Is There Agreement Between Clinical Outcomes as Perceived by the Surgeon and the Patient in Revision Total Hip Arthroplasty?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Assessment of Bone Defects
2.4. Evaluation of Functional Outcomes
2.5. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Analytical Results
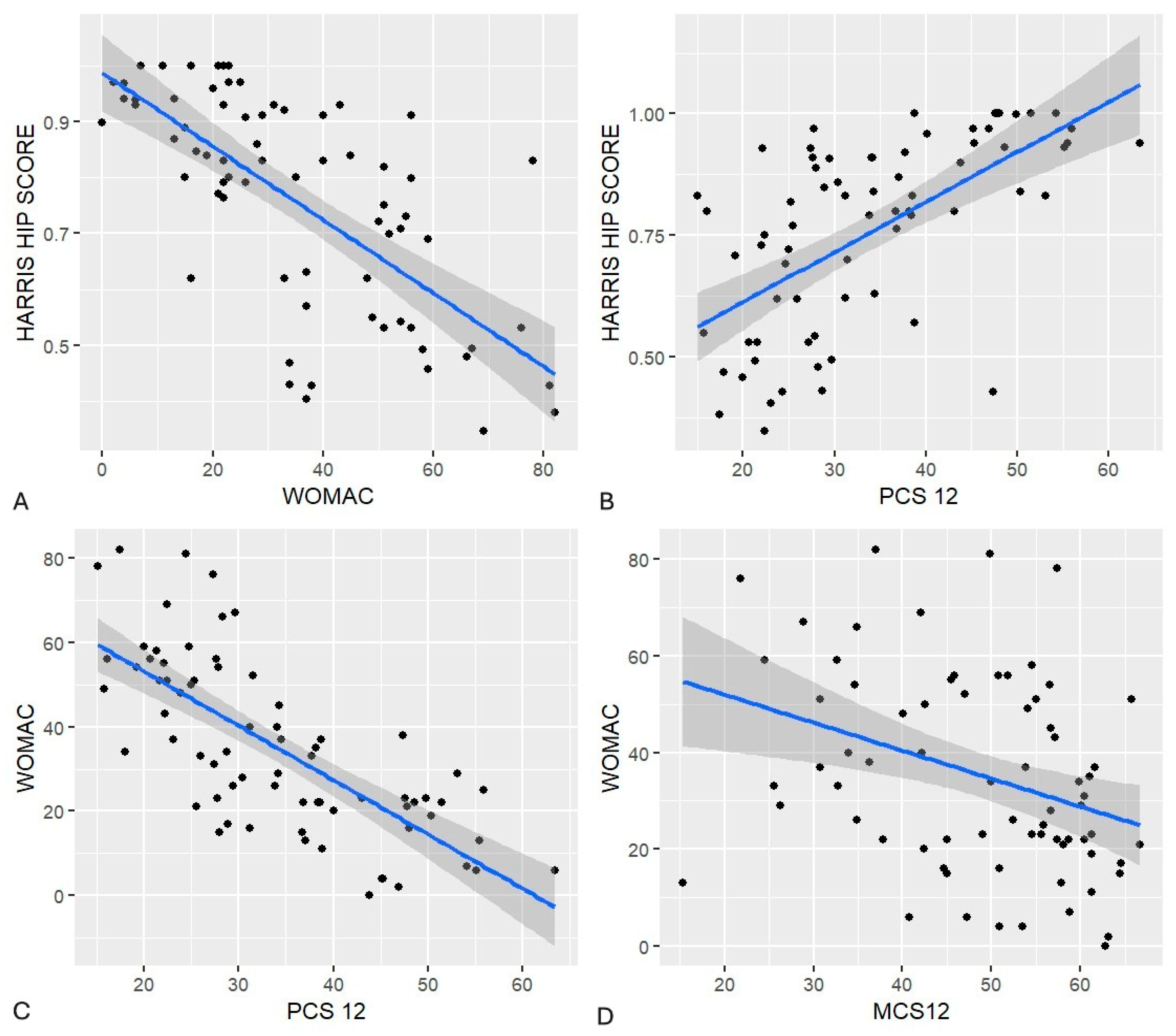
3.2.1. Surgeon-Reported Outcomes
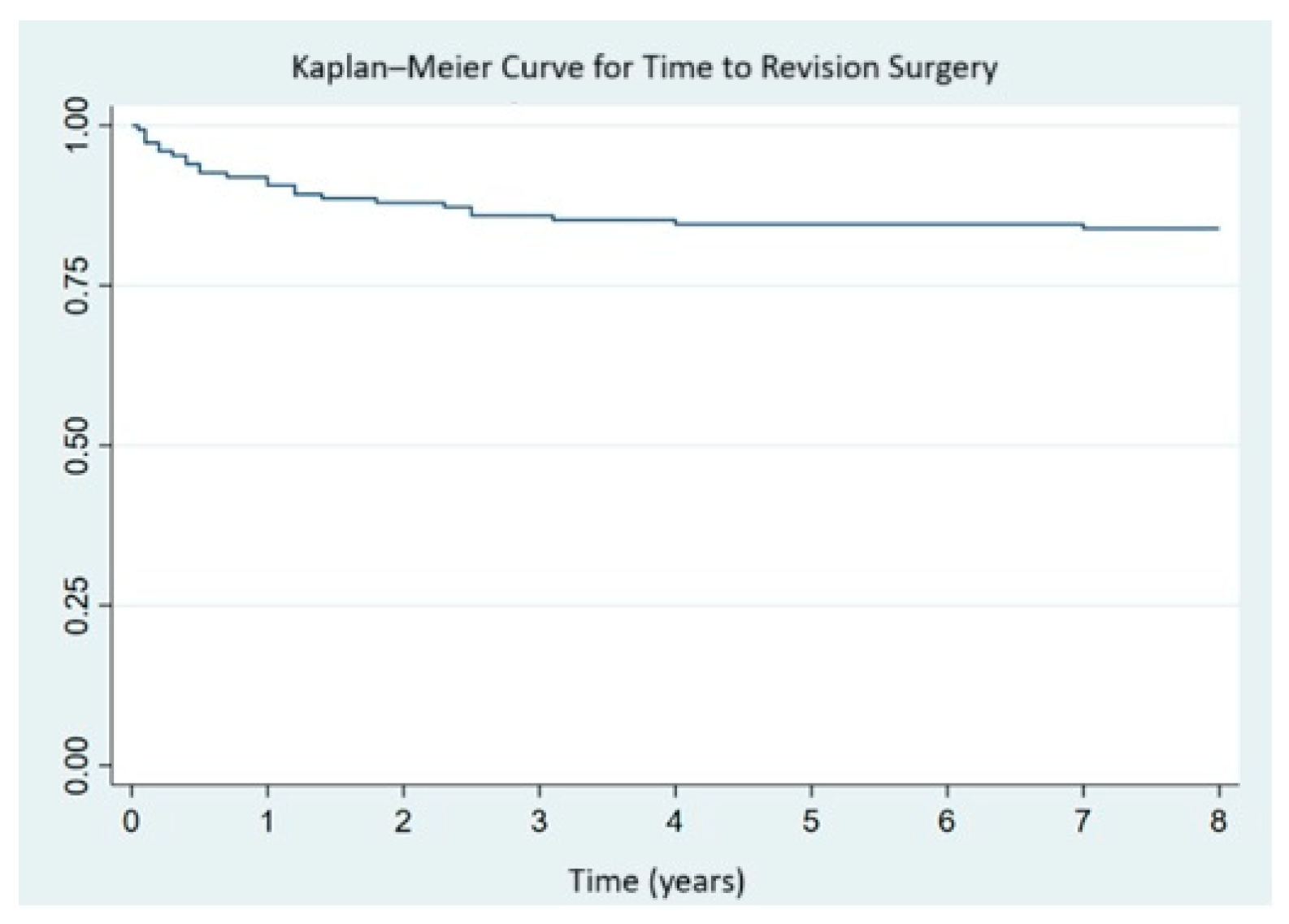
Implant Survival
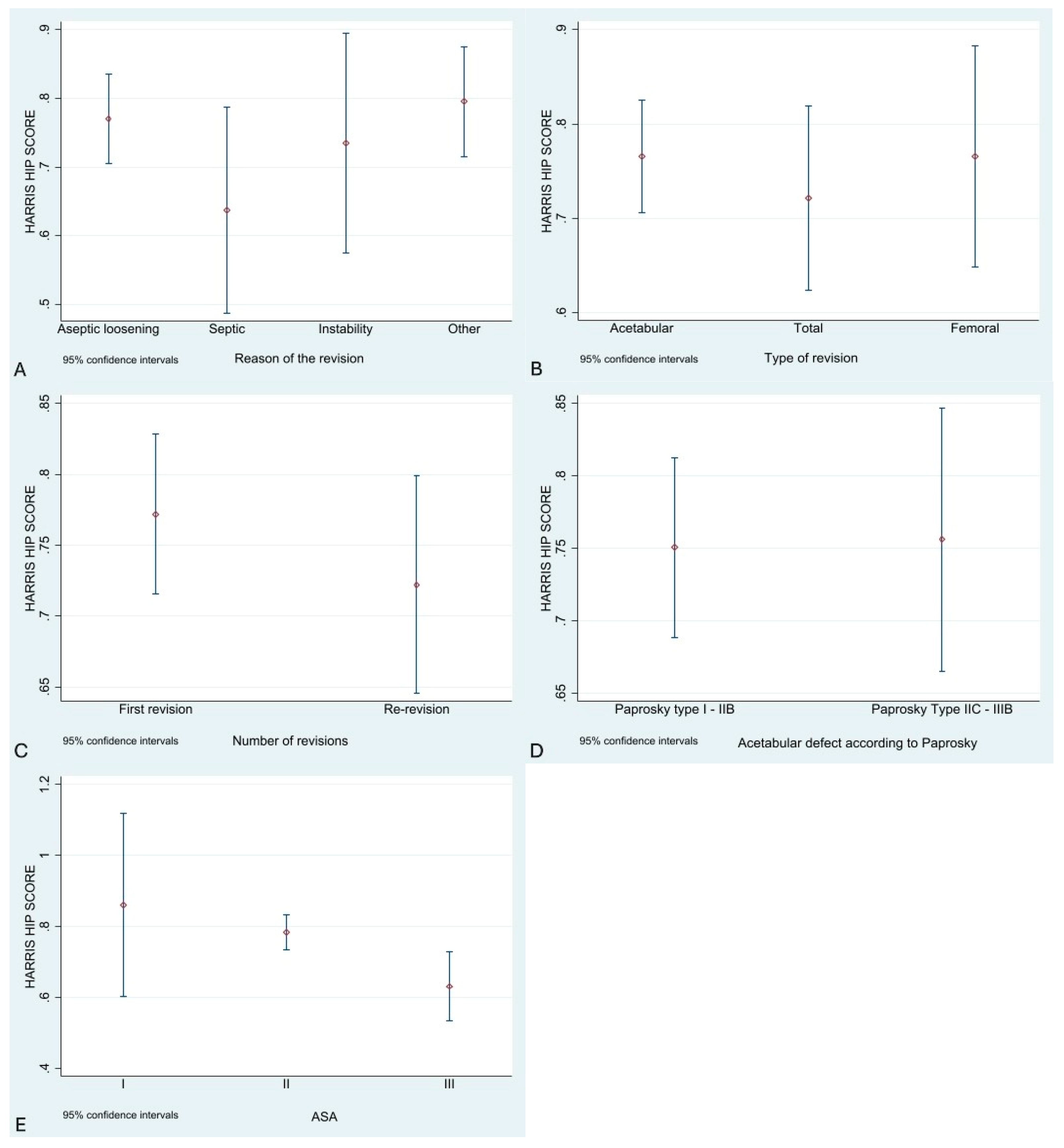
3.3. Functional Results (HHS)
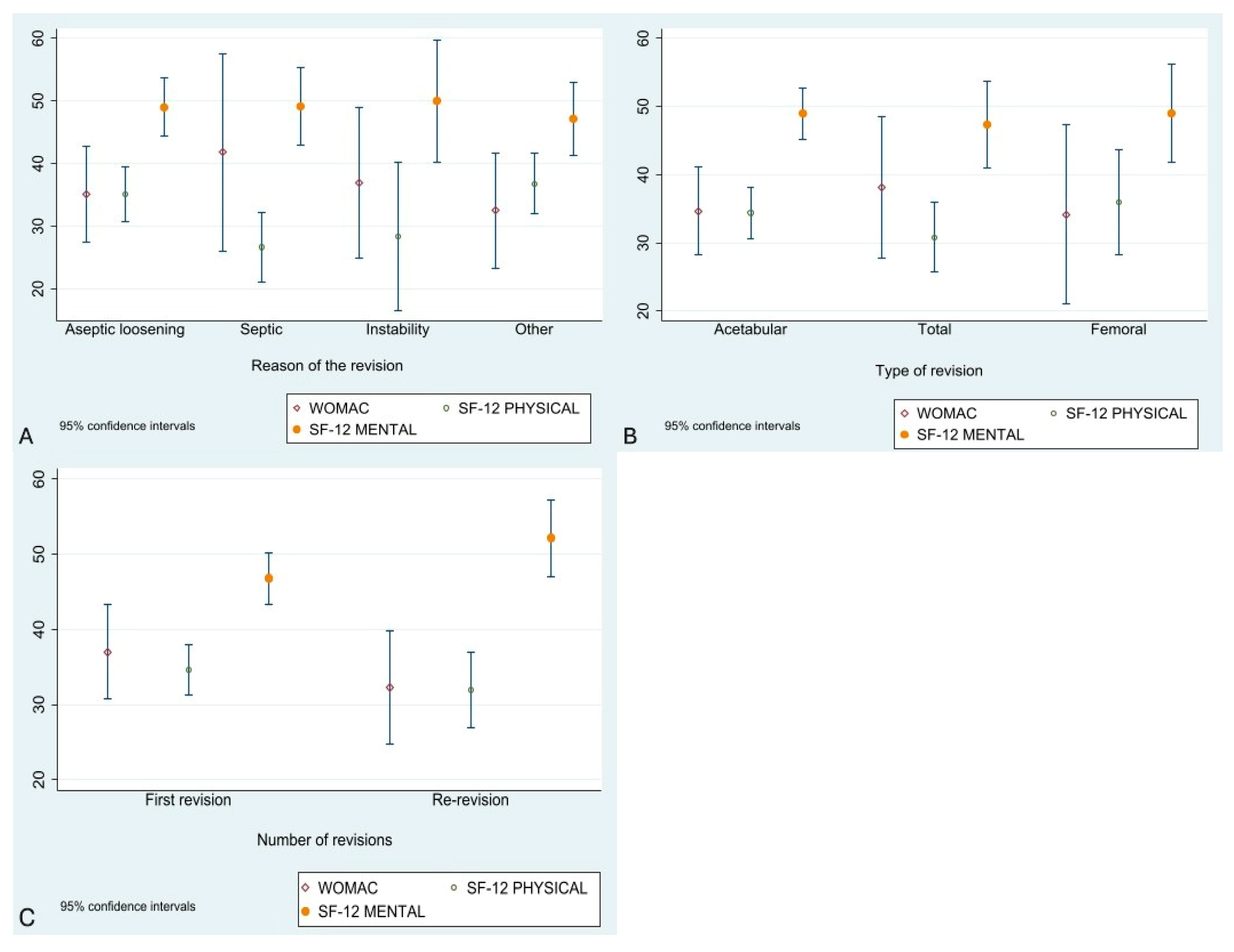
3.4. Patient-Reported Outcomes
3.5. Complications
3.5.1. Infection
3.5.2. Dislocation
3.5.3. Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| CoR | Center of Rotation |
| HHS | Harris Hip Score |
| RR | Relative Risk |
| rTHA | Revision Total Hip Arthroplasty |
| SF-12 | Short Form 12 |
| WOMAC | Western Ontario and McMaster Universities Arthritis Index |
References
- Moleon, M. Revisión del Componente Acetabular en Prótesis de Cadera; Hospitales Universitarios Virgen del Rocío: Sevilla, Spain, 2015; pp. 1–659. [Google Scholar]
- Abdelaal, M.S.; Restrepo, C.; Sharkey, P.F. Global Perspectives on Arthroplasty of Hip and Knee Joints. Orthop. Clin. N. Am. 2020, 51, 169–176. [Google Scholar] [CrossRef]
- Pivec, R.; Johnson, A.J.; Mears, S.C.; Mont, M.A. Hip arthroplasty. Lancet 2012, 380, 1768–1777. [Google Scholar] [CrossRef]
- Reid, C.; Grobler, G.; Dower, B.; Nortje, M.; Walters, J. Revision total hip arthroplasty: Addressing acetabular bone loss. SA Orthop. J. 2012, 11, 34–46. [Google Scholar]
