Effect of Open-Wedge High Tibial Osteotomy and Lateral Retinacular Release on the Articular Cartilage of the Patellofemoral Joint: Analysis Using Magnetic Resonance Imaging T2 Mapping
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Cohort
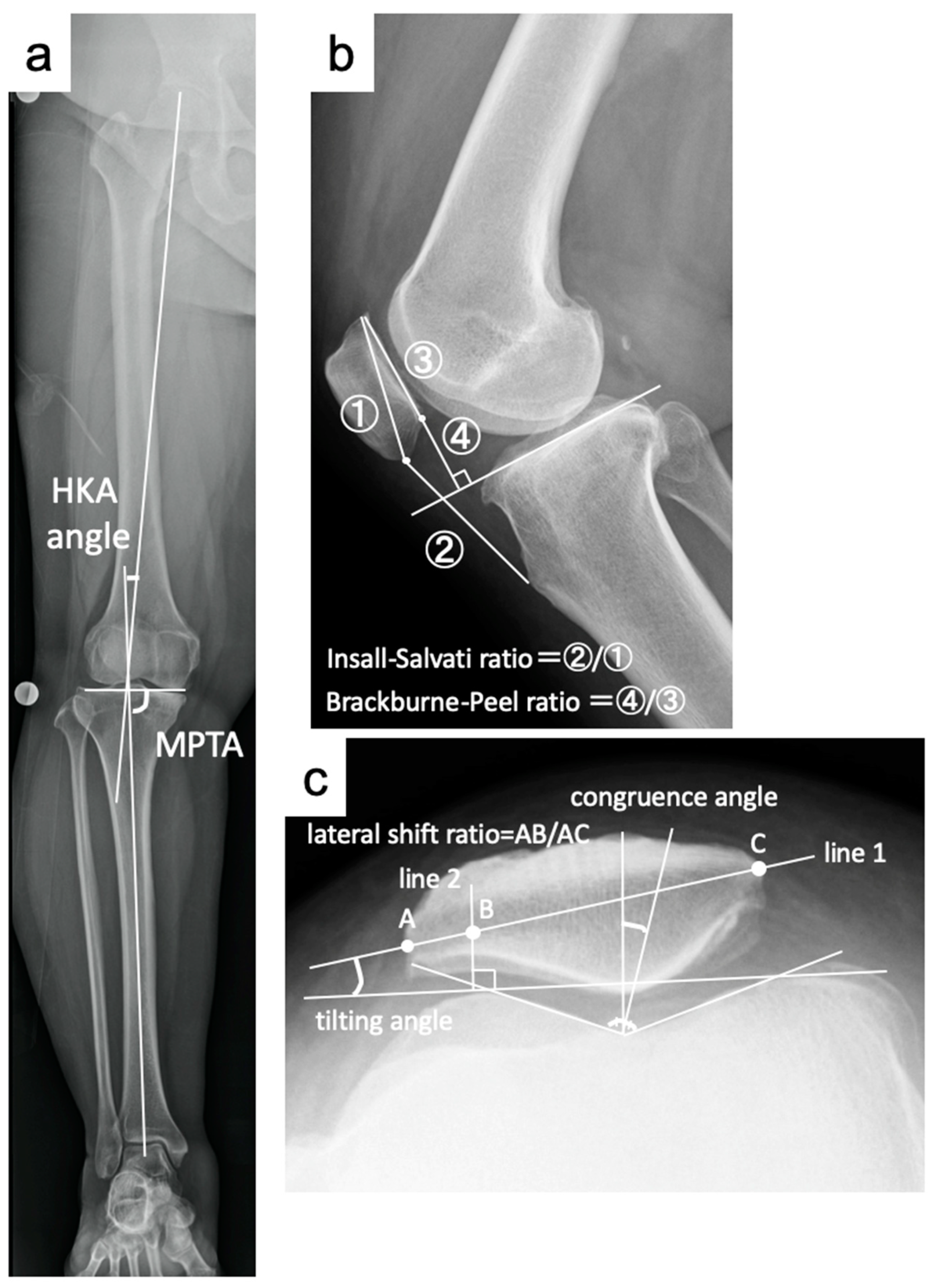
2.2. Radiological Evaluation
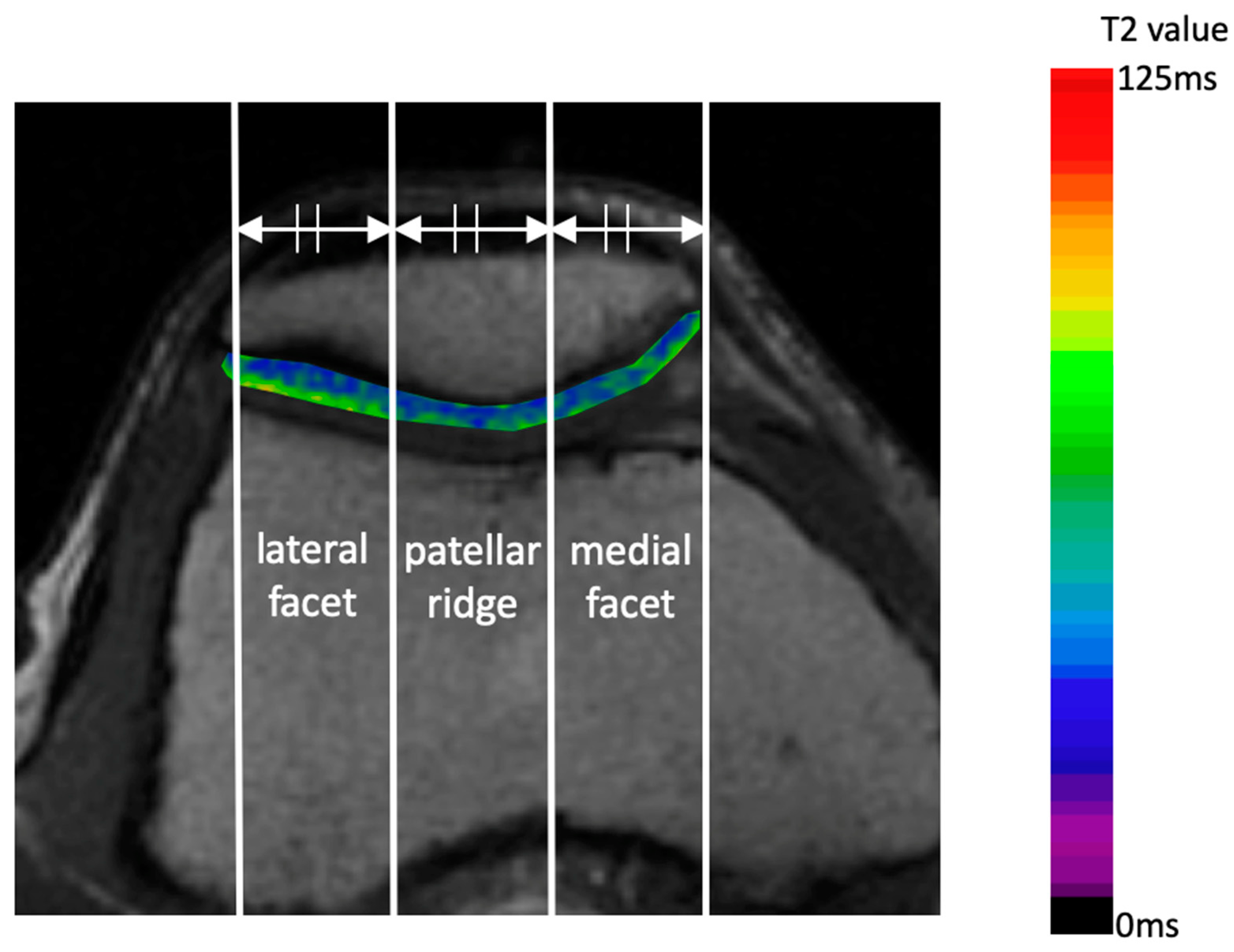
2.3. MRI T2 Mapping
2.4. Surgical Procedure
2.5. Statistical Analysis
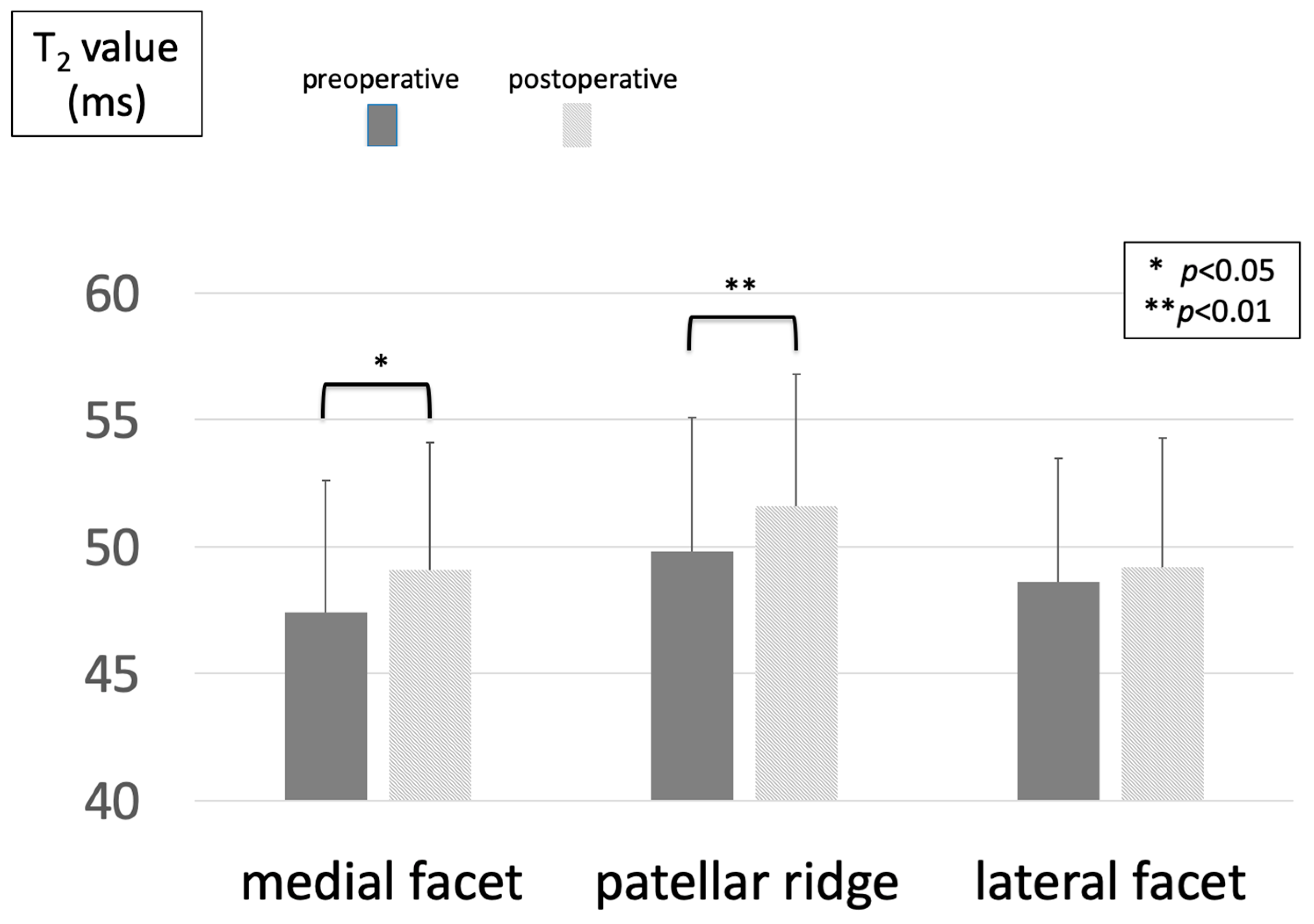
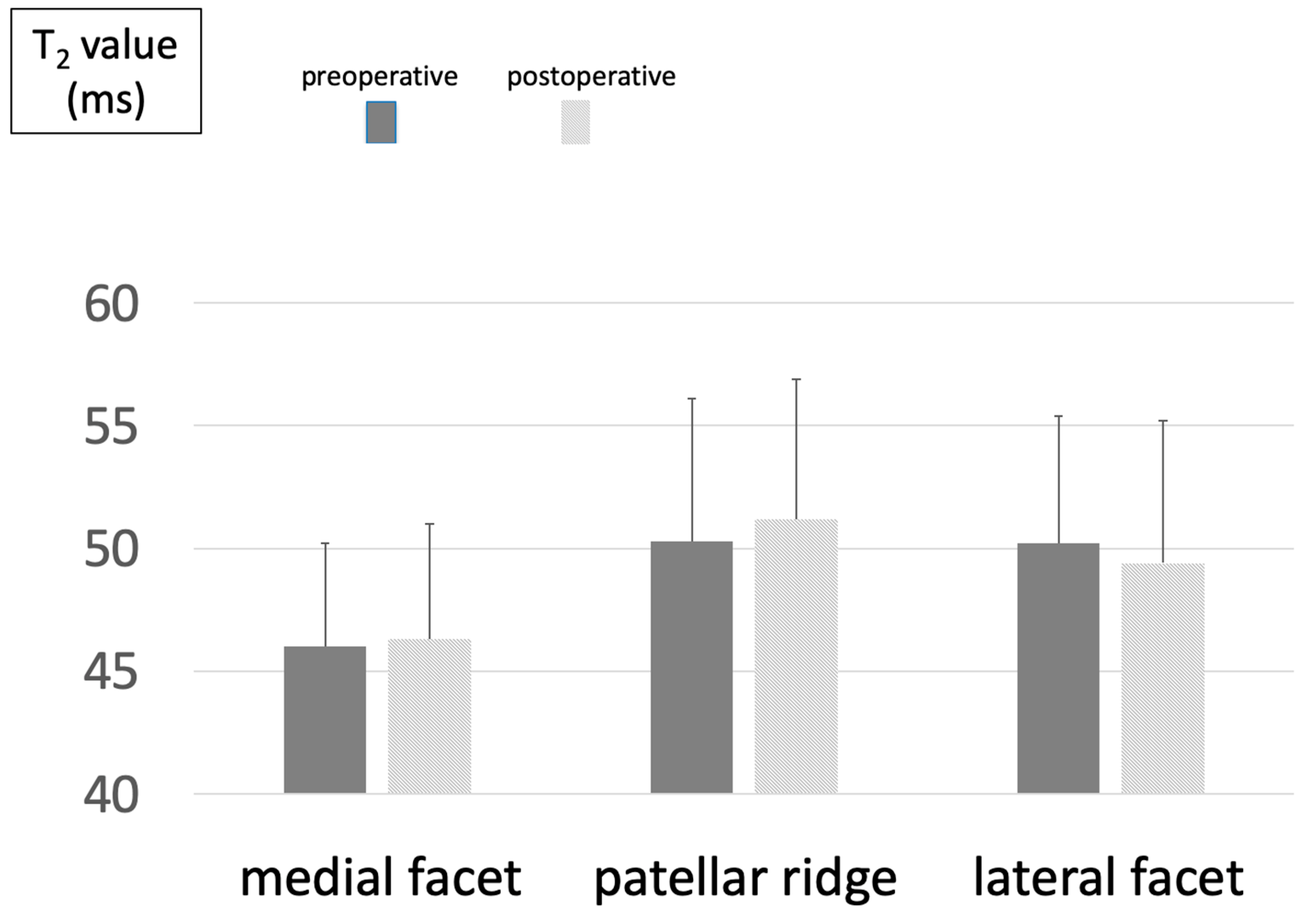
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OWHTO | Open-wedge high tibial osteotomy |
| LRR | Lateral retinacular release |
| MRI | Magnetic resonance imaging |
| KOA | Osteoarthritis of the knee |
| PF | Patellofemoral |
| MA | Mechanical axis |
| HKAA | Hip–knee–ankle angle |
| MPTA | Medial proximal tibial angle |
| PTA | Patellar tilt angle |
| SA | Sulcus angle |
| LSR | Lateral shift ratio |
| CA | Congruence angle |
| IS | Insall–Salvati |
| BP | Blackburn–Peel |
| MPTA | Medial proximal tibial angle |
| TSE | Turbo spin echo |
| TE | Multi-echo time |
| TR | Repetition time |
| FOV | Field of view |
| RFA | Radiofrequency ablation |
References
- Krakowski, P.; Rejniak, A.; Sobczyk, J.; Karpiński, R. Cartilage integrity: A review of mechanical and frictional properties and repair approaches in osteoarthritis. Healthcare 2024, 12, 1648. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.; Song, E.K.; Santoso, A.; Ingale, P.S.; Choi, I.S.; Seon, J.K. Survival and risk factor analysis of medial open wedge high tibial osteotomy for unicompartment knee osteoarthritis. Arthroscopy 2020, 36, 535–543. [Google Scholar] [CrossRef]
