1. Introduction
Falls are a leading cause of injury, disability, and loss of independence in older adults, with substantial effects on quality of life and healthcare use in rapidly aging regions, including the Middle East [
1,
2,
3]. The Otago Exercise Program (OEP) is a progressive strength and balance program that reduces falls and fall-related injuries and can be utilized for remote support, extending access where in-person services are constrained [
4,
5,
6,
7]. Telerehabilitation is a practical modality to scale evidence-based exercise for community-dwelling older adults [
8].
Successful telerehabilitation requires competent clinicians and supportive organizational and system factors. The American Physical Therapy Association (APTA) Telerehabilitation Clinical Practice Guideline (2024) emphasizes competency-based preparation, workflow and documentation standards, monitoring and safety, and outcome evaluation as prerequisites for safe and effective delivery in physical therapist practice [
9]. Complementing professional guidance, the World Health Organization (WHO) Package of Interventions for Rehabilitation (2023) specifies service-level requirements (workforce skills and assistive products/equipment) for prioritized interventions, and the WHO Global Strategy on Digital Health 2020–2025, together with Rehabilitation 2030, situates digital rehabilitation within broader health system strengthening in governance, interoperability, financing, and human resources [
10,
11,
12]. Collectively, these frameworks suggest that clinician training and educational exposure, rather than awareness alone, are likely levers for adoption.
To examine the determinants of clinician adoption, we applied the Unified Theory of Acceptance and Use of Technology (UTAUT). The UTAUT posits that adoption reflects Performance Expectancy (anticipated benefit), Effort Expectancy (perceived ease), Social Influence (norms), and Facilitating Conditions (training and infrastructure). In our dataset, the belief that telerehabilitation can effectively deliver the OEP operationalizes Performance Expectancy, and fall-prevention training plus educational background (degree earned outside vs. inside Saudi Arabia) approximate Facilitating Conditions. Familiarity with telerehabilitation is treated as a prior-exposure indicator rather than an Effort Expectancy proxy because ease-of-use items were not collected; Effort Expectancy and Social Influence are acknowledged gaps to be addressed prospectively.
A prior national work in Saudi Arabia established excellent internal consistency and test–retest reliability for the underlying survey and described therapists’ OEP knowledge and attitudes [
5]. However, the theory-aligned predictors of telerehabilitation-based OEP implementation have not been examined. It remains unclear whether familiarity translates into use or whether training and educational exposure more strongly shape belief and readiness to implement.
Guided by the UTAUT and consistent with the APTA and WHO implementation guidance, this study had three specific aims. First, we tested whether familiarity with telerehabilitation was associated with prior OEP prescriptions, examining whether exposure translates into use. Second, we identified predictors of belief in the efficacy of telerehabilitation for delivering the OEP, operationalizing the UTAUT’s Performance Expectancy construct. Third, we evaluated predictors of high readiness to implement remote fall prevention, defined as the conjunction of familiarity, adequate knowledge, and strong belief, serving as a behavioral-intention proxy. We hypothesized that specialized training and international educational exposure would independently predict both belief and readiness, while familiarity alone would not predict historical use.
2. Materials and Methods
2.1. Study Design and Data Source
We conducted a national, cross-sectional online survey of licensed physical therapists (PTs) practicing in Saudi Arabia between November 2023 and April 2024. The survey characterized the use of telerehabilitation to deliver the Otago Exercise Program (OEP) to older adults and identified the determinants of belief (perceived efficacy) and readiness to implement the OEP via telerehabilitation. Reporting followed the STROBE guidance for observational studies (checklist available on request). Sampling, instrument development, and model specifications were prespecified and are described below.
2.2. Participants and Recruitment
Eligible participants were licensed PTs practicing in Saudi Arabia. PT students, interns, and nonlicensed personnel were excluded. Recruitment used convenience channels, including professional associations and groups, departmental mailing lists, and social media. Denominator counts for outreach channels were unavailable; a response rate could not be calculated. Generalizability is therefore limited, and selection bias is possible, as noted in the Discussion. Demographic and professional characteristics are shown in
Table 1.
2.3. Instrument Development and Validation
The survey was adapted from a prior national work in Saudi Arabia that reported strong content and face validity and high reliability for the OEP and telerehabilitation items (knowledge Cronbach α ≈ 0.98; attitudes α ≈ 0.97; two-week test–retest ICC ≈ 0.92–0.93) [
5]. Before rollout, a four-member expert panel (geriatrics, digital health, rehabilitation) conducted a content review, and clinicians with ≥7 years of experience provided additional face validity feedback. A pilot study (
n = 30) confirmed reliability and usability. Instrument content and administration were identical in the pilot and main phases; data were pooled for analysis with a prespecified pilot-exclusion sensitivity (2.8). Scale development and reliability followed health-measurement best practices [
13,
14].
The instrument included the following: Section A, demographic/professional characteristics (14 items); Section B, OEP knowledge (15 items); and Section C, attitudes toward the OEP and telerehabilitation (13 Likert-type items; 1 = strongly disagree to 5 = strongly agree, plus “not applicable”). Item wording is provided in the prior publication and the Supplement [
5].
2.4. Measures and UTAUT Operationalization
Determinants were structured using the UTAUT [
15].
2.4.1. Outcomes
The OEP prescription (use behavior): ever prescribed the OEP to older adults (yes/no).
Belief that telerehabilitation can effectively deliver the OEP (Performance Expectancy): single 5-point Likert item (higher = stronger belief), analyzed with ordinal logistic regression.
Readiness to implement the OEP via telerehabilitation (behavioral-intention proxy): binary composite (definition in 2.5).
2.4.2. Predictors and Covariates
Telerehabilitation familiarity (exposure indicator): familiar vs. not familiar (binary).
Fall-prevention training/certification (Facilitating Conditions): yes/no.
Educational background (Facilitating Conditions): highest degree earned outside vs. inside Saudi Arabia.
Practice context: sector/setting and region of practice.
Demographics: age group, sex, and years in practice (categorical).
2.4.3. UTAUT Mapping
In this dataset, belief operationalized Performance Expectancy, and training and educational background approximated Facilitating Conditions. Familiarity was treated as prior exposure (not an Effort Expectancy proxy) because ease-of-use items were not collected. Effort Expectancy and Social Influence were not measured and are identified as gaps for future work. Construct-to-variable mapping and coding are summarized in
Table 1 [
15].
2.4.4. UTAUT Operationalization
We used the UTAUT to structure determinants of telerehabilitation adoption. Performance Expectancy was represented by the 5-point belief item (“telerehabilitation can effectively deliver OEP”). Facilitating Conditions were approximated by fall-prevention training/certification, educational background (outside vs. inside Saudi Arabia), and practice context. Familiarity was treated as prior exposure. Effort Expectancy and Social Influence were not directly measured and are acknowledged as limitations (
Table 1).
Table 1.