- Innocenti, M.; Smulders, K.; Willems, J.H.; Goosen, J.H.M.; van Hellemondt, G. Patient-reported outcome measures, complication rates, and re-revision rates are not associated with the indication for revision total hip arthroplasty: A prospective evaluation of 647 consecutive patients. Bone Jt. J. 2022, 104, 859–866. [Google Scholar] [CrossRef]
- Lübbeke, A.; Katz, J.N.; Perneger, T.V.; Hoffmeyer, P. Primary and revision hip arthroplasty: 5-Year outcomes and influence of age and comorbidity. J. Rheumatol. 2007, 34, 394–400. [Google Scholar]
- Johnston, R.C.; Brand, R.A.; Crowninshield, R.D. Reconstruction of the hip. A mathematical approach to determine optimum geometric relationships. J. Bone Jt. Surg. 1979, 61, 639–652. [Google Scholar] [CrossRef]
- Raut, V.V.; Siney, P.D.; Wroblewski, B.M. Cemented Charnley revision arthroplasty for severe femoral osteolysis. J. Bone Jt. Surg. Br. Vol. 1995, 77, 362–365. [Google Scholar] [CrossRef]
- Rosenberg, A.G. Cementless acetabular components: The gold standard for socket revision. J. Arthroplast. 2003, 18 (Suppl. 1), 118–120. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration, HHS. Guidance for Industry Use in Medical Product Development to Support Labeling Claims Guidance for Industry. Clin. Fed. Regist. 2009, 1–39. [Google Scholar]
- Saleh, K.J.; Holtzman, J.; Gafni, A.; Saleh, L.; Jaroszynski, G.; Wong, P.; Woodgate, I.; Davis, A.; Gross, A.E. Development, test reliability and validation of a classification for revision hip arthroplasty. J. Orthop. Res. 2001, 19, 50–56. [Google Scholar] [CrossRef]
