Traditional Korean Medicine Services and Its Association with Knee Surgery and Opioid Use in Patients with Knee Osteoarthritis: A Nationwide Retrospective Study in Korea
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
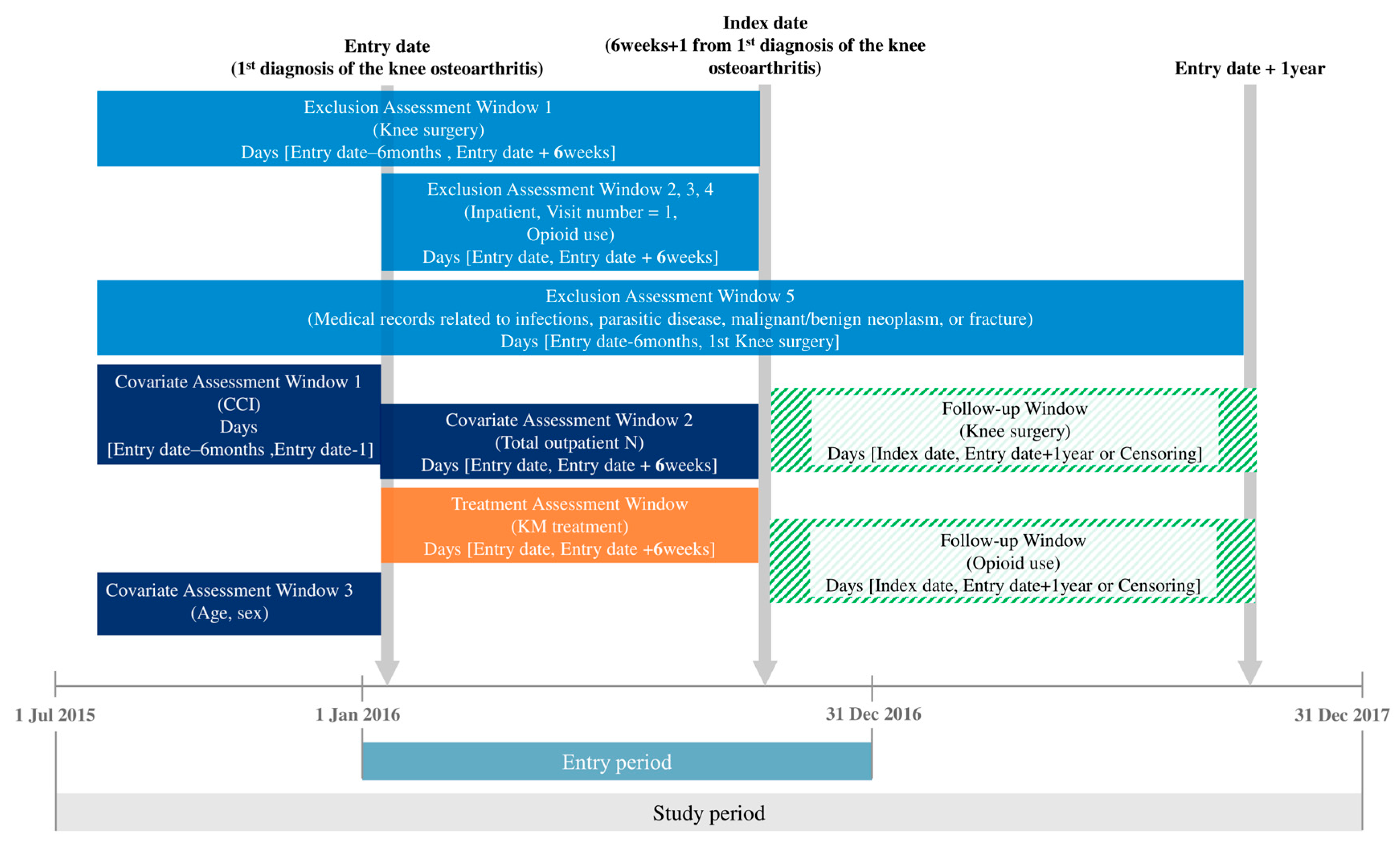
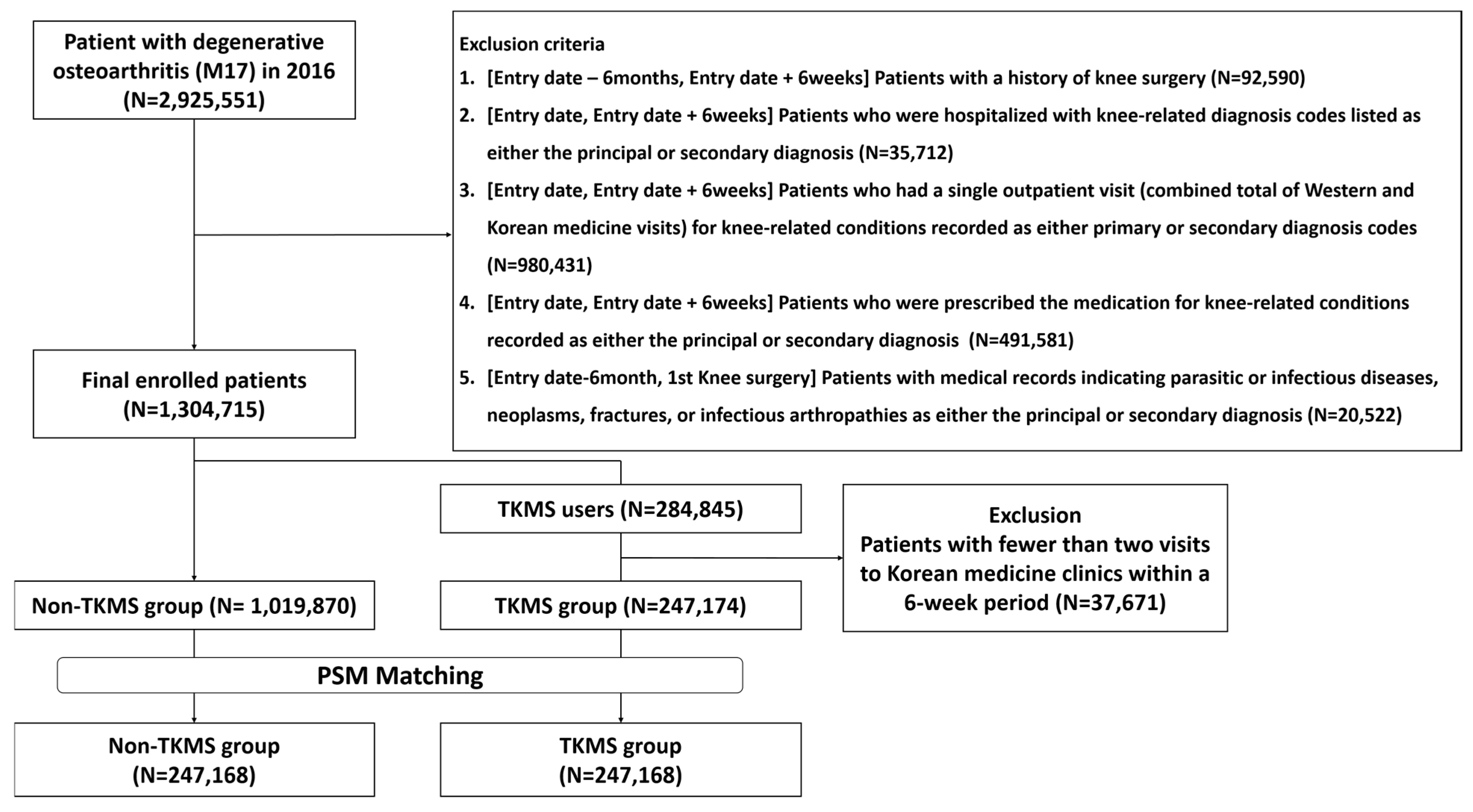
2.2. Study Population
2.3. Intervention
2.4. Outcome Measures
2.5. Statistical Analysis
3. Results
3.1. Baseline Statistics
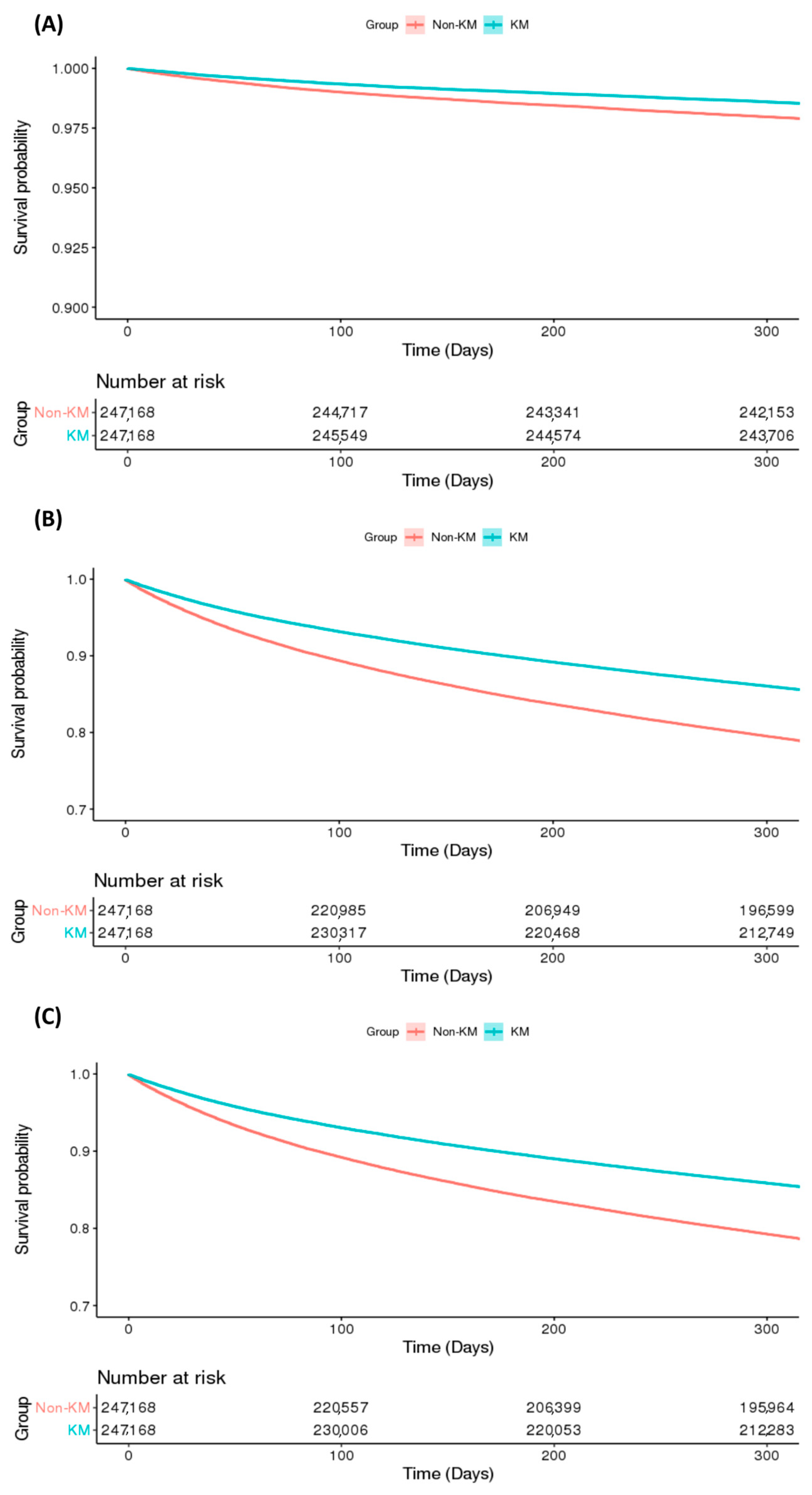
3.2. Comparison of Knee Surgery and Opioid Use by TKMS Use
3.3. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CCI | Charlson comorbidity index |
| CI | Confidence interval |
| HIRA | Health Insurance Review and Assessment Service |
| HR | Hazard ratio |
| KM | Korean medicine |
| KOA | Knee osteoarthritis |
| PH | Proportional hazard |
| PSM | Propensity score matching |
| SMD | Standardized mean difference |
| TKA | Total knee arthroplasty |
References
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and treatment of hip and knee osteoarthritis: A review. JAMA 2021, 325, 568–578. [Google Scholar] [CrossRef]
- Cui, A.; Li, H.; Wang, D.; Zhong, J.; Chen, Y.; Lu, H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. eClinicalMedicine 2020, 29, 100587. [Google Scholar] [CrossRef]
- Korean Statistical Information Service. Available online: https://kosis.kr/statHtml/statHtml.do?orgId=350&tblId=TX_35001_A061&conn_path=I2 (accessed on 28 August 2025).
