Avoiding Hallux Sesamoidectomy: A Narrative Review
Abstract
1. Introduction
1.1. Sesamoidectomy
1.2. Extracorporeal Shockwave Therapy (ESWT) and Platelet-Rich Plasma (PRP)
1.3. Scope of This Article
2. ESWT and PRP for Sesamoid Pathologies
2.1. ESWT, PRP, and Related Therapies for Sesamoid Pathologies
2.2. ESWT and PRP for Foot Problems Similar to Sesamoid Pathologies
3. Surgeries for Sesamoid Pathologies
3.1. Surgeries for Sesamoid Fracture Nonunion
3.2. Surgeries for Plantar Keratosis
3.3. Surgeries for Sesamoiditis
3.4. Surgeries for AVN of the Sesamoid
4. Summary
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ADL | Activity of daily living |
| AOFAS | The American Orthopedic Foot & Ankle Society |
| AVN | Avascular necrosis |
| CBMA | Concentrated bone marrow aspirate |
| FAAM | Foot and Ankle Ability Measure |
| FFI | Foot Function Index |
| FN | Fracture nonunion |
| HVA | Hallux valgus angle |
| IMA | Intermetatarsal angle |
| JSSF | Japanese Society for Surgery of the Foot |
| OLT | Osteochondral lesions of the talus |
| RTA | Return to activity |
| SEFAS | Self-Reported Foot and Ankle Score |
| VAS | Visual analog scale |
References
- Boike, A.; Schnirring-Judge, M.; McMillin, S. Sesamoid disorders of the first metatarsophalangeal joint. Clin. Podiatr. Med. Surg. 2011, 28, 269–285. [Google Scholar] [CrossRef]
- Zinman, H.; Keret, D.; Reis, N.D. Fracture of the medial sesamoid bone of the hallux. J. Trauma 1981, 21, 581–582. [Google Scholar] [CrossRef]
- Van Hal, M.E.; Keene, J.S.; Lange, T.A.; Clancy, W.G., Jr. Stress fractures of the great toe sesamoids. Am. J. Sports Med. 1982, 10, 122–128. [Google Scholar] [CrossRef]
- Nayfa, T.; Sorto, L. The incidence of hallux abductus following tibial sesamoidectomy. J. Am. Podiatr. Med. Assoc. 1982, 72, 617–620. [Google Scholar] [CrossRef] [PubMed]
- Kaiman, M.E.; Piccora, R. Tibial sesamoidectomy: A review of the literature and retrospective study. J. Foot Surg. 1983, 22, 286–289. [Google Scholar] [PubMed]
- Hulkko, A.; Orava, S.; Pellinen, P.; Puranen, J. Stress fractures of the sesamoid bones of the first metatarsophalangeal joint in athletes. Arch. Orth. Traum. Surg. 1985, 104, 113–117. [Google Scholar] [CrossRef]
- Ogata, K.; Sugioka, Y.; Urano, Y.; Chikama, H. Idiopathic osteonecrosis of the first metatarsal sesamoid. Skeletal. Radiol. 1986, 15, 141–145. [Google Scholar] [CrossRef]
- Richardson, E.G. Injuries to the hallucal sesamoids in the athlete. Foot Ankle 1987, 7, 229–244. [Google Scholar] [CrossRef] [PubMed]
- Orava, S.; Hulkko, A. Delayed unions and nonunions of stress fractures in athletes. Am. J. Sports Med. 1988, 16, 378–382. [Google Scholar] [CrossRef]
- Leventen, E.O. Sesamoid disorders and treatment. An update. Clin. Orthop. Relat. Res. 1991, 269, 236–240. [Google Scholar] [CrossRef]
- Giurini, J.; Chrzan, J.; Gibbons, G.; Habershaw, G. Sesamoidectomy for the treatment of chronic neuropathic ulcerations. J. Am. Podiatr. Med. Assoc. 1991, 81, 167–173. [Google Scholar] [CrossRef]
- Carro, L.P.; Echevarria Llata, J.I.; Martinez Agueros, J.A. Arthroscopic medial bipartite sesamoidectomy of the great toe. Arthroscopy 1999, 15, 321–323. [Google Scholar] [CrossRef]
- Grace, D.L. Sesamoid problems. Foot Ankle Clin. 2000, 5, 609–627. [Google Scholar]