- Paprosky, W.G.; Perona, P.G.; Lawrence, J.M. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J. Arthroplast. 1994, 9, 33–44. [Google Scholar] [CrossRef]
- Lyman, S.; Lee, Y.Y.; Franklin, P.D.; Li, W.; Mayman, D.J.; Padgett, D.E. Validation of the HOOS, JR: A Short-form Hip Replacement Survey. Clin. Orthop. Relat. Res. 2016, 474, 1472–1482. [Google Scholar] [CrossRef]
- Klässbo, M.; Larsson, E.; Mannevik, E. Hip disability and osteoarthritis outcome score: An extension of the Western Ontario and McMaster Universities Osteoarthritis Index. Scand. J. Rheumatol. 2003, 32, 46–51. [Google Scholar] [CrossRef]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar]
- Sánchez, F.I.; Abellan, J.M.; Martínez, J.E.; Méndez, I. Estimación de un Algoritmo para el Cálculo de Utilidades de Estados de Salud Descritos Mediante el SF-6D (SF-36); Universidad de Murcia: Murcia, Spain, 2008. [Google Scholar]
- Biring, G.S.; Masri, B.A.; Greidanus, N.V.; Duncan, C.P.; Garbuz, D.S. Predictors of quality of life outcomes after revision total hip replacement. J. Bone Jt. Surg. Br. Vol. 2007, 89, 1446–1451. [Google Scholar] [CrossRef]
- Davis, A.M.; Agnidis, Z.; Badley, E.; Kiss, A.; Waddell, J.a.P.; Gross, A.E. Predictors of Functional Outcome Two Years Following Revision Hip Arthroplasty. J. Bone Jt. Surg. 2006, 88, 685–691. [Google Scholar]
- Harada, S.; Hamai, S.; Shiomoto, K.; Hara, D.; Fujii, M.; Ikemura, S.; Motomura, G.; Nakashima, Y. Patient-reported outcomes after primary or revision total hip arthroplasty: A propensity score-matched Asian cohort study. PLoS ONE 2021, 16, e0252112. [Google Scholar] [CrossRef] [PubMed]
