Own Typology of Body Posture Based on Research Using the Diers Formetric III 4D System
Abstract
1. Introduction
2. Materials and Methods
2.1. Examination of Body Posture Using Diers Formetric III 4D Method
- The inflexion point ICT (mm), which is the cervical-thoracic inflexion point, i.e., the point of the highest surface inclination in the cervical spine (above the kyphotic apex),
- The kyphotic apex KA (VPDM) (mm), which is the posterior apex of the sagittal profile in the thoracic spine,
- The inflexion point ITL (mm), which is the thoracolumbar inflexion point, i.e., the point of the highest negative surface inclination in the area between the kyphotic and lordotic apexes,
- The lordotic apex LA (VPDM) (mm), which is the anterior apex of the sagittal profile in the lumbar spine (Figure 2),
- The inflexion point ILS (mm), which is the lumbar-sacral inflexion point, i.e., the point of the highest positive slope of the surface between the lordotic apex and sacral kyphosis,
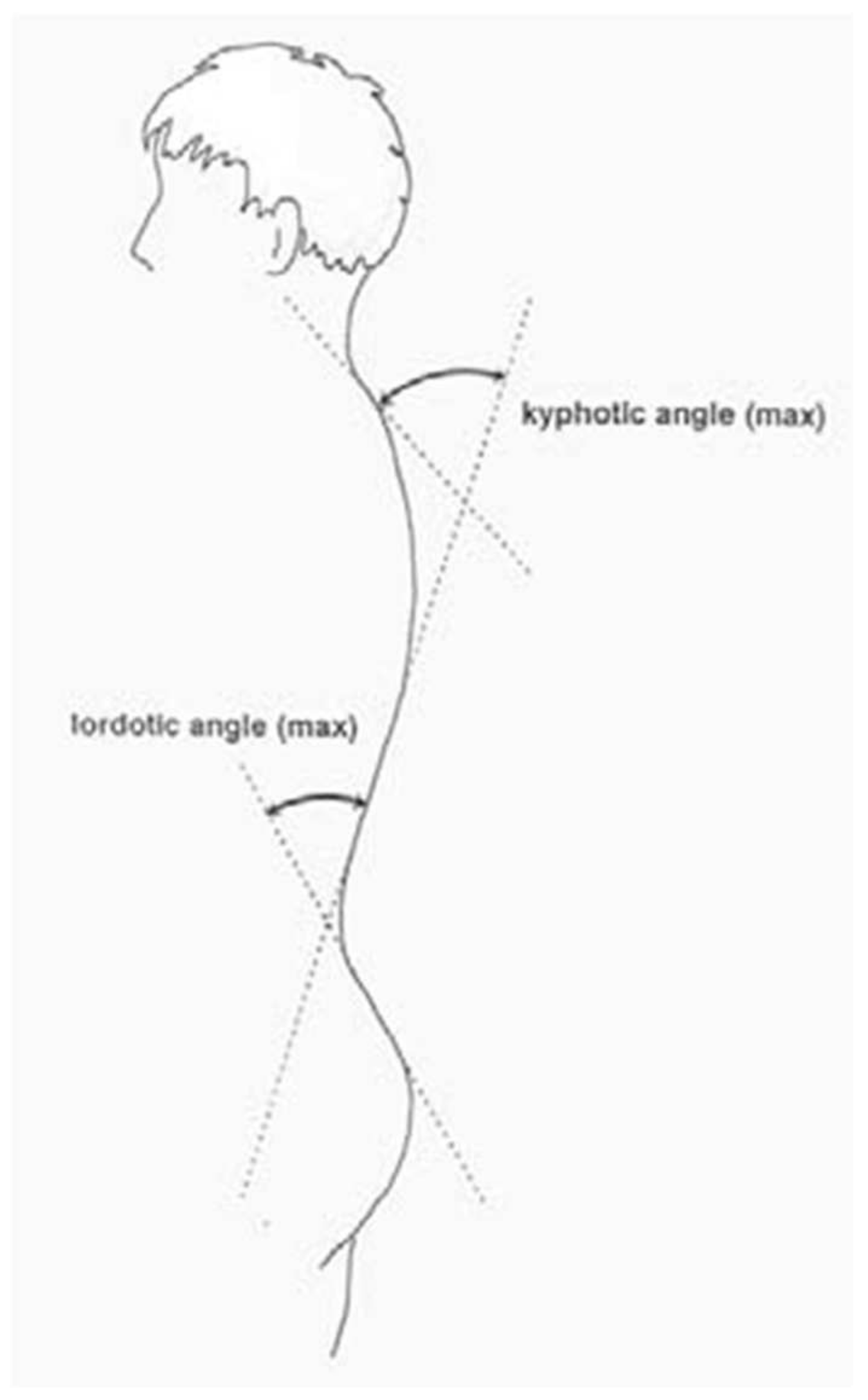
- The kyphotic angle ICT-ITL (max) (°), which is the maximum angle of kyphosis, measured between the tangents to the surface of the upper inflexion point ICT near VP and the thoracolumbar inflexion point ITL,
- The kyphotic angle VP-ITL (°) is the kyphosis angle measured between VP and the thoracolumbar inflexion point ITL,
- The lordotic angle ICT-ITL (max), which is the maximum lordosis angle measured between the tangents to the surface of the thoracolumbar inflexion point ITL and the lower lumbar-sacral inflexion point ILS,
- The lordotic angle ITL-DM (°), which is the angle of lordosis measured between the tangents to the surface of the lumbar-sacral inflexion point ITL and DM (Figure 3). The reliability of body posture and spinal analysis using the Diers Formetric III 4D was confirmed by comparison with digital and numerically analysed X-ray images. The results of body posture measurement were based on the standards created by Harzman [40]. The values of 42° ≤ K ≤ 55°; 33° ≤ L ≤ 47° [41] were adopted as the standard for the angles of thoracic kyphosis and lumbar lordosis.
2.2. Methods of Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Wilczyński, J. Electromyographic activity of the erector spinae and convexity as well as concavity of spinal curvature in children. Children 2021, 8, 1168. [Google Scholar] [CrossRef] [PubMed]
- Puszczałowska-Lizis, E.; Lizis, P. Assessment of body posture of school youth from urban environment. Med. Rev. Univ. Rzesz. 2007, 2, 147–155. [Google Scholar]
- Nowotny, J.; Podlasiak, P.; Zawieska, D. Posture Defect Analysis System; PW: Warsaw, Poland, 2003. [Google Scholar]
