Refining the Clinical Pathway for Nasotracheal Intubation: An Updated Decision Making Algorithm
Abstract
1. Introduction
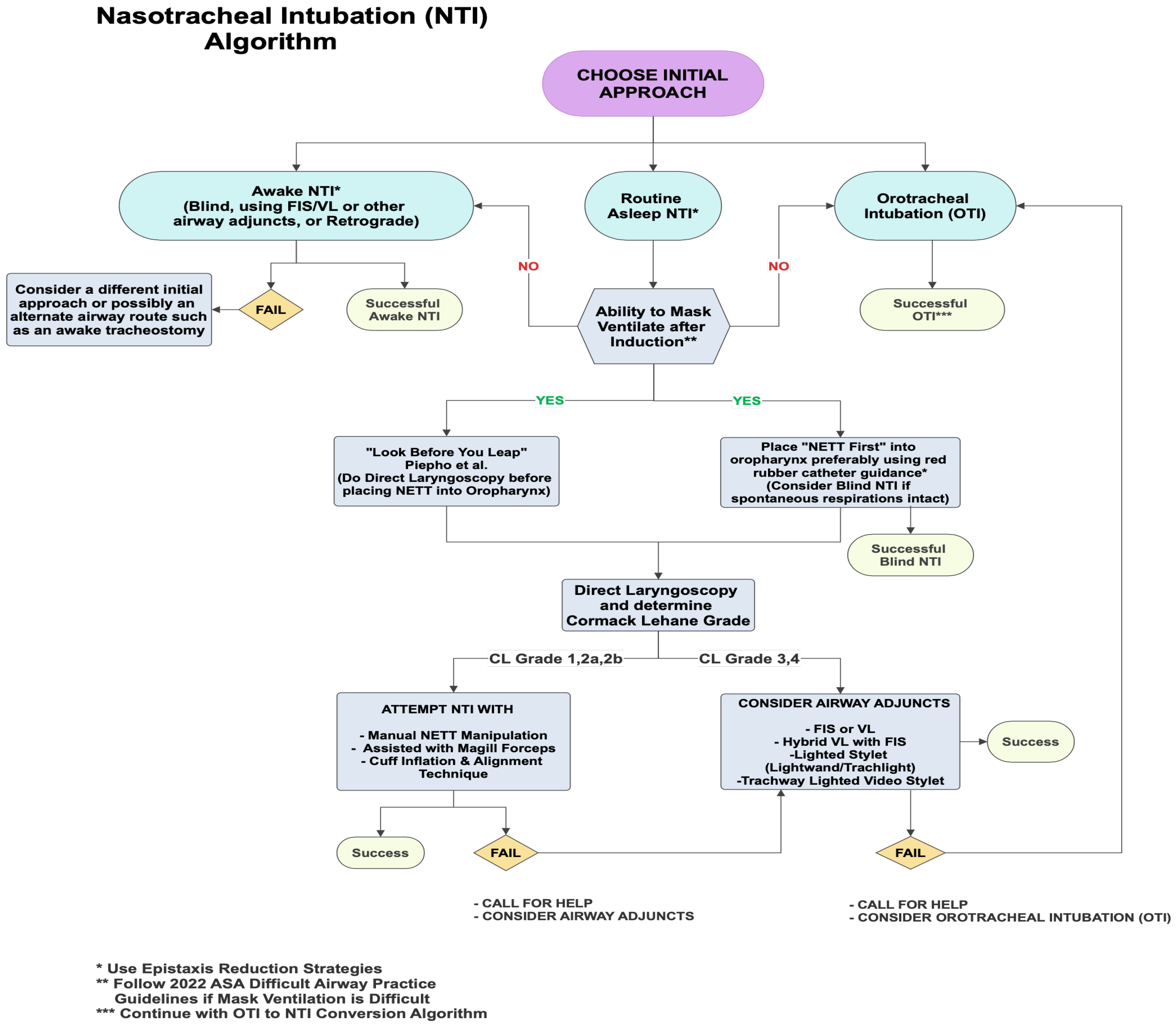
2. Choosing an Initial NTI Approach
2.1. Routine Asleep NTI (RNTI) Approach
- (1)
- Quickly attempting an OTI.
- (2)
- Placing a supraglottic airway (SGA).
- (3)
- Waking the patient up and attempting an awake NTI.
- (1)
- The “Look before you leap” option advocated by Piepho et al. [5] involves obtaining a glottic view with DL before placing the NETT into the oropharynx. Piepho et al. [5] recommended passing the NETT through the nares only in patients with a grade 1 or 2 Cormack–Lehane (CL) view and using alternate adjunct guided techniques otherwise [5]. Lesser experienced clinicians may find this approach more reassuring.
- (2)
- A more traditional option is placing the NETT into the oropharynx first (“NETT first”) before obtaining a glottic view with DL. The downside to this approach is that the clinician may occasionally encounter a difficult 3/4 CL grade during subsequent DL, making it challenging to advance the NETT situated in the oropharynx through the glottis. Albeit rare, there is also potential for severe epistaxis with initial NETT insertion, which may lead to aspiration of blood and render alternative options, such as FIS-assisted NTI, difficult [11]. Telescoping the NETT with a red rubber Robinson catheter, amongst other epistaxis reduction measures, is encouraged to reduce the possibility of severe epistaxis and help guide the NETT through the nasal pathway [12].
