Ippoliti, A. Critical Limb Ischaemia for Thrombosed Common Femoral Artery Aneurysm: A Successful Hybrid Treatment. Int. Arch. Vasc. Med. 2021, 4, 012. [Google Scholar] [CrossRef]
- Kibrik, P.; Arustamyan, M.; Stern, J.R.; Dua, A. A systematic review of the diagnosis, management, and outcomes of true profunda femoris artery aneurysm. J. Vasc. Surg. 2020, 71, 2145–2151. [Google Scholar] [CrossRef]
- Nakai, S.; Uchida, T.; Kuroda, Y.; Ohba, E.; Mizumoto, M.; Yamashita, A. Surgical repair of deep femoral artery aneurysm complicated by deep vein thrombosis and pulmonary embolism. J. Vasc. Surg. Cases Innov. Tech. 2021, 7, 408–410. [Google Scholar] [CrossRef] [PubMed]
- Baird, R.J.; Gurry, J.F.; Kellam, J.; Plume, S.K. Arteriosclerotic femoral artery aneurysms. Can. Med. Assoc. J. 1977, 117, 1306–1307. [Google Scholar] [PubMed]
- Fagge, C.H. Aneurysm of the Common Femoral Artery; Excision of Aneurysm and Common Femoral Vein. Proc. R. Soc. Med. 1908, 1, 232–233. [Google Scholar] [CrossRef] [PubMed]
- Lyazidi, Y.; Abissegue, Y.; Chtata, H.; Taberkant, M. Endovascular Treatment of 2 True Degenerative Aneurysms of Superficial Femoral Arteries. Ann. Vasc. Surg. 2015, 30, 307.e1–307.e5. [Google Scholar] [CrossRef]
- Mohan, I.V.; Stephen, M.S. Peripheral Arterial Aneurysms: Open or Endovascular Surgery? Prog. Cardiovasc. Dis. 2013, 56, 36–56. [Google Scholar] [CrossRef]
- Parsa, P.; Cantu, K.; Eidt, J.; Gable, D.; Pearl, G. Case Report: A Durable Open Repair of a Rare Profunda Aneurysm. Ann. Vasc. Surg. 2017, 44, 424.e7–424.e10. [Google Scholar] [CrossRef]
- Moriuchi, H.; Maeda, T.; Koide, M.; Kunii, Y.; Watanabe, K. Surgical, endovascular, and hybrid treatment of deep femoral artery aneurysm: Three case reports. Clin. Case Rep. 2023, 11, e7853. [Google Scholar] [CrossRef]
- Castelli, M.A.; Battú, C.C.; Lima, M.; Pfund, G.; de Luca, I.; Zaefferer, P. Total endovascular repair of a common femoral artery aneurysm with a bifurcated endograft through a single ipsilateral approach. J. Vasc. Surg. Cases Innov. Tech. 2024, 10, 101566. [Google Scholar] [CrossRef]
- Mufty, H.; Daenens, K.; Houthoofd, S.; Fourneau, I. Endovascular Treatment of Isolated Degenerative Superficial Femoral Artery Aneurysm. Ann. Vasc. Surg. 2018, 49, 311.e11–311.e14. [Google Scholar] [CrossRef]
- Azéma, L.; Davaine, J.M.; Guyomarch, B.; Chaillou, P.; Costargent, A.; Patra, P.; Gouëffic, Y. Endovascular Repair of Common Femoral Artery and Concomitant Arterial Lesions. Eur. J. Vasc. Endovasc. Surg. 2011, 41, 787–793. [Google Scholar] [CrossRef]
- Sokhal, B.S.; Ma, Y.; Rajagopalan, S. Femoral artery aneurysms. Br. J. Hosp. Med. 2022, 83, 1–10. [Google Scholar] [CrossRef]
- Kamal, D.M.; Mamalchi, S.B.A. A True Bilateral Superficial Femoral Artery Aneurysm: A Case Report. Cureus 2023, 15, e49599. [Google Scholar] [CrossRef]
- Mauritz, A.; Van Langenhove, K.; Van Wiemeersch, S.; Dedrye, L.; Verbrugghe, A.; Ceuppens, S. Two-staged repair of a giant iliac aneurysm and open repair of a true deep femoral artery aneurysm in Loeys-Dietz syndrome type V: A case report and review of literature. Acta Chir. Belg. 2024, 125, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Ratschiller, T.; Müller, H.; Schachner, T.; Fellner, F.; Sulzbacher, G.; Zierer, A. Femoral Artery Aneurysm Repair in a Patient With a Fibrillin-2 Mutation. Vasc. Endovasc. Surg. 2018, 52, 583–586. [Google Scholar] [CrossRef] [PubMed]
- Twine, C.P.; Wood, A.; Gordon, A.; Hill, S.; Whiston, R.; Williams, I.M. Incidence and Survival Outcome Following Femoral Artery Reconstruction During Endovascular Abdominal Aortic Aneurysm Repair. Vasc. Endovasc. Surg. 2011, 45, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Wolthuis, A.; Watkinson, A.; Kinsella, D.; Thompson, J. Complex iliac and bilateral common femoral artery aneurysms: A novel hybrid procedure. Surgery 2006, 4, 111–113. [Google Scholar] [CrossRef]