- Schulte, T.L.; Hierholzer, E.; Boerke, A.; Lerner, T.; Liljenqvist, U.; Bullmann, V.; Hackenberg, L. Raster stereography versus radiography in the long-term follow-up of idiopathic scoliosis. J. Spinal Disord. Tech. 2008, 21, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Arndt, C.; Berkhoff, G.; Schräder, C. Videorasterstereographische Untersuchungen vor und nach Atlasimpulstherapie [Videoraster Stereographic Examinations Before and After Atlas Impulse Therapy]. Man. Med. 2002, 40, 220–223. (In German) [Google Scholar] [CrossRef]
- Drerup, B. Improvements in measuring vertebral rotation from the projection of the pradicles. J. Appl. Biomech. 1985, 18, 369–378. [Google Scholar] [CrossRef]
- Drerup, B.; Hierholzer, E. Automatic localization of anatomical landmarks on the back surface and construction of a body-fixed coordinate system. J. Appl. Biomech. 1987, 20, 961–970. [Google Scholar] [CrossRef]
- Drerup, B.; Hierholzer, E. Movement of the human pelvis and displacement of related anatomical landmarks on the body surface. J. Appl. Biomech. 1987, 20, 971–997. [Google Scholar] [CrossRef]
- Drerup, B.; Ellger, B.; Meyer zu Bentrup, F.M.; Hierholzer, E. Functional rasterstereographic images. A new method for biomechanical analysis of skeletal geometry. Orthopäde 2001, 30, 242–250. [Google Scholar] [CrossRef]
- Drerup, B.; Hierholzer, E. Evaluation of frontal radiographs of scoliotic spines—Part I Measurement of position and orientation of vertebra and assessment of clinical shape parameters. J. Biomech. 1992, 25, 1357–1362. [Google Scholar] [CrossRef]
- Drerup, B.; Hierholzer, E. Evaluation of frontal radiographs of scoliotic spines—Part II. Relations between lateral deviation, lateral tilt and axial rotation of vertebrae. J. Appl. Biomech. 1992, 25, 1443–1450. [Google Scholar] [CrossRef]
- Drerup, B.; Hierholzer, E.; Ellger, B. Shape analysis of lateral and frontal projection of spine curves assessed from rasterstereographs. In Research into Spinal Deformities 1; Sevastic, J., Diab, K., Eds.; IOS Press: Amsterdam, The Netherlands, 1997; Volume 37, pp. 271–275. [Google Scholar]
- Frerich, J.; Hertzler, K.; Knott, P.; Mardjetko, S. Comparison of Radiographic and Surface Topography Measurements in Adolescents with Idiopathic Scoliosis. Open Orthop. J. 2012, 27, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Frobin, W.; Hierholzer, E. Analysis of human back shape using surfaces curvatures. J. Appl. Biomech. 1982, 14, 379–390. [Google Scholar] [CrossRef] [PubMed]
- Frobin, W.; Hierholzer, E. Automatic measurement of body surfaces using rasterstereography. Part I: Image scan and control point measurement. Photogramm. Eng. Remote Sens. 1983, 49, 377–384. [Google Scholar]
- Frobin, W.; Hierholzer, E. Automatic measurement of body surfaces using rasterstereography. Part II: Analysis of the rasterstereographic line pattern and 3-D surface reconstruction. Photogramm. Eng. Remote Sens. 1983, 49, 1443–1452. [Google Scholar]