- Goshima, K.; Sawaguchi, T.; Shigemoto, K.; Iwai, S.; Nakanishi, A.; Inoue, D.; Shima, Y. Large opening gaps, unstable hinge fractures, and osteotomy line below the safe zone cause delayed bone healing after open-wedge high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1291–1298. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.I.; Kim, D.K.; Song, S.J.; Lee, S.H.; Bae, D.K. Medial open-wedge high tibial osteotomy may adversely affect the patellofemoral joint. Arthroscopy 2017, 33, 811–816. [Google Scholar] [CrossRef]
- Otakara, E.; Nakagawa, S.; Arai, Y.; Inoue, H.; Kan, H.; Nakayama, Y.; Fujii, Y.; Ueshima, K.; Ikoma, K.; Fujiwara, H.; et al. Large deformity correction in medial open-wedge high tibial osteotomy may cause degeneration of patellofemoral cartilage: A retrospective study. Medicine 2019, 98, e14299. [Google Scholar] [CrossRef]
- Tanaka, T.; Matsushita, T.; Miyaji, N.; Ibaraki, K.; Nishida, K.; Oka, S.; Araki, D.; Kanzaki, N.; Hoshino, Y.; Matsumoto, T.; et al. Deterioration of patellofemoral cartilage status after medial open-wedge high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1347–1354. [Google Scholar] [CrossRef] [PubMed]
- Komaki, S.; Nakagawa, S.; Arai, Y.; Inoue, A.; Kaihara, K.; Hino, M.; Kan, H.; Takahashi, K. Cartilage degeneration of patellofemoral joint occurs in open wedge high tibial osteotomy, rather than in hybrid closed wedge high tibial osteotomy, during the early postoperative period: A qualitative analysis using MRI T(2) mapping. J. Orthop. Surg. 2023, 31, 10225536221151132. [Google Scholar] [CrossRef] [PubMed]