- Roessler, P.P.; Jaenisch, M.; Kuhlmann, M.; Wacker, M.; Johannes Wagenhäuser, P.; Gravius, S.; Wirtz, D.C. The augment-and-modular-cage revision system for reconstruction of severe acetabular defects—Two-year clinical and radiographic results. Int. Orthop. 2019, 43, 2269–2278. [Google Scholar] [CrossRef] [PubMed]
- Philpott, A.; Weston-Simons, J.S.; Grammatopoulos, G.; Bejon, P.; Gill, H.S.; McLardy-Smith, P.; Gundle, R.; Murray, D.; Pandit, H. Predictive outcomes of revision total hip replacement—A consecutive series of 1176 patients with a minimum 10-year follow-up. Maturitas 2014, 77, 185–190. [Google Scholar] [CrossRef]
- Driscoll, D.A.; Anderson, C.G.; Bornes, T.D.; Nocon, A.; Bostrom, M.P.G.; Sculco, T.P.; Sculco, P.K. Does Acetabular Bone Loss Severity Associate With Patient-Reported Outcome Measures and Reoperation Rate in Revision Total Hip Arthroplasty? J. Arthroplast. 2023, 38, S189–S193. [Google Scholar] [CrossRef] [PubMed]
- Golinelli, D.; Grassi, A.; Tedesco, D.; Sanmarchi, F.; Rosa, S.; Rucci, P.; Amabile, M.; Cosentino, M.; Bordini, B.; Fantini, M.P.; et al. Patient reported outcomes measures (PROMs) trajectories after elective hip arthroplasty: A latent class and growth mixture analysis. J. Patient-Rep. Outcomes 2022, 6, 95. [Google Scholar] [CrossRef] [PubMed]
- Fortin, P.R.; Clarke, A.E.; Joseph, L.; Liang, M.H.; Tanzer, M.; Ferland, D.; Phillips, C.; Partridge, A.J.; Bélisle, P.; Fossel, A.H.; et al. Outcomes of total hip and knee replacement: Preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999, 42, 1722–1728. [Google Scholar] [CrossRef]