- Frobin, W.; Hierholzer, E. Calibration and model reconstruction in analytical close-range stereophotogrammetry. Part I: Mathematical fundamentals. Photogramm. Eng. Remote Sens. 1982, 48, 67–72. [Google Scholar]
- Frobin, W.; Hierholzer, E. Calibration and model reconstruction in analytical close-range stereophotogrammetry. Part II: Special evaluation procedures for rasterstereography and moiré topography. Photogramm. Eng. Remote Sens. 1982, 48, 215–220. [Google Scholar]
- Frobin, W.; Hierholzer, E. Rasterstereography: A photographic method for measurement of body surfaces. Photogramm. Eng. Remote Sens. 1981, 47, 1717–1724. [Google Scholar]
- Frobin, W.; Hierholzer, E. Video rasterstereography: A method for on-line measurement of body surfaces. Photogramm. Eng. Remote Sens. 1991, 57, 1341–1345. [Google Scholar]
- Furian, T.C.; Rapp, W.; Eckert, S.; Wild, M.; Betsch, M. Spinal posture and pelvic position. Orthop. Rev. 2013, 5, 29–33. [Google Scholar]
- Goh, S.; Price, R.I.; Leedman, P.J.; Singer, K.P. Rasterstereographic Analysis of the thoracic sagittal curvature. J. Musculoskelet. Res. 1999, 3, 137–142. [Google Scholar] [CrossRef]
- Hackenberg, L. Stellenwert der Rückenformanalyse in der Therapie von Wirbelsäulendeformitäten [Significance of Back Shape Analysis in the Treatment of Spinal Deformities]. In Habilitation; Klinik und Poliklinik für Allgemeine Orthopädie, Westfälische Wilhelms-Universität Münster: Münster, Germany, 2003. (In German) [Google Scholar]
- Hackenberg, L. Valuation of body surface measurements: Accuracy rating of anatomical landmarks. In Research into Spinal Deformities; Stokes, I., Ed.; IOS Press: Amsterdam, The Netherlands, 1999; Volume 59, pp. 25–28. [Google Scholar]
- Hackenberg, L.; Hierholzer, E. 3-D back surface analysis of severe idiopathic scoliosis by rasterstereography: Comparison of rasterstereographic and digitised radiometric data. In Research into Spinal Deformities; Tanguy, A., Peuchot, B., Eds.; IOS Press: Amsterdam, The Netherlands, 2002; Volume 88, pp. 86–89. [Google Scholar]
- Hackenberg, L.; Hierholzer, E.; Bullmann, V.; Liljenqvist, U.; Götze, C. Rasterstereographic analysis of axial back surface rotation in standing versus forward bending posture in idiopathic scoliosis. Eur. Spine J. 2006, 15, 1144–1149. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hackenberg, L.; Hierholzer, E.; Liljenqvist, U. Accuracy of rasterstereography versus radiography in idiopathic scoliosis after anterior correction and fusion. In Research into Spinal Deformities; Grivas, B., Ed.; IOS Press: Amsterdam, The Netherlands, 2002; Volume 91, pp. 241–245. [Google Scholar]