- Lobenhoffer, P.; Agneskirchner, J.D. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2003, 11, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Farr, J. Debridement synovectomy, and lateral release. AAOS Course Lect. 2004, 382, 1–6. [Google Scholar]
- Kolowich, P.A.; Paulos, L.E.; Rosenberg, T.D.; Farnsworth, S. Lateral release of the patella: Indications and contraindications. Am. J. Sports. Med. 1990, 18, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Kato, K.; Arai, Y.; Ikoma, K.; Nakagawa, S.; Inoue, H.; Kan, H.; Matsuki, T.; Fujiwara, H.; Kubo, T. Early postoperative cartilage evaluation by magnetic resonance imaging using T2 mapping after arthroscopic partial medial meniscectomy. Magn. Reason. Imaging 2015, 33, 1274–1280. [Google Scholar] [CrossRef] [PubMed]
- Lindstrand, A.; Boegård, T.; Egund, N.; Thorngren, K.G. Use of a guide instrument for compartmental knee arthroplasty. Acta Orthop. Scand. 1982, 53, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Paley, D.; Tetsworth, K. Mechanical axis deviation of the lower limbs. Preoperative planning of uniapical angular deformities of the tibia or femur. Clin. Orthop. Relat. Res. 1992, 280, 48–64. [Google Scholar]
- Caton, J.; Deschamps, G.; Chambat, P.; Lerat, J.L.; Dejour, H. Patella infera. Apropos of 128 cases. Rev. Chir. Orthop. Réparatrice Appar. Mot. 1982, 68, 317–325. [Google Scholar] [PubMed]
- Merchant, A.C.; Mercer, R.L.; Jacobsen, R.H.; Cool, C.R. Roentgeno- graphic analysis of patella-femoral congruence. J. Bone J. Surg. 1974, 56, 1391. [Google Scholar] [CrossRef]