- Chen, L.; Zhou, Y.; Zhang, L.; Huang, Y.; Tang, H. Revision total hip arthroplasty in patients with ankylosing spondylitis: Mid-term results. Orthop. Traumatol. Surg. Res. 2022, 109, 103504. [Google Scholar] [CrossRef] [PubMed]
- Tirumala, V.; Klemt, C.; van den Kieboom, J.; Xiong, L.; Kwon, Y.M. Comparison of patient reported outcome measures after single versus two-stage revision for chronic infection of total hip arthroplasty: A retrospective propensity score matched cohort study. Arch. Orthop. Trauma Surg. 2021, 141, 1789–1796. [Google Scholar] [CrossRef]
- Josipović, P.; Moharič, M.; Salamon, D. Translation, cross-cultural adaptation and validation of the Slovenian version of Harris Hip Score. Health Qual. Life Outcomes 2020, 18, 335. [Google Scholar] [CrossRef]
- Dettoni, F.; Pellegrino, P.; La Russa, M.R.; Bonasia, D.E.; Blonna, D.; Bruzzone, M.; Castoldi, F.; Rossi, R. Validation and cross cultural adaptation of the Italian version of the harris hip score. Hip Int. 2015, 25, 91–97. [Google Scholar] [CrossRef]
- Peña, P.; Ortega, M.A.; Buján, J.; De la Torre, B. Influence of psychological distress in patients with hypoallergenic total knee arthroplasty. Treatment algorithm for patients with metal allergy and knee osteoarthritis. Int. J. Environ. Res. Public Health 2021, 18, 5997. [Google Scholar] [CrossRef]
- Peña, P.; Ortega, M.A.; Buján, J.; De la Torre, B. Decrease of quality of life, functional assessment and associated psychological distress in patients with hypoallergenic total knee arthroplasty. J. Clin. Med. 2020, 9, 3270. [Google Scholar] [CrossRef] [PubMed]