- Hackenberg, L.; Hierholzer, E.; Pötzl, W.; Götze, C.; Liljenqvist, U. Rasterstereographic back shape analysis in idiopathic scoliosis after posterior correction and fusion. Clin. Biomech. 2003, 19, 883–889. [Google Scholar] [CrossRef] [PubMed]
- Hackenberg, L.; Liljenqvist, U.; Hierholzer, E.; Halm, H. Rasterstereografische Oberflächenvermessung idiopathischer Skoliosen nach VDS [Raster Stereographic Surface Measurement of Idiopathic Scoliosis According to VDS]. Orthopädie 2000, 138, 353–359. [Google Scholar]
- Hanfy, H.; Awad, M.; Hamid, A.; Allah, A. Effect of Exercise on Postural Kyphosis. Indian J. Physiother. Occup. Ther. 2012, 6, 190–195. (In German) [Google Scholar]
- Hierholzer, E. Is it possible to use surface topography in operation planning and therapy control. In Research into Spinal Deformities; Sevastic, J., Diab, K., Eds.; IOS Press: Amsterdam, The Netherlands, 1997; Volume 37, pp. 493–496. [Google Scholar]
- Hierholzer, E. Objektive Analyse der Rückenform von Skoliosepatienten; Gustav Fischer Verlag: Stuttgart, Germany; New York, NY, USA, 1993. (In German) [Google Scholar]
- Hierholzer, E.; Drerup, B. First Experiences with Clinical Applications of Video Rasterstereography; Surface Topography and Spinal Deformity: New York, NY, USA, 1992. [Google Scholar]
- Hierholzer, E.; Drerup, B.; zu Bentrup, F.M. Influence of length discrepancy on rasterstereographic back shape parameters. In Research into Spinal Deformities 1; IOS Press: Amsterdam, The Netherlands, 1997; Volume 37, pp. 265–269. [Google Scholar]
- Huysmans, T.; Haex, B.; Van Audekercke, R.; Vander Sloten, J.; Van der Perre, G. Three-dimensional mathematical reconstruction of spinal shape, based on active contours. J. Appl. Biomech. 2004, 37, 1793–1798. [Google Scholar] [CrossRef]
- Knott, P. A comparison of automatic vs. manual detection of anatomical landmarks during surface topography evaluation using the formetric 4D system. Open Orthop. J. 2012, 7, O19. [Google Scholar]
- Drerup, B.; Hierholzer, E. Back shape measurement using video rasterstereography and three-dimensional reconstruction of spinal shape. Clin. Biomech. 1994, 9, 28–36. [Google Scholar] [CrossRef]
- Liljenqvist, U.; Halm, H.; Hierholzer, E.; Drerup, B.; Weiland, M. 3-dimensional surface measurement of spinal deformities with video rasterstereography. Z. Orthop. Ihre Grenzgeb. 1998, 136, 57–64. [Google Scholar] [CrossRef]
- Lippold, C.; Danesh, G.; Schilgen, M.; Drerup, B.; Hackenberg, L. Relationship betrween Thoracic, Lordotic, and Pelvic Inclination and Craniofacial Morphology in Adults. Angle Orthod. 2006, 76, 779–785. [Google Scholar]
- Harzmann, H.C. Optischer Gipsabdruck hilft bei der Rückenanalyse. Süddeutscher Orthopädenkongress [Optical Plaster Cast Aids Back Analysis]. Kongressausgabe 1999, 2, 15. (In German) [Google Scholar]