- Michael, J.W.; Schlüter-Brust, K.U.; Eysel, P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch. Aerzteblatt Online 2010, 107, 152–162. [Google Scholar] [CrossRef]
- Taqi, A.O.H.; Knaggs, R. Trends in opioid prescribing in primary care patients with knee osteoarthritis: A population based observational study. Value Health 2017, 20, A540–A541. [Google Scholar] [CrossRef]
- Brophy, R.H.; Fillingham, Y.A. AAOS Clinical Practice Guideline Summary: Management of Osteoarthritis of the Knee (Nonarthroplasty), Third Edition. J. Am. Acad. Orthop. Surg. 2022, 30, e721–e729. [Google Scholar] [CrossRef]
- Benyamin, R.; Trescot, A.M.; Datta, S.; Buenaventura, R.M.; Adlaka, R.; Sehgal, N.; Glaser, S.E.; Vallejo, R. Opioid complications and side effects. Pain Physician 2008, 11, S105. [Google Scholar] [CrossRef]
- Kan, H.; Chan, P.; Chiu, K.; Yan, C.; Yeung, S.; Ng, Y.; Shiu, K.; Ho, T. Non-surgical treatment of knee osteoarthritis. Hong Kong Med. J. 2019, 25, 127–133. [Google Scholar] [CrossRef]
- Peng, H.; Ou, A.; Huang, X.; Wang, C.; Wang, L.; Yu, T.; Zhang, Y.; Zhang, Y. Osteotomy around the knee: The surgical treatment of osteoarthritis. Orthop. Surg. 2021, 13, 1465–1473. [Google Scholar] [CrossRef]
- Quinn, R.H.; Murray, J.N.; Pezold, R.; Sevarino, K.S. Surgical Management of Osteoarthritis of the Knee. J. Am. Acad. Orthop. Surg. 2018, 26, e191–e193. [Google Scholar] [CrossRef]
- Wang, K.; Xing, D.; Dong, S.; Lin, J. The global state of research in nonsurgical treatment of knee osteoarthritis: A bibliometric and visualized study. BMC Musculoskelet. Disord. 2019, 20, 407 . [Google Scholar] [CrossRef]
- Lim, B. Korean medicine coverage in the National Health Insurance in Korea: Present situation and critical issues. Integr. Med. Res. 2013, 2, 81–88. [Google Scholar] [CrossRef]
- Kessler, C.S.; Dhiman, K.S.; Kumar, A.; Ostermann, T.; Gupta, S.; Morandi, A.; Mittwede, M.; Stapelfeldt, E.; Spoo, M.; Icke, K. Effectiveness of an Ayurveda treatment approach in knee osteoarthritis—A randomized controlled trial. Osteoarthr. Cartil. 2018, 26, 620–630. [Google Scholar] [CrossRef]
- Stoll, V.; Trube, J.; Johnson, T.; Darbhanga, J.; Mehra, R.S. The Role of Osteopathic Manipulative Treatment in Osteoarthritis: A Scoping Review. Cureus 2024, 16, e74440. [Google Scholar] [CrossRef]
- Reichardt, A.; Passmore, S.R.; Toth, A.; Olin, G. Utilization of chiropractic services in patients with osteoarthritis and spine pain at a publicly funded healthcare facility in Canada: A retrospective study. J. Back Musculoskelet. Rehabil. 2022, 35, 1075–1084. [Google Scholar] [CrossRef]
- Witt, C.; Brinkhaus, B.; Jena, S.; Linde, K.; Streng, A.; Wagenpfeil, S.; Hummelsberger, J.; Walther, H.; Melchart, D.; Willich, S. Acupuncture in patients with osteoarthritis of the knee: A randomised trial. Lancet 2005, 366, 136–143. [Google Scholar] [CrossRef]
- Kim, T.-H.; Kim, K.H.; Kang, J.W.; Lee, M.; Kang, K.-W.; Kim, J.E.; Kim, J.-H.; Lee, S.; Shin, M.-S.; Jung, S.-Y. Moxibustion treatment for knee osteoarthritis: A multi-centre, non-blinded, randomised controlled trial on the effectiveness and safety of the moxibustion treatment versus usual care in knee osteoarthritis patients. PLoS ONE 2014, 9, e101973. [Google Scholar] [CrossRef]
- Chen, N.; Wang, J.; Mucelli, A.; Zhang, X.; Wang, C. Electro-acupuncture is beneficial for knee osteoarthritis: The evidence from meta-analysis of randomized controlled trials. Am. J. Chin. Med. 2017, 45, 965–985. [Google Scholar] [CrossRef]
- Lee, S.K.; Oh, E.J.; Bae, G.H.; Woo, J.H.; Lee, Y.J.; Ha, I.-H.; Kim, J.Y.; Kim, D. Integrative Korean medicine treatment for inpatients with osteoarthritis of the knee: An observational study. Medicine 2024, 103, e39183. [Google Scholar] [CrossRef]
- Health Insurance Review & Assessment Service. Opendata. Available online: https://opendata.hira.or.kr/or/orb/A/rsrcrList.do?rsrcTaskId=M20241029002#none (accessed on 1 June 2025).
