Diagnostic Utility of Red Flags for Detecting Spinal Malignancies in Patients with Low Back Pain: A Scoping Review
Abstract
1. Background
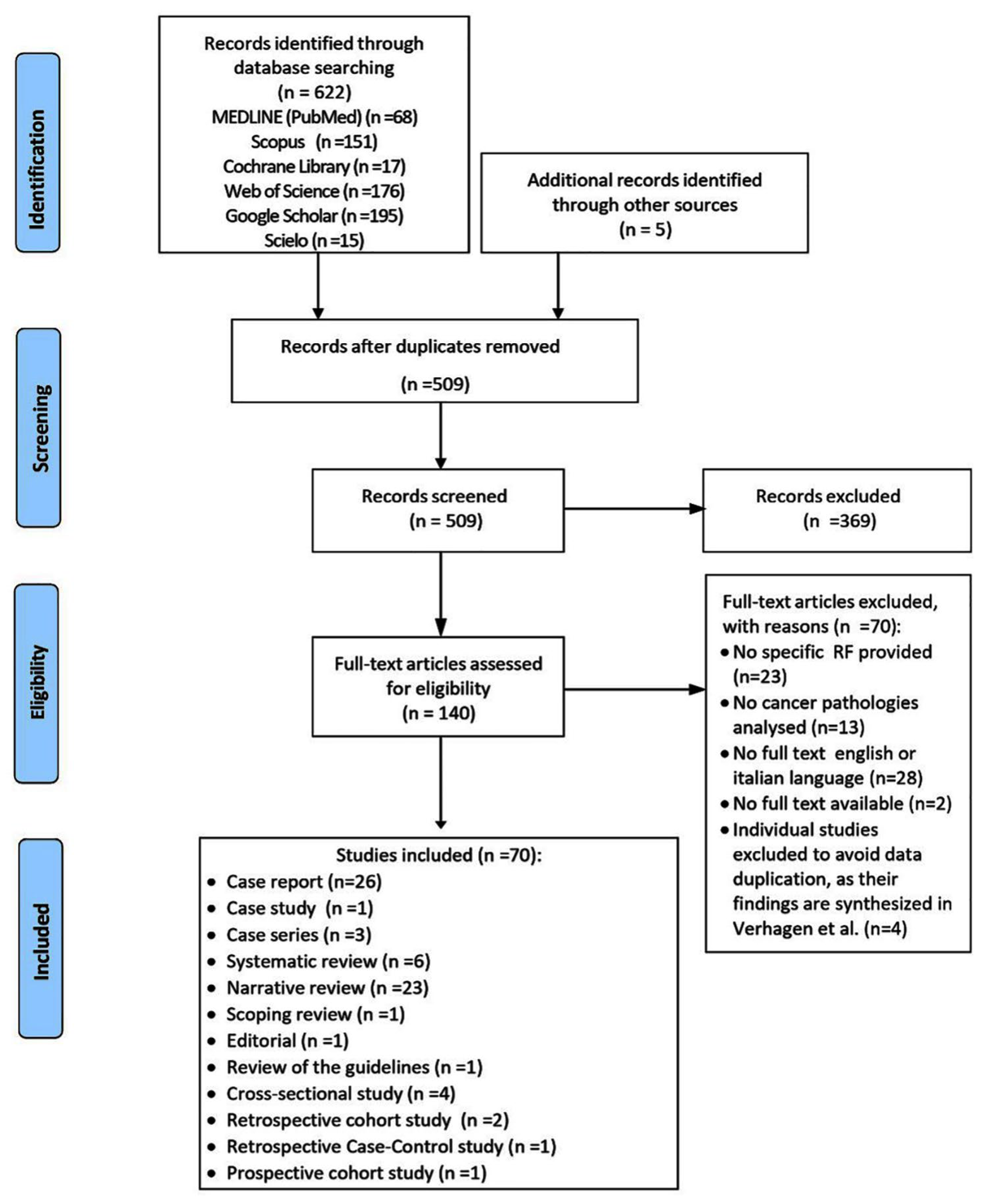
2. Materials and Methods
2.1. Research Question
2.2. Protocol and Registration
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Search Strategy
2.6. Selection of Studies
2.7. Data Extraction
2.8. Data Synthesis
3. Results
3.1. Characteristics of the Included Studies
3.2. Patient Assessment and Clinical Findings
3.2.1. Case Reports, Case Series, Case Studies
3.2.2. Observational Studies
3.3. Cancer-Specific RFs
3.3.1. Case Reports, Case Series, Case Studies
3.3.2. Observational Studies
3.3.3. Review Studies
3.4. Differential Diagnosis
3.4.1. Case-Based Studies
3.4.2. Observational Studies
4. Discussion
4.1. Implications for Clinical Practice
4.2. Research Implications
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
Appendix A. Search Strategy and Grey Iterature
| Date: 15 March 2025 | ||
| DATABASE | SEARCH STRATEGY | RESULTS |
| MEDLINE | ((“Low Back Pain”[MeSH Terms] OR “Low Back Pain”[All Fields] OR “low back ache”[All Fields] OR “lumbodynia”[All Fields]) AND (“tumor”[All Fields] OR “cancer”[All Fields] OR “malignancy”[All Fields] OR “neoplasm”[All Fields] OR “tumour”[All Fields]) AND (“red flags”[All Fields] OR “red herrings”[All Fields] OR “red flag”[All Fields] OR “red herring”[All Fields])) | 68 |
| WEB OF SCIENCE | (“low back pain” OR lumbago OR “lower back pain” OR “low backache” OR “low back ache”) AND (“differential diagnosis” OR referral OR consultation OR “physical examination” OR inspection OR observation OR screening OR “red flag” OR “red herring” OR “specific pathology” OR “serious pathology” OR “severe pathology” OR “tumor” OR cancer OR “malignancy” OR “neoplasm”) | 176 |
| SciELO | (“low NEXT back NEXT pain” OR “lumbar pain” OR “lumbago” OR “low back ache” OR “low backache”) AND (“tumor” OR cancer OR “malignancy” OR “neoplasm” OR “oncological disease” OR “cancer disease”) AND (“differential diagnosis” OR diagnosis OR symptoms OR signs OR findings OR referral OR consultation OR “physical examination” OR inspection OR observation OR screening) | 15 |
| COCHRANE LIBRARY | (“low back pain” OR lumbago OR “lower back pain” OR “low backache” OR “low back ache”) AND (“differential diagnosis” OR diagnosis OR symptoms OR signs OR findings OR referral OR consultation OR “physical examination” OR inspection OR observation OR screening) AND (“red flag” OR “red herring” OR “specific pathology” OR “serious pathology” OR “serious disorder” OR “specific disorder” OR “serious disease” OR “specific disease”) AND (“tumor” OR cancer OR “malignancy” OR “neoplasm”) | 17 |
| SCOPUS | (“low back pain” OR lumbago OR “lower back pain” OR “low backache” OR “low back ache”) AND (“differential diagnosis” OR diagnosis OR symptoms OR signs OR findings OR referral OR consultation OR “physical examination” OR inspection OR observation OR screening) AND (“red flag” OR “red herring” OR “specific pathology” OR “serious pathology” OR “serious disorder” OR “specific disorder” OR “serious disease” OR “specific disease”) AND (“tumor” OR cancer OR “malignancy” OR “neoplasm” | 151 |
| GOOGLE SCHOLAR | “low back pain” AND “differential diagnosis” AND “red flag” AND (“tumor” OR “malignancy”) | 195 |
Appendix B. Studies Added from Grey Literature
- Kaur R; Kaur L; Iqbal A; Patel, N. Urothelial Carcinoma With Bone Metastasis Mimicking Sciatica: A Common Neoplasm With an Uncommon Presentation. Cureus 2024, 16, e55259. https://doi.org/10.7759/cureus.55259
- Patel, H.G.; Tabassum, S.; Shaikh, S. E. coli Sepsis: Red Flag for Colon Carcinoma-A Case Report and Review of the Literature. Case Rep. Gastrointest. Med. 2017, 2017, 2570524. https://doi.org/10.1155/2017/2570524. PMID: 28695023; PMCID: PMC5485293.