- Biedert, R.; Hintermann, B. Stress fractures of the medial great toe sesamoids in athletes. Foot Ankle Int. 2003, 24, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Saxena, A.; Krisdakumtorn, T. Return to activity after sesamoidectomy in athletically active individuals. Foot Ankle Int. 2003, 24, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Milia, M.J.; Cohen, B.E.; Anderson, R.B. Plantar approach for isolated fibular hallux sesamoidectomy. Tech. Foot. Ankle Surg. 2003, 2, 268–271. [Google Scholar] [CrossRef]
- Lee, S.; James, W.C.; Cohen, B.E.; Davis, W.H.; Anderson, R.B. Evaluation of hallux alignment and functional outcome after isolated tibial sesamoidectomy. Foot Ankle Int. 2005, 26, 803–809. [Google Scholar] [CrossRef]
- Ozkoç, G.; Akpinar, S.; Ozalay, M.; Hersekli, M.A.; Pourbagher, A.; Kayaselçuk, F.; Tandogan, R.N. Hallucal sesamoid osteonecrosis: An overlooked cause of forefoot pain. J. Am. Podiatr. Med. Assoc. 2005, 95, 277–280. [Google Scholar] [CrossRef]
- Chan, P.K.; Lui, T.H. Arthroscopic fibular sesamoidectomy in the management of the sesamoid osteomyelitis. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 664–667. [Google Scholar] [CrossRef]
- Morsi, E. Tibial sesamoidectomy of the great toe in heavy manual workers. Foot 2007, 17, 21–24. [Google Scholar] [CrossRef]
- Waizy, H.; Jäger, M.; Abbara-Czardybon, M.; Schmidt, T.G.; Frank, D. Surgical treatment of AVN of the fibular (lateral) sesamoid. Foot Ankle Int. 2008, 29, 231–236. [Google Scholar] [CrossRef]
- Bichara, D.A.; Henn, R.F.; Theodore, G.H. Sesamoidectomy for hallux sesamoid fractures. Foot Ankle Int. 2012, 33, 704–706. [Google Scholar] [CrossRef]
- Kurian, J.; McCall, D.A.; Ferkel, R.D. Dorsolateral excision of the fibular sesamoid. Tech. Foot. Ankle Surg. 2014, 13, 226–235. [Google Scholar] [CrossRef][Green Version]
- Canales, M.B.; DeMore, M., III; Bowen, M.F.; Ehredt, D.J., Jr.; Razzante, M.C. Fact or fiction? Iatrogenic hallux abducto valgus secondary to tibial sesamoidectomy. J. Foot Ankle Surg. 2015, 54, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Kane, J.M.; Brodsky, J.W.; Daoud, Y. Radiographic results and return to activity after sesamoidectomy for fracture. Foot Ankle Int. 2017, 38, 1100–1106. [Google Scholar] [CrossRef]
- Ford, S.E.; Adair, C.R.; Cohen, B.E.; Davis, W.H.; Ellington, J.K.; Jones, C.P.; Anderson, R.B. Efficacy, outcomes, and alignment following isolated fibular sesamoidectomy via a plantar approach. Foot Ankle Int. 2019, 40, 1375–1381. [Google Scholar] [CrossRef]
- Pearson, J.M.; Moraes, L.V.M.; Paul, K.D.; Peng, J.; Chinnakkannu, K.; McKissack, H.M.; Shah, A. Is fibular sesamoidectomy a viable option for sesamoiditis? A retrospective study. Cureus 2019, 11, 4939. [Google Scholar] [CrossRef] [PubMed]
- Dean, R.S.; Coetzee, J.C.; McGaver, R.S.; Fritz, J.E.; Nilsson, L.J. Functional outcome of sesamoid excision in athletes. Am. J. Sports. Med. 2020, 48, 3603–3609. [Google Scholar] [CrossRef]
- Mehtar, M.; Saragas, N.P.; Ferrao, P.N. Functional and patient reported outcomes following lateral hallucal sesamoidectomy. Foot 2020, 43, 101656. [Google Scholar] [CrossRef]
- Levaj, I.; Knežević, I.; Dimnjaković, D.; Smoljanović, T.; Bojanić, I. First metatarsophalangeal joint arthroscopy of 36 consecutive cases. Acta Chir. Orthop. Traumatol. Cech. 2021, 88, 211–216. [Google Scholar] [CrossRef]
- Saxena, A.; Fournier, M.; Patel, P.; Maffulli, N. Sesamoidectomy in athletes: Outcomes from 2-centers. J. Foot Ankle Surg. 2022, 61, 139–142. [Google Scholar] [CrossRef]