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- World Health Organization. Introduction to Drug Utilization Research. Available online: https://apps.who.int/iris/handle/10665/42627 (accessed on 9 September 2025).
- Koch, E.; Johnell, K.; Kauppi, K. Longitudinal effects of using and discontinuing central nervous system medications on cognitive functioning. Pharmacoepidemiol. Drug Saf. 2023, 32, 446–454. [Google Scholar] [CrossRef]
- Numan, L.; Ramjankhan, F.Z.; Oberski, D.L.; Oerlemans, M.I.; Aarts, E.; Gianoli, M.; Van Der Heijden, J.J.; De Jonge, N.; Van Der Kaaij, N.P.; Meuwese, C.L. Propensity score-based analysis of long-term outcome of patients on HeartWare and HeartMate 3 left ventricular assist device support. ESC Heart Fail. 2021, 8, 1596–1603. [Google Scholar] [CrossRef]
- Andrade, C. Survival analysis, Kaplan-Meier curves, and Cox regression: Basic concepts. Indian J. Psychol. Med. 2023, 45, 434–435. [Google Scholar] [CrossRef]
- Levinger, P.; Menz, H.B.; Wee, E.; Feller, J.A.; Bartlett, J.R.; Bergman, N.R. Physiological risk factors for falls in people with knee osteoarthritis before and early after knee replacement surgery. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1082–1089. [Google Scholar] [CrossRef]
- Charlesworth, J.; Fitzpatrick, J.; Perera, N.K.P.; Orchard, J. Osteoarthritis- a systematic review of long-term safety implications for osteoarthritis of the knee. BMC Musculoskelet Disord. 2019, 20, 151. [Google Scholar] [CrossRef]
- Kjellberg, J.; Kehlet, H. A nationwide analysis of socioeconomic outcomes after hip and knee replacement. Dan Med. J. 2016, 63, A5257. [Google Scholar]
- Huizinga, J.L.; Stanley, E.E.; Sullivan, J.K.; Song, S.; Hunter, D.J.; Paltiel, A.D.; Neogi, T.; Edwards, R.R.; Katz, J.N.; Losina, E. Societal cost of opioid use in symptomatic knee osteoarthritis patients in the United States. Arthritis Care Res. 2022, 74, 1349–1358. [Google Scholar] [CrossRef]
- Krebs, E.E.; Gravely, A.; Nugent, S.; Jensen, A.C.; DeRonne, B.; Goldsmith, E.S.; Kroenke, K.; Bair, M.J.; Noorbaloochi, S.J.J. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: The SPACE randomized clinical trial. JAMA 2018, 319, 872–882. [Google Scholar] [CrossRef]
- Fuggle, N.; Curtis, E.; Shaw, S.; Spooner, L.; Bruyère, O.; Ntani, G.; Parsons, C.; Conaghan, P.G.; Corp, N.; Honvo, G.J.D.; et al. Safety of opioids in osteoarthritis: Outcomes of a systematic review and meta-analysis. Drugs Aging 2019, 36, 129–143. [Google Scholar] [CrossRef]
- Thorlund, J.; Turkiewicz, A.; Prieto-Alhambra, D.; Englund, M. Opioid use in knee or hip osteoarthritis: A region-wide population-based cohort study. Osteoarthr. Cartil. 2019, 27, 871–877. [Google Scholar] [CrossRef]
- Maher, R.L.; Hanlon, J.; Hajjar, E.R. Clinical consequences of polypharmacy in elderly. Expert Opin. Drug Saf. 2014, 13, 57–65. [Google Scholar] [CrossRef]