- Henschke, N.; Maher, C.G.; Ostelo, R.W.; de Vet, H.C.; Macaskill, P.; Irwig, L. Red flags to screen for malignancy in patients with low-back pain. Cochrane Database Syst. Rev. 2013, 2013, CD008686. https://doi.org/10.1002/14651858.CD008686.pub2. PMID: 23450586; PMCID: PMC10631455.
- Finucane, L.; Greenhalgh, S.; Selfe, J. What are the Red flags to aid the early detection of metastatic bone disease as a cause of back pain? Physiother. Pract. Res. 2017, 38, 73–77.
- Delladio, M.; Maselli, F.; Testa, M. Red flags or red herrings: what is the actual weight of the signs and symptoms of alarm in the evaluation of patients with low back pain/Red flags o red herrings: Qual e il reale peso dei segni e sintomi di allarme nella valutazione del paziente con lombalgia. Sci. Riabil. 2013, 15, 5+. Available online: https://link.gale.com/apps/doc/A331080126/AONE?u=anon~1cf485a3 (accessed on 9 March 2025).
Appendix C. Excluded Studies with Reasons
| Author, Year | Reference (Title, Doi (or Link If Not Available) | Reason for Exclusion |
| Menezes, 2025 | Clinical and radiological parameters in malignant spinal tumors: A descriptive analysis DOI: 10.1590/1413-785220253301e285913 | No specific data on low back pain; only overall numbers of patients with back pain and those with lumbar metastases provided. |
| Seddio, 2024 | The incidence, providers involved, and patient factors associated with diagnosis of specific lumbar spine pathology subsequent an initial nonspecific low back pain diagnosis DOI: 10.1016/j.spinee.2024.10.008 | No data on how many patients with LBP developed cancer; no database in Supplementary Materials; no specific RFs reported. |
| Jenkins, 2024 | Diagnostic imaging in the management of older adults with low back pain: analysis from the BAck Complaints in Elders: Chiropractic—Australia cohort study DOI: 10.1186/s12998-024-00562-z | No cancer cases identified. |
| Lee, 2024 | Appropriateness of magnetic resonance imaging of the lumbar spine orders for low back pain in a general hospital DOI: 10.1177/20101058241248208 | No information on patients with confirmed cancer diagnosis and associated red flags. |
| Meidinger, 2023 | A Model of Triage of Serious Spinal Pathologies and Therapeutic Options Based on a Delphi Study DOI: 10.3390/medicina59071283 | Focuses on hypotheses, not on patients; no cancer analyzed; not relevant |
| Karpuz, 2023 | The Red and Yellow Flag Awareness Level of Family Physicians in Low Back Pain DOI: 10.33880/EJFM.2023120304 | No tumor-specific red flags for LBP reported; focused on physiotherapists’ responses; not relevant. |
| Dixit, 2023 | Low Back and Neck Pain DOI: 10.1007/978-3-031-23488-0_46 | No full text available |
| Guerra, 2023 | Screen time and low back pain in children and adolescents: a systematic review of Brazilian studies DOI: 10.1590/1984-0462/2023/41/2021342 | Focuses on non-specific LBP and telephone use; not relevant to cancer. |
| Aliaga-Chávez, 2022 | Presentación histopatológica atípica en médula ósea de mieloma múltiple DOI: 10.35434/rcmhnaaa.2022.151.1016 | Full text with no English or Italian language |
| Álvarez-Restrepo, 2022 | Metanephric Adenoma: differential diagnosis of upper tract urothelial carcinoma. A Case Report DOI: 10.15446/cr.v8n1.92283 | No relevant or specified red flags; not relevant. |
| Melman, 2022 | Many people admitted to hospital with a provisional diagnosis of nonserious back pain are subsequently found to have serious pathology as the underlying cause DOI: 10.1007/s10067-022-06054-w | Red flags not extracted; not relevant. |
| Sporniak, 2022 | In search of “red flag” symptoms accompanying spinal pain in diffuse large B-cell lymphoma DOI: 10.20452/pamw.16283 | No red flags identified; not relevant. |
| Konbaz, 2021 | Sequestrated Lumbar Disc Herniation Mimicking Spinal Neoplasm DOI: 10.7759/cureus.18529 | No patients with cancer reported; not relevant. |
| Sacoto García, 2021 | Evolution of low back pain in cancer patients treated with interventional pain management DOI: 10.20986/resed.2021.3901/2020 | Full text with no English or Italian language |
| Machado, 2020 | Emergency department care for low back pain: Should we adopt recommendations from primary care guidelines? DOI: 10.1111/1742-6723.13593 | No red flags in patients with LBP and cancer reported; not relevant. |
| Urrutia, 2020 | Management of patients with low back pain in the emergency department: Is it feasible to follow evidence-based recommendations? DOI: 10.1111/1742-6723.13544 | Only red flags mentioned, but not associated with specific pathologies; not relevant. |
| Ceballos, 2020 | Malignant tumor of the spine http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0864-215X2020000200009&lng=es&nrm=iso Epub 01-Feb-2021 (accessed on 8 March 2025) | Full text with no English or Italian language |
| Pizarro, 2020 | Síndrome de Cushing provocado por carcinoma suprarrenal gigante. Caso clínico DOI: 10.4067/S0034-98872020001101679 | Full text with no English or Italian language |
| Santos, 2020 | Antegrade insertion of a double J catheter in the treatment of malignant ureteral obstruction: a retrospective analysis of the results obtained with a modified technique at a university hospital DOI: 10.1590/0100-3984.2019.0090 | LBP mentioned in the abstract only as a complication after catheter insertion; not relevant. |
| Al Somali, 2019 | Red Flags” signs among Physician’s with acute back pain In Saudi Arabia DOI: 10.5281/zenodo.2552537 | No cancer-related red flags; questionnaire-based study; not relevant. |
| Carmenathy, 2019 | Astrocitoma medular de alto grado no infiltrante. http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1028-99332019000500640&lng=es&nrm=iso Epub 29-Oct-2019 (accessed on 8 March 2025) | Full text with no English or Italian language |
| Cook, 2018 | Red flag screening for low back pain: nothing to see here, move along: a narrative review DOI: 10.1136/bjsports-2017-098352 | No cancer-specific red flags reported; not relevant. |
| Strudwick, 2018 | Review article: Best practice management of low back pain in the emergency department (part 1 of the musculoskeletal injuries rapid review series) DOI: 10.1111/1742-6723.12907 | No specific red flags for LBP with cancer reported; not relevant. |
