Alterations in the Temporomandibular Joint Space Following Orthognathic Surgery Based on Cone Beam Computed Tomography: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
- Population (P): Patients qualified for orthognathic surgery (with or without orthodontic preparation).
- Exposure (E): Orthognathic surgical procedures, including Le Fort I osteotomy, BSSO, intraoral vertical ramus osteotomy (IVRO), and high oblique sagittal split osteotomy (HSSO).
- Comparator (C): Preoperative TMJ space measurements.
- Outcome (O): Quantitative changes in TMJ space, measured in the sagittal and/or coronal planes using CBCT.
2.3. Data Sources
2.4. Search Strategy
2.5. Study Selection
2.6. Data Extraction
2.7. Risk of Bias and Quality Assessment
3. Results
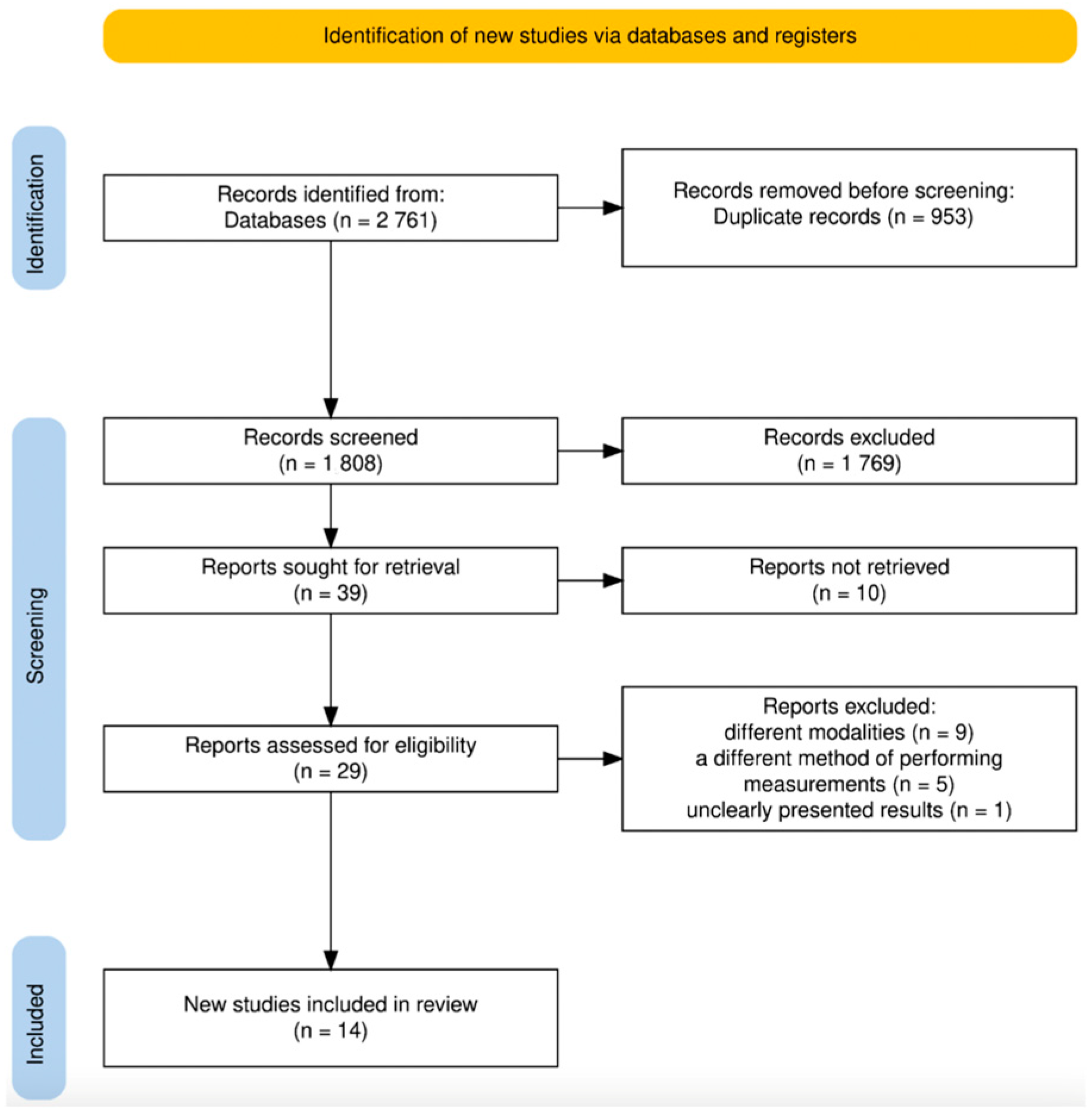
3.1. Search Results
3.2. Study Characteristics
3.3. Risk of Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TMJ | Temporomandibular joint |
| TMDs | Temporomandibular disorders |
| AJS | Anterior joint space |
| SJS | Superior joint space |
| PJS | Posterior joint space |
| LJS | Lateral joint space |
| MJS | Medial joint space |
| OSA | Obstructive sleep apnea |
| BSSO | Bilateral sagittal split osteotomy |
| IVRO | Intraoral vertical ramus osteotomy |
| HSSO | High oblique sagittal split osteotomy |
References
- American Association of Oral and Maxillofacial Surgeons (AAOMS). Indications for Orthognathic Surgery. 2025. Available online: https://aaoms.org/wp-content/uploads/2025/01/ortho_indications.pdf (accessed on 1 September 2025).