2.1.1. RNTI Scenario with CL Grade 1/2 View
2.1.2. RNTI Scenario with CL Grade 3/4 View
2.2. Awake NTI Approach
2.3. Initial Orotracheal Intubation (OTI) Approach
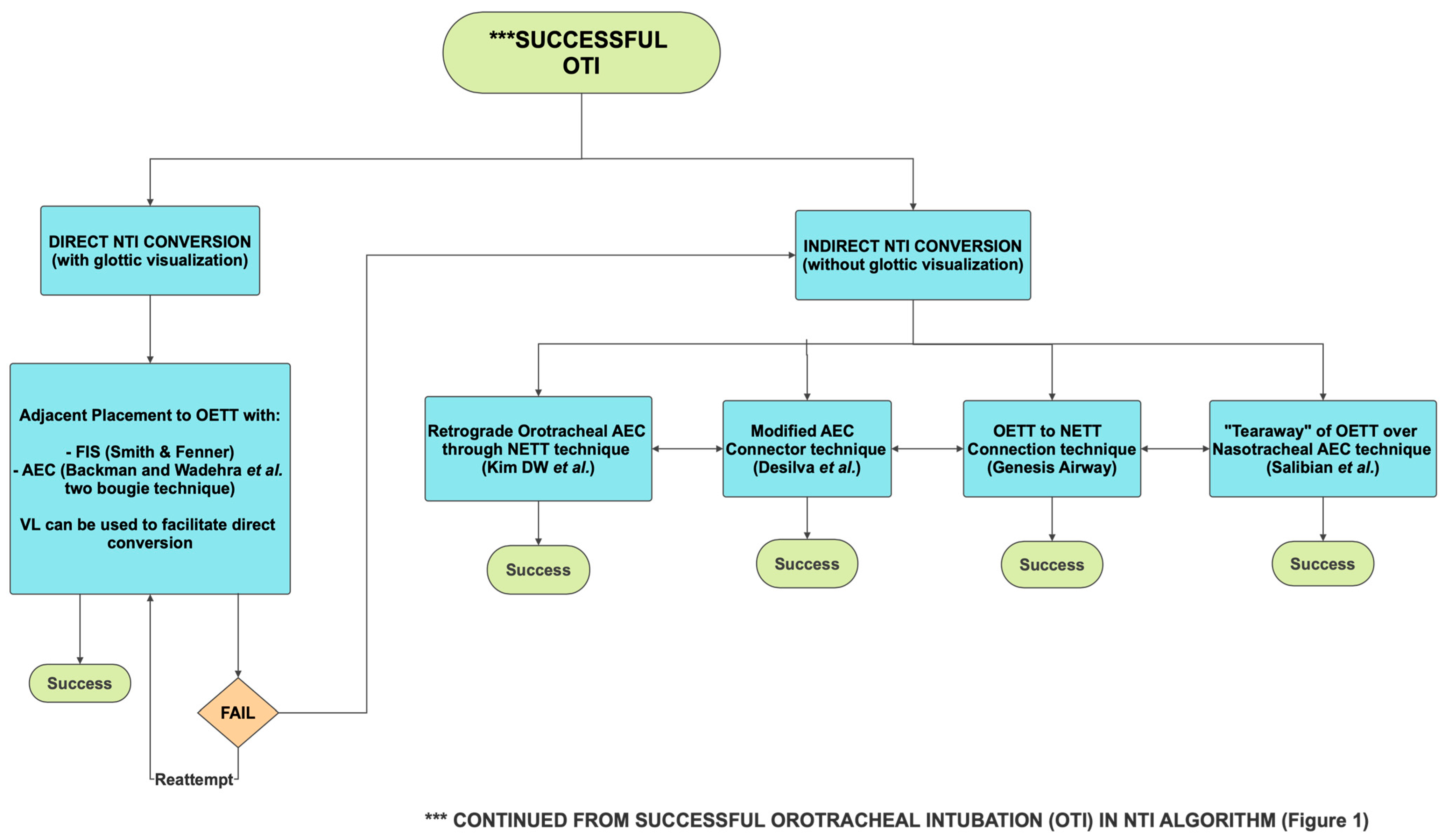
3. Orotracheal Intubation (OTI) to Nasotracheal Intubation (NTI) Conversion
3.1. Direct OTI to NTI Conversion with Glottic Visualization
3.2. Indirect OTI to NTI Conversion Without Glottic Visualization
4. Controlling Epistaxis
5. Conclusions
Methodology
Supplementary Materials
Funding
Acknowledgments
Conflicts of Interest
References
- Park, D.H.; Lee, C.A.; Jeong, C.Y.; Yang, H.S. Nasotracheal intubation for airway management during anesthesia. Anesth. Pain. Med. 2021, 16, 232–247. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.E.; Shutt, L.E. Nasotracheal intubation for head and neck surgery. Anaesthesia 2003, 58, 249–256. [Google Scholar] [CrossRef]
- Chauhan, V.; Acharya, G. Nasal intubation: A comprehensive review. Indian J. Crit. Care Med. 2016, 20, 662–667. [Google Scholar] [CrossRef]
- Yoo, H.; Choi, J.M.; Jo, J.Y.; Lee, S.; Jeong, S.M. Blind nasal intubation as an alternative to difficult intubation approaches. J. Dent. Anesth. Pain. Med. 2015, 15, 181–184. [Google Scholar] [CrossRef]
- Piepho, T.; Thierbach, A.; Werner, C. Nasotracheal intubation: Look before you leap. Br. J. Anaesth. 2005, 94, 859–860. [Google Scholar] [CrossRef]
- Backman, S.B.; Uria, M.; Kost, K.; Schricker, T. Case report: Nasotracheal intubation—Look before leaping to assess the laryngeal view. Can. J. Anaesth. 2008, 55, 302–305. [Google Scholar] [CrossRef]
- Prasanna, D.; Bhat, S. Nasotracheal Intubation: An Overview. J. Maxillofac. Oral. Surg. 2014, 13, 366–372. [Google Scholar] [CrossRef]
- Cincotta, F.A.; Neidorff, C. Blind awake nasotracheal intubation. Anesth. Prog. 1977, 24, 15–17. [Google Scholar] [PubMed Central]
- Dhasmana, S.; Singh, V.; Pal, U.S. Awake Blind Nasotracheal Intubation in Temporomandibular Joint Ankylosis Patients under Conscious Sedation Using Fentanyl and Midazolam. J. Maxillofac. Oral. Surg. 2010, 9, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Apfelbaum, J.L.; Hagberg, C.A.; Connis, R.T.; Abdelmalak, B.B.; Agarkar, M.; Dutton, R.P.; Fiadjoe, J.E.; Greif, R.; Klock, P.A.; Mercier, D.; et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology 2022, 136, 31–81. [Google Scholar] [CrossRef] [PubMed]