- Insall, J.N.; Salvati, E. Patella position in the normal knee joint. Radiology 1971, 101, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Blackburne, J.S.; Peel, T.E. A new method of measuring patellar height. J. Bone J. Surg. Br. 1977, 59, 241–242. [Google Scholar] [CrossRef] [PubMed]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Ogata, H.; Mori, M.; Jingushi, Y.; Matsuzaki, H.; Katahira, K.; Ishimatsu, A.; Enokizu-Ogawa, A.; Taguchi, K.; Moriwaki, A.; Yoshida, M. Impact of visceral fat on the prognosis of coronavirus disease 2019: An observational cohort study. BMC Infect. Dis. 2021, 21, 1240. [Google Scholar] [CrossRef] [PubMed]
- Mainil-Varlet, P.; Aigner, T.; Brittberg, M.; Bullough, P.; Hollander, A.; Hunziker, E.; Kandel, R.; Nehrer, S.; Pritzker, K.; Roberts, S.; et al. Histological assessment of cartilage repair: A report by the Histology Endpoint Committee of the International Cartilage Repair Society (ICRS). J. Bone J. Surg. Am. 2003, 85, 45–57. [Google Scholar] [CrossRef]
- Fonseca, L.P.R.M.D.; Kawatake, E.H.; Pochini, A.C. Lateral patellar retinacular release: Changes over the last ten years. Rev. Bras. Ortop. 2017, 52, 442–449. [Google Scholar] [CrossRef]
- Mosher, T.J.; Dardzinski, B.J. Cartilage MRI T2 relaxation time mapping: Overview and applications. Semin. Musculoskelet Radiol. 2004, 8, 355–368. [Google Scholar] [CrossRef] [PubMed]
- Mittal, S.; Pradhan, G.; Singh, S.; Batra, R. T1 and T2 mapping of articular cartilage and menisci in early osteoarthritis of the knee using 3-Tesla magnetic resonance imaging. Pol. J. Radiol. 2019, 84, e549–e564. [Google Scholar] [CrossRef] [PubMed]
- Goshima, K.; Sawaguchi, T.; Horii, T.; Shigemoto, K.; Iwai, S.; Hatsuchi, Y. Patellofemoral osteoarthritis progression after open-wedge high tibial osteotomy does not affect the clinical outcomes or survivorship at minimum 7 years’ Follow-Up. Arthroscopy 2024, 40, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Lüring, C.; Eschweiler, J.; Baroncini, A.; Driessen, A.; Spiezia, F.; Tingart, M.; Maffulli, N. Isolated arthroscopic lateral retinacular release for lateral patellar compression syndrome. Life 2021, 11, 295. [Google Scholar] [CrossRef]
- Aderinto, J.; Cobb, A.G. Lateral release for patellofemoral arthritis. Arthroscopy 2002, 18, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Panni, A.S.; Cerciello, S.; Vasso, M. Patellofemoral instability: Surgical treatment of soft tissues. Joints 2013, 1, 34–39. [Google Scholar] [PubMed]
- Clifton, R.; Ng, C.Y.; Nutton, R.W. What is the role of lateral retinacular release? J. Bone J. Surg. Br. 2010, 92, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Ostermeier, S.; Holst, M.; Hurschler, C.; Windhagen, H.; Stukenborg-Colsman, C. Dynamic measurement of patellofemoral kinematics and contact pressure after lateral retinacular release: An in vitro study. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 547–554. [Google Scholar] [CrossRef] [PubMed]
- Saito, T.; Takeuchi, R.; Ara, Y.; Yoshida, T.; Koshino, T. High tibial osteotomy with anterior advancement of distal fragment for medial and patellofemoral compartmental osteoarthritis of the knee. Knee 2002, 9, 127–132. [Google Scholar] [CrossRef]
- Christodoulou, N.A.; Tsaknis, R.N.; Sdrenias, C.V.; Galanis, K.G.; Mavrogenis, A.F. Improvement of proximal tibial osteotomy results by lateral retinacular release. Clin. Orthop. Relat. Res. 2005, 441, 340–345. [Google Scholar] [CrossRef]
- Li, M.; Lu, Z.; Zhang, H.; Tu, Y.; Di, Z.; Bai, J. Effect of open-wedge high tibial osteotomy and lateral patellofemoral retinacular release on patellar position: An X-ray imaging-based comparative study. Quant. Imaging Med. Surg. 2023, 13, 2860–2870. [Google Scholar] [CrossRef]