- Laughlin, M.S.; Vidal, E.A.; Drtil, A.A.; Goytia, R.N.; Mathews, V.; Patel, A.R. Mortality After Revision Total Hip Arthroplasty. J. Arthroplast. 2021, 36, 2353–2358. [Google Scholar] [CrossRef]
- Lübbeke, A.; Roussos, C.; Barea, C.; Köhnlein, W.; Hoffmeyer, P. Revision Total Hip Arthroplasty in Patients 80 Years or Older. J. Arthroplast. 2012, 27, 1041–1046. [Google Scholar] [CrossRef]
- Jones, M.D.; Parry, M.; Whitehouse, M.R.; Blom, A.W. Early death following revision total hip arthroplasty. Hip Int. 2018, 28, 400–406. [Google Scholar] [CrossRef]
- Badarudeen, S.; Shu, A.C.; Ong, K.L.; Baykal, D.; Lau, E.; Malkani, A.L. Complications After Revision Total Hip Arthroplasty in the Medicare Population. J. Arthroplast. 2017, 32, 1954–1958. [Google Scholar] [CrossRef]
- Strehle, J.; DelNotaro, C.; Orler, R.; Isler, B. The outcome of revision hip arthroplasty in patients older than age 80 years: Complications and social outcome of different risk groups. J. Arthroplast. 2000, 15, 690–697. [Google Scholar] [CrossRef]
- Parvizi, J.; Pour, A.E.; Keshavarzi, N.R.; D’Apuzzo, M.; Sharkey, P.F.; Hozack, W.J. Revision Total Hip Arthroplasty in Octogenarians. J. Bone Jt. Surg. Am. Vol. 2007, 89, 2612–2618. [Google Scholar] [CrossRef]
- Radcliffe, G.S.; Tomichan, M.C.; Andrews, M.; Stone, M.H. Revision hip surgery in the elderly: Is it worthwhile? J. Arthroplast. 1999, 14, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.J.; Kremers, H.M.; Abdel, M.P.; Larson, D.R.; Ransom, J.E.; Berry, D.J.; Lewallen, D.G. Long-term Mortality after Revision THA. Clin. Orthop. Relat. Res. 2018, 476, 420–4266. [Google Scholar] [CrossRef] [PubMed]