- Hoel, R.W.; Connolly, R.M.G.; Takahashi, P.Y. Polypharmacy management in older patients. Mayo Clin. Proc. 2021, 96, 242–256. [Google Scholar] [CrossRef]
- Jyrkkä, J.; Enlund, H.; Lavikainen, P.; Sulkava, R.; Hartikainen, S. Association of polypharmacy with nutritional status, functional ability and cognitive capacity over a three-year period in an elderly population. Pharmacoepidemiol. Drug Saf. 2011, 20, 514–522. [Google Scholar] [CrossRef]
- Liu, C.-Y.; Duan, Y.-S.; Zhou, H.; Wang, Y.; Tu, J.-F.; Bao, X.-Y.; Yang, J.-W.; Lee, M.S.; Wang, L.-Q. Clinical effect and contributing factors of acupuncture for knee osteoarthritis: A systematic review and pairwise and exploratory network meta-analysis. BMJ Evid.-Based Med. 2024, 29, 374–384. [Google Scholar] [CrossRef]
- Zahlan, G.; De Clifford-Faugère, G.; Nguena Nguefack, H.L.; Guénette, L.; Pagé, M.G.; Blais, L.; Lacasse, A. Polypharmacy and excessive polypharmacy among persons living with chronic pain: A cross-sectional study on the prevalence and associated factors. J. Pain Res. 2023, 16, 3085–3100. [Google Scholar] [CrossRef]
- Li, N.; Guo, Y.; Gong, Y.; Zhang, Y.; Fan, W.; Yao, K.; Chen, Z.; Dou, B.; Lin, X.; Chen, B.; et al. The Anti-Inflammatory Actions and Mechanisms of Acupuncture from Acupoint to Target Organs via Neuro-Immune Regulation. J. Inflamm. Res. 2021, 14, 7191–7224. [Google Scholar] [CrossRef]
- Wang, X.; Wang, J.; Han, R.; Yu, C.; Shen, F. Neural circuit mechanisms of acupuncture effect: Where are we now? Front. Neurol. 2024, 15, 1399925. [Google Scholar] [CrossRef]
- Liang, Y.; Xu, Y.; Zhu, Y.; Ye, H.; Wang, Q.; Xu, G. Efficacy and safety of Chinese herbal medicine for knee osteoarthritis: Systematic review and meta-analysis of randomized controlled trials. Phytomedicine 2022, 100, 154029. [Google Scholar] [CrossRef]
- Lee, Y.J.; Jo, H.R.; Kim, S.H.; Sung, W.S.; Kim, E.J. Efficacy and safety of pharmacopuncture and bee venom acupuncture for knee osteoarthritis: A systematic review and meta-analysis. J. Korean Med. 2020, 41, 55–83. [Google Scholar] [CrossRef]
- Lee, N.-W.; Kim, G.-H.; Heo, I.; Kim, K.-W.; Ha, I.-H.; Lee, J.-H.; Hwang, E.-H.; Shin, B.-C. Chuna (or Tuina) Manual Therapy for Musculoskeletal Disorders: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid.-Based Complement. Altern. Med. 2017, 2017, 8218139. [Google Scholar] [CrossRef]
- Kim, D.; Baek, G.G.; Shin, B.-C. An umbrella review of systematic reviews for Chuna (or Tuina) manual therapy on musculoskeletal disorders. Perspect. Integr. Med. 2023, 2, 142–154. [Google Scholar] [CrossRef]
- Vickers, A.J.; Vertosick, E.A.; Lewith, G.; MacPherson, H.; Foster, N.E.; Sherman, K.J.; Irnich, D.; Witt, C.M.; Linde, K. Acupuncture for chronic pain: Update of an individual patient data meta-analysis. J. Pain 2018, 19, 455–474. [Google Scholar] [CrossRef]