- Harzmann, H. Methode und Klinische Einsatzmöglichkeiten der dreidimensionalen Rückenoberflächenvermessung mit der Videorasterstereographie (VRS). In Individuelle Gesundheitsleistungen (IGEL) in der Orthopädie; Leithoff, P., Sadler, B., Eds.; Georg Thieme Verlag: Stuttgart, Germany, 2001; pp. 81–104. (In German) [Google Scholar]
- Domagalska, M.E. Neurophysiological Aspects of Diagnosis and Therapy in Posture Deviations; WSA: Bielsko Biała, Poland, 2009; pp. 25–56. [Google Scholar]
- Czaprowski, D.; Stoliński, Ł.; Tyrakowski, M.; Kozinoga, M.; Kotwicki, T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Radczuk, M.; Kasprzak, J. Radiation doses received by children during radiographs. Probl. Hig. Epidemiol. 2014, 95, 956–963. [Google Scholar]
- Betsch, M.; Wild, M.; Jungbluth, P.; Hakimi, M.; Windolf, J.; Haex, B.; Horstmann, T.; Rapp, W. Reliability and validity of 4D rasterstereography under dynamic condition. Comput. Biol. Med. 2011, 41, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Zmyślna, A.; Żurawski, A.Ł.; Śliwiński, G.; Śliwiński, Z.W.; Kiebzak, W.P. Assessment of Body Posture of Children With Chest Pain. Front. Pediatr. 2021, 9, 704087. [Google Scholar] [CrossRef] [PubMed]
- Weigel, S.; Dullien, S.; Grifka, J.; Jansen, P. Comparison between rasterstereographic scan and orthopedic examination for posture assessment: An observational study. Front. Surg. 2024, 11, 1461569. [Google Scholar] [CrossRef]
- Żurawski, A.; Śliwiński, Z.; Suliga, E.; Śliwiński, G.; Wypych, Ż.; Kiebzak, W. Effect of Thoracic Kyphosis and Lumbar Lordosis on the Distribution of Ground Reaction Forces on the Feet. Orthop. Res. Rev. 2022, 14, 187–197. [Google Scholar] [CrossRef]
- Zmyślna, A.; Kiebzak, W.; Żurawski, A.; Pogorzelska, J.; Kotela, I.; Kowalski, T.J.; Śliwiński, Z.; Śliwiński, G. Effect of physiotherapy on spinal alignment in children with postural defects. Int. J. Occup. Med. Environ. Health 2019, 32, 25–32. [Google Scholar] [CrossRef]
- Jorgić, B.M.; Đorđević, S.N.; Hadžović, M.M.; Milenković, S.; Stojiljković, N.; Olanescu, M.; Peris, M.; Suciu, A.; Popa, D.; Plesa, A. The Influence of Body Composition on Sagittal Plane Posture among Elementary School-Aged Children. Children 2023, 11, 36. [Google Scholar] [CrossRef]
- Turner-Smith, A.R.; Harris, J.; Houghton, G.R.; Jefferson, R.J. A method for analysis of back shape in scoliosis. J. Appl. Biomech. 1988, 21, 497–509. [Google Scholar] [CrossRef]


| Sex | Age | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| 10 Years | 11 Years | 12 Years | ||||||
| N | % | N | % | N | % | N | % | |
| Girls | 66 | 49.24 | 47 | 43.93 | 30 | 48.39 | 143 | 47.18 |
| Boys | 67 | 50.76 | 61 | 56.07 | 32 | 51.61 | 160 | 52.82 |
| Total | 133 | 43.85 | 108 | 35.55 | 62 | 20.60 | 303 | 100 |