| Andrašinová, 2018 | Low back pain in the elderly https://www.internimedicina.cz/pdfs/int/2018/03/11.pdf#:~:text=Bolesti%20doln%C3%AD%20%C4%8D%C3%A1sti%20zad%20(low%20back%20pain%20%E2%80%93,pohybuje%20mezi%2013%E2%80%9350%20%%20(Bressler%20et%20al.,%201999) (accessed on 8 March 2025) | Full text with no English or Italian language |
| Jùnior, 2018 | Thoracolumbar epidural arachnoid cyst of difficult clinical management: Case Report. DOI: 10.1590/s1808-185120181701177954 | Case report on cysts without tumor signs; not relevant. |
| López-Ruiz, 2018 | Schwannoma pélvico retroperitoneal que simula un leiomioma: reporte de un caso y revisión bibliográfica. DOI: 10.24245/gom.v86i3.1964 | Full text with no English or Italian language |
| Yang, 2017 | Low Back Pain in Adolescents: A 1-Year Analysis of Eventual Diagnoses DOI: 10.1097/BPO.0000000000000653 | No red flags reported; not relevant. |
| Bartoloni, 2017 | Low Back Pain Imaging Management in the Elderly Population DOI: 10.1007/S40134-017-0194-Z | Red flags not directly mentioned; not relevant. |
| Cardoso, 2017 | Meningioma de localización lumbar en un paciente con virus de inmunodeficiencia humana http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S2221-24342017000200010&lng=es&nrm=iso (accessed on 8 March 2025) | Full text with no English or Italian language |
| Garcia, 2017 | Return to Work after Breast Cancer http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0465-546X2017000100051&lng=es&nrm=iso (accessed on 8 March 2025) | Full text with no English or Italian language |
| Almeida, 2017 | Low back pain—a diagnostic approach DOI: 10.5935/1806-0013.20170034 | Cancer not clearly mentioned; not relevant. |
| Velázquez, 2016 | Single cutaneous metastasis due to bladder urothelial carcinoma http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1029-30192016000800014&lng=es&nrm=iso (accessed on 8 March 2025) | Full text with no English or Italian language |
| Braun, 2016 | Ivory vertebra: imaging findings in different diagnoses DOI: 10.1590/0100-3984.2014.0103 | No red flags reported; focused only on radiologists; not relevant. |
| Massoud, 2016 | Myeloid Sarcoma Presenting as Low Back Pain in the Pediatric Emergency Department DOI: 10.1016/j.jemermed.2016.01.033 | Case report included in Verhagen’s systematic review; excluded here to avoid methodological errors; not relevant. |
| Patel, 2016 | ACR Appropriateness Criteria Low Back Pain DOI: 10.1016/j.jacr.2016.06.008 | Based on 1996 guidelines (inclusion criteria set from 1999 onwards) and does not distinguish between tumors and infections; not relevant |
| Goldschmidt, 2016 | Presenting Signs of Multiple Myeloma and the Effect of Diagnostic Delay on the Prognosis DOI: 10.3122/jabfm.2016.06.150393 | Back pain considered as a generic red flag/symptom; unclear whether patients with back pain had other red flags; classified under ‘no cancer analyzed’; not relevant. |
| Betancourt, 2015 | Generalidades de los tumores de la región sacrococcígea http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1608-89212015000300026&lng=es&nrm=iso (accessed on 8 March 2025) | Full text with no English or Italian language |
| Romo, 2015 | Spinal cord compression due to nonleukemic granulocytic sarcoma DOI: 10.1016/j.rccan.2015.03.003 | Full text with no English or Italian language |
| Guzmàn, 2015 | Association between diastematomyelia and medullo epithelioma. Case report and literature review DOI: 10.4067/S0717-92272015000200004. | Full text with no English or Italian language |
| Mabry, 2014 | Metastatic cancer mimicking mechanical low back pain: a case report DOI: 10.1179/2042618613Y.0000000056 | Case report included in Verhagen’s systematic review; excluded here to avoid methodological errors; not relevant. |
| Thiruganasambandamoorthy, 2014 | Risk factors for serious underlying pathology in adult emergency department nontraumatic low back pain patients DOI: 10.1016/j.jemermed.2013.08.140 | No red flags specifically associated with cancer reported; not relevant |
| Neves, 2014 | A formação de profissionais de saúde para a prevenção de lesões musculoesqueléticas ligadas ao trabalho a nível da coluna lombar: uma revisão sistemática DOI: 10.1016/j.rpsp.2014.01.001 | Full text with no English or Italian language |
| Vera Vicuña, 2014 | Análisis retrospectivo sobre la utilidad de las herramientas de valoración funcional, en las dolencias lumbares a nivel del ámbito laboral http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0465-546X2014000500035&lng=es&nrm=iso (accessed on 8 March 2025) | Full text with no English or Italian language |
| Finucane, 2013 | Metastatic disease masquerading as mechanical low back pain; atypical symptoms which may raise suspicion DOI: 10.1016/j.math.2013.02.009 | Included in Verhagen’s systematic review; excluded here to avoid methodological errors; not relevant. |
| Underwood, 2013 | Red flags for back pain DOI: 10.1136/bmj.f7432 | Only comments on reviews already included; no cancer-specific red flags reported; not relevant. |
| Pinho; 2012 | Solid variant of aneurysmal bone cist on the distal extremity of the radius in a child DOI: 10.1016/j.rbo.2015.05.005 | Full text with no English or Italian language |
| Calvo-Muñoz, 2012 | Prevalence of Low Back Pain during Childoohd and Adolescence. A Systematic Review http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1135-57272012000400003&lng=es&nrm=iso (accessed on 8 March 2025) | Full text with no English or Italian language |
| Martínez Suárez, 2012 | Consideraciones generales del dolor lumbar agudo. http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1726-67182012000100005&lng=es&nrm=iso (accessed on 8 March 2025) | Full text with no English or Italian language |
| Boissonnault, 2012 | Physical therapists referring patients to physicians: A review of case reports and series DOI: 10.2519/JOSPT.2012.3890 | No red flags for cancer-related low back pain reported; not relevant. |
| Karumanchery, 2012 | An unusual case of back pain: A large Pheochromocytoma in an 85 year old woman. DOI: 10.1016/j.ijscr.2011.10.006 | No red flags reported; not relevant. |
| Şahin Onat, 2011 | Schwannoma which has only sign mechanical backache: A case report https://www.scopus.com/inward/record.uri?eid=2-s2.0-84864143302&partnerID=40&md5=68066901a498fb5110e86d87c1b82288 (accessed on 8 March 2025) | No full text avaliable |