UTAUT mapping.
| UTAUT Construct | Definition (Clinician Adoption) | Measured
Variable(s) | Coding/
Cut-Points | Model Role | Gap and Next-Step Measure |
|---|
| Performance Expectancy | Belief technology improves outcomes/efficiency | “Telerehabilitation can effectively deliver OEP” | Likert 1–5 (higher = stronger) | Outcome (belief); descriptive in readiness framing | Add outcome-expectancy items specific to tele-exercise |
| Effort Expectancy | Perceived ease of use | Not directly measured | — | — | Add usability/ease-of-use items (UTAUT-adapted/SUS-style) |
| Social Influence | Peer/leader endorsement | Not directly measured | — | — | Add supervisor/peer norms and patient preference items |
| Facilitating Conditions | Training/infrastructure/support enabling use | Fall-prevention training (Y/N); education outside vs. inside the KSA; sector/setting | Binary/categorical | Predictors (belief, readiness) | Add items on platform access, IT/helpdesk, reimbursement clarity |
| Behavioral Intention | Intention to use | Readiness composite (main: familiarity and knowledge ≥4 and belief ≥4) | Binary (ready vs. not) | Outcome (not used as a predictor) | Consider a separate intention scale with behavioral anchors |
| Use Behavior | Actual adoption | Prior OEP prescription (Y/N) | Binary | Outcome | Add frequency/intensity of OEP delivery; tele-only vs. hybrid |
| Exposure indicator (not UTAUT) | Prior exposure/experience | Familiarity with telerehabilitation | Binary | Covariate: predictor of use | Keep as exposure; avoid misclassifying as Effort Expectancy |
2.5. Readiness Definition and Rationale
“High telerehabilitation readiness” required the fulfillment of the following three criteria: (i) familiarity with telerehabilitation, (ii) knowledge ≥ 4/5, and (iii) belief ≥ 4/5. This conjunctive threshold reflects implementation practice, in which exposure and favorable appraisal are prerequisites for safe clinical deployment. To mitigate circularity, the primary readiness model excluded knowledge and belief as predictors (anti-tautology rule). As secondary, exploratory specifications, we evaluated models that included knowledge and belief and a “two-of-three” readiness threshold; qualitative inferences were unchanged.
2.6. Data Management and Missing Data
Data were screened for duplicates and implausible entries using time-stamp, IP, and email heuristics; none were identified. Item-level missingness was low. Analyses used complete-case data for each model. Model-specific sample sizes are reported in table footnotes. The prespecified category structure was retained. Instability due to sparse cells was addressed through penalized likelihood in sensitivity analyses and with cautious interpretation.
2.7. Statistical Analysis
All tests were two-sided with α = 0.05. Descriptive statistics summarized participant characteristics (
Table 2). The OEP use by familiarity was compared using Pearson χ
2 (degrees of freedom and exact
p reported;
Table 2 and
Figure 1).
2.7.2. Diagnostics and Fit
Multicollinearity was assessed using variance inflation factors (VIFs). In an extended readiness model that included belief, VIFs ranged from 1.13 to 1.72 (
Supplementary Table S2).
Goodness of fit was evaluated using the Akaike Information Criterion (AIC) and the Hosmer–Lemeshow test for logistic models; ordinal models reported the AIC and pseudo-R
2 [
17].
The proportional odds assumption was tested for ordinal models (Brant-type test). If violated, a partial proportional odds model was prespecified [
16,
18].
Where helpful, bootstrap 95% CIs (1000 resamples) are reported in the Supplement to illustrate the estimated precision in small-event settings [
19].
2.7.3. Software
We conducted analyses in Excel, SPSS version 27, and R version 4.4.2. Penalized likelihood logistic regression used Firth’s method [
20,
21].
2.8. Sensitivity Analyses (Small-Event Robustness)
Given that 21 participants met the readiness criterion, we prespecified two robustness checks: (1) Firth’s penalized logistic regression to reduce small-sample bias and address potential separation [
20,
21] and (2) pilot-exclusion analysis to re-estimate the readiness model after removing pilot respondents (n = 30; main-phase sample n = 87; readiness events n = 16). Both analyses used the same covariates as the primary readiness model and are summarized in
Supplementary Material S1, Table S1. As reported in the Results and Supplement, training and education outside Saudi Arabia remained statistically significant with directionally consistent magnitudes (for example, Firth: training OR = 3.74; university outside OR = 4.15; no-pilot: training OR = 4.85; university outside OR = 5.35), supporting robustness to small-event bias and pilot inclusion.
2.9. Ethical Considerations
The study complied with the Declaration of Helsinki and local regulations. Electronic informed consent was obtained from all participants before they were granted access to the survey. The Institutional Review Board of King Saud University approved the study protocol (KSU–HE–23–387; approval date: 11 April 2023). Only de-identified data were analyzed; anonymity was maintained throughout.
3. Results
3.1. Participant Characteristics
Among 120 licensed PTs surveyed nationwide, specialized fall-prevention training and international educational exposure emerged as independent predictors of readiness to implement remote fall-prevention programs. In contrast, familiarity with telerehabilitation alone did not predict prior use of the OEP. These key findings and supporting analyses are detailed below.
Participants were 57.5% male (
n = 69). Most were aged 25–34 years (60.0%,
n = 72), followed by 35–44 years (25.0%,
n = 30). By region, the Central area had the highest representation (46.7%,
n = 56), followed by Northern (19.2%,
n = 23). Highest qualifications were bachelor’s (49.2%), master’s (35.8%), PhD (11.7%), clinical doctorate (2.5%), and postgraduate diploma (0.8%). Overall, 28.3% of the participants (
n = 34) obtained their highest degree outside Saudi Arabia. Clinical experience was ≤5 years in 44.1%, 6–10 years in 25.0%, and ≥11 years in 30.8% of the participants. In total, 35.8% of the participants (
n = 43) reported fall-prevention training, 70.0% (
n = 84) reported familiarity with telerehabilitation, and 22.5% (
n = 27) had been prescribed the OEP (
Table 2).
Table 2.
Participant characteristics (N = 120).
Table 2.
Participant characteristics (N = 120).