- Gaasbeek, R.; Welsing, R.; Barink, M.; Verdonschot, N.; van Kampen, A. The influence of open and closed high tibial osteotomy on dynamic patellar tracking: A biomechanical study. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 978–984. [Google Scholar] [CrossRef]
- Bito, H.; Takeuchi, R.; Kumagai, K.; Aratake, M.; Saito, I.; Hayashi, R.; Sasaki, Y.; Saito, T. Opening wedge high tibial osteotomy affects both the lateral patellar tilt and patellar height. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 955–960. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Lee, S.B.; Oh, W.S.; Kwon, Y.E.; Lee, B.K. Changes in patellofemoral alignment do not cause clinical impact after open-wedge high tibial osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Murayama, K.; Nakayama, H.; Murakami, T.; Yoshiya, S.; Otsuki, S.; Tachibana, T. The effect of concomitant arthroscopic lateral retinacular release on postoperative patellar position and orientation in open wedge high tibial osteotomy. Knee Surg. Relat. Res. 2018, 30, 241–246. [Google Scholar] [CrossRef] [PubMed]
| OWHTO Group | OWHTO + RL Group | p-Value | |
|---|---|---|---|
| gender (male/female) | 14/23 | 9/28 | 0.32 |
| age at surgery, mean ± SD (years) | 59.5 ± 10.5 | 59.3 ± 9.4 | 0.95 |
| height (cm) | 163.0 ± 8.5 | 162.5 ± 5.7 | 0.76 |
| weight (kg) | 64.8 ± 10.7 | 64.9 ± 13.5 | 0.98 |
| body mass index (kg/m2) | 24.3 ± 2.7 | 24.5 ± 4.4 | 0.84 |
| preoperative KOOS | |||
| ADL | 74.0 ± 16.5 | 77.6 ± 17.0 | 0.35 |
| pain | 60.9 ± 15.1 | 64.1 ± 20.7 | 0.45 |