| Bálint, 2011 | The modern international principles of diagnosing and treating low back pain https://www.scopus.com/pages/publications/79958810472?inward (accessed on 8 March 2025) | No full text avaliable |
| Oliveira, 2011 | Profile of the Population Cared for in a Referral Emergency Unit. DOI: 10.1590/S0104-11692011000300014 | Non-specific; LBP only mentioned; not relevant |
| Fialho, 2011 | Musculoskeletal system assessment in an emergency room DOI: 10.1590/S0482-50042011000300005 | No mention of cancer-related specific LBP and no database available; not relevant. |
| Nogueira, 2011 | Corpectomia da coluna toracolombar com colocação de cage por acesso único via posterior: técnica cirúrgica e resultados de seis pacientes DOI: 10.1590/S1808-18512011000200003 | Full text with no English or Italian language |
| Maraschin, 2010 | Dor lombar crônica e dor nos membros inferiores em idosas: etiologia em revisão DOI: 10.1590/S0103-51502010000400013 | Full text with no English or Italian language |
| Morales, 2010 | Plasmocitoma Óseo Solitario X1 DOI: 10.4321/s1699-695x2010000300014 | Full text with no English or Italian language |
| Valle Calvet, 2010 | Red flags of low back pain DOI: 10.1016/j.semreu.2009.09.006 | Full text with no English or Italian language |
| González, 2008 | Hipernefroma gigante: a propósito de un caso http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-74932008000100012&lng=es&nrm=iso (accessed on 8 March 2025) | Full text with no English or Italian language |
| Meneses, 2008 | Primary filum terminale ependymoma: a series of 16 cases DOI: 10.1590/S0004-282X2008000400017 | No red flags reported; not relevant. |
| Rectenwald, 2008 | A case study of back pain and renal cell carcinoma. DOI: 10.1016/j.jcme.2008.01.001 | Included in Verhagen’s systematic review; excluded here to avoid methodological errors; not relevant. |
| Ángel, 2007 | Diagnóstico situacional de las internas del reclusorio de mujeres de Manizales https://revistasojs.ucaldas.edu.co/index.php/hacialapromociondelasalud/article/view/1951 (accessed on 8 March 2025) | Full text with no English or Italian language |
| Duràn, 2007 | Dolor lumbar: enfoque basado en la evidencia. http://hdl.handle.net/10495/18924 (accessed on 8 March 2025) | Full text with no English or Italian language |
| Gonzalez, 2007 | Tumor de la glándula suprarrenal http://ve.scielo.org/scielo.php?script=sci_arttext&pid=S0798-05822007000100010&lng=es&nrm=iso (accessed on 8 March 2025) | Full text with no English or Italian language |
| Sizer, 2007 | Medical Screening for Red Flags in the Diagnosis and Management of Musculoskeletal Spine Pain DOI: 10.1111/j.1533-2500.2007.00112.x | No specific red flags for cancer-related low back pain reported; not relevant |
| Leerar, 2017 | Documentation of red flags by physical therapists for patients with low back pain. DOI: 10.1179/106698107791090105 | No mention of low back pain associated with cancer; not relevant. |
| Rives, 2004 | Evaluation and treatment of low back pain in family practice DOI: 10.3122/jabfm.17.suppl_1.s23 | No specific red flags for LBP and cancer; only mentioned with infections; not relevant. |
| Barsa, 2003 | Red Flags in the diagnosis and treatment of the low back pain https://www.scopus.com/pages/publications/0141493730?inward (accessed on 8 March 2025) | Full text with no English or Italian language |
| Hudson, 2002 | Low back pain: A simple protocol for GPs https://hdl.handle.net/10520/AJA02599333_3131 (accessed on 8 March 2025) | No tumor-specific red flags reported; not relevant. |
| Arce, 2001 | Recognizing spinal cord emergencies https://www.aafp.org/pubs/afp/issues/2001/0815/p631.pdf (accessed on 8 March 2025) | Insufficient data provided and main cancer-associated red flags not reported; not relevant. |
References
- Burton, A.K.; COST B13 Working Group. European Guidelines for Prevention in Low Back Pain; University of Huddersfield: Huddersfield, UK, 2004; pp. 1–53. [Google Scholar]
- Feller, D.; Giudice, A.; Maritati, G.; Maselli, F.; Rossettini, G.; Meroni, R.; Lullo, G.; Hutting, N.; Mourad, F. Physiotherapy Screening for Referral of a Patient with Peripheral Arterial Disease Masquerading as Sciatica: A Case Report. Healthcare 2023, 11, 1527. [Google Scholar] [CrossRef]
- Maselli, F.; Storari, L.; Barbari, V.; Colombi, A.; Turolla, A.; Gianola, S.; Rossettini, G.; Testa, M. Prevalence and incidence of low back pain among runners: A systematic review. BMC Musculoskelet. Disord. 2020, 21, 343. [Google Scholar] [CrossRef]
- Maselli, F.; Esculier, J.F.; Storari, L.; Mourad, F.; Rossettini, G.; Barbari, V.; Pennella, D.; Cataldi, F.; Viceconti, A.; Geri, T.; et al. Low back pain among Italian runners: A cross-sectional survey. Phys. Ther. Sport 2021, 48, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Maselli, F.; Testa, M. Superficial peroneal nerve schwannoma presenting as lumbar radicular syndrome in a non-competitive runner. J. Back Musculoskelet. Rehabil. 2019, 32, 361–365. [Google Scholar] [CrossRef] [PubMed]
- Blyth, F.M.; Briggs, A.M.; Schneider, C.H.; Hoy, D.G.; March, L.M. The Global Burden of Musculoskeletal Pain—Where to From Here? Am. J. Public Health 2019, 109, 35–40. [Google Scholar] [PubMed]
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2017, 392, 1789–1858. [Google Scholar]
- Han, C.S.; Hancock, M.J.; Downie, A.; Jarvik, J.G.; Koes, B.W.; Machado, G.C.; Verhagen, A.P.; Williams, C.M.; Maher, C.G. Red flags to screen for vertebral fracture in patients presenting with low back pain. Cochrane Database Syst. Rev. 2022, 2022, CD014461. [Google Scholar] [CrossRef] [PubMed Central]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Galliker, G.; Scherer, D.E.; Trippolini, M.A.; Rasmussen-Barr, E.; LoMartire, R.; Wertli, M.M. Low Back Pain in the Emergency Department: Prevalence of Serious Spinal Pathologies and Diagnostic Accuracy of Red Flags. Am. J. Med. 2020, 133, 60–72.e14. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 3 February 2025).
- Storari, L.; Piai, J.; Zitti, M.; Raffaele, G.; Fiorentino, F.; Paciotti, R.; Garzonio, F.; Ganassin, G.; Dunning, J.; Rossettini, G.; et al. Standardized Definition of Red Flags in Musculoskeletal Care: A Comprehensive Review of Clinical Practice Guidelines. Medicina 2025, 61, 1002. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Suspected Cancer: Recognition and Referral. NICE Guideline NG12. Available online: https://www.nice.org.uk/guidance/ng12 (accessed on 7 April 2025).