- Moorhead, A.; Winters, R.; Serra, M. Le Fort Osteotomy. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK564372/ (accessed on 1 September 2025).
- Monson, L.A. Bilateral sagittal split osteotomy. Plast. Reconstr. Surg. 2013, 131, 968e–970e. [Google Scholar] [CrossRef]
- Jain, D.; Datana, S.; Chopra, S.S. Long-term skeletal stability of mandibular surgery with bilateral sagittal split ramus osteotomy—Advancement versus setback: A systematic review and meta-analysis. J. Indian Orthod. Soc. 2024, 58, 112–124. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Ellis, E., 3rd. Is there a difference in stability or neurosensory function between bilateral sagittal split osteotomy and intraoral vertical ramus osteotomy? J. Oral Maxillofac. Surg. 2015, 73, 1360–1371. [Google Scholar] [CrossRef] [PubMed]
- Hanna, T. Hanna’s modified sagittal split osteotomy (HSSO):An Alternative to Inverted L Osteotomy-Merging Function and Aesthetics for Enhanced Stability, Attractiveness, and Nerve Protection. J. Clin. Med. 2024, 13, 3438. [Google Scholar] [CrossRef]
- Bordoni, B.; Varacallo, M. Anatomy, Head and Neck, Temporomandibular Joint. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK538489/ (accessed on 1 September 2025).
- Lekaviciute, R.; Kriauciunas, A. Relationship Between Occlusal Factors and Temporomandibular Disorders: A Systematic Literature Review. Cureus 2024, 16, e54130. [Google Scholar] [CrossRef]
- Kapos, F.P.; Exposto, F.G.; Oyarzo, J.F.; Durham, J. Temporomandibular disorders: A review of current concepts in aetiology, diagnosis and management. Oral Surg. 2020, 13, 321–334. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.K.; MacBarb, R.F.; Wong, M.E.; Athanasiou, K.A. Temporomandibular disorders: A review of etiology, clinical management, and tissue engineering strategies. Int. J. Oral Maxillofac. Implants 2013, 28, e393–e414. [Google Scholar] [CrossRef]
- Xiao, M.; Yue, Q.; Qin, Z.; Hang, X.; Chen, X.; Ni, S. Unbalanced occlusal loading elicited remodeling responses in growing rat temporomandibular joints and Notch1/Hes1 signaling pathway expression. BMC Oral Health 2025, 25, 267. [Google Scholar] [CrossRef]
- Garrigós-Pedrón, M.; Elizagaray-García, I.; Domínguez-Gordillo, A.A.; Del-Castillo-Pardo-de-Vera, J.L.; Gil-Martínez, A. Temporomandibular disorders: Improving outcomes using a multidisciplinary approach. J. Multidiscip. Healthc. 2019, 12, 733–747. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Ma, L.L.; Wang, Y.Y.; Yang, Z.H.; Huang, D.; Weng, H.; Zeng, X.T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef] [PubMed]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef]
- Yang, W.; Chen, Y.; Li, J.; Jiang, N. Assessment of condylar positional changes in severe skeletal class II malocclusion after surgical-orthodontic treatment. Clin. Oral Investig. 2023, 27, 3683–3693. [Google Scholar] [CrossRef]
- Zhang, Y.L.; Liu, Y.; Shu, J.H.; Xu, X.C.; Liu, Z. Morphological study of the changes after sagittal split ramus osteotomy in patients with facial asymmetry: Measurements of 3-dimensional modelling. Br. J. Oral Maxillofac. Surg. 2018, 56, 925–930. [Google Scholar] [CrossRef]
- Chen, S.; Lei, J.; Wang, X.; Fu, K.Y.; Farzad, P.; Yi, B. Short- and long-term changes of condylar position after bilateral sagittal split ramus osteotomy for mandibular advancement in combination with Le Fort I osteotomy evaluated by cone-beam computed tomography. J. Oral Maxillofac. Surg. 2013, 71, 1956–1966. [Google Scholar] [CrossRef]