| QOL | 38.3 ± 17.7 | 42.2 ± 20.2 | 0.38 |
| sports | 44.1 ± 23.0 | 52.0 ± 25.0 | 0.16 |
| symptom | 64.4 ± 17.6 | 70.7 ± 17.0 | 0.12 |
| postoperative KOOS | |||
| ADL | 90.7 ± 9.8 | 91.4 ± 11.6 | 0.80 |
| pain | 82.6 ± 13.4 | 84.8 ± 15.2 | 0.55 |
| QOL | 69.7 ± 21.1 | 71.8 ± 22.6 | 0.70 |
| sports | 70.8 ± 21.4 | 71.3 ± 22.5 | 0.93 |
| symptom | 82.8 ± 12.7 | 86.1 ± 14.1 | 0.32 |
| opening width (mm) | 8.3 ± 2.2 | 8.2 ± 2.1 | 0.82 |
| OWHTO Group | OWHTO + RL Group | |||||
|---|---|---|---|---|---|---|
| Pre | Post | p Value | Pre | Post | p Value | |
| HKA angle (°) | −5.0 ± 2.6 | 3.4 ± 1.6 | <0.001 * | −4.3 ± 2.0 | 4.0 ± 1.6 | <0.001 * |
| MPTA (°) | 84.1 ± 1.8 | 91.6 ± 2.0 | <0.001 * | 84.6 ± 2.4 | 92.3 ± 2.6 | <0.001 * |
| IS ratio | 1.11 ± 0.13 | 1.11 ± 0.14 | 0.53 | 1.15 ± 0.17 | 1.15 ± 0.17 | 0.95 |
| BP ratio | 0.85 ± 0.08 | 0.71 ± 0.10 | <0.001 * | 0.88 ± 0.11 | 0.75 ± 0.10 | <0.001 * |
| tilting angle (°) | 8.6 ± 3.7 | 5.7 ± 3.6 | <0.001 * | 7.9 ± 3.6 | 6.9 ± 4.2 | 0.02 * |
| lateral shift ratio | 12.6 ± 4.8 | 11.0 ± 5.5 | 0.07 | 12.5 ± 5.2 | 12.1 ± 6.0 | 0.69 |
| congruence angle (°) | −5.8 ± 10.6 | −6.3 ± 10.4 | 0.55 | −7.2 ± 9.1 | −7.4 ± 7.5 | 0.85 |
| OWHTO Group | OWHTO + RL Group | p-Value | |
|---|---|---|---|
| ΔHKA (°) | 8.4 ± 2.2 | 8.3 ± 2.1 | 0.85 |
| ΔMPTA (°) | 7.6 ± 2.2 | 7.7 ± 1.9 | 0.77 |
| ΔIS ratio | 0.0 ± 0.1 | 0.0 ± 0.1 | 0.63 |
| ΔBP ratio | −0.15 ± 0.11 | −0.13 ± 0.10 | 0.43 |
| Δtilting angle | −2.9 ± 2.1 | −1.0 ± 2.6 | <0.01 * |
| Δlateral shift ratio | −1.7 ± 5.4 | −0.3 ± 5.1 | 0.28 |
| Δcongruence angle | −0.5 ± 5.5 | −0.2 ± 5.3 | 0.76 |
| OWHTO Group | OWHTO + RL Group | p-Value | ||
|---|---|---|---|---|
| ICRS grade (0/1/2/3/4) | ||||