- Jeon, D.G.; Song, J.; Kim, S.K.; Ji, S.H. Massive Epistaxis during Nasotracheal Intubation. J. Korean Dent. Soc. Anesth. 2013, 13, 51–54. [Google Scholar] [CrossRef]
- Lera, S.; Machan, M.; Derefaka, G. A Safer Technique for Nasal Intubation: A Literature Review. Open J. Anesthesiol. 2017, 7, 275–285. [Google Scholar] [CrossRef]
- Nakamura, S.; Watanabe, T.; Hiroi, E.; Sasaki, T.; Matsumoto, N.; Hori, T. Cuff damage during naso-tracheal intubation for general anesthesia in oral surgery. Masui 1997, 46, 1508–1514. (In Japanese) [Google Scholar] [PubMed]
- Gorback, M.S. Inflation of the endotracheal tube cuff as an aid to blind nasal endotracheal intubation. Anesth. Analg. 1987, 66, 916–917. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Gupta, E.; Kumar, S.; Rani Sharma, K.; Rani Gupta, N. Cuff inflation-supplemented laryngoscope-guided nasal intubation: A comparison of three endotracheal tubes. Anesth. Analg. 2013, 116, 619–624. [Google Scholar] [CrossRef]
- Goodine, C.; Sparrow, K.; Asselin, M.; Hung, D.; Hung, O. The alignment approach to nasotracheal intubation. Can. J. Anaesth. 2016, 63, 991–992. [Google Scholar] [CrossRef]
- Choudhry, D.K.; Brenn, B.R.; Lutwin-Kawalec, M.; Sacks, K.; Nesargi, S.; He, Z. Effect of 90° counterclockwise rotation of the endotracheal tube on its advancement through the larynx during nasal fiberoptic intubation in children: A randomized and blinded study. Paediatr. Anaesth. 2016, 26, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Abrons, R.O.; Vansickle, R.A.; Ouanes, J.P. Seldinger technique for nasal intubation: A case series. J. Clin. Anesth. 2016, 34, 609–611. [Google Scholar] [CrossRef] [PubMed]
- Techanivate, A.; Kumwilaisak, K.; Worasawate, W.; Tanyong, A. Estimation of the proper length of nasotracheal intubation by Chula formula. J. Med. Assoc. Thai 2008, 91, 173–180. [Google Scholar] [PubMed]
- Whitten, C. Use of A Nasal Airway to Assist Ventilation During Fiberoptic Intubation. Airway Jedi. 2016. Available online: https://airwayjedi.com/2015/09/16/use-of-a-nasal-airway-to-assist-ventilation-during-fiberoptic-intubation/ (accessed on 30 September 2025).