| Characteristic | Category | n | % |
|---|
| Gender | Male | 69 | 57.5% |
| | Female | 51 | 42.5% |
| Age | <25 | 8 | 6.7% |
| | 25–34 | 72 | 60.0% |
| | 35–44 | 30 | 25.0% |
| | 45–54 | 9 | 7.5% |
| | 55–64 | 1 | 0.8% |
| Region | Central | 56 | 46.7% |
| | Northern | 23 | 19.2% |
| | Southern | 21 | 17.5% |
| | Western | 17 | 14.2% |
| | Eastern | 3 | 2.5% |
| Highest Qualification | Bachelor degree | 59 | 49.2% |
| | Master degree | 43 | 35.8% |
| | PhD | 14 | 11.7% |
| | Clinical doctorate | 3 | 2.5% |
| | Postgraduate diploma | 1 | 0.8% |
| University Location | University in Saudi Arabia | 86 | 71.7% |
| | University outside Saudi Arabia | 34 | 28.3% |
| Years of Clinical Experience | <2 years | 13 | 10.8% |
| | 2–5 years | 40 | 33.3% |
| | 6–10 years | 30 | 25.0% |
| | 11–15 years | 12 | 10.0% |
| | 16–20 years | 12 | 10.0% |
| | >20 years | 13 | 10.8% |
| Fall Prevention Training | No | 77 | 64.2% |
| | Yes | 43 | 35.8% |
| Familiar with Telerehab | No | 36 | 30.0% |
| | Yes | 84 | 70.0% |
| Previously Prescribed OEP | No | 93 | 77.5% |
| | Yes | 27 | 22.5% |
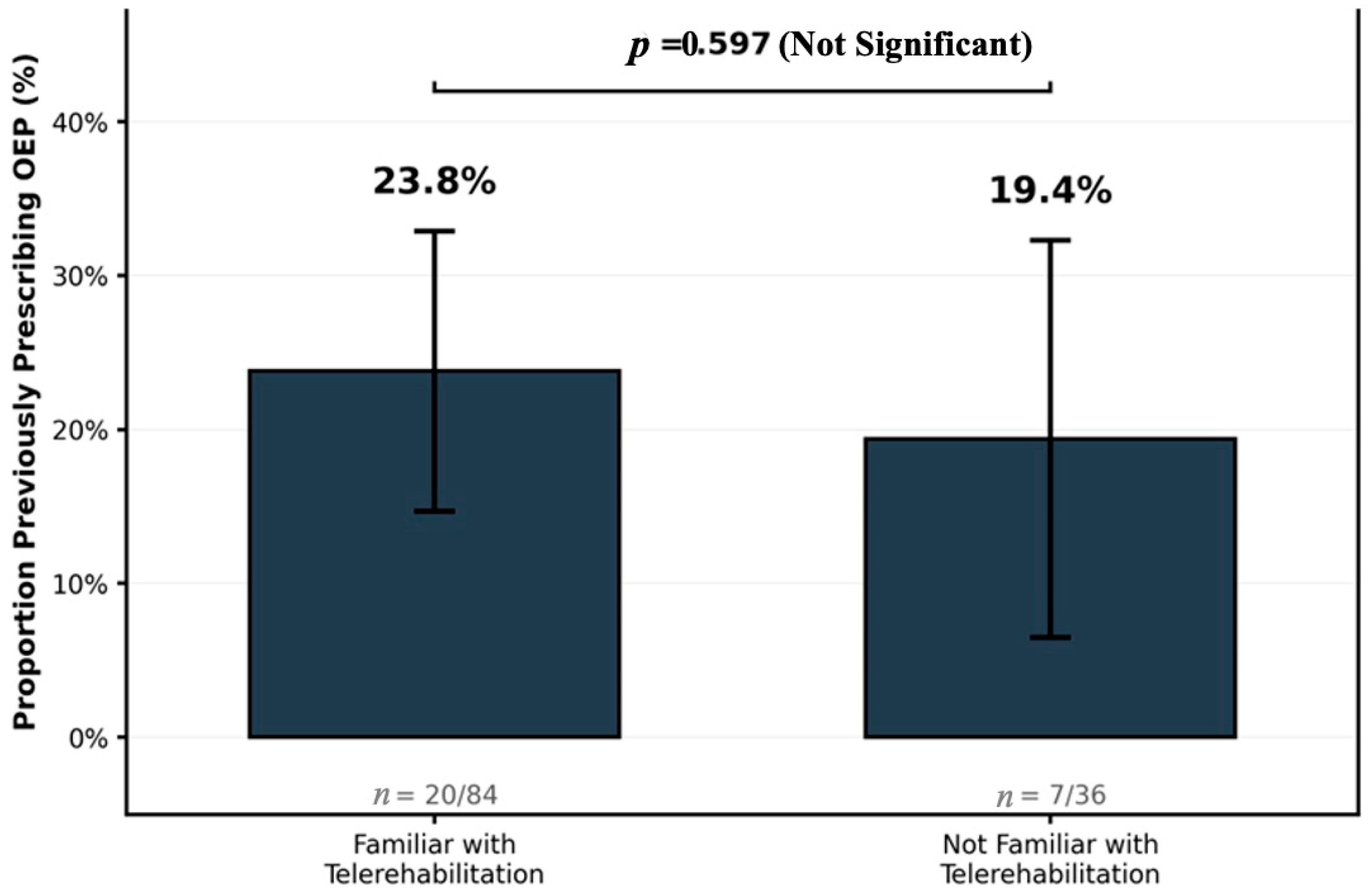
3.2. OEP Use by Telerehabilitation Familiarity
In the bivariate analysis, the OEP prescriptions did not differ by familiarity with telerehabilitation (
Table 3; χ
2(1) = 0.28;
p = 0.597). Among the participants familiar with telerehabilitation, 23.8% (20/84) had prescribed the OEP when compared with 19.4% (7/36) of participants unfamiliar with telerehabilitation.
Figure 1 shows this non-significant difference.
Figure 1.
Percentage of PTs who have prescribed the OEP, stratified by self-reported familiarity with telerehabilitation. Proportions are shown with counts. Difference not significant (χ
2(1) = 0.28;
p = 0.597). Note: Data correspond to
Table 3.
Figure 1.
Percentage of PTs who have prescribed the OEP, stratified by self-reported familiarity with telerehabilitation. Proportions are shown with counts. Difference not significant (χ
2(1) = 0.28;
p = 0.597). Note: Data correspond to
Table 3.
3.3. Predictors of Belief in Telerehabilitation Effectiveness (Ordinal Model)
Multivariable ordinal logistic regression (
n = 117 complete cases) examined predictors of belief that telerehabilitation can effectively deliver the OEP (Performance Expectancy). Fall-prevention training was associated with higher belief (odds ratio [OR] = 3.997; 95% CI = 1.568–10.184;
p = 0.004). Familiarity with telerehabilitation was not associated with belief (OR = 0.921; 95% CI = 0.410–2.068;
p = 0.841). Clinical experience (6–10 years; >10 years vs. <5 years) was not significant (
Table 4). These results indicate that formal training, rather than simple exposure, aligns with higher performance expectations for telerehabilitation in the OEP.