- Bovonratwet, P.; Malpani, R.; Ottesen, T.D.; Tyagi, V.; Ondeck, N.T.; Rubin, L.E.; Grauer, J.N. Aseptic revision total hip arthroplasty in the elderly: Quantifying the risks for patients over 80 years old. Bone Jt. J. 2018, 100B, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.; Garbuz, D.S.; Greidanus, N.V.; Masri, B.A.; Duncan, C.P. Quality of Life Outcomes in Revision vs Primary Total Hip Arthroplasty. A Prospective Cohort Study. J. Arthroplast. 2008, 23, 550–553. [Google Scholar] [CrossRef]
| Mean or n (SD) | Min–Max or % | |
|---|---|---|
| Age | 74.93 (±13.38) | 34–97 |
| BMI | 26.96 (±6.49) | 16.6–44 |
| Type of revision | ||
| 73 | 49.0% |
| 32 | 21.47% |
| 44 | 29.53% |
| Sex | Male: 66 | 44.3% |
| Female: 83 | 65.7% | |
| ASA | ASA I: 10 | 6.71% |
| ASA II: 91 | 61.07% | |
| ASA III: 45 | 30.2% | |
| ASA IV: 3 | 2.01% | |
| Reason for primary arthroplasty | Coxarthrosis: 78 | 55.71% |
| NAV: 11 | 7.85% | |
| Fracture: 26 | 18.67% | |
| Other: 25 | 16.10% | |
| Reason for revision | Dislocation: 18 | 12.08% |
| Fracture: 8 | 5.37% | |
| Loosening: 63 | 42.28% | |
| Wear: 12 | 8.05% | |
| Pain: 8 | 5.37% | |
| Infection: 20 | 13.42% | |
| Rupture: 8 | 5.37% | |
| Cotyloiditis: 3 | 2.01% | |
| Other: 9 | 6.04% | |
| Acetabular defect according to Paprosky | I–IIB: 88 | 75.23% |
| IIC–IIIB: 29 | 24.77% | |
| Acetabular defect according to Saleh | I–II: 83 | 70.94% |
| III–V: 34 | 29.06% | |