- Mohammadzadeh, A.; Haghighi, M.; Naderi, B.; Chaudhry, A.; Khan, Z.H.; Rasouli, M.R.; Saadat, S. Comparison of two different methods of fiber-optic nasal intubation: Conventional method versus facilitated method (NASAL-18). Ups. J. Med. Sci. 2011, 116, 138–141. [Google Scholar] [CrossRef]
- Syal, R.; Parvez, M.; Kothari, N.; Abbas, H.; Kumar, R.; Singh, S.; Choudhary, G. Comparison of Conventional Technique versus Modified Tube First Technique of Awake Nasotracheal Fiber-optic Intubation: A Randomized Control Open-Label Trial. Anesth. Essays Res. 2020, 14, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Spinella, M.K.; Nathan, H.; Wilson, T.; Perez, D.E. A Reliable Protocol for Fiberoptic Nasal Intubation. J. Oral. Maxillofac. Surg. 2025, 83, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Ryoo, S.H.; Park, K.N.; Karm, M.H. The utilization of video laryngoscopy in nasotracheal intubation for oral and maxillofacial surgical procedures: A narrative review. J. Dent. Anesth. Pain. Med. 2024, 24, 1–17. [Google Scholar] [CrossRef]
- Tseng, K.Y.; Lu, I.C.; Shen, Y.C.; Lin, C.H.; Chen, P.N.; Cheng, K.I. A comparison of the video laryngoscopes with Macintosh laryngoscope for nasotracheal intubation. Asian J. Anesth. 2017, 55, 17–21. [Google Scholar] [CrossRef]
- Jiang, J.; Ma, D.X.; Li, B.; Wu, A.S.; Xue, F.S. Videolaryngoscopy versus direct laryngoscopy for nasotracheal intubation: A systematic review and meta-analysis of randomised controlled trials. J. Clin. Anesth. 2019, 52, 6–16. [Google Scholar] [CrossRef]
- Kwak, H.J.; Lee, S.Y.; Lee, S.Y.; Cho, S.H.; Kim, H.S.; Kim, J.Y. McGrath Video Laryngoscopy Facilitates Routine Nasotracheal Intubation in Patients Undergoing Oral and Maxillofacial Surgery: A Comparison with Macintosh Laryngoscopy. J. Oral. Maxillofac. Surg. 2016, 74, 256–261. [Google Scholar] [CrossRef]
- King, B.J.; Padnos, I.; Mancuso, K.; Christensen, B.J. Comparing Video and Direct Laryngoscopy for Nasotracheal Intubation. Anesth. Prog. 2020, 67, 193–199. [Google Scholar] [CrossRef]
- Votruba, J.; Michalek, P.; Brozek, T.; Bruthans, J. King Vision videolaryngoscope for nasal intubation in predicted difficult airway due to maxillofacial emergencies: A retrospective cohort study. Eur. J. Anaesthesiol. 2020, 37, 506–507. [Google Scholar] [CrossRef] [PubMed]
- Gupta, N.; Gupta, A.; Sarma, R.; Batra, A.; Madan, K. Video laryngoscopy vs. direct laryngoscopy for nasotracheal intubation in oromaxillofacial surgery: A systematic review and meta-analysis of randomized controlled trials. Korean J. Anesth. 2021, 74, 439–448. [Google Scholar] [CrossRef]
- Yeom, J.H.; Oh, M.K.; Shin, W.J.; Ahn, D.W.; Jeon, W.J.; Cho, S.Y. Randomized comparison of the effectiveness of nasal intubation using a GlideScope video laryngoscope with Magill forceps versus vascular forceps in patients with a normal airway. Can. J. Anaesth. 2017, 64, 1176–1181. [Google Scholar] [CrossRef] [PubMed]
- Kang, R.; Jeong, J.S.; Ko, J.S.; Ahn, J.; Gwak, M.S.; Choi, S.J.; Hwang, J.Y.; Hahm, T.S. Neutral Position Facilitates Nasotracheal Intubation with a GlideScope Video Laryngoscope: A Randomized Controlled Trial. J. Clin. Med. 2020, 9, 671. [Google Scholar] [CrossRef]
- Lin, C.H.; Tseng, K.Y.; Su, M.P.; Chuang, W.M.; Hu, P.Y.; Cheng, K.I. Cuff inflation technique is better than Magill forceps technique to facilitate nasotracheal intubation guiding by GlideScope® video laryngoscope. Kaohsiung J. Med. Sci. 2022, 38, 796–803. [Google Scholar] [CrossRef]
- Nedrud, S.M.; Baasch, D.G.; Cabral, J.D.; McEwen, D.S.; Dasika, J. Combined Video Laryngoscope and Fiberoptic Nasal Intubation. Cureus 2021, 13, e19482. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, R.E.; Gunning, M.D.G. Oral to nasal endotracheal tube exchange using both video and flexible laryngoscopes. South. Afr. J. Anesth. Analg. 2018, 24, 168–169. [Google Scholar] [CrossRef]
- Douglas, B.; Stacey, N.; Salam, S.; Jayanth, D. A hybrid nasal intubation technique for the head and neck surgical patient: A case series and review of the literature. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2021, 131, e38–e39. [Google Scholar]
- Dong, Y.; Li, G.; Wu, W.; Su, R.; Shao, Y. Lightwand-guided nasotracheal intubation in oromaxillofacial surgery patients with anticipated difficult airways: A comparison with blind nasal intubation. Int. J. Oral. Maxillofac. Surg. 2013, 42, 1049–1053. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.T.; Lin, C.H.; Tseng, K.Y.; Shen, Y.C.; Chen, C.H.; Chuang, W.M.; Cheng, K.I. Trachway in assistance of nasotracheal intubation with a preformed nasotracheal tube in patients undergoing oral maxillofacial surgery. Br. J. Anaesth. 2014, 113, 720–721. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Hu, R.; Wu, L.; Sun, P.; Zhang, Z. A comparison between the Disposcope endoscope and fibreoptic bronchoscope for nasotracheal intubation: A randomized controlled trial. BMC Anesth. 2019, 19, 163. [Google Scholar] [CrossRef] [PubMed]
- Morgan, J.P., 3rd; Haug, R.H.; Holmgreen, W.C. Awake blind nasoendotracheal intubation: A comprehensive review. J. Oral. Maxillofac. Surg. 1994, 52, 1303–1311. [Google Scholar] [CrossRef]
- Theresa, C.; Valente, J. Blind Nasotracheal Intubation Video. Available online: https://emedicine.medscape.com/article/1663655-technique?form=fpf#showall (accessed on 30 September 2025).