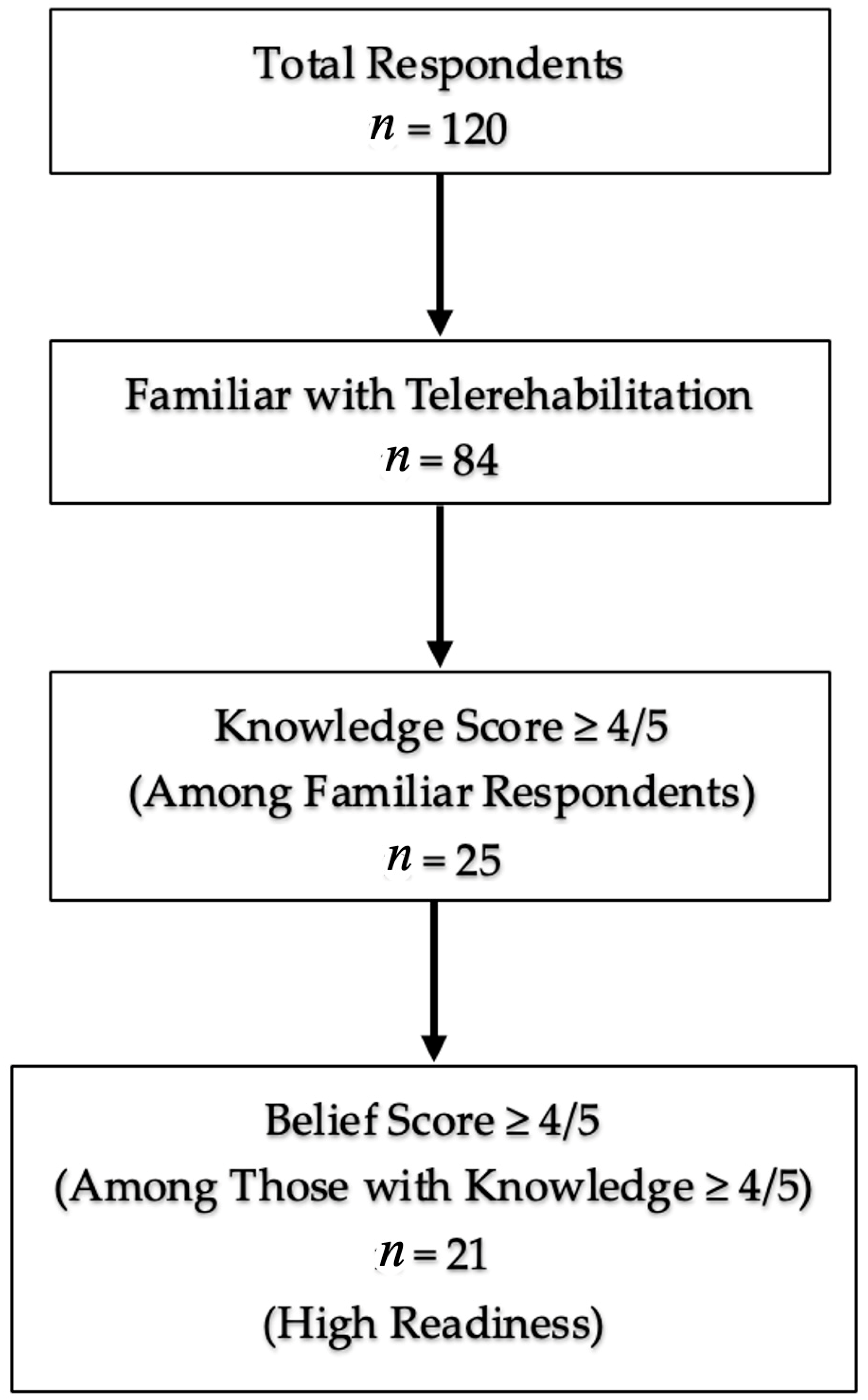
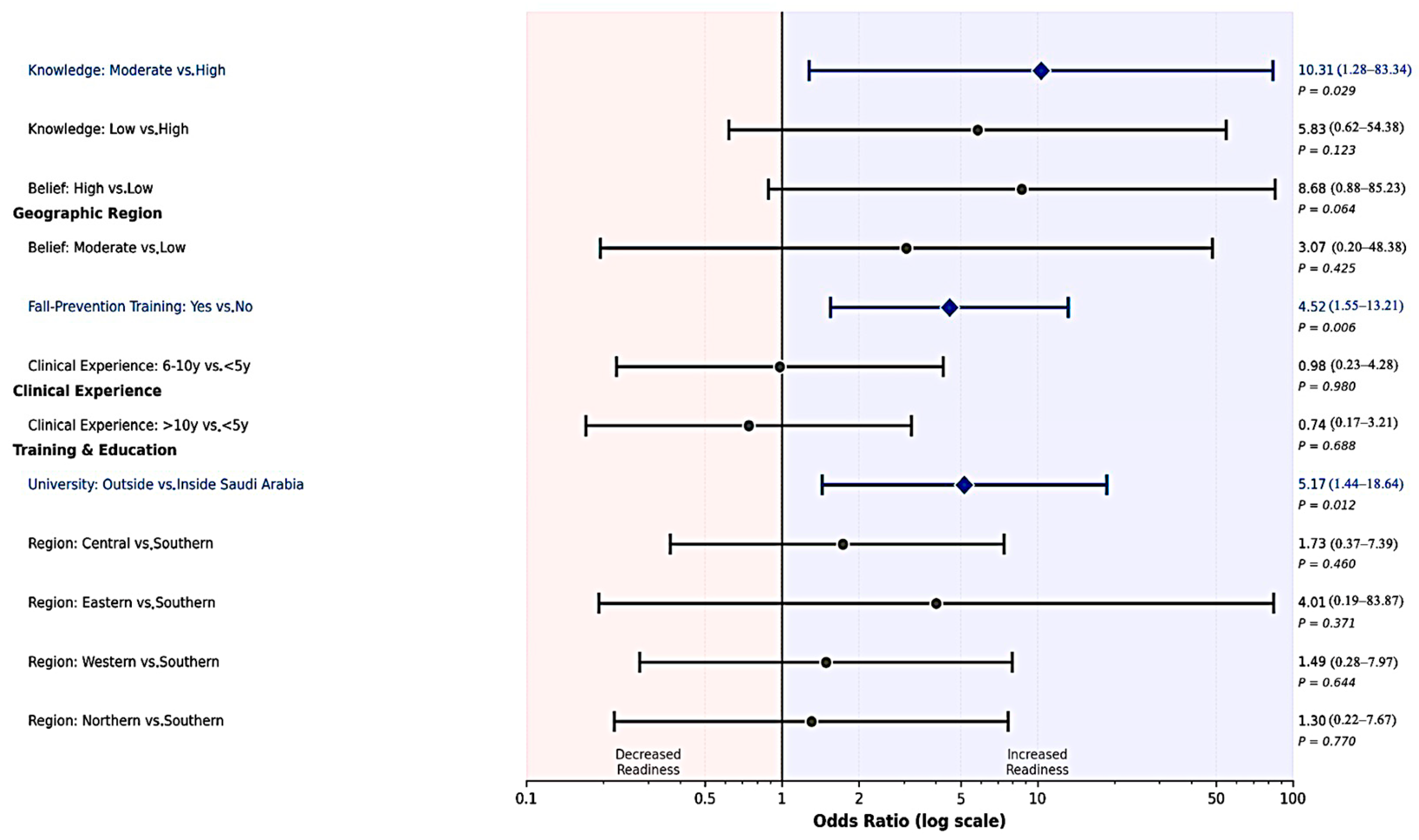
3.4. Predictors of High Telerehabilitation Readiness (Binary Model)
Readiness was defined a priori as familiarity with telerehabilitation, knowledge ≥ 4/5, and belief ≥ 4/5. In the primary multivariable logistic model (
n = 117; 21 “ready” events), fall-prevention training and education outside Saudi Arabia were independently associated with higher odds of readiness: training (OR = 4.520; 95% CI = 1.546–13.210;
p = 0.006) and university outside Saudi Arabia (OR = 5.170; 95% CI = 1.435–18.636;
p = 0.012). Compared with high knowledge, moderate knowledge was associated with higher readiness (OR = 10.309; 95% CI = 1.276–83.336;
p = 0.029), whereas low knowledge was not significant (OR = 5.829;
p = 0.123). Belief categories trended in the expected direction (e.g., high vs. low belief OR = 8.680;
p = 0.064), but were not significant with α = 0.05 in this specification; belief and knowledge contribute to the readiness definition and were handled to avoid tautology. Neither clinical experience nor region was associated with readiness (
Table 5).