- Huang, L.; Tang, S.; Zou, R.; Ouyang, K.X.; Piao, Z. The three-dimensional evaluation of positional change in mandibular condyle after intraoral vertical ramus osteotomy. J. Stomatol. Oral Maxillofac. Surg. 2021, 122, 477–481. [Google Scholar] [CrossRef]
- Vogl, T.J.; Zyada, W.; Helal, R.; Naguib, N.N.; Lingwal, N.; Nour-Eldin, N.-E.A. Pre- and Post-Operative Cone Beam Computed Tomography Assessment of the Temporomandibular Joint in Patients with Orthognathic Surgery. Diagnostics 2024, 14, 1389. [Google Scholar] [CrossRef]
- Kuehle, R.; Berger, M.; Saure, D.; Hoffmann, J.; Seeberger, R. High oblique sagittal split osteotomy of the mandible: Assessment of the positions of the mandibular condyles after orthognathic surgery based on cone-beam tomography. Br. J. Oral Maxillofac. Surg. 2016, 54, 638–642. [Google Scholar] [CrossRef] [PubMed]
- Han, S.-H.; Park, J.H.; Seo, H.Y.; Chae, J.-M. Temporomandibular Joint Space Changes in Skeletal Class III Malocclusion Patients with Orthognathic Surgery. Appl. Sci. 2023, 13, 9241. [Google Scholar] [CrossRef]
- Kim, Y.-I.; Cho, B.-H.; Jung, Y.-H.; Son, W.-S.; Park, S.-B. Cone-beam computerized tomography evaluation of condylar changes and stability following two-jaw surgery: Le Fort I osteotomy and mandibular setback surgery with rigid fixation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 111, 681–687. [Google Scholar] [CrossRef]
- Abbasi, A.J.; Azadbakht, M.; Mosavat, F.; Bayati, M. Cone-Beam Computed Tomography Evaluation of the Mandibular Condyle and Articular Spaces Following Orthognathic Surgery Using Freehand Articulation Method in Patients With Class II and III Skeletal Deformity. Int. J. Dent. 2024, 2024, 4269097. [Google Scholar] [CrossRef]
- Tabrizi, R.; Shahidi, S.; Bahramnejad, E.; Arabion, H. Evaluation of Condylar Position after Orthognathic Surgery for Treatment of Class II Vertical Maxillary Excess and Mandibular Deficiency by Using Cone-Beam Computed Tomography. J. Dent. 2016, 17, 318–325. [Google Scholar]
- Ravelo, V.; Olate, G.; de Moraes, M.; Huentequeo, C.; Sacco, R.; Olate, S. Condylar Positional Changes in Skeletal Class II and Class III Malocclusions after Bimaxillary Orthognathic Surgery. J. Pers. Med. 2023, 13, 1544. [Google Scholar] [CrossRef]
- da Silva, R.J.; Valadares Souza, C.V.; Souza, G.A.; Ambrosano, G.M.B.; Freitas, D.Q.; Sant’Ana, E.; de Oliveira-Santos, C. Changes in condylar volume and joint spaces after orthognathic surgery. Int. J. Oral Maxillofac. Surg. 2018, 47, 511–517. [Google Scholar] [CrossRef]
- Roman, R.; Almășan, O.; Hedeșiu, M.; Băciuț, M.; Bran, S.; Popa, D.; Ban, A.; Dinu, C. Evaluation of the Mandibular Condyle Morphologic Relation before and after Orthognathic Surgery in Class II and III Malocclusion Patients Using Cone Beam Computed Tomography. Biology 2022, 11, 1353. [Google Scholar] [CrossRef]
- Meral, S.E.; Koç, O.; Tosun, E.; Tüz, H.H. Effects of sagittal split ramus osteotomy on condylar position and ramal orientation in patients with mandibular asymmetry. Clin. Oral Investig. 2023, 28, 65. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Wolford, L.M.; Perez, D.; Laskin, D.M.; Ellis, E., 3rd. Does Orthognathic Surgery Cause or Cure Temporomandibular Disorders? A Systematic Review and Meta-Analysis. J. Oral Maxillofac. Surg. 2017, 75, 1835–1847. [Google Scholar] [CrossRef] [PubMed]
- Meger, M.; Fatturi, A.; Gerber, J.; Weiss, S.; Rocha, J.; Scariot, R.; Wambier, L. Impact of orthognathic surgery on quality of life of patients with dentofacial deformity: A systematic review and meta-analysis. Br. J. Oral Maxillofac. Surg. 2021, 59, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Coclici, A.; Hedeşiu, M.; Bran, S.; Băciuţ, M.; Dinu, C.; Rotaru, H.; Roman, R. Early and long-term changes in the muscles of the mandible following orthognathic surgery. Clin. Oral Investig. 2019, 23, 3437–3444. [Google Scholar] [CrossRef] [PubMed]