- Nakajima, K. Arthroscopic sesamoidectomy for hallux sesamoid disorders. J. Foot Ankle Surg. 2022, 61, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Vesely, B.; Sikora, R.R.; Dial, D. Partial excision of a tibial sesamoid fracture nonunion in a patient with congenital absence of fibular sesamoid: A case study. J. Am. Podiatr. Med. Assoc. 2023, 113, 21–43. [Google Scholar] [CrossRef]
- Engasser, W.M.; Coetzee, J.C.; Seybold, J.D.; Dock, C.C.; Seiffert, K.J.; Stone McGaver, R.; Attia, A.K.; Den Hartog, B.D. Early functional outcomes and complications of tibial and/or peroneal sesamoidectomy utilizing a burr through a medial approach. Foot Ankle Int. 2024, 45, 1070–1075. [Google Scholar] [CrossRef]
- Auersperg, V.; Trieb, K. Extracorporeal shock wave therapy: An update. EFORT. Open Rev. 2020, 5, 584–592. [Google Scholar] [CrossRef]
- Van Lieshout, E.M.M.; Den Hartog, D. Effect of platelet-rich plasma on fracture healing. Injury 2021, 52, S58–S66. [Google Scholar] [CrossRef] [PubMed]
- Lv, F.; Li, Z.; Jing, Y.; Sun, L.; Li, Z.; Duan, H. The effects and underlying mechanism of extracorporeal shockwave therapy on fracture healing. Front. Endocrinol. 2023, 14, 1188297. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.J.; Liu, H.C.; Fu, T.H. The effects of extracorporeal shockwave on acute high-energy long bone fractures of the lower extremity. Arch. Orthop. Trauma Surg. 2007, 127, 137–142. [Google Scholar] [CrossRef]
- An, W.; Ye, P.; Zhu, T.; Li, Z.; Sun, J. Platelet-rich plasma combined with autologous grafting in the treatment of long bone delayed union or non-union: A meta-analysis. Front. Surg. 2021, 8, 621559. [Google Scholar] [CrossRef]
- Alves, E.M.; Angrisani, A.T.; Santiago, M.B. The use of extracorporeal shock waves in the treatment of osteonecrosis of the femoral head: A systematic review. Clin. Rheumatol. 2009, 28, 1247–1251. [Google Scholar] [CrossRef]
- D’Agostino, C.; Romeo, P.; Amelio, E.; Sansone, V. Effectiveness of ESWT in the treatment of Kienböck’s disease. Ultrasound Med. Biol. 2011, 37, 1452–1456. [Google Scholar] [CrossRef]
- Häußer, J.; Wieber, J.; Catalá-Lehnen, P. The use of extracorporeal shock wave therapy for the treatment of bone marrow oedema—A systematic review and meta-analysis. J. Orthop. Surg. Res. 2021, 16, 369. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Ye, L.; Liu, H.; Yang, P.; Yang, B. Extracorporeal shock wave therapy for the treatment of osteoarthritis: A systematic review and meta-analysis. Biomed. Res. Int. 2020, 2020, 1907821. [Google Scholar] [CrossRef]
- Jhan, S.-W.; Wu, K.-T.; Chou, W.-Y.; Chen, P.-C.; Wang, C.-J.; Huang, W.-C.; Cheng, J.-H. A comparative analysis of platelet-rich plasma alone versus combined with extracorporeal shockwave therapy in athletes with patellar tendinopathy and knee pain: A randomized controlled trial. Knee Surg. Relat. Res. 2024, 36, 47. [Google Scholar] [CrossRef] [PubMed]
- Arnó, A.; García, O.; Hernán, I.; Sancho, J.; Acosta, A.; Barret, J.P. Extracorporeal shock waves, a new non-surgical method to treat severe burns. Burns 2010, 36, 844–849. [Google Scholar] [CrossRef]
- Vidal, X.; Morral, A.; Costa, L.; Tur, M. Radial extracorporeal shock wave therapy (rESWT) in the treatment of spasticity in cerebral palsy: A randomized, placebo-controlled clinical trial. NeuroRehabilitation 2011, 29, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Romeo, P.; Lavanga, V.; Pagani, D.; Sansone, V. Extracorporeal shock wave therapy in musculoskeletal disorders: A review. Med. Princ. Pract. 2014, 23, 7–13. [Google Scholar] [CrossRef]