3.5. Model Diagnostics, Multicollinearity, and Assumption Checks
Variance inflation factors (VIFs) were computed in an extended readiness model that included belief. VIFs ranged from 1.13 to 1.72 (highest for university outside vs. local = 1.72), indicating low multicollinearity (
Supplementary Table S2). Proportional odds testing supported the use of the ordinal specification for belief (test details available on request). Goodness of fit was assessed using the Akaike Information Criterion (AIC) and Hosmer–Lemeshow test for logistic models; ordinal models reported the AIC and pseudo-R
2 [
17]. Diagnostics were consistent with an acceptable fit given the small-event constraints. In accordance with STROBE, exact
p-values and 95% CIs are reported in
Table 3,
Table 4 and
Table 5, and model-specific sample sizes are stated.
3.6. Sensitivity Analyses for Small-Event Robustness
Two prespecified sensitivity analyses addressed the limited number of readiness events (
n = 21). First, Firth’s penalized logistic regression yielded attenuated but statistically significant estimates for training (OR = 3.74;
p = 0.010) and education outside Saudi Arabia (OR = 4.15;
p = 0.018). Second, pilot-exclusion analyses (main-phase sample only,
n = 87; 16 ready events) produced consistent associations: training (OR = 4.85;
p = 0.025) and university outside (OR = 5.35;
p = 0.037). These checks suggest that the primary findings are robust considering a small-sample bias and not driven by the pilot subgroup (
Supplementary Material S1, Table S1).
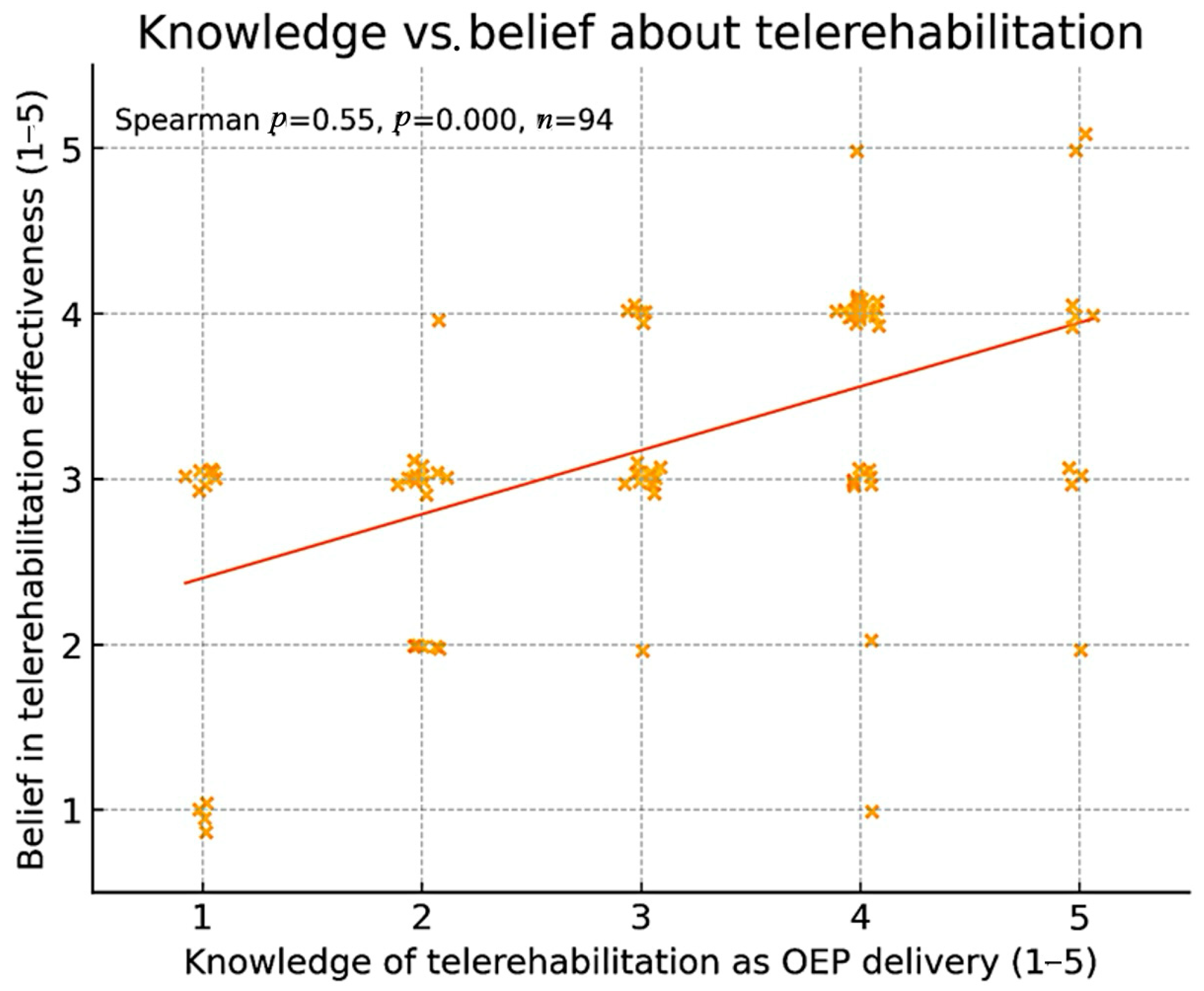
3.7. Ancillary and Figure-Based Findings
Exploratory correlation analysis showed a weak but statistically significant positive association between self-rated knowledge of telerehabilitation and belief in its effectiveness (Spearman ρ = 0.26;
p = 0.004), as depicted in
Figure 2.
Figure 3 shows the derivation of the high-readiness group (
n = 21) from the total sample (
n = 120) based on the predefined criteria (familiarity, knowledge, belief).
Figure 4 provides a visual summary of these multivariable associations, highlighting that fall-prevention training and education outside Saudi Arabia emerged as the strongest independent predictors of readiness.
3.8. Missing Data and Analytic Samples
Complete-case analyses for regression models yielded
n = 117, indicating minimal item-level missingness from the full sample of 120. Model-specific sample sizes are reported in table footnotes to facilitate reproducibility and appraisal of precision (
Table 3,
Table 4 and
Table 5).
4. Discussion
This study challenges the assumption that digital familiarity alone drives clinical adoption of telerehabilitation. Among licensed Saudi physical therapists, specialized fall-prevention training and international educational exposure, not simple awareness, predicted readiness to implement evidence-based remote fall prevention. These findings have direct implications for health system investments: awareness campaigns are unlikely to shift practice without competency-based training and curricular reform targeted to telerehabilitation skills.
In brief, (1) telerehabilitation familiarity was not associated with the OEP prescription in the bivariate analysis; (2) fall-prevention training was independently associated with stronger belief that the OEP can be delivered effectively via telerehabilitation; and (3) training and earning a highest degree outside Saudi Arabia were independently associated with higher odds of high readiness in multivariable models, with robust results obtained from Firth penalization and pilot-exclusion sensitivity analyses.
Taken together, the results align with the implementation theory: competency and enabling conditions drive adoption more than exposure alone. They extend the Saudi literature on the OEP knowledge and attitudes by identifying theory-aligned determinants of intention to implement the OEP through digital modalities [
5].