- DePalma, M.G. Red flags of low back pain. J. Am. Acad. Physician Assist. 2020, 33, 8–11. [Google Scholar] [CrossRef]
- Casazza, B.A. Diagnosis and Treatment of Acute Low Back Pain. Am. Fam. Physician 2012, 85, 343–350. [Google Scholar]
- Finucane, L.M.; Downie, A.; Mercer, C.; Greenhalgh, S.M.; Boissonnault, W.G.; Pool-Goudzwaard, A.L.; Beneciuk, J.M.; Leech, R.L.; Selfe, J. International Framework for Red Flags for Potential Serious Spinal Pathologies. J. Orthop. Sports Phys. Ther. 2020, 50, 272–285. [Google Scholar] [CrossRef] [PubMed]
- Maselli, F.; Palladino, M.; Barbari, V.; Storari, L.; Rossettini, G.; Testa, M. The diagnostic value of Red Flags in thoracolumbar pain: A systematic review. Disabil. Rehabil. 2022, 44, 1190–1206. [Google Scholar] [CrossRef] [PubMed]
- Joanna Briggs Institute. JBI Reviewer’s Manual. 2020. Available online: https://jbi.global/ (accessed on 1 September 2024).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Notarangelo, G.; Giovannico, G.; Bruno, F.; Milella, C.; Mourad, F.; Maselli, F. Red flags useful to screen for suspect cancer in patients with low back pain: A scoping review protocol. medRxiv 2024. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Mabry, L.M.; Ross, M.D.; Tonarelli, J.M. Metastatic cancer mimicking mechanical low back pain: A case report. J. Man. Manip. Ther. 2014, 22, 162–169. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Finucane, L. Metastatic disease masquerading as mechanical low back pain; atypical symptoms which may raise suspicion. Man. Ther. 2013, 18, 624–627. [Google Scholar] [CrossRef] [PubMed]
- Massoud, M.; Del Bufalo, F.; Caterina Musolino, A.M.; Schingo, P.M.; Gaspari, S.; Pisani, M.; Orazi, C.; Reale, A.; Raucci, U. Myeloid Sarcoma Presenting as Low Back Pain in the Pediatric Emergency Department. J. Emerg. Med. 2016, 51, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Rectenwald, R. A case study of back pain and renal cell carcinoma. J. Chiropr. Med. 2008, 7, 24–27. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Verhagen, A.P.; Downie, A.; Maher, C.G.; Koes, B.W. Most red flags for malignancy in low back pain guidelines lack empirical support: A systematic review. Pain 2017, 158, 1860–1868. [Google Scholar] [CrossRef] [PubMed]
- Kahn, E.A. A Young Female Athlete with Acute Low Back Pain Caused by Stage IV Breast Cancer. J. Chiropr. Med. 2017, 16, 230–235. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cataldi, F.; Brindisino, F.; Angilecchia, D.; Andreani, A.; Giovannico, G. Neoplastic malignant cord compression mimicking low back pain: A case report. Physiother. Res. Int. 2023, 28, e1971. [Google Scholar] [CrossRef] [PubMed]
- Ng, G.S.N.; Chow, I.S.W. Colorectal Cancer Presenting as Sacral Pain at a Chiropractic Clinic. Cureus 2023, 15, E39277. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bang, J.S.; Adsul, N.; Lim, J.H.; Jang, I.T. Extra-Osseous Ewing Sarcoma of Sciatic Nerve Masquerading as Benign Nerve Sheath Tumor and Presented as Lumbar Radiculopathy: Case Report and Review of Literature. World Neurosurg. 2018, 115, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Chu, E.C.; Trager, R.J.; Yee, W.J.; Ng, K.K. Lumbar Schwannoma as a Rare Cause of Radiculopathy in the Chiropractic Office: A Case Report. Cureus 2022, 14, E31758. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Brindisino, F.; Scrimitore, A.; Pennella, D.; Bruno, F.; Pellegrino, R.; Maselli, F.; Lena, F.; Giovannico, G. Aggressive Vertebral Hemangioma and Spinal Cord Compression: A Particular Direct Access Case of Low Back Pain to Be Managed—A Case Report. Int. J. Environ. Res. Public Health 2022, 19, 13276. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Leri, J.P. Metastatic Cancer of the Thoracic and Lumbar Spine Presenting as Mid- and Low Back Pain in a Long Distance Runner. J. Chiropr. Med. 2018, 17, 121–127. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kaur, R.; Kaur, L.; Iqbal, A.; Patel, N. Urothelial Carcinoma with Bone Metastasis Mimicking Sciatica: A Common Neoplasm With an Uncommon Presentation. Cureus 2024, 16, e55259. [Google Scholar] [CrossRef]
- Patel, H.G.; Tabassum, S.; Shaikh, S. E. coli Sepsis: Red Flag for Colon Carcinoma—A Case Report and Review of the Literature. Case Rep. Gastrointest. Med. 2017, 2017, 2570524. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de Moraes, F.B.; Cardoso, A.L.; Tristão, N.A.; Pimenta, W.E., Jr.; Daher, S.; de Souza Carneiro, S.; Barbosa, N.P.; de Lima Malta, N.; Ribeiro, N.B. Primary liposarcoma of the lumbar spine: Case report. Rev. Bras. Ortop. 2015, 47, 124–129. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Antunes, A.A.; Siqueira TMJr Falcão, E. Vesical metastasis of gastric adenocarcinoma. Int. Braz. J. Urol. 2004, 30, 403–405. [Google Scholar] [CrossRef] [PubMed]
- Ata, F.; Yousaf, Z.; Al Kalaji, B.N.; Ashour, A.A.; Fael, M.; Eun Kim, G.; Bint IBilal, A.; Elaiwy, O.; Jones, A. Back pain as an initial feature of advanced gastric cancer mimicking multiple myeloma: A case report and literature review. Qatar Med. J. 2022, 2022, 53. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tan, W.J.; Lee, H.Y.; Yap, W.M.Q.; Nolan, C.P.; Oh, J.Y.-L. An Atypical Presentation of Metastatic Ewing Sarcoma to the Spine. Indian Spine J. 2021, 4, 240–242. [Google Scholar] [CrossRef]
- Mannarini, M.; Maselli, F.; Giannotta, G.; Cioeta, M.; Giovannico, G. Low back pain as main symptom in Low-grade Appendiceal Mucinous Neoplasm (LAMN): A case report. Physiother. Theory Pract. 2024, 21, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Sahu, P.K.; Shankar Ganesh, G. Physiotherapeutic management of a patient with spinal Schwannoma: A case report. J. Bodyw. Mov. Ther. 2020, 24, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Marin, J.R. A Teenage Girl with Acute Back Pain. Clin. Pediatr. Emerg. Med. 2007, 8, 65–68. [Google Scholar] [CrossRef]
- Soerensen, B. Mechanical diagnosis and therapy (MDT) approach for assessment and identification of serious pathology. Man. Ther. 2011, 16, 406–408. [Google Scholar] [CrossRef] [PubMed]
- Falavigna, A.; Righesso Neto, O.; dos Santos, J.A.; Ferraz, F.A. Cavernous angioma of the cauda equina: Case report. Arq. Neuropsiquiatr. 2004, 62, 531–534. [Google Scholar] [CrossRef] [PubMed]
- Arnold, P.M.; Park, M.C.; Newell, K.; Kepes, J.J.; Thrasher, J.B. Thoracic spinal cord compression secondary to metastatic synovial sarcoma: Case report. Coluna/Columna 2009, 8, 206–211. [Google Scholar] [CrossRef]
- Pitombo, P.F.; Moura, R.; Miranda, R.H. Continuous spinal block in a patient undergoing partial gastrectomy:Case report. Braz. J. Anesthesiol. 2009, 59, 481–486. [Google Scholar] [CrossRef]
- Pinto-Lopes, P.; Fonseca, F.A.; Silva, R.; von Hafe, P.; Fonseca, E. Indolent systemic mastocytosis limited to the bone: A case report and review of the literature. Sao Paulo Med. J. 2013, 131, 198–204. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- dos Santos, M.M.; Proença, S.M.; Reis, M.I.; Viana, R.M.; Martins, L.M.; Colaço, J.M.; Nunes, F.M. Spontaneous rupture of renal angiomyolipoma during pregnancy. Rev. Bras. Ginecol. Obstet. 2014, 36, 377–380. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.; Vital, L.; Serdoura, F.; Pinho, A.R.; Veludo, V. Spondylectomy for primary Ewing lumbar sarcoma in children. Rev. Bras. Ortop. 2020, 55, 649–652. [Google Scholar] [CrossRef]
- Ortiz, E.R.; Duarte, A.; Leonardo, M.; Rodríguez, V.; Jovanny, L. Metástasis pulmonar y pleural en cáncer de pene, una patología infrecuente. Rev. Médica Risaralda 2021, 27, 170–180. Available online: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0122-06672021000200170 (accessed on 8 March 2025).