- Kale, P.; Shrivastava, S.; Balusani, P.; Pundkar, A. Therapeutic potential of platelet-rich plasma in fracture healing: A comprehensive review. Cureus 2024, 16, 62271. [Google Scholar] [CrossRef]
- Liang, Y.; Li, J.; Wang, Y.; He, J.; Chen, L.; Chu, J.; Wu, H. Platelet rich plasma in the repair of articular cartilage injury: A narrative review. Cartilage 2022, 13, 19476035221118419. [Google Scholar] [CrossRef]
- Randelli, P.; Arrigoni, P.; Ragone, V. Platelet rich plasma in arthroscopic rotator cuff repair: A prospective RCT study, 2-year follow-up. J. Shoulder Elb. Surg. 2011, 20, 518–528. [Google Scholar] [CrossRef]
- Radice, F.; Yánez, R.; Gutiérrez, V.; Rosales, J.; Pinedo, M.; Coda, S. Comparison of magnetic resonance imaging findings in anterior cruciate ligament grafts with and without autologous platelet-derived growth factors. Arthroscopy 2010, 26, 50–57. [Google Scholar] [CrossRef]
- Zhang, Y.; Xing, F.; Luo, R.; Duan, X. Platelet-rich plasma for bone fracture treatment: A systematic review of current evidence in preclinical and clinical studies. Front. Med. 2021, 8, 676033. [Google Scholar] [CrossRef]
- Filardo, G.; Previtali, D.; Napoli, F.; Candrian, C.; Zaffagnini, S.; Grassi, A. PRP injections for the treatment of knee osteoarthritis: A meta-analysis of randomized controlled trials. Cartilage 2020, 13, 364S–375S. [Google Scholar] [CrossRef]
- Jamal, M.S.; Hurley, E.T.; Asad, H.; Asad, A.; Taneja, T. The role of platelet rich plasma and other orthobiologics in bone healing and fracture management: A systematic review. J. Clin. Orthop. Trauma 2022, 25, 101759. [Google Scholar] [CrossRef] [PubMed]
- Kadakia, A.R.; Molloy, A. Current concepts review: Traumatic disorders of the first metatarsophalangeal joint and sesamoid complex. Foot Ankle Int. 2011, 32, 834–839. [Google Scholar] [CrossRef] [PubMed]
- Robertson, G.A.J.; Goffin, J.S.; Wood, A.M. Return to sport following stress fractures of the great toe sesamoids: A systematic review. Br. Med. Bull. 2017, 122, 135–149. [Google Scholar] [CrossRef]
- Shimozono, Y.; Hurley, E.T.; Brown, A.J.; Kennedy, J.G. Sesamoidectomy for hallux sesamoid disorders: A systematic review. J. Foot Ankle Surg. 2018, 57, 1186–1190. [Google Scholar] [CrossRef]
- Stein, C.J.; Sugimoto, D.; Slick, N.R.; Lanois, C.J.; Dahlberg, B.W.; Zwicker, R.L.; Micheli, L.J. Hallux sesamoid fractures in young athletes. Phys. Sportsmed. 2019, 47, 441–447. [Google Scholar] [CrossRef]
- Artioli, E.; Mazzotti, A.; Di Paola, G.; Sgubbi, F.; Gemini, G.; Zielli, S.O.; Faldini, C. Hallux sesamoid nonunion: A comprehensive systematic review of current evidence. J. Pers. Med. 2025, 15, 342. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Saxena, A.; Yun, A.; Patel, R.; Gerdesmeyer, L.; Maffulli, N. Radial soundwave for sesamoidopathy in athletes: A pilot study. J. Foot Ankle Surg. 2016, 55, 1333–1335. [Google Scholar] [CrossRef]
- Le, H.M.; Stracciolini, A.; Stein, C.J.; Quinn, B.J.; Jackson, S.S. Platelet rich plasma for hallux sesamoid injuries: A case series. Phys. Sportsmed. 2022, 50, 181–184. [Google Scholar] [CrossRef]
- Callahan, E.A.; Peyser, K.; Espiritu-McKay, T. Leukocyte-rich platelet-rich plasma for osteonecrosis of sesamoid in a performing artist: A case report. J. Danc. Med. Sci. 2025, 29, 61–63. [Google Scholar] [CrossRef]
- Shimozono, Y.; Seow, D.; Kennedy, J.G. Concentrated bone marrow aspirate injection for hallux sesamoid disorders. J. Foot Ankle Surg. 2022, 61, 633–636. [Google Scholar] [CrossRef]