- Tu, J.F.; Yang, J.W.; Shi, G.X.; Yu, Z.S.; Li, J.L.; Lin, L.L.; Du, Y.Z.; Yu, X.G.; Hu, H.; Liu, Z.; et al. Efficacy of intensive acupuncture versus sham acupuncture in knee osteoarthritis: A randomized controlled trial. Arthritis Rheumatol. 2021, 73, 448–458. [Google Scholar] [CrossRef]
- Rush, B.; Fruhstorfer, C. Residual confounding prohibits interpretation of results after propensity score matching. Am. J. Cardiol. 2018, 121, 670. [Google Scholar] [CrossRef]
| n | Non-TKMS | TKMS | SMD | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Total N | 494,336 | 247,168 | 100.0 | 247,168 | 100.0 | - | |
| Sex | Male | 124,083 | 62,052 | 25.1 | 62,031 | 25.1 | 0.00 |
| Female | 370,253 | 185,116 | 74.9 | 185,137 | 74.9 | 0.00 | |
| Age_group | <40 | 23,623 | 11,806 | 4.8 | 11,817 | 4.8 | 0.00 |
| 40–49 | 39,746 | 19,889 | 8.1 | 19,857 | 8.0 | 0.00 | |
| 50–59 | 99,842 | 49,921 | 20.2 | 49,921 | 20.2 | 0.00 | |
| 60–69 | 144,042 | 72,021 | 29.1 | 72,021 | 29.1 | 0.00 | |
| 70–79 | 141,196 | 70,547 | 28.5 | 70,649 | 28.6 | 0.00 | |
| ≥80 | 45,887 | 22,984 | 9.3 | 22,903 | 9.3 | 0.00 | |
| Payer type | NHI | 494,336 | 247,168 | 100.0 | 247,168 | 100.0 | - |
| CCI_group | 0 | 321,832 | 160,886 | 65.1 | 160,946 | 65.1 | 0.00 |
| 1 | 109,688 | 54,879 | 22.2 | 54,809 | 22.2 | 0.00 | |
| ≥ 2 | 62,816 | 31,403 | 12.7 | 31,413 | 12.7 | 0.00 | |
| Total outpatient N | 2–5 | 293,374 | 146,687 | 59.4 | 146,687 | 59.4 | 0.00 |
| 6–11 | 142,445 | 71,247 | 28.8 | 71,198 | 28.8 | 0.00 | |
| ≥12 | 58,517 | 29,234 | 11.8 | 29,283 | 11.9 | 0.00 | |
| F/u surgery survival event | No | 485,359 | 241,862 | 97.9 | 243,497 | 98.5 | −0.05 |
| Yes | 8977 | 5306 | 2.2 | 3671 | 1.5 | 0.05 | |
| F/u opioid use survival event | No | 405,320 | 194,298 | 78.6 | 211,022 | 85.4 | −0.18 |
| Yes | 89,016 | 52,870 | 21.4 | 36,146 | 14.6 | 0.18 | |
| F/u surgery or opioid use survival event | No | 404,195 | 193,657 | 78.4 | 210,538 | 85.2 | −0.18 |
| Yes | 90,141 | 53,511 | 21.7 | 36,630 | 14.8 | 0.18 | |
| Variable | Knee Surgery | Opioid Use | Knee Surgery or Opioid Use | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value * | |
| TKMS use (ref. Non-TKMS) | ||||||
| KM | 0.69 (0.66–0.72) | <0.0001 | 0.66 (0.65–0.66) | <0.0001 | 0.66 (0.65–0.67) | <0.0001 |
| Multivariate model | ||||||
| TKMS use (ref. Non-TKMS) | ||||||
| KM | 0.69 (0.66–0.72) | <0.0001 | 0.65 (0.64–0.66) | <0.0001 | 0.65 (0.64–0.66) | <0.0001 |
| Sex (ref. Male) | ||||||
| Female | 1.25 (1.18–1.31) | <0.0001 | 1.23 (1.21–1.25) | <0.0001 | 1.22 (1.20–1.24) | <0.0001 |
| Age (ref. <40) | ||||||
| 40–49 | 1.11 (0.96–1.28) | 0.1598 | 1.61 (1.51–1.71) | <0.0001 | 1.59 (1.49–1.69) | <0.0001 |
| 50–59 | 1.33 (1.17–1.50) | <0.0001 | 2.51 (2.37–2.66) | <0.0001 | 2.44 (2.31–2.58) | <0.0001 |
| 60–69 | 1.48 (1.30–1.67) | <0.0001 | 3.29 (3.11–3.48) | <0.0001 | 3.15 (2.98–3.33) | <0.0001 |
| 70–79 | 1.66 (1.47–1.88) | <0.0001 | 4.16 (3.92–4.40) | <0.0001 | 3.95 (3.74–4.17) | <0.0001 |