- Dyson, A.; Saunders, P.R.; Giesecke, A.H. Awake blind nasal intubation: Use of a simple whistle. Anaesthesia 1990, 45, 71–72. [Google Scholar] [CrossRef]
- King, H.K.; Wooten, J.D. Blind nasal intubation by monitoring end-tidal CO2. Anesth. Analg. 1989, 69, 412–413. [Google Scholar] [CrossRef] [PubMed]
- Asai, T. Use of the endotrol endotracheal tube and a light wand for blind nasotracheal intubation. Anesthesiology 1999, 91, 1557. [Google Scholar] [CrossRef]
- Tsukamoto, M.; Hitosugi, T.; Yokoyama, T. Awake fiberoptic nasotracheal intubation for patients with difficult airway. J. Dent. Anesth. Pain. Med. 2018, 18, 301–304. [Google Scholar] [CrossRef]
- Ahmad, I. NYSORA: Regional and Topical Anesthesia for Awake Endotracheal Intubation. Available online: https://www.nysora.com/techniques/head-and-neck-blocks/airway/regional-topical-anesthesia-awake-endotracheal-intubation/#toc (accessed on 30 September 2025).
- Liu, J.H.; Xue, F.S.; Liao, X.; Zhang, Y.M. Awake nasal intubation using a combination of the EndoFlex tube and fibreoptic bronchoscopy in patients with difficult airways. Acta Anaesthesiol. Scand. 2010, 54, 121–122. [Google Scholar] [CrossRef]
- Sharma, D.; Bithal, P.K.; Rath, G.P.; Pandia, M.P. Effect of orientation of a standard polyvinyl chloride tracheal tube on success rates during awake flexible fibreoptic intubation. Anaesthesia 2006, 61, 845–848. [Google Scholar] [CrossRef]
- Lomax, S.L.; Johnston, K.D.; Marfin, A.G.; Yentis, S.M.; Kathawaroo, S.; Popat, M.T. Nasotracheal fibreoptic intubation: A randomised controlled trial comparing the GlideRite® (Parker-Flex® Tip) nasal tracheal tube with a standard pre-rotated nasal RAE™ tracheal tube. Anaesthesia 2011, 66, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Meena, K.; Meena, R.K.; Palanisamy, D.; Deepesh Nayak, A.P. An innovative technique for nasotracheal fiberoptic intubation using SNPA and its comparison with conventional technique: RCT. Natl. J. Maxillofac. Surg. 2023, 14, 41–46. [Google Scholar] [CrossRef]
- Johnston, K.D.; Rai, M.R. Conscious sedation for awake fibreoptic intubation: A review of the literature. Can. J. Anaesth. 2013, 60, 584–599. [Google Scholar] [CrossRef] [PubMed]
- Kramer, A.; Müller, D.; Pförtner, R.; Mohr, C.; Groeben, H. Fibreoptic vs videolaryngoscopic (C-MAC® D-BLADE) nasal awake intubation under local anaesthesia. Anaesthesia 2015, 70, 400–406. [Google Scholar] [CrossRef]
- Gupta, N.; Garg, R.; Saini, S.; Kumar, V. GlideScope video laryngoscope-assisted nasotracheal intubation by cuff-inflation technique in head and neck cancer patients. Br. J. Anaesth. 2016, 116, 559–560. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A. Nasal Retrograde Intubation in Oromaxillofacial Surgery Patients with Limited Mouth Opening: A Cross-sectional Study. Int. J. Sci. Stud. 2018, 6, 57–61. [Google Scholar] [CrossRef]
- Vadepally, A.K.; Sinha, R.; Kumar, A.V.S.S.S. Retrograde intubation through nasal route in patients with limited mouth opening undergoing oral and maxillofacial surgery. J. Oral. Biol. Craniofac. Res. 2018, 8, 30–34. [Google Scholar] [CrossRef]
- Smith, J.E.; Fenner, S.G. Conversion of orotracheal to nasotracheal intubation with the aid of the fibreoptic laryngoscope. Anaesthesia 1993, 48, 1016. [Google Scholar] [CrossRef] [PubMed]
- Wadehra, A.; Tandon, M.S.; Ganjoo, P. A two-bougie technique for safer oro- to nasotracheal tube exchange in a difficult airway. Anaesthesia 2010, 65, 1231–1232. [Google Scholar] [CrossRef]
- Kim, D.W.; Kim, K.N.; Sun, J.E.; Lim, H.J. Conversion of an oral to nasal intubation in difficult nasal anatomy patients: Two case reports. BMC Anesth. 2021, 21, 72. [Google Scholar] [CrossRef]
- Desilva, M.; Maan, R.; Helwany, M.E.; Bhuller, A.S. Oral to Nasal Endotracheal Tube Exchange: Modification to Enable Wider Applicability of an “Old Connector” Technique—A Case Report. A A Pract. 2023, 17, e01703. [Google Scholar] [CrossRef]
- Salibian, H.; Jain, S.; Gabriel, D.; Azocar, R.J. Conversion of an oral to nasal orotracheal intubation using an endotracheal tube exchanger. Anesth. Analg. 2002, 95, 1822. [Google Scholar] [CrossRef] [PubMed]
- Genesis Airway Innovations. Available online: https://genesisairway.com/genesis-oral-nasal-endotracheal-tube-posterior-facing-bevel/ (accessed on 30 September 2025).