- Relvas-Silva, M.; Lima, E.R.; Silva, M.R.; Neves, N. Laparoscopic-assisted Resection of a Retroperitoneal Lumbar Nerve Root Neurofibroma: A Case Report. Rev. Bras. Ortop. 2024, 59 (Suppl. 1), e109–e113. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pucciarelli, L.R.M.; Cunha, M.C.F.d.; Moscardini, I.S.; Chedid, D.A.; Paiva, M.; Miyasaka, M.; Vieira, R.S. Giant cell tumor with vertebral aneurysmatic bone cyst in a young—A case report. Coluna/Columna 2024, 23, e289734. [Google Scholar] [CrossRef]
- Madson, T.J. Considerations in physical therapy management of a non-responding patient with low back pain. Physiother. Theory Pract. 2017, 33, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Chu, E.C.; Trager, R.J.; Lai, C.R.; Leung, B.K. Presumptive Prostate Cancer Presenting as Low Back Pain in the Chiropractic Office: Two Cases and Literature Review. Cureus 2022, 14, E30575. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ahmad, T.; Ahmed Hussain, M.F.; Hameed, A.A.; Manzar, N.; Lakdawala, R.H. Conservative surgery for osteoid osteoma of the lumbar vertebrae. Surg. Neurol. Int. 2014, 5, 24. [Google Scholar] [CrossRef] [PubMed]
- Muñoz Moya, J.; Alfaro Aguirre, M.; Leiva Silva, M.; Kakarieka Weisskopf, E.; López Sáez, M. Tumor miofibroblástico inflamatorio: Presentación variable de una misma patología. Rev. Chil. Pediatr. 2019, 90, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Downie, A.; Williams, C.M.; Henschke, N.; Hancock, M.J.; Ostelo, R.W.; de Vet, H.C.; Macaskill, P.; Irwig, L.; van Tulder, M.W.; Koes, B.W.; et al. Red flags to screen for malignancy and fracture in patients with low back pain: Systematic review. BMJ 2013, 347, F7095, Erratum in BMJ 2014, 348, G7. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Henschke, N.; Maher, C.G.; Ostelo, R.W.; de Vet, H.C.; Macaskill, P.; Irwig, L. Red flags to screen for malignancy in patients with low-back pain. Cochrane Database Syst. Rev. 2013, 2013, CD008686. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Henschke, N.; Maher, C.G.; Refshauge, K.M. Screening for malignancy in low back pain patients: A systematic review. Eur. Spine J. 2007, 16, 1673–1679. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Janny, M.; Pasquier, M.; Descarreaux, M.; Marchand, A.-A. Diagnosis Value of Patient Evaluation Components Applicable in Primary Care Settings for the Diagnosis of Low Back Pain: A Scoping Review of Systematic Reviews. J. Clin. Med. 2023, 12, 3581. [Google Scholar] [CrossRef]
- Finucane, L.; Greenhalgh, S.; Selfe, J. What are the Red flags to aid the early detection of metastatic bone disease as a cause of back pain? Physiother. Pract. Res. 2017, 38, 73–77. [Google Scholar]
- Krasin, E.; Schermann, H.; Snir, N.; Tudor, A.; Behrbalk, E. A Quick and Comprehensive Guide to Differential Diagnosis of Neck and Back Pain: A Narrative Review. SN Compr. Clin. Med. 2022, 4, 232. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bardin, L.D.; King, P.; Maher, C.G. Diagnostic triage for low back pain: A practical approach for primary care. Med. J. Aust. 2017, 206, 268–273. [Google Scholar] [CrossRef]
- Casser, H.R.; Seddigh, S.; Rauschmann, M. Acute Lumbar Back Pain: Investigation, Differential Diagnosis, and Treatment. Dtsch. Aerzteblatt Int. 2016, 113, 223–234. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Will, J.S.; Bury, D.C.; Miller, J.A. Mechanical Low Back Pain. Am. Fam. Physician 2018, 98, 421–428. [Google Scholar] [PubMed]
- Kinkade, S. Evaluation and treatment of acute low back pain. Am. Fam. Physician 2007, 75, 1181–1188. [Google Scholar] [PubMed]
- Lurie, J.D. What diagnostic tests are useful for low back pain? Best Pract. Res. Clin. Rheumatol. 2005, 19, 557–575. [Google Scholar] [CrossRef] [PubMed]
- Della-Giustina, D.A. Emergency department evaluation and treatment of back pain. Emerg. Med. Clin. N. Am. 1999, 17, 877–893. [Google Scholar] [CrossRef] [PubMed]
- Siemionow, K.; Steinmetz, M.; Bell, G.; Ilaslan, H.; McLain, R.F. Identifying serious causes of back pain: Cancer, infection, fracture. Clevel. Clin. J. Med. 2008, 75, 557–566. [Google Scholar] [CrossRef] [PubMed]
- Soar, H.; Comer, C.; Wilby, M.J.; Baranidharan, G. Lumbar radicular pain. BJA Educ. 2022, 22, 343–349. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Becker, J.A.; Stumbo, J.R. Back pain in adults. Prim. Care Clin. Off. Prac. 2013, 40, 271–288. [Google Scholar] [CrossRef] [PubMed]
- Borczuk, P. An evidence-based approach to the evaluation and treatment of low back pain in the emergency department. Emerg. Med. Pract. 2013, 15, 1–23. [Google Scholar] [PubMed]
- Winters, M.E.; Kluetz, P.; Zilberstein, J. Back pain emergencies. Med. Clin. 2006, 90, 505–523. [Google Scholar] [CrossRef]
- Corwell, B.N.; Davis, N.L. The emergent evaluation and treatment of neck and back pain. Emerg. Med. Clin. N. Am. 2020, 38, 167–191. [Google Scholar] [CrossRef] [PubMed]
- Della-Giustina, D. Acute low back pain: Recognizing the “red flags” in the workup. Consultant 360 2013, 53, 436–440. [Google Scholar] [CrossRef]
- Tavee, J.O.; Levin, K.H. Low Back Pain. Continuum (Minneap Minn) 2017, 23, 467–486. Available online: https://continuum.aan.com/doi/10.1212/CON.0000000000000449 (accessed on 8 March 2025). [CrossRef] [PubMed]
- Della-Giustina, D. Evaluation and treatment of acute back pain in the emergency department. Emerg. Med. Clin. N. Am. 2015, 33, 311–326. [Google Scholar] [CrossRef]
- Hayes, K.; Huckstadt, A.; Daggett, D. Acute Low Back Pain in the Emergency Department. Adv. Emerg. Nurs. J. 2006, 28, 234–247. [Google Scholar] [CrossRef]
- Harwood, M.I.; Smith, B.J. Low Back Pain: A Primary Care Approach. Clin. Fam. Pract. 2005, 7, 279–303. [Google Scholar] [CrossRef]
- Delladio, M.; Maselli, F.; Testa, M. Red flags or red herrings: What is the actual weight of the signs and symptoms of alarm in the evaluation of patients with low back pain/Red flags o red herrings [Qual e il reale peso dei segni e sintomi di allarme nella valutazione del paziente con lombalgia]. Sci. Riabil. 2013, 15, 5–23. Available online: https://link.gale.com/apps/doc/A331080126/AONE?u=anon~1cf485a3 (accessed on 8 March 2025).