- Enami, K.; Yamada, K.; Kageyama, T.; Taguchi, A. Morphological changes in the temporomandibular joint before and after sagittal splitting ramus osteotomy of the mandible for skeletal mandibular protrusion. Cranio 2013, 31, 123–132. [Google Scholar] [CrossRef]
- Park, S.B.; Yang, Y.M.; Kim, Y.I.; Cho, B.H.; Jung, Y.H.; Hwang, D.S. Effect of bimaxillary surgery on adaptive condylar head remodeling: Metric analysis and image interpretation using cone-beam computed tomography volume superimposition. J. Oral Maxillofac. Surg. 2012, 70, 1951–1959. [Google Scholar] [CrossRef]
- Dolwick, M.F.; Widmer, C.G. Orthognathic Surgery as a Treatment for Temporomandibular Disorders. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 303–323. [Google Scholar] [CrossRef]
- Uetanabaro, L.C.; Gerber, J.T.; dos Santos, K.M.; Meger, M.N.; da Costa, D.J.; Küchler, E.C.; Sebastiani, A.M.; Scariot, R. Prevalence and associated factors of myofascial pain in orthognathic patients with skeletal class II malocclusion. Oral Maxillofac. Surg. 2023, 27, 25–31. [Google Scholar] [CrossRef]
- Ferri, J.; Nicot, R.; Maes, J.M.; Raoul, G.; Lauwers, L. Condylar resorptions and orthodontic-surgical treatment: State of the art. Int. Orthod. 2016, 14, 503–527. [Google Scholar] [CrossRef]
- Kim, Y.-J.; Oh, K.-M.; Hong, J.-S.; Lee, J.-H.; Kim, H.-M.; Reyes, M.; Cevidanes, L.H.; Park, Y.-H. Do patients treated with bimaxillary surgery have more stable condylar positions than those who have undergone single-jaw surgery? J. Oral Maxillofac. Surg. 2012, 70, 2143–2152. [Google Scholar] [CrossRef] [PubMed]
- Dujoncquoy, J.P.; Ferri, J.; Raoul, G.; Kleinheinz, J. Temporomandibular joint dysfunction and orthognathic surgery: A retrospective study. Head Face Med. 2010, 6, 27. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Turvey, T.A.; Phillips, C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: An update and extension. Head Face Med. 2007, 3, 21. [Google Scholar] [CrossRef] [PubMed]
- Moroi, A.; Yoshizawa, K.; Iguchi, R.; Ikawa, H.; Kosaka, A.; Hotta, A.; Tsutsui, T.; Saida, Y.; Ueki, K. The amount of mandibular setback influence on occlusal force following sagittal split ramus osteotomy. J. Craniomaxillofac. Surg. 2015, 43, 1743–1748. [Google Scholar] [CrossRef]
- Tseng, Y.C.; Hsu, K.J.; Chen, K.K.; Wu, J.H.; Chen, C.M. Relationship between Frontal Gap and Postoperative Stability in the Treatment of Mandibular Prognathism. Biomed. Res. Int. 2016, 2016, 7046361. [Google Scholar] [CrossRef]
- Verhelst, P.J.; Van der Cruyssen, F.; De Laat, A.; Jacobs, R.; Politis, C. The Biomechanical Effect of the Sagittal Split Ramus Osteotomy on the Temporomandibular Joint: Current Perspectives on the Remodeling Spectrum. Front. Physiol. 2019, 10, 1021. [Google Scholar] [CrossRef] [PubMed]
- Chae, J.M.; Park, J.H.; Tai, K.; Mizutani, K.; Uzuka, S.; Miyashita, W.; Seo, H.Y. Evaluation of condyle-fossa relationships in adolescents with various skeletal patterns using cone-beam computed tomography. Angle Orthod. 2020, 90, 224–232. [Google Scholar] [CrossRef]
- Paknahad, M.; Shahidi, S. Association between condylar position and vertical skeletal craniofacial morphology: A cone beam computed tomography study. Int. Orthod. 2017, 15, 740–751. [Google Scholar] [CrossRef] [PubMed]
- Diwakar, R.; Bucci, R.; Kaushik, A.; Bansal, A.; Bucci, P.; Kochhar, A.S.; Spagnuolo, G. Three-Dimensional Assessment of Temporomandibular Joint Morphology and Facial Asymmetry in Individuals with Different Vertical Skeletal Growth Patterns. Int. J. Environ. Res. Public Health 2023, 20, 1437. [Google Scholar] [CrossRef]