- Yogo, N.; Sasaki, T.; Kozumi, M.; Kinoshita, Y.; Muto, Y.; Hirai, K.; Yoshino, Y. Oral to nasal endotracheal tube exchange using tracheal tube guide and video laryngoscope in a pediatric patient with facial burns: A case report. Int. J. Emerg. Med. 2022, 15, 42. [Google Scholar] [CrossRef]
- Ji, S.; Song, J.; Kim, S.K.; Kim, M.Y.; Kim, S. Fiberoptic bronchoscope and C-MAC video laryngoscope assisted nasal-oral tube exchange: Two case reports. J. Dent. Anesth. Pain. Med. 2017, 17, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Gentry, W.B.; Shanks, C.A. Reevaluation of a maneuver to visualize the anterior larynx after intubation. Anesth. Analg. 1993, 77, 161–163. [Google Scholar] [CrossRef]
- Nakata, Y.; Niimi, Y. Oral-to-nasal endotracheal tube exchange in patients with bleeding esophageal varices. Anesthesiology 1995, 83, 1380–1381. [Google Scholar] [CrossRef]
- Sanuki, T.; Hirokane, M.; Matsuda, Y.; Sugioka, S.; Kotani, J. The Parker Flex-Tip tube for nasotracheal intubation: The influence on nasal mucosal trauma. Anaesthesia 2010, 65, 8–11. [Google Scholar] [CrossRef]
- Jafari, A.; Gharaei, B.; Kamranmanesh, M.R.; Aghamohammadi, H.; Nobahar, M.R.; Poorzamany, M.; Shahrabi, M.; Solhpour, A. Wire reinforced endotracheal tube compared with Parker Flex-Tip tube for oral fiberoptic intubation: A randomized clinical trial. Minerva Anestesiol. 2014, 80, 324–329. [Google Scholar] [PubMed]
- Vivian, V.H.; Anaes, D.; Pardon, T.L.; Van Zundert, A.A.J. Modified Retrograde Nasal Intubation: A New Airway Technique and Devices. Anesth. Prog. 2021, 68, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Dutta, A.; Chari, P.; Mohan, R.A.; Manhas, Y. Oral to nasal endotracheal tube exchange in a difficult airway: A novel method. Anesthesiology 2002, 97, 1324–1325. [Google Scholar] [CrossRef]
- De-Armendi, A.; Shukry, M.; Mayhew, J.F. Changing an oral endotracheal tube to a nasal tube in Pierre-Robin sequence. Paediatr. Anaesth. 2009, 19, 1240–1241. [Google Scholar] [CrossRef] [PubMed]
- Benumof, J.L.; Augoustides, J.G. Rigorously Maintaining a “Targeted Depth of Insertion” for an Airway Exchange Catheter During Tracheal Tube Exchange. J. Cardiothorac. Vasc. Anesth. 2019, 33, 3414–3415. [Google Scholar] [CrossRef]
- Inoue, S.; Fujimoto, Y.; Kawano, Y.; Furuya, H. Difficult passage of the endotracheal tube and massive nasal bleeding during awake nasal fiberoptic intubation in a patient with airway obstruction caused by neck hematoma—A case report. Middle East. J. Anaesthesiol. 2011, 21, 125–127. [Google Scholar] [PubMed]
- Sim, W.S.; Chung, I.S.; Chin, J.U.; Park, Y.S.; Cha, K.J.; Lee, S.C.; Kim, Y.C. Risk factors for epistaxis during nasotracheal intubation. Anaesth. Intensive Care 2002, 30, 449–452. [Google Scholar] [CrossRef]
- Lim, H.S.; Kim, D.; Lee, J.; Son, J.S.; Lee, J.R.; Ko, S. Reliability of assessment of nasal flow rate for nostril selection during nasotracheal intubation. J. Clin. Anesth. 2012, 24, 270–274. [Google Scholar] [CrossRef]
- Tong, J.L.; Tung, A. A Randomized Trial Comparing the Effect of Fiberoptic Selection and Guidance Versus Random Selection, Blind Insertion, and Direct Laryngoscopy, on the Incidence and Severity of Epistaxis After Nasotracheal Intubation. Anesth. Analg. 2018, 127, 485–489. [Google Scholar] [CrossRef]
- Thota, R.S.; Doctor, J.R. Evaluation of paranasal sinuses on available computed tomography in head and neck cancer patients: An assessment tool for nasotracheal intubation. Indian. J. Anaesth. 2016, 60, 960–961. [Google Scholar] [CrossRef]
- Tan, Y.L.; Wu, Z.H.; Zhao, B.J.; Ni, Y.H.; Dong, Y.C. For nasotracheal intubation, which nostril results in less epistaxis: Right or left?: A systematic review and meta-analysis. Eur. J. Anaesthesiol. 2021, 38, 1180–1186. [Google Scholar] [CrossRef]