- Scala, V.A.; Kikuchi, C.K. Sesamoid avascular necrosis and stress fracture treated with core decompression and biologic augmentation. Hawaii J. Health Soc. Welf. 2022, 81, 16–18. [Google Scholar] [PubMed]
- Kwok, I.H.Y.; Ieong, E.; Aljalahma, M.A.; Haldar, A.; Welck, M. Extracorporeal shock wave treatment in foot and ankle fracture non-unions—A review. Foot 2022, 51, 101889. [Google Scholar] [CrossRef]
- Cao, J.; Zhang, C.; Huang, H.; Yang, L.; Duan, X. Bone marrow edema syndrome of the foot treated with extracorporeal shock wave therapy: A retrospective case series. J. Foot Ankle Surg. 2021, 60, 523–528. [Google Scholar] [CrossRef]
- Omodani, T. Extracorporeal shock wave therapy combined with platelet-rich plasma injection to treat the nonunion of a stress fracture of the proximal phalanx of the great toe: A case report. Cureus 2024, 16, 55877. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.B.; McBryde, A.M. Autogenous bone grafting of hallux sesamoid nonunions. Foot Ankle Int. 1997, 18, 293–296. [Google Scholar] [CrossRef]
- Blundell, C.M.; Nicholson, P.; Blackney, M.W. Percutaneous screw fixation for fractures of the sesamoid bones of the hallux. J. Bone Jt. Surg. Br. 2002, 84-B, 1138–1141. [Google Scholar] [CrossRef]
- Pagenstert, G.I.; Valderrabano, V.; Hintermann, B. Medial sesamoid nonunion combined with hallux valgus in athletes: A report of two cases. Foot Ankle Int. 2006, 27, 135–140. [Google Scholar] [CrossRef]
- Park, Y.H.; Son, S.W.; Ahn, S.J.; Yoo, H.S.; Kim, H.J. Postoperative outcome of screw fixation with autogenous bone grafting for the management of hallux sesamoid fracture nonunion. Arch. Orthop. Trauma. Surg. 2024, 145, 92. [Google Scholar] [CrossRef]
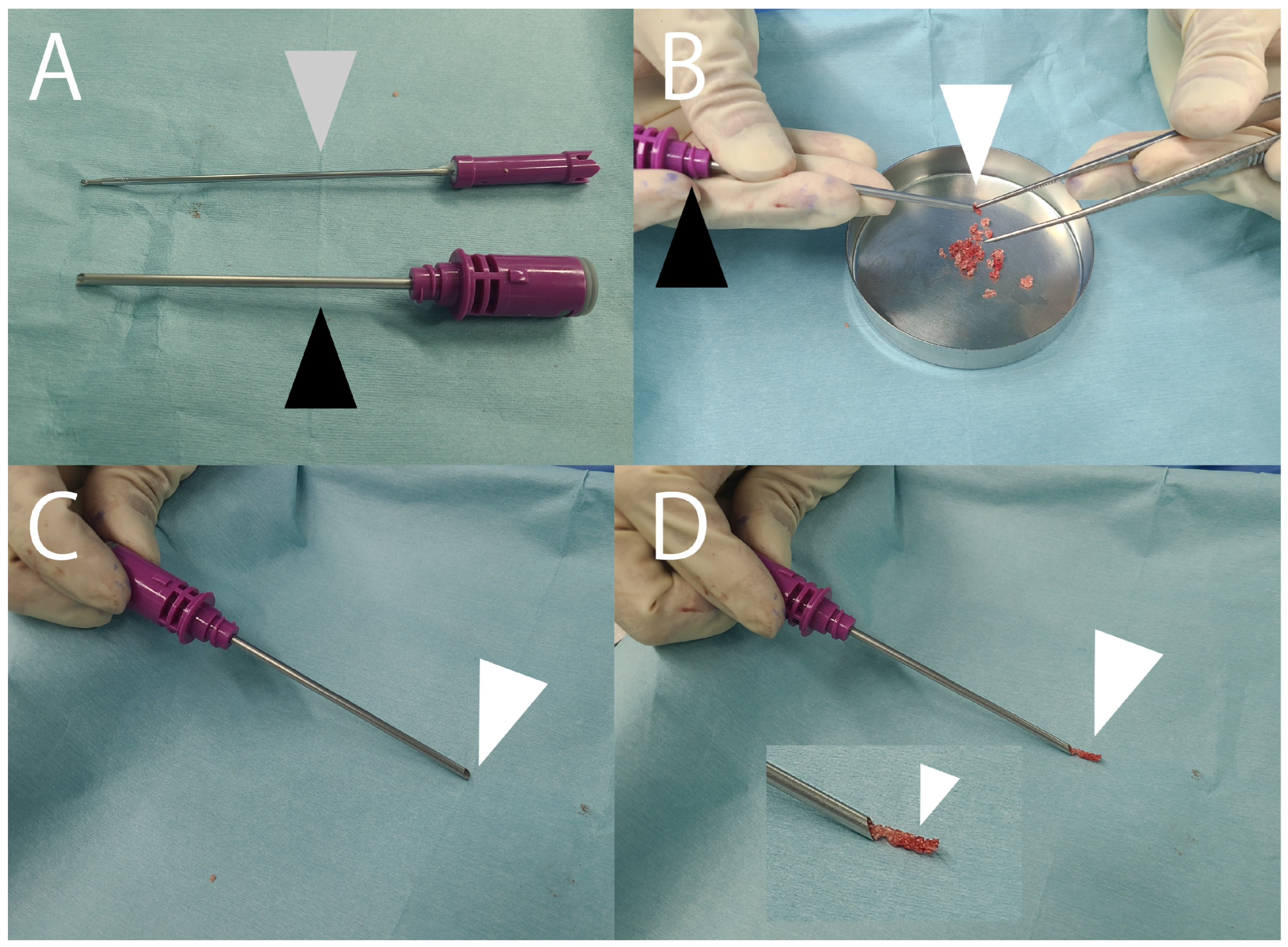
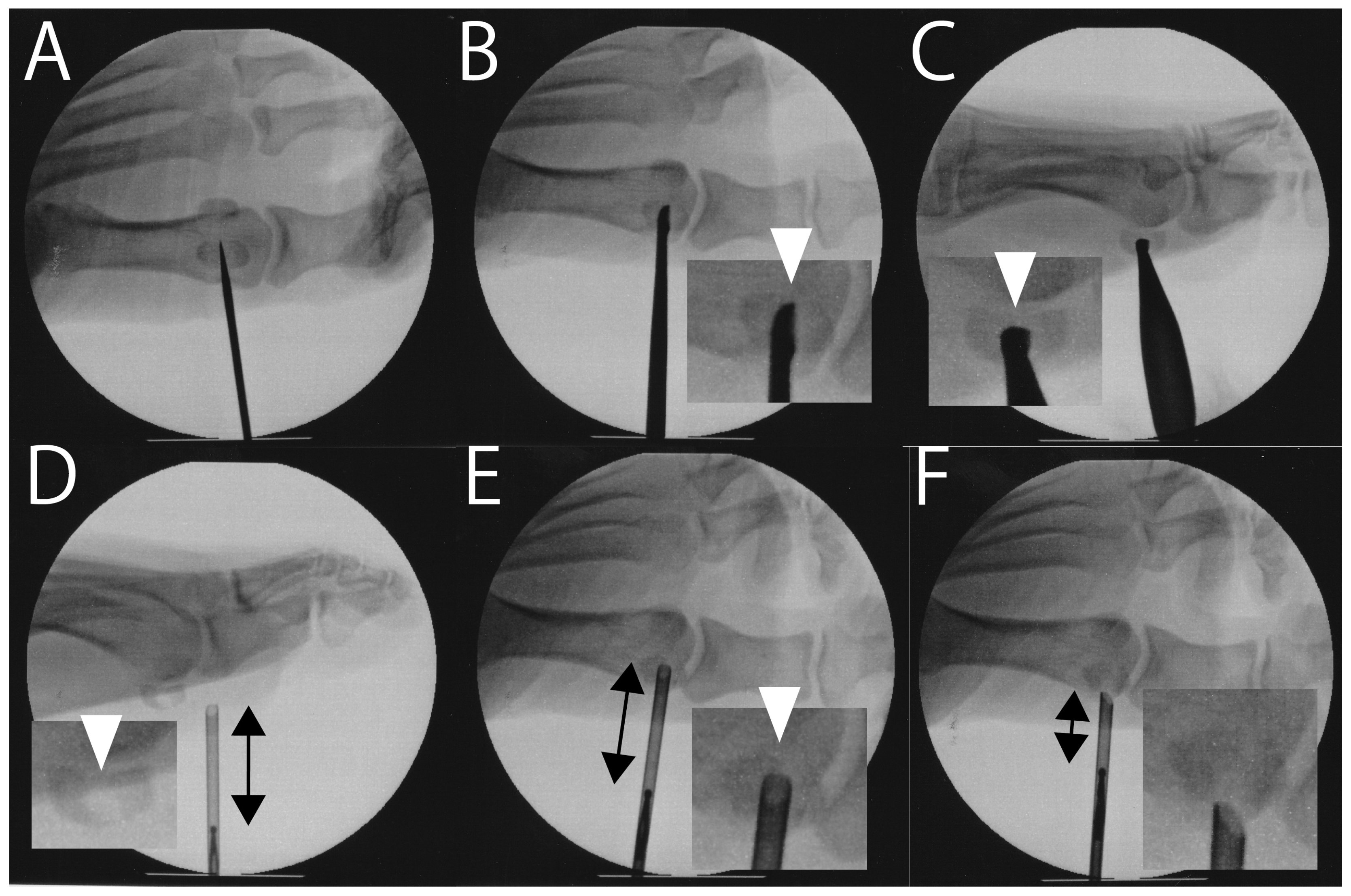
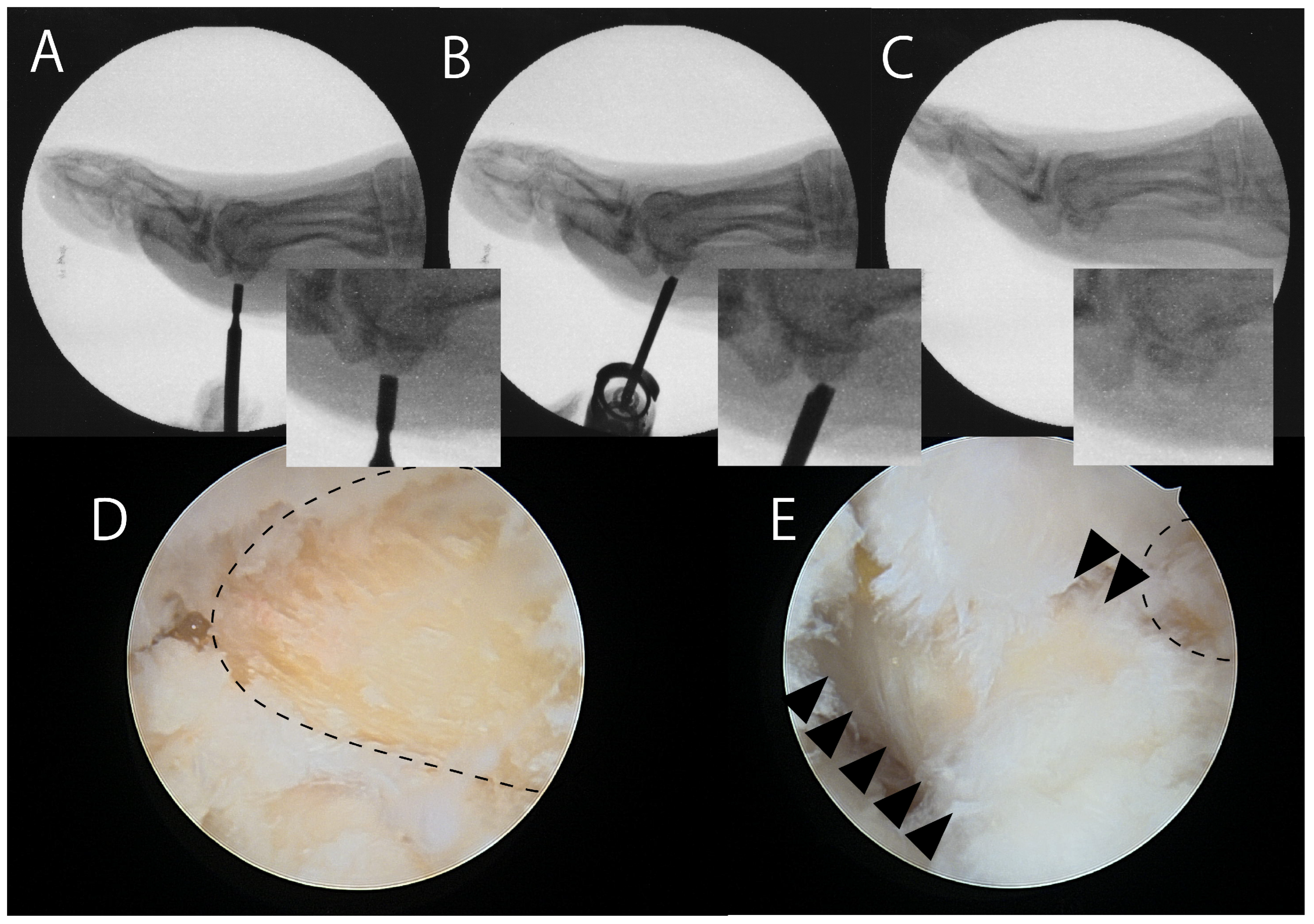
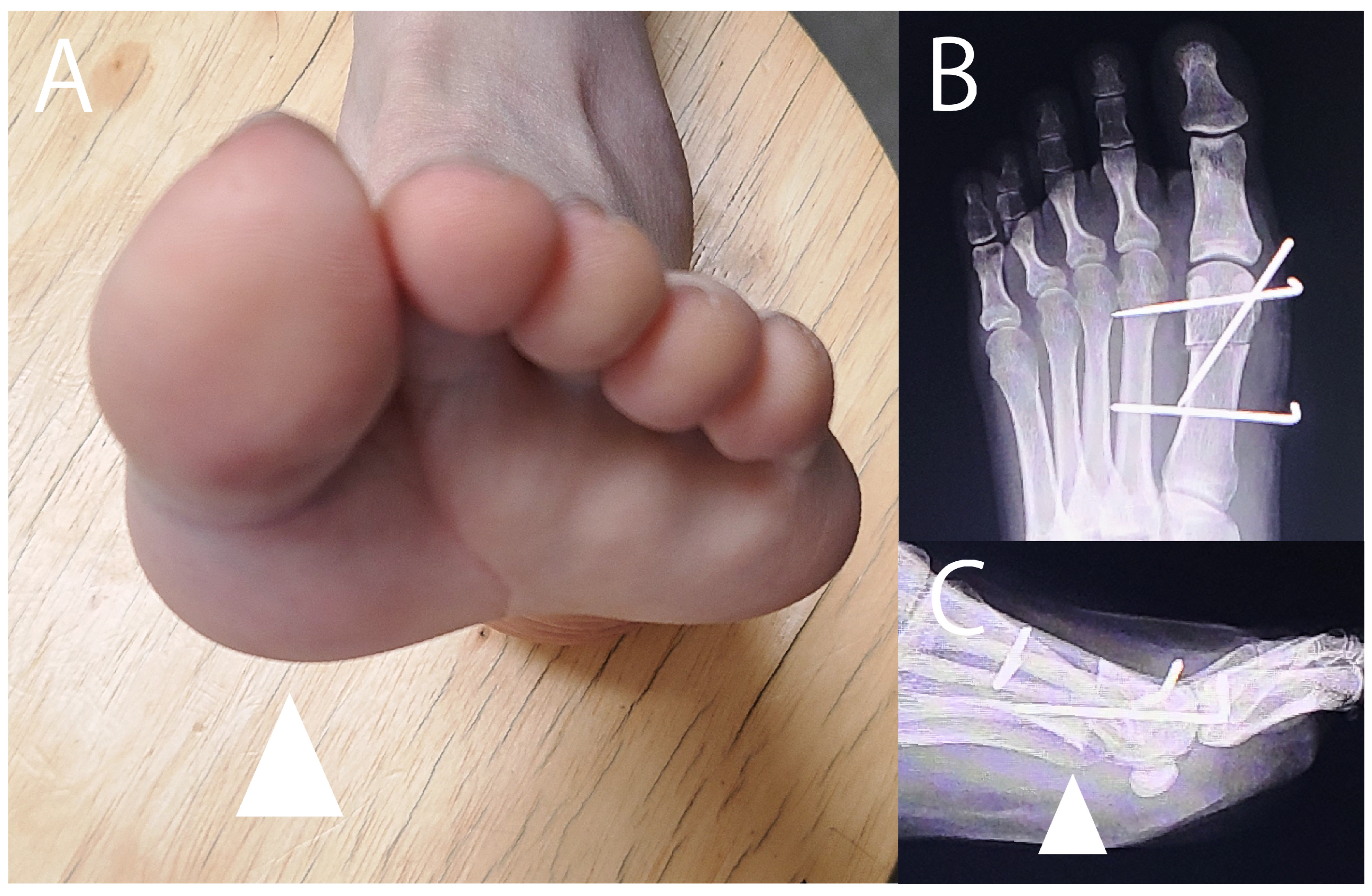
- Nakajima, K. Arthroscopic autologous bone grafting for hallux sesamoid fracture nonunion results in a high rate of complete resolution. Arthrosc. Sports. Med. Rehabil. 1789, 4, e1789–e1797. [Google Scholar] [CrossRef]
- Moran, C.J.; Viard, B.; Tourné, Y. Long term follow up on treatment of hallux sesamoid fracture with temporary first metatarsal joint internal fixation. Foot 2024, 60, 102104. [Google Scholar] [CrossRef] [PubMed]
- Riley, J.; Selner, M. Internal fixation of a displaced tibial sesamoid fracture. J. Am. Podiatr. Med. Assoc. 2001, 91, 536–539. [Google Scholar] [CrossRef]
- Aquino, M.D.; Devincentis, A.F.; Keating, S.E. Tibial sesamoid planing procedure: An appraisal of 26 feet. J. Foot. Surg. 1984, 23, 226–230. [Google Scholar] [PubMed]
- Van Enoo, R.E.; Cane, E.M. Tibial sesamoid planing for intractable plantar keratoses. Clin. Podiatr. Med. Surg. 1991, 8, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Mann, R.A.; Wapner, K.L. Tibial sesamoid shaving for treatment of intractable plantar keratosis. Foot Ankle 1992, 13, 196–198. [Google Scholar] [CrossRef]
- Oloff, L.M.; Schulhofer, S.D. Sesamoid complex disorders. Clin. Podiatr. Med. Surg. 1996, 13, 497–513. [Google Scholar] [CrossRef]
- Cohen, B.E. Hallux sesamoid disorders. Foot. Ankle. Clin. 2009, 14, 91–104. [Google Scholar] [CrossRef]
- Bartosiak, K.; McCormick, J.J. Avascular necrosis of the sesamoids. Foot. Ankle Clin. 2019, 24, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Mauler, F.; Wanivenhaus, F.; Böni, T.; Berli, M. Nonsurgical treatment of osteomyelitis of the hallux sesamoids: A case series and literature review. J. Foot Ankle Surg. 2017, 56, 666–669. [Google Scholar] [CrossRef] [PubMed]