- Noh, K.J.; Baik, H.S.; Han, S.S.; Jang, W.; Choi, Y.J. Differences in mandibular condyle and glenoid fossa morphology in relation to vertical and sagittal skeletal patterns: A cone-beam computed tomography study. Korean J. Orthod. 2021, 51, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Alhammadi, M.S.; Fayed, M.S.; Labib, A. Three-dimensional assessment of temporomandibular joints in skeletal Class I, Class II, and Class III malocclusions: Cone beam computed tomography analysis. J. World Fed. Orthod. 2016, 5, 80–86. [Google Scholar] [CrossRef]
- Major, P.W.; Kinniburgh, R.D.; Nebbe, B.; Prasad, N.G.; Glover, K.E. Tomographic assessment of temporomandibular joint osseous articular surface contour and spatial relationships associated with disc displacement and disc length. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 152–161. [Google Scholar] [CrossRef]
- Hall, H.D.; Indresano, A.T.; Kirk, W.S.; Dietrich, M.S. Prospective multicenter comparison of four temporomandibular joint operations. J. Oral Maxillofac. Surg. 2005, 63, 1174–1179. [Google Scholar] [CrossRef]
- Hall, H.D.; Navarro, E.Z.; Gibbs, S.J. One- and three-year prospective outcome study of modified condylotomy for treatment of reducing disc displacement. J. Oral Maxillofac. Surg. 2000, 58, 7–17. [Google Scholar] [CrossRef]
- Hall, H.D.; Navarro, E.Z.; Gibbs, S.J. Prospective study of modified condylotomy for treatment of nonreducing dis displacement. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000, 89, 147–158. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Studies involved patients undergoing orthognathic surgery, specifically Le Fort I osteotomy, BSSO, and/or IVRO and/or HSSO. | Studies that assessed TMJ space only at a single time measurement (i.e., either preoperative or postoperative only) and/or measured non-comparable anatomical reference points. |
| Studies that reported TMJ space measurements acquired at least twice, both preoperatively and postoperatively. | Studies that used methods relying on superimposed 3D models for TMJ space evaluation. |
| Studies that assessed joint space dimensions in the sagittal and/or coronal planes, using consistent anatomical reference points to obtain measurements of anterior, posterior, superior, medial, or lateral joint spaces. | Pilot studies, ex vivo studies, cross-sectional studies, review articles, pre-prints, editorials, conference abstracts. |
| Retrospective pre–post studies. | The full text of the article was not accessible. |
| The full-text is accessible. |
| Author, Study Location, and Year of Publication | Sample Size–Skeletal Class, Age, Gender | Type of Procedure | CBCT Parameters | Time of CBCT Before/After | Preoperative Measurements in the Sagittal Plane (mm) | Postoperative Measurements in the Sagittal Plane (mm) | p-Value | Preoperative Measurements in the Coronal Plane (mm) | Postoperative Measurements in the Coronal Plane (mm) | p-Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kim et al., South Korea, 2010 [24] | 26 patients 26 class III 14 females 12 males mean age: 21.30 ± 4.38 | 26 BSSO + Le Fort I | DCT Pro (Vatech, Seoul, Republic of Korea) 20 × 19 cm field of view, 90 kVp, 4 mA | T0 presurgery T1 postsurgery 6 months T2 follow-up 18 months | T0 AJS (R) 1.81 AJS (L) 1.68 SJS (R) 2.67 SJS (L) 2.67 PJS (R) 2.43 PJS (L) 2.69 | T1 AJS (R) 2.40 AJS (L) 2.25 SJS (R) 2.70 SJS (L) 2.68 PJS (R) 2.28 PJS (L) 2.18 | T2 AJS (R) 1.88 AJS (L) 1.92 SJS (R) 2.42 SJS (L) 2.69 PJS (R) 2.25 PJS (L) 2.44 | 0.04 * 0.01 * 0.46 0.99 0.70 0.23 | NR | NR | NR | |||||