| Functional assessment | mean (SD) | Min–Max |
| Harris Hip Score | 0.75 (0.20) | 0.34–1 |
| WOMAC total | 35.47 (20.72) | 0–82 |
| SF-12 | ||
| 33.72 (11.71) | 15.02–63.46 |
| 48.53 (12.20) | 15.26–66.67 |
| Complications | n (%) | |
| Post-revision infection | Early (1 month): 3 (2.04%) Late: 4 (2.72%) | |
| Hip dislocation | Early (3 months): 13 (8.78%) Late: 3 (2.04%) | |
| Mortality | Early: 4 (2.01%) Total: 29 (19.59%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casas-Gallego, V.; Ortega, M.A.; de la Torre-Escuredo, B.J. Is There Agreement Between Clinical Outcomes as Perceived by the Surgeon and the Patient in Revision Total Hip Arthroplasty? J. Clin. Med. 2025, 14, 7488. https://doi.org/10.3390/jcm14217488
Casas-Gallego V, Ortega MA, de la Torre-Escuredo BJ. Is There Agreement Between Clinical Outcomes as Perceived by the Surgeon and the Patient in Revision Total Hip Arthroplasty? Journal of Clinical Medicine. 2025; 14(21):7488. https://doi.org/10.3390/jcm14217488
Chicago/Turabian StyleCasas-Gallego, Víctor, Miguel A. Ortega, and Basilio J. de la Torre-Escuredo. 2025. "Is There Agreement Between Clinical Outcomes as Perceived by the Surgeon and the Patient in Revision Total Hip Arthroplasty?" Journal of Clinical Medicine 14, no. 21: 7488. https://doi.org/10.3390/jcm14217488
APA StyleCasas-Gallego, V., Ortega, M. A., & de la Torre-Escuredo, B. J. (2025). Is There Agreement Between Clinical Outcomes as Perceived by the Surgeon and the Patient in Revision Total Hip Arthroplasty? Journal of Clinical Medicine, 14(21), 7488. https://doi.org/10.3390/jcm14217488