4.1. Principal Findings in the Context of Existing Evidence
The null association between familiarity with telerehabilitation and OEP prescription (χ
2 = 0.28;
p = 0.597) challenges the assumption that awareness or exposure translates into use. Prior evidence across rehabilitation and broader health IT domains shows that passive familiarity is often insufficient to change behavior without structured training, workflow integration, and supportive organizational conditions. Clinical practice guidance from the APTA emphasizes competency-based preparation (technology setup, remote examination skills, safety monitoring, documentation, and outcome evaluation) as a prerequisite for safe and effective telerehabilitation, which includes the elements that extend beyond simple exposure [
22]. Our results are consistent with this guidance and its implication that readiness is built and not assumed [
9].
The association between fall-prevention training and increased belief in the effectiveness of telerehabilitation for the OEP is theoretically and empirically sound. The efficacy of OEP in reducing falls among community-dwelling older adults is well established in randomized trials and meta-analyses [
23,
24,
25,
26]. Clinicians who have completed structured training are more likely to understand intervention components, dosing, safety thresholds, and outcome tracking. These competencies likely enhance confidence that the OEP can be delivered remotely without compromising outcomes [
27]. Digital adaptations of the OEP have also demonstrated feasibility and safety for remote use among older adults [
5,
28].
At the system level, global policy frameworks integrate telerehabilitation within health system strengthening and highlight the importance of workforce capacity and structural supports. The WHO Package of Interventions for Rehabilitation specifies service-level requirements, including workforce skills and assistive products, for prioritized interventions [
10]. The WHO Global Strategy on Digital Health 2020–2025 and Rehabilitation 2030 situate digital care within governance, financing, interoperability, and human resources reform [
11,
12]. Our finding that training and educational context—rather than familiarity—predict readiness aligns with these frameworks’ focus on capacity building and conducive conditions [
29].
International educational exposure, independent of training, knowledge, and experience, as a predictor of readiness, suggests that curricula, clinical placements, and academic environments encountered abroad may foster durable digital-health competencies and an implementation mindset. Post-pandemic curricula in North America, Europe, and Australasia increasingly embed telehealth assessment, patient monitoring, and documentation [
30]. This observation is consistent with diffusion-of-innovation theories and implementation frameworks, such as CFIR, which emphasize individuals’ knowledge and beliefs, as well as the roles of inner setting (culture, learning climate) and outer setting (policy, payment) in adoption [
29].
4.2. Interpretation Through the UTAUT and CFIR Lenses
We prespecified the UTAUT as the organizing framework. In this dataset, the belief that telerehabilitation can effectively deliver the OEP operationalizes Performance Expectancy, and fall-prevention training and educational background approximate Facilitating Conditions [
31]. Effort Expectancy and Social Influence were not directly measured and are acknowledged gaps.
Within this framework, the data suggest that Facilitating Conditions may be proximal drivers of adoption: those with formal fall-prevention training and those educated outside Saudi Arabia—contexts in which digital-health competencies may be integrated into curricula—were more likely to report readiness. This pattern is consistent with the UTAUT’s premise that supportive conditions (training, resources, organizational support) enable users to translate expectations into behavior and with the APTA guideline’s emphasis on competency-based preparation [
15].
CFIR complements this view by emphasizing multilevel determinants. Even when individuals hold favorable beliefs, adoption may be hindered if inner-setting features (leadership engagement, learning climate, IT support, workflow) are not aligned with outer-setting factors (reimbursement for virtual visits, licensing, data privacy regulations) [
32]. This may explain why training predicted belief and readiness, whereas familiarity did not correlate with prescription behavior in the bivariate analysis. In short, exposure alone does not produce practice change; competency development, along with organizational and policy support, is required [
29].
4.3. Competence Versus Exposure: Why Familiarity Is Not Enough
The operational distinction between “familiarity” (prior exposure) and “training” (competence building) clarifies the mechanisms underlying our results. Familiarity may reduce anxiety or perceived effort—the elements akin to Effort Expectancy—but it does not confer protocol knowledge (exercise progression, contraindications), remote assessment skills (safety checks, camera positioning, validated performance measures), or proficiency with documentation and data security required for compliant telepractice. Structured training can provide these elements, close the knowledge-to-practice gap, and strengthen confidence in the fact that remote OEP delivery is safe and effective, hence increasing Performance Expectancy among trained clinicians. This interpretation aligns with telerehabilitation evidence syntheses, showing clinical equivalence or noninferiority to in-person delivery when programs are implemented with adequate preparation and support [
33].
Digital delivery of fall-prevention exercise is feasible and effective when adherence and progression are supported. StandingTall, a home-based eHealth balance exercise program, reduced falls among community-dwelling older adults in a large randomized trial, reinforcing the plausibility of remote strength and balance interventions for fall risk reduction [
34]. Such trials elevate, rather than diminish, the importance of clinician training to translate evidence into routine telepractice.
4.4. Educational Context and Readiness: Potential Mechanisms
The independent association between an international highest degree and readiness may reflect several mechanisms: curricular exposure to telehealth competencies; clinical placements involving hybrid or remote care; academic cultures emphasizing evidence-based practice, quality improvement, and interprofessional teamwork; and organizational matching, in which internationally educated therapists work in settings with stronger IT infrastructure and leadership support for digital care. Although our survey was not designed to test these pathways, the association remained significant after Firth penalization and after excluding pilot data, indicating a robust signal that merits qualitative follow-up and multilevel modeling [
9].
4.5. Methodological Considerations
A small number of “high readiness” events (
n = 21) limit precision and raise the risk of overfitting. We mitigated these concerns by prespecifying an exploratory interpretation, applying Firth’s penalized logistic regression to reduce small-sample bias and address quasi-separation (yielding attenuated yet significant odds ratios for training and international education), and conducting a pilot-exclusion sensitivity analysis with consistent results [
34]. VIFs were low (≈1.13–1.72) in the specification most prone to overlap (including belief), suggesting that multicollinearity is not a driver. These diagnostics support the reliability of the direction of associations, while wide confidence intervals underscore the need for replication to refine effect sizes [
29].
Our readiness definition—requiring familiarity > 4/5, knowledge ≥ 4/5, and belief ≥4/5—reflects a conservative implementation stance in which exposure and favorable appraisal are prerequisites for safe deployment. As knowledge and belief contribute to the outcome, we excluded them from the primary readiness model to avoid tautology; exploratory specifications that included them were labeled as hypothesis-generating. Future work should validate a readiness scale independent of these components (for example, behavioral-intention instruments or objective implementation behavior such as counts of OEP tele-prescriptions over time). The future UTAUT-based studies in this population should incorporate validated scales for the remaining original constructs, specifically Effort Expectancy and Social Influence, to provide a more complete model of technology adoption.
Convenience sampling and the absence of a response-rate denominator limit generalizability; respondents may be more academically engaged or more digitally inclined than the broader PT population. The cross-sectional design precludes causal inference. Self-reporting may introduce social desirability or recall bias. These limitations are common in early implementation studies [
35] and should be addressed in future research using probability sampling, longitudinal follow-up, and objective behavioral outcomes.
4.6. Implications for Practice, Education, and Policy
Awareness campaigns are insufficient to increase the implementation of OEP via telerehabilitation. Clinicians and service leaders should prioritize competency-based training aligned with the APTA telerehabilitation guidelines, covering remote assessment workflows, exercise progression and safety, documentation standards, emergency procedures, and outcome evaluation [
9]. Embedding mentored tele-sessions and simulation-based practice can accelerate skill acquisition and confidence. As self-reported readiness often fails to predict actual use, services should pair training with systematic audits of objective indicators (e.g., number of remote OEP initiations, adherence rates, and delivered dosage).