- Almeida, D.C.; Kraychete, D.C. Low back pain—A diagnostic approach. Rev. Dor 2017, 18, 173–177. [Google Scholar] [CrossRef]
- Verhagen, A.P.; Downie, A.; Popal, N.; Maher, C.; Koes, B.W. Red flags presented in current low back pain guidelines: A review. Eur. Spine J. 2016, 25, 2788–2802. [Google Scholar] [CrossRef] [PubMed]
- Underwood, M. Diagnosing acute nonspecific low back pain: Time to lower the red flags? Arthritis Rheum. 2009, 60, 2855–2857. [Google Scholar] [CrossRef] [PubMed]
- Reito, A.; Kyrölä, K.; Pekkanen, L.; Paloneva, J. Specific spinal pathologies in adult patients with an acute or subacute atraumatic low back pain in the emergency department. Int. Orthop. 2018, 42, 2843–2849. [Google Scholar] [CrossRef] [PubMed]
- Cooney, F.; Graham, C.; Jeffrey, S.; Hellawell, M. Documentation of spinal red flags during physiotherapy assessment. Br. J. Healthc. Manag. 2017, 23, 574–580. [Google Scholar] [CrossRef]
- Chu, E.C.; Trager, R.J. Prevalence of Serious Pathology Among Adults with Low Back Pain Presenting for Chiropractic Care: A Retrospective Chart Review of Integrated Clinics in Hong Kong. Med Sci Monit. 2022, 28, E938042. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- van Tol, F.R.; Kamm, I.M.L.P.; Versteeg, A.L.; Suijkerbuijk, K.P.M.; Verkooijen, H.M.; Oner, C.; Verlaan, J.J. The use of red flags during the referral chain of patients surgically treated for symptomatic spinal metastases. Neurooncol Pract. 2023, 10, 301–306. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Premkumar, A.; Godfrey, W.; Gottschalk, M.B.; Boden, S.D. Red Flags for Low Back Pain Are Not Always Really Red: A Prospective Evaluation of the Clinical Utility of Commonly Used Screening Questions for Low Back Pain. J. Bone Jt. Surg. Am. 2018, 100, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Erausquin, T.I.; Rosado Pardo, J.A.; Vital, J.M.; Sarotto, A.J.; Besse, M. Manifestación clínica inicial de la lipomatosis epidural lumbar grado III de Naka: Serie de casos. Rev. Asoc. Argent. Ortop. Traumatol. 2024, 89, 6–14. [Google Scholar] [CrossRef]
- Henschke, N.; Maher, C.G.; Refshauge, K.M.; Herbert, R.D.; Cumming, R.G.; Bleasel, J.; York, J.; Das, A.; McAuley, J.H. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum. 2009, 60, 3072–3080. [Google Scholar] [CrossRef] [PubMed]
- Tsiang, J.T.; Kinzy, T.G.; Thompson, N.; Tanenbaum, J.E.; Thakore, N.L.; Khalaf, T.; Katzan, I.L. Sensitivity and specificity of patient-entered red flags for lower back pain. Spine J. 2019, 19, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Feller, D.; Chiarotto, A.; Koes, B.; Maselli, F.; Mourad, F. Red flags for potential serious pathologies in people with neck pain: A systematic review of clinical practice guidelines. Arch Physiother. 2024, 14, 105–115. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Variables | Number of Studies |
|---|---|
| TOTAL STUDIES | 30 |
| Nation | |
| Usa | 9 |
| Brazil | 7 |
| Portugal | 4 |
| Italy | 3 |
| Hong Kong | 2 |
| Pakistan | 2 |
| South Korea | 1 |
| Singapore | 1 |
| India | 1 |
| Denmark | 1 |
| Colombia | 1 |
| Cile | 1 |
| Year | |
| Last 10 years (2014–2025) | 22 |
| Previous studies (1999–2013) | 8 |
| Variables | Number of Participants |
| TOTAL PARTECIPANTS | 32 |
| Men | 15 |
| Women | 17 |
| Age | |
| ≤20 years | 5 |
| >20 and ≤ 50 years old | 10 |
| >50 and < 65 years old | 9 |
| ≥65 years old | 8 |
| Setting | |
| Direct access to the clinic or hospital | 23 |
| Chiropractor clinic/private practice | 6 |
| Private practice physiotherapist | 3 |
| Onset | |
| Acute spontaneous (until 3 months) | 10 |
| Chronic spontaneous (3 months onwards) | 18 |
| With causes | 3 |
| Not reported | 1 |
| Comorbidities | |
| Cancer | 14 |
| Smoking and alcohol | 2 |
| Chronic exposure wood smoke | 1 |
| Cardiac/vascular disorders | 4 |
| Neurological Diseases | 1 |
| Diabetes | 3 |
| Kidney disorders | 1 |
| Thyroid Diseases | 1 |
| Gastrointestinal Disorders | 3 |
| Orthopedic Pathologies | 2 |
| Obesity | 2 |
| Rheumatic Diseases | 1 |
| Gynecological pathologies | 2 |
| Pregnancy | 1 |
| Not reported | 16 |
| Clinical signs | |
| Lumbar pain | 32 |
| Abdominal pain | 6 |
| Abdominal stiffness | 3 |
| Chest pain | 1 |
| Fever/Chills | 1 |
| Lumbar tenderness | 7 |
| Reduced range of movement (ROM) | 4 |
| Radiating pain | 14 |
| Neurological signs | 22 |
| Muscle weakness | 9 |
| Reduction in osteotendinous reflexes | 3 |
| Presence of palpable mass | 2 |
| Scoliosis | 2 |
| Dysuria | 1 |
| Clenched Fist Percussion Test | 1 |
| Supine Sign | 1 |
| Renal Murphy sign | 1 |
| Asthenia | 1 |
| Adynamia | 1 |
| Hemoptysis | 1 |
| Images and findings | |
| Colonoscopy | 2 |
| Cystoscopy | 2 |
| Esophagogastroduodenoscopy | 1 |
| Fluorescent in situ hybridization | 1 |
| Magnetic resonance imaging | 23 |
| Scintigraphy | 3 |
| Ultrasounds | 4 |
| PET positron emission tomography | 5 |
| CT Computed Axial Tomography | 18 |
| Mammography | 1 |
| X-rays | 23 |
| Biopsy | 20 |
| PSA Testing | 2 |
| Blood test | 17 |
| Diagnosis | |
| Breast cancer | 1 |
| Stomach cancer | 2 |
| Lung cancer | 2 |
| Colon cancer | 2 |
| Prostate cancer | 2 |
| Pancreatic cancer | 1 |
| Kidney cancer | 1 |
| Pelvic cancer | 1 |
| Penis cancer | 1 |
| Urothelial cancer | 1 |
| Appendix cancer | 1 |
| Ewing Sarcoma | 3 |
| Lumbar Schwannoma | 2 |
| Leukemia | 1 |
| Primary Bone Liposarcoma | 1 |
| Osteoid osteoma | 2 |
| Secondary metastatic lesion | 17 |
| Cavernous Angioma | 1 |
| Giant cell cancer | 1 |
| Mastocytosis | 1 |
| Neurofibroma | 1 |
| Inflammatory myofibroblastic cancer | 1 |
| Reported results | |
| Treated | 3 |
| Partially care for | 9 |
| Dead | 5 |
| In treatment | 10 |
| Not reported | 5 |
| Red Flags | Explicitly Reported as Absent | Inferred from Clinical Data | Reported by Authors | Not Mentioned |
|---|---|---|---|---|
| Failure of conservative treatment | 0 | 17 | 4 | 11 |
| Pain duration > 3 months | 0 | 17 | 0 | 15 |
| Age > 50 | 0 | 16 | 1 | 15 |
| Progressively worsening pain | 0 | 11 | 1 | 20 |
| Abnormal blood tests | 0 | 7 | 0 | 25 |
| Radiating pain | 4 | 9 | 0 | 19 |
| Pain duration > 1 month | 0 | 7 | 0 | 25 |
| Age < 18 | 0 | 4 | 0 | 28 |
| Systemic symptoms (fever, chills, night sweats, fatigue, malaise) | 9 | 11 | 1 | 11 |