| Chen et al., People’s Republic of China, 2013 [19] | 27 patients 27 class II mean age: 27.0 ± 5.4 | 27 BSSO + Le Fort I | DCT Pro (Vatech, Seoul, Republic of Korea) 16 × 10 cm field of view, 90 kVp, 7.0 mA | T0 1 week before T1 3–5 days after surgery T2 3 months after T3 12 ± 3 month after | T0 AJS (R) 2.39 AJS (L) 2.20 SJS (R) 2.97 SJS (L) 2.84 PJS (R) 2.79 PJS (L) 2.71 | T1 AJS (R) 3.31 AJS (L) 3.33 SJS (R) 3.90 SJS (L) 3.71 PJS (R) 2.66 PJS (L) 2.74 | T2 AJS (R) 2.35 AJS (L) 2.24 SJS (R) 2.51 SJS (L) 2.41 PJS (R) 2.18 PJS (L) 2.16 | T3 AJS (R) 2.39 AJS (L) 2.23 SJS (R) 2.46 SJS (L) 2.34 PJS (R) 2.17 PJS (L) 2.10t | T1–T0 p < 0.05 T1–T0 p < 0.05 T1–T0 p < 0.05 T2–T1 p < 0.05 T2–T0 p < 0.05 T1–T0 p < 0.05 T2–T1 p < 0.05 T2–T0 p < 0.05 T2–T1 p < 0.05 T2–T1 p < 0.05 | NR | NR | NR | ||||
| Kuehle et al., Germany, 2016 [22] | 50 patients 24 class II 26 class III 32 females 18 males mean age: 26.3 ± 7.4 | 50 HSSO + Le Fort I | Gallileos Comfort plus system (Sirona Dental Systems GmbH, Bensheim, Germany) 15.4 cm × 0.125 mm for each voxel, 98 kV, 3–6 mA | two weeks preoperatively/2–4 days postop- eratively/9 months | changes after surgery CLASS II AJS (R) -0.52 AJS (L) −0.49 SJS (R) −0.29 SJS (L) −0.25 PJS (R) −0.43 PJS (L) −0.33 CLASS III AJS (R) −0.29 AJS (L) −0.52 SJS (R) −0.85 SJS (L) −0.65 PJS (R) −0.97 PJS (L) −0.52 | changes after 9-month follow-up CLASS II AJS (R) 0.03 AJS (L) 0.03 SJS (R) 0.78 SJS (L) 0.68 PJS (R) 0.88 PJS (L) 0.78 CLASS III AJS (R) 0.10 AJS (L) −0.07 SJS (R) −0.01 SJS (L) 0.36 PJS (R) 0.02 PJS (L) 0.19 | 0.20 0.21 0.02 * 0.04 * 0.00 * 0.05 * 0.3 0.4 0.00 * 0.00 * 0.00 * 0.01 * | NR | NR | NR | ||||||
| Tabrizi et al., Iran, 2016 [26] | 22 patients 22 class II 25 females 7 males mean age: 22.18 ± 5.6 | 22 BSSO + Le Fort I | New Tom VGI Flex (Image work Co.; White Plains, NY, USA) 15 × 15 cm with 0.3 mm slice | T0 couple days before surgery T1 one month after surgery T2 9 months after surgery | SJS 3.62 (T0) SJS 3.62 (T0) SJS 4.13 (T1) | SJS 4.13 (T1) SJS 3.80 (T2) SJS 3.80 (T2) | p < 0.05 * p > 0.05 p > 0.05 | NR | NR | NR | ||||||
| Da Silva et al., Brazil, 2018 [28] | 57 patients 57 class II 40 females 17 males mean age: 31.4 | 57 BSSO + Le Fort I | i-CAT Next Generation scanner (Imaging Sciences International, Hatfield, PA, USA) 120 kVp, 5 mA, 23 × 17 cm field of view, 0.4 mm voxel size | Pre-surgical/at least 6 months | AJS 3.5 SJS 2.9 PJS 3.1 | AJS 3.6 SJS 2.6 PJS 2.92 | 0.39 0.00 * 0.12 | MJS 3.8 | MJS 2.93 | <0.00 * | ||||||
| Zhang et al., China, 2018 [18] | 10 patients 10 class III 5 females 5 males mean age: 25.0 | 10 BSSO | CT (KaVo 3D eXam) 120 kVp, 3–8 mA, 0.4 mm | 6 months before/6 months after | AJS (R) 2.71 AJS (L) 2.54 SJS (R) 1.82 SJS (L) 1.71 PJS (R) 2.34 PJS (L) 2.66 | AJS (R) 2.70 AJS (L) 2.53 SJS (R) 2.17 SJS (L) 2.24 PJS (R) 2.56 PJS (L) 2.52 | p > 0.05 p > 0.05 p < 0.01 * p < 0.01 * p > 0.05 p > 0.05 | LJS (R) 2.20 LJS (L) 2.86 MJS (R) 2.27 MJS (L) 1.74 | LJS (R) 2.62 LJS (L) 2.69 MJS (R) 2.41 MJS (L) 2.47 | p < 0.05 * p > 0.05 p > 0.05 p < 0.01 * | ||||||
| Huang et al., China, 2020 [20] | 21 patients 21 class III 11 females 10 males Age: 18–33 | 21 IVRO | NewTom scanner (Imaging Science International, Hatfield, PA, USA) field of view: 200 × 400 mm, 120 kVp, 47.7 mA, 0.4 mm voxel size | T0 before surgery T1 one week after surgery T2 6 months after surgery | T0 AJS (R) 1.56 AJS (L) 1.45 SJS (R) 2.07 SJS (L) 2.19 PJS (R) 1.63 PJS (L) 1.85 | T1 AJS (R) 1.18 AJS (L) 1.14 SJS (R) 4.73 SJS (L) 5.34 PJS (R) 4.18 PJS (L) 4.93 | T2 AJS (R) 1.61 AJS (L) 1.50 SJS (R) 2.72 SJS (L) 3.26 PJS (R) 2.33 PJS (L) 2.74 | NS NS 0.00 * 0.00 * 0.00 * 0.00 * | NR | NR | NR | |||||