PT curricula at entry-to-practice and postgraduate levels should integrate digital-health competencies across the continuum, with explicit instruction in fall epidemiology, OEP dosing and progression, remote safety checks, and video-based performance measures. Capstone projects and clinical rotations that include remote delivery can normalize hybrid models early in professional formation. These directions align with WHO strategies that emphasize workforce capacity building as foundational for scaling digital health [
15].
Translating individual readiness into sustained practice requires organizational and policy infrastructure. Health system administrators should ensure secure, interoperable platforms; standardized documentation frameworks; reimbursement that recognizes remote fall-prevention services as billable encounters; and accessible technology with appropriate training for older adults and caregivers. The WHO PIR provides service-level resourcing guidance, and Rehabilitation 2030 underscores the intersectoral partnerships needed to extend access to underserved populations [
29].
Within the KSA, a prior national work established strong psychometric properties for instruments measuring the OEP knowledge and attitudes among PTs and provided baseline data on professional perspectives [
5]. This study identifies theory-driven predictors of belief in telerehabilitation efficacy and readiness to implement remote fall prevention, highlighting two actionable targets: specialized fall-prevention training and international educational exposure. Ministries of health and higher education, academic institutions, and professional licensing bodies can leverage these determinants to develop a digitally competent rehabilitation workforce capable of delivering safe, evidence-based telerehabilitation for fall prevention. As the KSA confronts the clinical and economic implications of rapid population aging, these findings offer direction for workforce strategies that expand equitable access to fall-prevention services through scalable digital care models.
4.7. Future Research
To address the implementation of remote occupational exercise programs (OEP) for older adults, it is crucial to conduct adequately powered prospective studies that follow physical therapists over time. These studies should aim to test sequence effects: targeted training increases beliefs, which in turn increase readiness, leading to the prescription of remote OEP and subsequent patient enrollment. To strengthen causal inferences, it is important to include objective implementation outcomes, such as the number of remote OEP initiations, adherence rates, and delivered dosages.
Furthermore, multilevel implementation evaluations guided by the Consolidated Framework for Implementation Research (CFIR) and the RE-AIM framework should be undertaken to identify both inner- and outer-setting determinants. Key factors to consider include leadership support, IT infrastructure, reimbursement policies, and the availability of digital-literacy resources for older adults. These evaluations will provide insights into how individual readiness translates into sustained practice change.
In addition, it is essential to assess the effectiveness and safety of tele-delivered OEP within real-world settings. This assessment should focus on patient-level metrics, including adherence to programs, falls and near-falls, balance measurements, and patient-reported outcomes. Pragmatic studies, such as StandingTall, demonstrate the potential of remote balance exercise programs, and similar trials in Saudi settings can further evaluate aspects of effectiveness, acceptability, and cost-effectiveness [
36].
Lastly, future studies utilizing the UTAUT in this population should incorporate validated scales for the remaining original constructs, specifically Effort Expectancy and Social Influence. This inclusion will help quantify their contributions to intention, Performance Expectancy, and overall readiness for engaging with the remote OEP.
5. Conclusions
Specialized fall-prevention training and international educational exposure—proxies for robust Facilitating Conditions—emerged as the key correlates of belief in telerehabilitation efficacy and readiness to implement the OEP among Saudi PTs. At the same time, familiarity alone did not predict use. These results, consonant with the APTA guidance and WHO system-level frameworks, highlight the need to move beyond the awareness of competency-based preparation and organizational enablement to scale evidence-based fall-prevention interventions. Health system leaders, educators, and professional societies should prioritize structured upskilling, curricular reform that embeds digital-health competencies, and policies that support safe, reimbursable remote care. Larger, longitudinal, and multilevel studies are warranted to refine effect sizes, clarify mechanisms, and ensure that clinician readiness translates into sustained adoption and improved outcomes for older adults at risk of falls.
Supplementary Materials
The following supporting information can be downloaded at
https://www.mdpi.com/article/10.3390/jcm14217838/s1, Table S1. Sensitivity analyses for the readiness outcome (high readiness vs. not). Table S2. Variance inflation factors (VIFs) for the extended readiness model.
Author Contributions
All authors contributed significantly to the study, including the design, execution, data acquisition, analysis, interpretation, drafting, revision, and critical review. All authors have read and agreed to the published version of the manuscript.
Funding
The authors would like to thank Ongoing Research Funding Program, (ORFFT-2025-115-1), King Saud University, Riyadh, Saudi Arabia for financial support.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and ethical approval was granted by the Institutional Review Board of King Saud University (KSU–HE–23–387; approval date: 11 April 2023).
Informed Consent Statement
Electronic informed consent was obtained from all participants prior to survey access. The article does not include any identifiable patient details or images; therefore, the MDPI patient consent for publication is not applicable.
Data Availability Statement
Data are available upon reasonable request to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| Abbreviation | Expansion |
| AIC | Akaike Information Criterion |
| APTA | American Physical Therapy Association |
| CFIR | Consolidated Framework for Implementation Research |
| CI | Confidence interval |
| DPT | Doctor of Physical Therapy |
| ICC | Intraclass correlation coefficient |
| IT | Information technology |
| KSA | Kingdom of Saudi Arabia |
| OEP | Otago Exercise Program |
| OR | Odds ratio |
| PIR | Package of Interventions for Rehabilitation |
| PhD | Doctor of Philosophy |
| PT | Physical therapy/physiotherapy |
| PTs | Physical therapists/physiotherapists |
| RE-AIM | Reach, Effectiveness, Adoption, Implementation, Maintenance |
| SPSS | Statistical Package for the Social Sciences |
| UTAUT | Unified Theory of Acceptance and Use of Technology |
| VIF | Variance inflation factor(s) |
| WHO | World Health Organization |
References
- Bindawas, S.M. The Changing Incidence and Prevalence of Falls and Its Disability Burden Among the Geriatric Population in Saudi Arabia from 1990 to 2019: A Longitudinal Analysis Using Global Burden of Disease Study Data. Cureus 2023, 15, e49117. [Google Scholar] [CrossRef]