| ≥80 | 0.79 (0.67–0.91) | 0.0013 | 4.20 (3.96–4.45) | <0.0001 | 3.97 (3.75–4.20) | <0.0001 |
| CCI (ref. 0) | ||||||
| 1 | 0.91 (0.86–0.95) | 0.0002 | 1.10 (1.08–1.12) | <0.0001 | 1.10 (1.08–1.11) | <0.0001 |
| 2 | 0.58 (0.54–0.62) | <0.0001 | 1.07 (1.05–1.09) | <0.0001 | 1.06 (1.04–1.08) | <0.0001 |
| Total outpatient N (ref. 2–5) | ||||||
| 6–11 | 1.56 (1.49–1.63) | <0.0001 | 1.31 (1.29–1.33) | <0.0001 | 1.32 (1.30–1.34) | <0.0001 |
| ≥12 | 1.62 (1.52–1.72) | <0.0001 | 1.34 (1.32–1.37) | <0.0001 | 1.35 (1.32–1.38) | <0.0001 |
| TKMS Use | Non-TKMS | |||||
|---|---|---|---|---|---|---|
| Matched Number | Event | Matched Number | Event | HR (95%CI) | p-Value * | |
| n | n (%) | n | n (%) | |||
| Knee surgery | ||||||
| 4 weeks | 235,249 | 3765 | 235,249 | 5493 | 0.68 (0.66–0.71) | <0.0001 |
| 8 weeks | 255,971 | 3601 | 255,971 | 5063 | 0.71 (0.68–0.74) | <0.0001 |
| 10 weeks | 262,747 | 3438 | 262,747 | 4833 | 0.71 (0.68–0.74) | < 0.0001 |
| Opioid use | ||||||
| 4 weeks | 235,249 | 36,471 | 235,249 | 53,185 | 0.65 (0.64–0.66) | <0.0001 |
| 8 weeks | 255,971 | 35,429 | 255,971 | 52,005 | 0.65 (0.64–0.66) | <0.0001 |
| 10 weeks | 262,747 | 34,348 | 262,747 | 50,332 | 0.65 (0.64–0.66) | <0.0001 |
| Surgery or opioid use | ||||||
| 4 weeks | 235,249 | 36,975 | 235,249 | 53,876 | 0.65 (0.64–0.66) | <0.0001 |
| 8 weeks | 255,971 | 35,890 | 255,971 | 52,616 | 0.65 (0.64–0.66) | <0.0001 |
| 10 weeks | 262,747 | 34,799 | 262,747 | 50,900 | 0.65 (0.65–0.66) | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seok, H.W.; Go, H.-Y.; Ryu, W.-H.; Lee, Y.J.; Ha, I.-H.; Kim, D. Traditional Korean Medicine Services and Its Association with Knee Surgery and Opioid Use in Patients with Knee Osteoarthritis: A Nationwide Retrospective Study in Korea. J. Clin. Med. 2025, 14, 7152. https://doi.org/10.3390/jcm14207152
Seok HW, Go H-Y, Ryu W-H, Lee YJ, Ha I-H, Kim D. Traditional Korean Medicine Services and Its Association with Knee Surgery and Opioid Use in Patients with Knee Osteoarthritis: A Nationwide Retrospective Study in Korea. Journal of Clinical Medicine. 2025; 14(20):7152. https://doi.org/10.3390/jcm14207152
Chicago/Turabian StyleSeok, Hwang Woo, Ho-Yeon Go, Won-Hyung Ryu, Yoon Jae Lee, In-Hyuk Ha, and Doori Kim. 2025. "Traditional Korean Medicine Services and Its Association with Knee Surgery and Opioid Use in Patients with Knee Osteoarthritis: A Nationwide Retrospective Study in Korea" Journal of Clinical Medicine 14, no. 20: 7152. https://doi.org/10.3390/jcm14207152
APA StyleSeok, H. W., Go, H.-Y., Ryu, W.-H., Lee, Y. J., Ha, I.-H., & Kim, D. (2025). Traditional Korean Medicine Services and Its Association with Knee Surgery and Opioid Use in Patients with Knee Osteoarthritis: A Nationwide Retrospective Study in Korea. Journal of Clinical Medicine, 14(20), 7152. https://doi.org/10.3390/jcm14207152