| Roman et al., Romania, 2022 [29] | 28 patients 14 class II 14 class III 19 females 9 males mean age: 26.85 ± 6.54 (class II) mean age: 26.64 ± 6.87 (class III) | 28 BSSO + Le Fort I | Promax 3D Max (Planmeca, Helsinki, Finland) 23 × 23 × 16 cm, 0.4 mm voxel size, 86–88 kV, 6–8 mA | T0 before surgery T1 two days after surgery | CLASS II AJS 2.45 PJS 2.75 CLASS III AJS 2.15 PJS 2.01 | CLASS II AJS 2.87 PJS 3.49 CLASS III AJS 2.00 PJS 2.16 | 0.02 * 0.01 * 0.14 0.5 | CLASS II MJS 2.98 CLASS III MJS 2.02 | CLASS II MJS 2.91 CLASS III MJS 2.55 | 0.41 0.01 * | ||||||
| Han et al., Republic of Korea, 2023 [23] | 26 patients 26 class III 15 females 11 males mean age: 19.6 ± 2.8 | 10 BSSO 16 BSSO + Le Fort I | PSR 9000N (Asahi Alphard Vega, Kyoto, Japan) C-mode: Scan size 2003 179 mm; voxel size 0.39 mm; field of view 19.97 cm | T0 pretreatment T1 presurgery T2 postsurgery T3 posttreatment and/or T4 retention (at least 1 year posttreatment) | T0 AJS 1.43 SJS 2.21 PJS 1.56 | T1 AJS 1.57 SJS 2.27 PJS 1.53 | T2 AJS 1.78 SJS 2.30 PJS 1.52 | T3 AJS 1.60 SJS 2.31 PJS 1.53 | T4 AJS 1.64 SJS 2.22 PJS 1.57 | 0.27 0.98 0.99 | T0 MJS 1.96 CJS 2.01 LJS 1.50 | T1 MJS 1.88 CJS 2.04 LJS 1.49 | T2 MJS 2.30 CJS 2.07 LJS 1.54 | T3 MJS 2.08 CJS 2.01 LJS 1.55 | T4 MJS 2.09 CJS 2.25 LJS 1.75 | 0.20 0.82 0.58 |
| Meral et al., Turkey, 2023 [30] | 27 patients (NR) | 27 BSSO | i-CAT Next Generation scanner (Imaging Sciences International, Hatfield, PA, USA) 120 kVp, 5–7 mAs, 23 × 17 cm field of view, 0.3 mm voxel size | NR | CONTROL GROUP SJS 2.24 AJS 2.26 PJS 1.87 CONTRALATERAL GROUP SJS 2.67 AJS 2.29 PJS 2.73 DEVIATION GROUP SJS 3.31 AJS 2.75 PJS 2.50 | CONTROL GROUP SJS 2.30 AJS 2.58 PJS 2.12 CONTRALATERAL GROUP SJS 2.49 AJS 2.19 PJS 2.55 DEVIATION GROUP SJS 2.69 AJS 2.74 PJS 2.21 | 0.64 0.05 * 0.10 0.57 0.59 0.83 0.05 * 0.86 0.36 | NR | NR | NR | ||||||
| Ravelo et al., Chile, 2023 [27] | 26 patients 15 class II 11 class III 14 females 12 males mean age: 27.9 ± 10.81 | BSSO + Le Fort I | NewTom 3D software, Vgi EVO model (Verona, Italy) 24 × 19 cm field of view, 110 kV, 8 mA | 21 days prior to the surgery/6 months after | CLASS II AJS (R) 1.34 AJS (L) 1.48 SJS (R) 2.61 SJS (L) 2.83 PJS (R) 3.03 PJS (L) 2.82 CLASS III AJS (R) 2.53 AJS (L) 2.15 SJS (R) 2.31 SJS (L) 1.98 PJS (R) 1.45 PJS (L) 1.17 | CLASS II AJS (R) 1.74 AJS (L) 1.84 SJS (R) 1.51 SJS (L) 1.52 PJS (R) 2.61 PJS (L) 2.37 CLASS III AJS (R) 1.81 AJS (L) 1.68 SJS (R) 1.55 SJS (L) 1.82 PJS (R) 1.63 PJS (L) 1.46 | CLASS II 0.00 * 0.00 * 0.00 * CLASS III 0.00 * 0.00 * 0.02 * | NR | NR | NR | ||||||
| Yang et al., Republic of China, 2023 [17] | 97 patients 97 class II 77 females 20 males mean age: 24.82 | 97 BSSO + Le Fort I + genioplasty | LCBCT unit (Morita Corp., Hyogo, Japan) 80 kV at 4.5 mA pulse operation | before orthodontics/12 months after surgery | AJS 1.68 SJS 3.09 PJS 2.87 | AJS 1.68 SJS 2.75 PJS 2.16 | 0.96 0.05 * 0.00 * | NR | NR | NR | ||||||
| Abbasi et al., Iran, 2024 [25] | 31 patients 15 class II 16 class III | 8 BSSO 23 BSSO + Le Fort I | Acteon Whitefox CBCT scanner 80 KVP, 5 mA, 0.3 mm voxel size, field of view 170 × 200 | before surgery/min 6 months after surgery | CLASS II SJS 2.46 AJS 2.10 PJS 3.04 CLASS III SJS 2.52 AJS 2.01 PJS 3.00 | CLASS II SJS 2.46 AJS 2.31 PJS 2.94 CLASS III SJS 2.52 AJS 2.13 PJS 2.89 | 0.18 0.01 * 0.01 * 0.48 0.20 0.01 * | CLASS II MJS 2.87 LJS 3.63 CLASS III MJS 2.81 LJS 3.40 | CLASS II MJS 2.84 LJS 3.62 CLASS III MJS 2.87 LJS 3.41 | 0.41 0.46 0.48 0.60 | ||||||