| Author (Year) | Study Type, Patient Number (Affected Sesamoid) | Diagnosis | Approach | Favorable Outcome | Unfavorable Outcome |
|---|---|---|---|---|---|
| Zinman (1981) [2] | Case report 1 (1 tibial) | 1 FN | Medial | Complete pain relief Return to full athletic activity | None reported |
| Van Hal (1982) [3] | Case series 4 (2 tibial; 2 fibular) | FN | Plantar medial | Asymptomatic (n = 4) | None reported |
| Nayfa (1982) [4] | Case series 11 (19 tibial) | Not specified | Not specified | Complete success (n = 11) Some improvement (n = 8) | Hallux valgus (42.1%) |
| Kaiman (1983) [5] | Case series 8 (8 tibial) | Not specified | Not specified | None reported | None reported |
| Hulkko (1985) [6] | Case series 5 (5 not specified) | 5 FN | Medial | Good result (n = 2) Training resumed 6–8 weeks after surgery | Mild symptoms during intensive training (n = 3) |
| Ogata (1986) [7] | Case series 4 (3 tibial; 1 fibular) | 4 AVN | Medial Fibular: Not specified | Excellent | None reported |
| Richardson (1987) [8] | Case series 2 (2 tibial) | FN | Medial | RTA of 3 months Asymptomatic (n = 2) | None reported |
| Orava (1988) [9] | Case series 5 (5 not specified) | 5 FN | Not specified | Excellent/good (n = 5) | None reported |
| Leventen (1990) [10] | Case series 20 (21 tibial; 2 fibular) | 8 sesamoiditis 15 not specified | Medial Plantar | Completely satisfied (n = 18) | None reported |
| Giurini (1991) [11] | Case series 24 (13 tibial; 13 tibial and fibular) | 24 diabetic neuropathic ulceration | Medial | Healed ulcer (n = 20) | Wound infection (n = 1) Re-ulceration (n = 4) |
| Carro (1999) [12] | Case report 1 (1 tibial) | 1 sesamoiditis | Arthroscopy | Successful excision | None reported |
| Grace (2000) [13] | Case series 11 (6 tibial; 5 fibular) | 2 prominent 3 fragmented 2 fracture 4 unclear | Not specified | Good (n = 6) Fair (n = 4) | Hallux valgus (n = 2) Poor outcome, retired from soccer (n = 1) |
| Biedert (2003) [14] | Case series 6 (6 tibial) | 6 FN | Medial | All good/excellent AOFAS 95.3 | Mild limitation of sports ability (n = 1) Plantar fasciitis (n = 1) |
| Saxena (2003) [15] | Case series 24 (16 tibial; 10 fibular) | Not specified | Medial Plantar Dorsolateral | Athlete RTA of 7.5 weeks (n = 11) Active patients RTA of 12 weeks (n = 13) | Hallux varus (n = 1) Hallux valgus (n = 1) Scarring with neuroma-like symptoms (n = 2) |
| Milia (2003) [16] | Case series 12 (13 fibular) | 5 osteochondritis 5 sesamoiditis 2 FN 1 planter keratosis | Plantar | Very satisfied (n = 9) Satisfied (n = 1) | VAS 88.7–19.6 Dissatisfied (n = 2) |
| Lee (2005) [17] | Case series 32 (32 tibial) | Not specified | Medial | All preoperative activities resumed (90%) | Postoperative VAS 18.5 Extreme difficulty or inability to stand on tip toes (30%) Transfer metatarsalgia (14%) |
| Ozkoç (2005) [18] | Case series 4 (2 tibial; 2 fibular) | 4 AVN | Medial Plantar | Pain free (n = 3) Satisfied (n = 1) | None reported |
| Chan (2006) [19] | Case report 1 (1 fibular) | osteomyelitis | Arthroscopy | Good functional recovery | No morbidity |
| Morsi (2007) [20] | Case series 13 (13 tibial) | Sesamoiditis | Plantarmedial | Return to heavy work at 12.5 weeks No pain (n = 12) | Mild pain on standing on tip toes (n = 1) |
| Waizy (2008) [21] | Case series 2 (2 fibular) | 2 AVN | Plantar | Complete resolution | None reported |