- Avraham, E.; Natour, M.; Obaid, W.; Karmeli, R. Superficial femoral artery access for endovascular aortic repair. J. Vasc. Surg. 2020, 71, 1538–1545. [Google Scholar] [CrossRef]
- Aaron, A.; El-Hag, S.; de Grandis, E.; Santilli, S.; Rosenberg, M.; Shafii, S.M.; Golzarian, J.; Faizer, R. The Superficial Femoral Artery: An Alternative Access for Percutaneous Endovascular Aneurysm Repair. Ann. Vasc. Surg. 2017, 38, 339–344. [Google Scholar] [CrossRef]
| Patient ID | Age/Sex | AAA/Size (cm) | CIAA Coexistence | CFAA Side/Size (cm) | AAA Treatment | CFAA Treatment | Order |
|---|---|---|---|---|---|---|---|
| Patient 1 | 76/M | Yes/5.5 | No | R/2.5 | Standard EVAR | Straight interposition grafting | First the AAA |
| Patient 2 | 77/M | Yes/8.3 | No | R/3 | Standard EVAR | Straight interposition grafting | First the AAA |
| Patient 3 | 62/M | Yes/5.5 | No | R/3.3 | Standard EVAR | Straight interposition grafting | First the AAA |
| Pt ID | Author/Ref | Year | Age/Sex | AAA/Size (cm) | CIAA/Side/Size (cm) | CFAA Side/Size (cm) | AAA Treatment | CIAA Treatment | CFAA Treatment | Order |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Wolthuis AM et al./[58] | Surgeon. 2006 | 74/M | No | Yes/R/3.2 | Bilate-Ral/R: 6 & L: 5 | Open interposition grafting for rupture, In the past | AUI (RIAA coiling, LCIA occluder) | Femoro-iliaco-femoral Y-bypass grafting | First the CIAA |
| 2 | Rancic Z et al./[32] | EJVES 2013 | 79/M | Yes/6.5 | No | NR/6.5 | Standard EVAR | - | Hybrid | First the AAA |
| 3 | Rancic Z et al./[32] | EJVES 2013 | 65/M | Yes/6 | No | NR/3.7 | Standard EVAR | - | Hybrid | First the AAA |
| 4 | Dolapoglu A et al./[30] | SAGE Open Med Case Rep 2017 | 67/M | No | Yes/Bilate-ral/NR | R/NR | - | Stented grafts–IIAs coiling (Conduit was used for access) | Bi-furcated inter-position grafting | First the CFAA |
| 5 | Vijayakumar V et al./[36] | BMJ Case Rep 2024 | 70/M | Yes/5.4 | No | L/2.4 | Standard EVAR | - | Straight inter- position grafting | First the AAA percutaneously |
| 6 | Kennedy RE et al./[22] | Vascular 2024 | 65/M | Yes/4.4 | Yes/Bilate-Ral/R: 2.8 & L: 2.7 | L/4.5 | Complex EVAR 1 | Complex EVAR 1 | Bi-furcated inter-position grafting | First the AAA & CIAAs |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Papadoulas, S.; Stathopoulou, M.; Tsimpoukis, A.; Papageorgopoulou, C.; Nikolakopoulos, K.; Krinos, N.; Skandali, A.; Zampakis, P.; Mustaqe, P.; Dogjani, A.; et al. Simultaneous Endovascular Abdominal Aortic Aneurysm Repair and Open Repair of Common Femoral Artery Aneurysm: Short Case Series and Current Review. J. Clin. Med. 2025, 14, 7988. https://doi.org/10.3390/jcm14227988
Papadoulas S, Stathopoulou M, Tsimpoukis A, Papageorgopoulou C, Nikolakopoulos K, Krinos N, Skandali A, Zampakis P, Mustaqe P, Dogjani A, et al. Simultaneous Endovascular Abdominal Aortic Aneurysm Repair and Open Repair of Common Femoral Artery Aneurysm: Short Case Series and Current Review. Journal of Clinical Medicine. 2025; 14(22):7988. https://doi.org/10.3390/jcm14227988
Chicago/Turabian StylePapadoulas, Spyros, Melina Stathopoulou, Andreas Tsimpoukis, Chrysanthi Papageorgopoulou, Konstantinos Nikolakopoulos, Nikolaos Krinos, Aliki Skandali, Petros Zampakis, Petraq Mustaqe, Agron Dogjani, and et al. 2025. "Simultaneous Endovascular Abdominal Aortic Aneurysm Repair and Open Repair of Common Femoral Artery Aneurysm: Short Case Series and Current Review" Journal of Clinical Medicine 14, no. 22: 7988. https://doi.org/10.3390/jcm14227988
APA StylePapadoulas, S., Stathopoulou, M., Tsimpoukis, A., Papageorgopoulou, C., Nikolakopoulos, K., Krinos, N., Skandali, A., Zampakis, P., Mustaqe, P., Dogjani, A., Mulita, F., & Leivaditis, V. (2025). Simultaneous Endovascular Abdominal Aortic Aneurysm Repair and Open Repair of Common Femoral Artery Aneurysm: Short Case Series and Current Review. Journal of Clinical Medicine, 14(22), 7988. https://doi.org/10.3390/jcm14227988