- Chaabna, K.; Jithesh, A.; Khawaja, S.; Aboughanem, J.; Mamtani, R.; Cheema, S. The epidemiology of unintentional falls among older people in the Middle East and North Africa: A systematic review and meta-analysis. J. Glob. Health 2025, 15, 04072. [Google Scholar] [CrossRef]
- Alenazi, A.M.; Alanazi, M.F.; Elnaggar, R.K.; Alshehri, M.M.; Alqahtani, B.A.; Alhowimel, A.S.; Alhwoaimel, N.A.; Alanazi, A.D.; Alotaibi, M.A.; Almutairi, S.M.; et al. Prevalence and risk factors for falls among community-dwelling adults in Riyadh area. PeerJ 2023, 11, e16478. [Google Scholar] [CrossRef]
- Thomas, S.; Mackintosh, S.; Halbert, J. Does the ‘Otago exercise programme’ reduce mortality and falls in older adults?: A systematic review and meta-analysis. Age Ageing 2010, 39, 681–687. [Google Scholar] [CrossRef]
- Alsaleh, H.M.; Alsaad, S.M.; Alabdulwahab, S.S.; Vennu, V.; Bindawas, S.M. Fall Prevention in Older Adults: Insights from Saudi Arabian Physical Therapists on the Otago Exercise Program. Risk Manag. Heal. Policy 2024, 17, 2689–2703. [Google Scholar] [CrossRef]
- Dong, M.; Liu, X.; Choi, Y.; Li, N. Effects of Otago Exercise Program and aquatic exercise on fall risk in older adults: A systematic review. Arch. Gerontol. Geriatr. 2025, 132, 105799. [Google Scholar] [CrossRef] [PubMed]
- Cederbom, S.; Arkkukangas, M. Impact of the fall prevention Otago Exercise Programme on pain among community-dwelling older adults: A short- and long-term follow-up study. Clin. Interv. Aging 2019, 14, 721–726. [Google Scholar] [CrossRef]
- Alrwaily, M. Delivering Musculoskeletal Rehabilitation in the Digital Era: A Perspective on Clinical Strategies for Remote Practice. Healthcare 2025, 13, 2286. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.C.; Deutsch, J.E.; Holdsworth, L.; Kaplan, S.L.; Kosakowski, H.; Latz, R.; McNeary, L.L.; O’Neil, J.; Ronzio, O.; Sanders, K.; et al. Telerehabilitation in Physical Therapist Practice: A Clinical Practice Guideline From the American Physical Therapy Association. Phys. Ther. 2024, 104, pzae045. [Google Scholar] [CrossRef]
- WHO. Package of Interventions for Rehabilitation; Module 1: Introduction; World Health Organization: Geneva, Switzerland, 2023; pp. 1–22. [Google Scholar]
- WHO. Global Strategy on Digital Health 2020–2025; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Vaughn, S.; Cournan, M. World health organization rehabilitation 2030: Call to action update. Rehabil. Nurs. J. 2024, 49, 143–146. [Google Scholar] [CrossRef] [PubMed]
- Boateng, G.O.; Neilands, T.B.; Frongillo, E.A.; Melgar-Quinonez, H.R.; Young, S.L. Best Practices for Developing and Validating Scales for Health, Social, and Behavioral Research: A Primer. Front. Public Health 2018, 6, 149. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- McCullagh, P. Regression models for ordinal data. J. R. Stat. Soc. Ser. B 1980, 42, 109–127. [Google Scholar] [CrossRef]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression, 3rd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2013; pp. 1–396. [Google Scholar]
- Brant, R. Assessing proportionality in the proportional odds model for ordinal logistic regression. Biometrics 1990, 46, 1171–1178. [Google Scholar] [CrossRef] [PubMed]
- Efron, B.; Tibshirani, R.J. An Introduction to the Bootstrap, 1st ed.; Chapman and Hall/CRC: New York, NY, USA, 1994; pp. 1–436. [Google Scholar]
- Firth, D. Bias reduction of maximum likelihood estimates. Biometrika 1993, 80, 27–38. [Google Scholar] [CrossRef]
- Heinze, G.; Schemper, M. A solution to the problem of separation in logistic regression. Stat. Med. 2002, 21, 2409–2419. [Google Scholar] [CrossRef]
- Holland, A.E. Appraisal of Clinical Practice Guideline: Telerehabilitation in Physical Therapist Practice: A Clinical Practice Guideline From the American Physical Therapy Association. J. Physiother. 2024, 70, 317. [Google Scholar] [CrossRef]
- Sherrington, C.; Fairhall, N.; Wallbank, G.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S. Exercise for preventing falls in older people living in the community: An abridged Cochrane systematic review. Br. J. Sports Med. 2020, 54, 885–891. [Google Scholar] [CrossRef]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, 2012, CD007146. [Google Scholar] [CrossRef]
- He, Z.; Wu, H.; Zhao, G.; Zhang, Y.; Li, C.; Xing, Y.; Xu, A.; Yang, J.; Wang, R. The effectiveness of digital technology-based Otago Exercise Program on balance ability, muscle strength and fall efficacy in the elderly: A systematic review and meta-analysis. BMC Public Health 2025, 25, 71. [Google Scholar] [CrossRef]
- Wu, S.; Guo, Y.; Cao, Z.; Nan, J.; Zhang, Q.; Hu, M.; Ning, H.; Huang, W.; Xiao, L.D.; Feng, H. Effects of Otago exercise program on physical function in older adults: A systematic review and meta-analysis of randomized controlled trials. Arch. Gerontol. Geriatr. 2024, 124, 105470. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.J.; Robertson, M.C.; Gardner, M.M.; Norton, R.N.; Tilyard, M.W.; Buchner, D.M. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ 1997, 315, 1065–1069. [Google Scholar] [CrossRef]
- Ries, J.D.; Carroll, M. Feasibility of a Small Group Otago Exercise Program for Older Adults Living with Dementia. Geriatrics 2022, 7, 23. [Google Scholar] [CrossRef] [PubMed]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef]
- Michell, A.; Besomi, M.; Seron, P.; Voigt, M.; Cubillos, R.; Parada-Hernandez, F.; Urrejola, O.; Ferreira-Pacheco, T.B.; De Oliveira-Silva, D.; Bianca Aily, J.; et al. Implementation of physiotherapy telerehabilitation before and post COVID-19 outbreak: A comparative narrative between South American countries and Australia. Salud Publica Mex. 2022, 64, S31–S39. [Google Scholar] [CrossRef]
- Wang, M.Y.; Chen, H.; Gong, C.; Peng, X.M.; Zhong, Y.B.; Wu, C.M.; Luo, Y.; Wu, Y.Q. Understanding the use intention and influencing factors of telerehabilitation in people with rehabilitation needs: A cross-sectional survey. Front. Public Health 2023, 11, 1274080. [Google Scholar] [CrossRef]
- Reardon, C.M.; Damschroder, L.J.; Ashcraft, L.E.; Kerins, C.; Bachrach, R.L.; Nevedal, A.L.; Domlyn, A.M.; Dodge, J.; Chinman, M.; Rogal, S. The Consolidated Framework for Implementation Research (CFIR) User Guide: A five-step guide for conducting implementation research using the framework. Implement. Sci. 2025, 20, 39. [Google Scholar] [CrossRef]
- Cottrell, M.A.; Galea, O.A.; O’Leary, S.P.; Hill, A.J.; Russell, T.G. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: A systematic review and meta-analysis. Clin. Rehabil. 2017, 31, 625–638. [Google Scholar] [CrossRef]
- Heinze, G.; Ploner, M.; Dunkler, D.; Southworth, H. Firth’s bias reduced logistic regression. R Package Version 2013, 1, 33. Available online: https://cran.r-project.org/web/packages/logistf/logistf.pdf (accessed on 2 November 2025).
- Almojaibel, A.A. Development and Validation of the Saudi Telehealth Acceptance Scale Based on the Unified Theory of Acceptance and Use of Technology. Saudi J. Med. Med. Sci. 2024, 12, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Delbaere, K.; Valenzuela, T.; Lord, S.R.; Clemson, L.; Zijlstra, G.A.R.; Close, J.C.T.; Lung, T.; Woodbury, A.; Chow, J.; McInerney, G.; et al. E-health StandingTall balance exercise for fall prevention in older people: Results of a two year randomised controlled trial. BMJ 2021, 373, n740. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).