| Bichara (2012) [22] | Case series 24 (15 tibial; 9 fibular) | 24 FN | Medial Dorsolateral | 91.6% RTA at 11.6 weeks VAS 6.2 → 0.7 | Hallux valgus (n = 1) Did not RTA (n = 1) |
| Kurian (2014) [23] | Case series 8 (8 fibular) | 3 AVN 5 FN | Dorsolateral | Excellent (n = 5) Good (n = 3) AOFAS 91 RTA 15 weeks | None reported |
| Canales (2015) [24] | Case series 5 (5 tibial) | Not specified | Medial | VAS 6.8 → 1 No significant changes in HVA and IMA | None reported |
| Kane (2017) [25] | Comparative study 46 (22 tibial; 24 fibular) | 46 FN | Medial Dorsolateral | No clinically significant changes in HVA and IMA | With complications (n = 11) Did not RTA (n = 3) Needed orthotics (n = 7) |
| Ford (2019) [26] | Case series 36 (36 fibular) | 5 AVN 3 fracture 1 FN 27 sesamoiditis | Plantar | Very satisfied (70%) Satisfied (18%) AOFAS 90 FFI 28.4 | Dissatisfied (3%) Very dissatisfied (9%) |
| Pearson (2019) [27] | Case series 12 (12 fibular) | 9 sesamoiditis 5 AVN | Plantar | FFI 8.3 | Transient neuritis (n = 2) Painful scar (n = 1) Infection (n = 1) |
| Dean (2020) [28] | Case series 82 (54 tibial 18 fibular) | 42 AVN 14 sesamoiditis 10 FN 9 prominent sesamoid 7 others | Medial Plantar | VAS 6.3 → 2.8 Return to sports within 4.6 months (80%) SF-12 59.3 → 86.7 | Unable to reach preinjury levels (13%) Unable to return to sports (20%) |
| Mehtar (2020) [29] | Case series 12 (14 fibular) | 8 sesamoiditis 2 FN 1 AVN 1 RA | Plantar | All excellent AOFAS 92.3 SEFAS 46.0 | Neuroma (n = 1) |
| Levaj (2021) [30] | Case series 5 (3 tibial; 2 fibular) | 5 FN | Arthroscopy | All very satisfied | None reported |
| Saxena (2022) [31] | Case series 68 (41 tibial; 29 fibular) | Not specified | Medial Plantar | RTA 11.0 weeks | Complication rate: 5.7% |
| Nakajima (2022) [32] | Case series 14 (13 tibial; 1 fibular; 1 tibial and fibular) | 12 FN 3 keratosis | Arthroscopy | VAS 75.4 → 14.3 JSSF 55.2 → 88.0 | Complication rate: 85% |
| Vesely (2023) [33] | Case report 1 (1 tibial) | 1 avulsion fracture | Plantar | Partial sesamoidectomy Able to return daily activity | Unable to return to softball |
| Engasser (2024) [34] | Case series 27 (10 tibial; 9 fibular; 8 tibial and fibular) | 7 sesamoiditis 6 FN 6 AVN 6 arthritis | Medial | Satisfaction rate: 80.6% FAAM ADL 58.3 → 83.2 FAAM Sport 26.4 → 63.7 VAS 51.0 → 24.0 | Complication rate: 37.9% Reoperation rate: 13.7% Continuous pain: 20% |
| Author (Year) | Diseases | Study Type (Cases) | Treatment | Outcomes | Complications |
|---|---|---|---|---|---|
| Saxena (2016) [61] | Sesamoiditis Sesamoid AVN Symptomatic bipartite sesamoid | Case series (10) | Radial ESWT | VAS 56 → 23 Roles and Maudsley score 3.1 → 1.5 Returned to activity at 10.1 weeks | One patient returned to activity at 1 year |
| Le (2022) [62] | Sesamoid stress fracture (1 unilateral tibial, 1 bilateral tibial) 1 bipartite fibular sesamoiditis | Case series (4) | PRP | Returned to sports at 6 weeks after first injection (n = 2) Required two injections; returned at 9 weeks after second injection (n = 1; bilateral) | None reported |
| Callahan (2025) [63] | Sesamoid AVN | Case report (1 fibular) | Leukocyte-rich PRP injection | NRS 4 → 0 at 2 months after injection NRS 4 at 2 years after injection | None reported |
| Shimozono (2022) [64] | Sesamoid AVN | Case series (11) | Core decompression Concentrated bone marrow aspirate injection | Return to sports activities (8/11) | Persistent pain (1/11) |