| patella | pre | 2/22/10/3/0 | 0/25/12/0/0 | 0.15 |
| post | 1/21/12/2/1 | 0/24/13/0/0 | 0.37 | |
| femur | pre | 0/17/15/5/0 | 0/10/23/4/0 | 0.16 |
| post | 0/12/16/9/0 | 0/13/21/3/0 | 0.16 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakagawa, S.; Kan, H.; Arai, Y.; Komaki, S.; Hino, M.; Inoue, A.; Takahashi, K. Effect of Open-Wedge High Tibial Osteotomy and Lateral Retinacular Release on the Articular Cartilage of the Patellofemoral Joint: Analysis Using Magnetic Resonance Imaging T2 Mapping. J. Clin. Med. 2025, 14, 595. https://doi.org/10.3390/jcm14020595
Nakagawa S, Kan H, Arai Y, Komaki S, Hino M, Inoue A, Takahashi K. Effect of Open-Wedge High Tibial Osteotomy and Lateral Retinacular Release on the Articular Cartilage of the Patellofemoral Joint: Analysis Using Magnetic Resonance Imaging T2 Mapping. Journal of Clinical Medicine. 2025; 14(2):595. https://doi.org/10.3390/jcm14020595
Chicago/Turabian StyleNakagawa, Shuji, Hiroyuki Kan, Yuji Arai, Shintaro Komaki, Manabu Hino, Atsuo Inoue, and Kenji Takahashi. 2025. "Effect of Open-Wedge High Tibial Osteotomy and Lateral Retinacular Release on the Articular Cartilage of the Patellofemoral Joint: Analysis Using Magnetic Resonance Imaging T2 Mapping" Journal of Clinical Medicine 14, no. 2: 595. https://doi.org/10.3390/jcm14020595
APA StyleNakagawa, S., Kan, H., Arai, Y., Komaki, S., Hino, M., Inoue, A., & Takahashi, K. (2025). Effect of Open-Wedge High Tibial Osteotomy and Lateral Retinacular Release on the Articular Cartilage of the Patellofemoral Joint: Analysis Using Magnetic Resonance Imaging T2 Mapping. Journal of Clinical Medicine, 14(2), 595. https://doi.org/10.3390/jcm14020595