- Boku, A.; Hanamoto, H.; Hirose, Y.; Kudo, C.; Morimoto, Y.; Sugimura, M.; Niwa, H. Which nostril should be used for nasotracheal intubation: The right or left? A randomized clinical trial. J. Clin. Anesth. 2014, 26, 390–394. [Google Scholar] [CrossRef]
- Sanuki, T.; Hirokane, M.; Kotani, J. Epistaxis during nasotracheal intubation: A comparison of nostril sides. J. Oral. Maxillofac. Surg. 2010, 68, 618–621. [Google Scholar] [CrossRef]
- Hung, K.C.; Chen, J.Y.; Ho, C.N.; Sun, C.K. The use of right nostril for nasotracheal intubation decreases the incidence of severe epistaxis: A small meta-analysis of randomized controlled trials. J. Clin. Anesth. 2021, 68, 110070. [Google Scholar] [CrossRef]
- Moore, D.C. Middle Turbinectomy: A Complication of IMPROPER Nasal Intubation? Anesthesiology 2000, 92, 1504. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Yu, J.; Kim, C.S.; Mun, T.; Jeong, W.S.; Choi, J.W.; Lee, K.; Kim, Y.K. Reverse tube direction and epistaxis in left nasotracheal intubation: A randomized controlled trial. Korean J. Anesth. 2024, 77, 596–604. [Google Scholar] [CrossRef] [PubMed]
- Won, D.; Kim, H.; Chang, J.E.; Lee, J.M.; Min, S.W.; Jung, J.; Yang, H.J.; Hwang, J.Y.; Kim, T.K. Effect of bevel direction on the tracheal tube pathway during nasotracheal intubation: A randomised trial. Eur. J. Anaesthesiol. 2021, 38, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Özkan, A.S.M.; Akbas, S.; Toy, E.; Durmus, M. North Polar Tube Reduces the Risk of Epistaxis during Nasotracheal Intubation: A prospective, Randomized Clinical Trial. Curr. Ther. Res. Clin. Exp. 2018, 90, 21–26. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, C.H.; Bahk, J.H.; Park, K.S. The influence of endotracheal tube tip design on nasal trauma during nasotracheal intubation: Magill-tip versus murphy-tip. Anesth. Analg. 2005, 101, 1226–1229. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.; Subar, P.; Witherell, H.; Ovodov, K.J. Reducing nasopharyngeal trauma: The urethral catheter-assisted nasotracheal intubation technique. Anesth. Prog. 2011, 58, 26–30. [Google Scholar] [CrossRef]
- Elwood, T.; Stillions, D.M.; Woo, D.W.; Bradford, H.M.; Ramamoorthy, C. Nasotracheal intubation: A randomized trial of two methods. Anesthesiology 2002, 96, 51–53. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.W.; Min, S.W.; Kim, C.S.; Chang, J.E.; Park, J.E.; Hwang, J.Y. The use of a nasogastric tube to facilitate nasotracheal intubation: A randomised controlled trial. Anaesthesia 2014, 69, 591–597. [Google Scholar] [CrossRef]
- Sasaki, R.; Koyasunaga, Y.; Agawa, K.; Watanabe, Y. Nasogastric Tube-guided Nasotracheal Intubation for Narrow Nasal Passage in Orthognathic Surgery. Plast. Reconstr. Surg. Glob. Open 2024, 12, e6130. [Google Scholar] [CrossRef]
- Bahk, J.H.; Ahn, W.S.; Lim, Y.J. Use of esophageal stethoscope as an introducer during nasotracheal intubation. Anesthesiology 2000, 92, 1503–1504. [Google Scholar] [CrossRef]
- Watt, S.; Pickhardt, D.; Lerman, J.; Armstrong, J.; Creighton, P.R.; Feldman, L. Telescoping tracheal tubes into catheters minimizes epistaxis during nasotracheal intubation in children. Anesthesiology 2007, 106, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.P.; Fang, X.; Chooah, O.; Albaqali, S.M.; Lin, W. Retropharyngeal internal carotid artery: A potential risk factor during nasotracheal intubation. Surg. Radiol. Anat. 2021, 43, 1769–1776. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, A.; Kawaraguchi, Y.; Fujita, M.; Goto, Y.; Shimokawa, M. Accidental retropharyngeal dissection extending close to the right common carotid artery during nasotracheal intubation: A case report. JA Clin. Rep. 2023, 9, 11. [Google Scholar] [CrossRef]
- Ahmed, M.E.; Refaie, B.M.; Abdelrahman, F.; Ragab, A.A. Pyriform sinus perforation during nasotracheal intubation: A case report. Int. J. Surg. Case Rep. 2020, 72, 351–354. [Google Scholar] [CrossRef]