| Scala (2022) [65] | Sesamoid AVN | Case report (1 tibial) | Core decompression Concentrated bone marrow aspirate with amniotic membrane matrix | Return to full athletic activities at 6 months | None reported |
| Author (Year) | Study Type | Disease | Treatment | Outcomes | Complications |
|---|---|---|---|---|---|
| Kwok (2022) [66] | Systematic review | 65 metatarsal stress fractures, 1 navicular stress fracture | ESWT | Union rates: Metatarsal 93.8% (61/65); Navicular 0% (0/1) | Soft tissue swelling (1/65), petechiae (1/65), bruising (1/65), pain (1/65) |
| Cao (2021) [67] | Case series (20 patients) | Bone marrow edema syndrome of the foot | ESWT | VAS: 7.7 → 2.4 AOFAS: 62.1 → 82.8 Edema area on MRI 132 → 41 mm2 | Transient skin erythema (2/20) |
| Omodani (2024) [68] | Case report | Proximal phalanx fracture nonunion | PRP + ESWT | Union achieved at 4 weeks | None reported |
| Author (Year) | Study Type Patient Number (Affected Sesamoid) | Procedure | Outcomes | Complications |
|---|---|---|---|---|
| Anderson (1997) [69] | Case series 18 (21 tibial) | Bone grafting | Union (19/21) Return to preinjury level of athletic and occupational activity (17/18) | Nonunion (2/21) Paresthesia (1/21) Hallux valgus (1/21) |
| Blundell (2002) [70] | Case series 9 (5 tibial, 4 fibular) | Percutaneous screw fixation | AOFAS 46.9 → 80.7 Return to previous activity levels by 3 months (100%) | No complications |
| Pagenstert (2006) [71] | Case series 2 (2 tibial) | Screw fixation | AOFAS 14 and 12 to 100 (both) at 12 weeks after surgery | No complaints |
| Park (2024) [72] | Case series 10 (9 tibial, 1 fibular) | Screw fixation | VAS 67.8 → 3.6 FFI 72.3 → 8.2 Union within 3 months after surgery (100%) | Hardware discomfort (2/10) |
| Nakajima (2022) [73] | Case series 11 (10 tibial, 1 fibular) | Arthroscopic bone grafting | VAS 72.0 → 12.0 VAS of 0 and JSSF of 100 observed in 9/11 | Persistent pain (2/11) |
| Moran (2024) [74] | Case series 32 (Not specified) | Temporary joint fixation | Union (94%) Return to work after 61 days Return to sports after 80 days | Nonunion (1/32) Postop. Arthritis (1/32) |
| Riley (2001) [75] * | Case report 1 (1 tibial) | Circled soft wire fixation | Return to full activities without limitation within 14 weeks | None reported |
| Author (Year) | Study Type Patient (Affected Sesamoid) | Outcomes | Complications |
|---|---|---|---|
| Aquino (1984) [76] | Case series 20 (26 tibial) | Subjective success rate: 88.8% Objective success rate: 76.9% | Poor results (3/26) |
| Van Enoo (1991) [77] | Case series 13 (17 tibial) | Complete resolution (15/17) | Mild calloused lesions (2/17) |
| Mann (1992) [78] | Case series 10 (11 tibial) | Excellent (5/11) Good (4/11) | Mild recurrent callus (1/11) |
| Grace (2000) [13] | Case series 7 (7 not specified) | Good (5/7) | Reflex sympathetic dystrophy (1/7) Insufficient bone removal (1/7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakajima, K. Avoiding Hallux Sesamoidectomy: A Narrative Review. J. Clin. Med. 2025, 14, 7687. https://doi.org/10.3390/jcm14217687
Nakajima K. Avoiding Hallux Sesamoidectomy: A Narrative Review. Journal of Clinical Medicine. 2025; 14(21):7687. https://doi.org/10.3390/jcm14217687
Chicago/Turabian StyleNakajima, Kenichiro. 2025. "Avoiding Hallux Sesamoidectomy: A Narrative Review" Journal of Clinical Medicine 14, no. 21: 7687. https://doi.org/10.3390/jcm14217687
APA StyleNakajima, K. (2025). Avoiding Hallux Sesamoidectomy: A Narrative Review. Journal of Clinical Medicine, 14(21), 7687. https://doi.org/10.3390/jcm14217687