| Vogl et al., Germany, 2024 [21] | 79 patients 29 class II 50 class III 41 females 38 males mean age: 26.62 ± 9.5 | 19 BSSO 60 BSSO + Le Fort I | PLANMECA ProMax-3D Max CBCT device (Planmeca Oy, Helsinki, Finland) field of view: 230 mm/160 mm 120 kV and 7.1 mA | Before surgery/after surgery with a median of 6 weeks | AJS (R) 2.10 AJS (L) 2.10 SJS (R) 2.50 SJS (L) 2.80 PJS (R) 2.20 PJS (L) 2.30 | AJS (R) 2.20 AJS (L) 2.10 SJS (R) 2.30 SJS (L) 2.60 PJS (R) 2.00 PJS (L) 1.90 | 0.13 0.26 0.01 * 0.01 * 0.01 * 0.00 * | LJS (R) 2.10 LJS (L) 2.30 MJS (R) 2.10 MJS (L) 2.10 | LJS (R) 1.90 LJS (L) 2.04 MJS (R) 1.90 MJS (L) 1.90 | 0.02 * 0.01 * 0.00 * 0.01 * | ||||||
| Study (Author, Year) | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Overall Rating |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kim et al., 2010 [24] | Yes | Yes | No | Yes | No | Yes | Yes | NR | Yes | Yes | Yes | NA | Fair |
| Chen et al., 2013 [19] | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Good |
| Kuehle et al., 2016 [22] | Yes | Yes | Yes | Yes | No | Yes | Yes | NR | Yes | Yes | Yes | NA | Good |
| Tabrizi et al., 2016 [26] | Yes | Yes | Yes | Yes | No | Yes | Yes | NR | Yes | Yes | Yes | NA | Good |
| Da Silva et al., 2018 [28] | Yes | Yes | Yes | Yes | No | Yes | Yes | NR | Yes | Yes | No | NA | Fair |
| Zhang et al., 2018 [18] | Yes | Yes | Yes | Yes | No | Yes | Yes | NR | Yes | Yes | No | NA | Fair |
| Huang et al., 2020 [20] | Yes | No | Yes | Yes | No | Yes | Yes | NR | Yes | Yes | Yes | NA | Fair |
| Roman et al., 2022 [29] | Yes | Yes | Yes | Yes | No | No | Yes | NR | Yes | Yes | No | NA | Fair |
| Han et al., 2023 [23] | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | NA | Fair |
| Meral et al., 2023 [30] | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | NA | Fair |
| Ravelo et al., 2023 [27] | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | NA | Good |
| Yang et al., 2023 [17] | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | NA | Good |
| Abbasi et al., 2024 [25] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NR | Yes | Yes | No | NA | Good |
| Vogl et al., 2024 [21] | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No | NA | Fair |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szcześniak, M.; Issa, J.; Ciszewska, A.; Okła, M.; Gałczyńska-Rusin, M.; Dyszkiewicz-Konwińska, M. Alterations in the Temporomandibular Joint Space Following Orthognathic Surgery Based on Cone Beam Computed Tomography: A Systematic Review. J. Clin. Med. 2025, 14, 7239. https://doi.org/10.3390/jcm14207239
Szcześniak M, Issa J, Ciszewska A, Okła M, Gałczyńska-Rusin M, Dyszkiewicz-Konwińska M. Alterations in the Temporomandibular Joint Space Following Orthognathic Surgery Based on Cone Beam Computed Tomography: A Systematic Review. Journal of Clinical Medicine. 2025; 14(20):7239. https://doi.org/10.3390/jcm14207239
Chicago/Turabian StyleSzcześniak, Marta, Julien Issa, Aleksandra Ciszewska, Maciej Okła, Małgorzata Gałczyńska-Rusin, and Marta Dyszkiewicz-Konwińska. 2025. "Alterations in the Temporomandibular Joint Space Following Orthognathic Surgery Based on Cone Beam Computed Tomography: A Systematic Review" Journal of Clinical Medicine 14, no. 20: 7239. https://doi.org/10.3390/jcm14207239
APA StyleSzcześniak, M., Issa, J., Ciszewska, A., Okła, M., Gałczyńska-Rusin, M., & Dyszkiewicz-Konwińska, M. (2025). Alterations in the Temporomandibular Joint Space Following Orthognathic Surgery Based on Cone Beam Computed Tomography: A Systematic Review. Journal of Clinical Medicine, 14(20), 7239. https://doi.org/10.3390/jcm14207239