- Thirion, C.; Abene, S.; Van Regemorter, V.; Van Boven, M.; Biermans, A.; Pharaoh, E.; Mestdagh, F. Cervicothoracic Emphysema After Nasotracheal Intubation Attempt: A Life-Threatening Complication—A Case Report. A A Pract. 2025, 19, e01884. [Google Scholar] [CrossRef] [PubMed]
- Enk, D.; Palmes, A.M.; Van Aken, H.; Westphal, M. Nasotracheal intubation: A simple and effective technique to reduce nasopharyngeal trauma and tube contamination. Anesth. Analg. 2002, 95, 1432–1436. [Google Scholar] [CrossRef] [PubMed]
- Ahmed-Nusrath, A.; Tong, J.L.; Smith, J.E. Pathways through the nose for nasal intubation: A comparison of three endotracheal tubes. Br. J. Anaesth. 2008, 100, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Lee, J.M.; Lee, J.; Hwang, J.Y.; Chang, J.E.; No, H.J.; Won, D.; Choi, S.; Min, S.W. Influence of Nasal Tip Lifting on the Incidence of the Tracheal Tube Pathway Passing Through the Nostril During Nasotracheal Intubation: A Randomized Controlled Trial. Anesth. Analg. 2018, 127, 1421–1426. [Google Scholar] [CrossRef]
- Katz, R.I.; Hovagim, A.R.; Finkelstein, H.S.; Grinberg, Y.; Boccio, R.V.; Poppers, P.J. A comparison of cocaine, lidocaine with epinephrine, and oxymetazoline for prevention of epistaxis on nasotracheal intubation. J. Clin. Anesth. 1990, 2, 16–20. [Google Scholar] [CrossRef]
- Dhakate, V.R.; Singam, A.P.; Bharadwaj, H.S. Evaluation of Nasopharyngeal Airway to Facilitate Nasotracheal Intubation. Ann. Maxillofac. Surg. 2020, 10, 57–60. [Google Scholar] [CrossRef]
- Canpolat, D.G.; Orbay, Y.S. Does a Nasal Airway Facilitate Nasotracheal Intubation or Not? A Prospective, Randomized, and Controlled Study. J. Oral. Maxillofac. Surg. 2021, 79, e1–e89. [Google Scholar] [CrossRef]
- Abd Al-Qader, B.K.; Abdulahad, S.A.; Mohammad, H.M. Nasotracheal intubation with the aid of nasopharyngeal airway. Anaesth. Pain Intensive Care 2024, 28, 50–54. [Google Scholar] [CrossRef]
- Kim, Y.C.; Lee, S.H.; Noh, G.J.; Cho, S.Y.; Yeom, J.H.; Shin, W.J.; Lee, D.H.; Ryu, J.S.; Park, Y.S.; Cha, K.J.; et al. Thermosoftening treatment of the nasotracheal tube before intubation can reduce epistaxis and nasal damage. Anesth. Analg. 2000, 91, 698–701. [Google Scholar] [CrossRef]
- Kim, E.M.; Chung, M.H.; Lee, M.H.; Choi, E.M.; Jun, I.J.; Yun, T.H.; Ko, Y.K.; Kim, J.H.; Jun, J.H. Is Tube Thermosoftening Helpful for Videolaryngoscope-Guided Nasotracheal Intubation?: A Randomized Controlled Trial. Anesth. Analg. 2019, 129, 812–818. [Google Scholar] [CrossRef]
- Seo, K.S.; Kim, J.H.; Yang, S.M.; Kim, H.J.; Bahk, J.H.; Yum, K.W. A new technique to reduce epistaxis and enhance navigability during nasotracheal intubation. Anesth. Analg. 2007, 105, 1420–1424. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Desilva, M.; Maan, R.; Helwany, M.; Shah, S.S. Refining the Clinical Pathway for Nasotracheal Intubation: An Updated Decision Making Algorithm. J. Clin. Med. 2025, 14, 7746. https://doi.org/10.3390/jcm14217746
Desilva M, Maan R, Helwany M, Shah SS. Refining the Clinical Pathway for Nasotracheal Intubation: An Updated Decision Making Algorithm. Journal of Clinical Medicine. 2025; 14(21):7746. https://doi.org/10.3390/jcm14217746
Chicago/Turabian StyleDesilva, Mahesh, Ramneek Maan, Muhammad Helwany, and Shalini S. Shah. 2025. "Refining the Clinical Pathway for Nasotracheal Intubation: An Updated Decision Making Algorithm" Journal of Clinical Medicine 14, no. 21: 7746. https://doi.org/10.3390/jcm14217746
APA StyleDesilva, M., Maan, R., Helwany, M., & Shah, S. S. (2025). Refining the Clinical Pathway for Nasotracheal Intubation: An Updated Decision Making Algorithm. Journal of Clinical Medicine, 14(21), 7746. https://doi.org/10.3390/jcm14217746