| Night pain | 0 | 6 | 5 | 21 |
| Neurological signs (reduced sensitivity, loss of sphincter control, gait deficit, altered reflexes) | 9 | 22 | 0 | 5 |
| History of cancer (personal) | 2 | 10 | 3 | 17 |
| History of surgery | 0 | 5 | 0 | 27 |
| Abdominal pain | 3 | 6 | 0 | 23 |
| Motor weakness | 1 | 9 | 0 | 22 |
| Unexplained weight loss | 3 | 8 | 3 | 18 |
| Family history of cancer | 1 | 5 | 0 | 26 |
| Severe and continuous pain | 0 | 4 | 2 | 26 |
| C-reactive protein > 10 mg/L | 0 | 3 | 0 | 29 |
| Bladder dysfunction (urinary retention or incontinence) | 8 | 11 | 0 | 23 |
| Palpable mass | 0 | 1 | 0 | 31 |
| Bowel dysfunction | 7 | 11 | 0 | 24 |
| Saddle anesthesia | 1 | 2 | 0 | 29 |
| Recent trauma | 1 | 1 | 0 | 30 |
| Recent infection | 0 | 1 | 0 | 31 |
| Smoking history | 0 | 1 | 0 | 31 |
| Pregnancy | 0 | 1 | 0 | 31 |
| Pain differing from previous episodes | 0 | 1 | 0 | 31 |
| Chronic exposure to wood smoke | 0 | 1 | 0 | 31 |
| Constant non-provocative pain | 0 | 1 | 0 | 31 |
| Improvement with NSAIDs | 0 | 0 | 2 | 30 |
| Change in symptom quality and pain resistant to analgesics | 0 | 0 | 1 | 31 |
| Figure | Type of Study | Red Flag | Diagnostic Accuracy |
|---|---|---|---|
| Premkumar 2018 [90] | Retrospective observational study | Age > 50 | Se 0.717; Sp 0.326; LR+ 1.060 (0.960–1.170); LR− 0.870 (0.680–1.110) |
| Age > 70 | Se 0.226; Sp 0.795; LR+ 1.100 (0.820–1.470); LR− 0.970 (0.90–1.060) | ||
| Henschke 2009 [92] | Prospective Cohort Study | Age > 50 | Sp 0.660 (0.630; 0.690) |
| Age > 70 | Sp 0.950 (0.940; 0.960) |
| First Author and Year of Publication | Type of Study | RF | Diagnostic Accuracy |
|---|---|---|---|
| Tsiang 2019 [93] | Retrospective case–control study | History of cancer | Se 0.917 Sp 0.778 |
| Night pain | Se 0.542 (0.328; 0.744) Sp 0.496 (0.448; 0.543) | ||
| Pain at rest | Se 0.250 (0.098; 0.467) Sp 0.698 (0.653; 0.740) | ||
| Urinary retention | Se 0.042 (0.001; 0.211) Sp0.958 (0.935; 0.974) | ||
| Premkumar 2018 [90] | Retrospective cohort study | History of cancer | Se 0.320; Sp 0.956; LR+ 7.250 (5.650;9.300); LR− 0.710 (0.640; 0.790) |
| Night pain | Se 0.554; Sp 0.418; LR+ 0.850 (0.830; 1.100); LR− 1.070 (0.900; 1.270) | ||
| Unexplained weight loss | Se 0.082; Sp 0.956; LR+ 1.870 (1.100; 3.170); LR− 0.960 (0.920; 1.010) | ||
| Henschke 2009 [92] | Prospective Cohort Study | History of cancer | Se 0.000 (0.000; 0.000); Sp 0.960 (0.950; 0.970) |
| Unexplained weight loss | Se 0.000 (0.000; 0.000); Sp 1.000 (0.990; 1.000) | ||
| Constant, progressive, non-mechanical pain | Se 0.000 (0.000; 0.000); Sp 0.970 (0.960; 0.980) | ||
| Gradual onset before the age of 40 | Se 0.000 (0.000; 0.000); Sp 0.910 (0.900; 0.930) | ||
| Insidious Onset | Se 0.000 (0.000, 0.000); Sp 0.830 (0.800; 0.850) | ||
| Systemic malaise | Se 0.000; Sp 0.980 (0.970; 0.980) |
| First Author and Year of Publication | Type of Study | RF | Diagnostic Accuracy |
|---|---|---|---|
| Henschke 2009 [92] | Prospective Cohort Study | Altered sensation from the trunk down | Se 0.000 (0.000; 0.000); Sp 0.980 (0.970; 0.990) |
| First Author and Year of Publication | Type of Study | Red Flag Combinations | Diagnostic Accuracy |
|---|---|---|---|
| Premkumar 2018 [90] | Retrospective cohort study | Combination of unexplained weight loss and history of cancer | Se 0.025; Sp 0.998; LR+ 10.250 (3.600; 29.210); LR− 0.980 (0.950; 1.000) |
| First Author and Year of Publication | Type of Study | Red Flag Combinations | Diagnostic Accuracy |
|---|---|---|---|
| Henschke 2013 [60] | Systematic review | Combination of age > 50 years, history of cancer, unexplained weight loss, and failure to improve with conservative therapy | Se 1.000 |
| Delladio 2013 [82] | Narrative review | Age combination > 50 years, history of cancer, unexplained weight loss, no improvement after one month | Se 1.000; Sp 0.600; LR+ 2.400; LR− 0.060; |
| Red Flag (RF) | Sensitivity | Specificity | LR+ | LR− | Source |
|---|---|---|---|---|---|
| Age > 50 years | 0.717 | 0.326 | 1.060 | 0.870 | Premkumar et al. [90] |
| History of cancer | 0.320 | 0.956 | 7.250 | 0.710 | Premkumar et al. [90] |
| Unexplained weight loss | 0.082 | 0.956 | 1.870 | 0.960 | Premkumar et al. [90] |
| Constant, progressive, non-mechanical pain | 0.000 | 0.9700 | 0.000 | 1.030 | Henschke et al. [92] |
| Combination of unexplained weight loss and history of cancer | 0.025 | 0.998 | 10.250 | 0.980 | Premkumar et al. [90] |
| Age combination > 50 years, history of cancer, unexplained weight loss, no improvement after one month | 1.000 | 0.600 | 2.400 | 0.060 | Delladio et al. [82] (data from secondary sources) |
| Combination of: history of cancer, age > 50, weight loss, failure of conservative treatment | 1.000 | — | — | — | Henschke et al. [60] (data from secondary sources) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Notarangelo, G.; Margelli, M.; Giovannico, G.; Bruno, F.; Milella, C.; Feller, D.; Dunning, J.; Storari, L.; Mourad, F.; Maselli, F. Diagnostic Utility of Red Flags for Detecting Spinal Malignancies in Patients with Low Back Pain: A Scoping Review. J. Clin. Med. 2025, 14, 7174. https://doi.org/10.3390/jcm14207174
Notarangelo G, Margelli M, Giovannico G, Bruno F, Milella C, Feller D, Dunning J, Storari L, Mourad F, Maselli F. Diagnostic Utility of Red Flags for Detecting Spinal Malignancies in Patients with Low Back Pain: A Scoping Review. Journal of Clinical Medicine. 2025; 14(20):7174. https://doi.org/10.3390/jcm14207174
Chicago/Turabian StyleNotarangelo, Gianluca, Michele Margelli, Giuseppe Giovannico, Francesco Bruno, Claudia Milella, Daniel Feller, James Dunning, Lorenzo Storari, Firas Mourad, and Filippo Maselli. 2025. "Diagnostic Utility of Red Flags for Detecting Spinal Malignancies in Patients with Low Back Pain: A Scoping Review" Journal of Clinical Medicine 14, no. 20: 7174. https://doi.org/10.3390/jcm14207174
APA StyleNotarangelo, G., Margelli, M., Giovannico, G., Bruno, F., Milella, C., Feller, D., Dunning, J., Storari, L., Mourad, F., & Maselli, F. (2025). Diagnostic Utility of Red Flags for Detecting Spinal Malignancies in Patients with Low Back Pain: A Scoping Review. Journal of Clinical Medicine, 14(20), 7174. https://doi.org/10.3390/jcm14207174