| χ2 = 0.716; df = 2; p = 0.698 | ||||||||
| Body Posture Variables | N | X | SD | Me | Min | Max | Confidence −95.00% | Confidence +95.00% |
|---|---|---|---|---|---|---|---|---|
| Inflexion point ICT (mm) | 303 | −0.149 | 9.955 | 1.98 | −19.99 | 21.62 | −1.279 | 0.980 |
| Kyphotic apex KA (VPDM) (mm) | 303 | −131.570 | 27.833 | −132.89 | −203.67 | −36.64 | −134.727 | −128.413 |
| Inflexion point ITL (mm) | 303 | −233.089 | 37.653 | −226.86 | −353.42 | −156.8 | −237.359 | −228.818 |
| Lordosis apex LA (VPDM) (mm) | 303 | −307.206 | 33.359 | −305.91 | −425.17 | −212.63 | −310.989 | −303.422 |
| Inflexion point ILS (mm) | 303 | −372.207 | 32.472 | −371.06 | −502.49 | −295.26 | −375.890 | −368.524 |
| Kyphosis angle ICT-ITL (max) (°) | 303 | 43.348 | 9.406 | 43.71 | 17.54 | 70.05 | 42.281 | 44.415 |
| Kyphosis angle VP-ITL (°) | 303 | 40.316 | 9.751 | 40.93 | 11.48 | 64.22 | 39.210 | 41.422 |
| Lordosis angle ITL-ITS (max) (°) | 303 | 40.263 | 9.321 | 40.31 | 9.44 | 66.57 | 39.205 | 41.320 |
| Lordosis angle ITL-DM (°) | 303 | 36.654 | 9.163 | 36.67 | 7.55 | 63.21 | 35.614 | 37.693 |
| Body Posture Variables | N | X | SD | Me | Min | Max | Confidence −95.00% | Confidence +95.00% |
|---|---|---|---|---|---|---|---|---|
| Inflexion point ICT (mm) | 143 | 1.562 | 9.922 | 4.195 | −19.78 | 21.62 | −0.084 | 33.208 |
| Kyphotic apex KA (VPDM) (mm) | 143 | −126.348 | 30.352 | −127.585 | −202.94 | −36.64 | −131.383 | −121.313 |
| Inflexion point ITL (mm) | 143 | −228.560 | 37.802 | −221.535 | −353.42 | −156.8 | −234.832 | −222.289 |
| Lordotic apex LA (VPDM) (mm) | 143 | −304.258 | 34.162 | −302.315 | −394.33 | −217.67 | −309.925 | −298.590 |
| Inflexion point ILS (mm) | 143 | −371.211 | 33.523 | −370.07 | −454.31 | −295.26 | −376.773 | −365.650 |
| Kyphosis angle ICT-ITL (max) (°) | 143 | 41.781 | 9.210 | 41.17 | 17.54 | 60.82 | 40.253 | 43.309 |
| Kyphosis angle VP-ITL (°) | 143 | 38.757 | 9.332 | 38.34 | 15.59 | 58.04 | 37.209 | 40.306 |
| Lordosis angle ITL-ITS (max) (°) | 143 | 41.870 | 9.177 | 41.635 | 21.57 | 66.57 | 40.347 | 43.392 |
| Lordosis angle ITL-DM (°) | 143 | 38.145 | 9.032 | 38.405 | 11.72 | 63.21 | 35.614 | 37.693 |
| Body Posture Variables | N | X | SD | Me | Min | Max | Confidence −95.00% | Confidence +95.00% |
|---|---|---|---|---|---|---|---|---|
| Inflexion point ICT (mm) | 160 | −1.678 | 9.764 | 0.9 | −19.99 | 16.76 | −3.208 | −0.149 |
| Kyphotic apex KA (VPDM) (mm) | 160 | −136.233 | 24.543 | −136.13 | −203.67 | −42.77 | −140.078 | −132.389 |
| Inflexion point ITL (mm) | 160 | −237.133 | 37.172 | −233.1 | −340.19 | −161.12 | −242.955 | −231.310 |
| Lordotic apex LA (VPDM) (mm) | 160 | −309.838 | 32.506 | −308.21 | −425.17 | −212.63 | −314.930 | −304.747 |
| Inflexion point ILS (mm) | 160 | −373.096 | 31.583 | −371.09 | −502.49 | −306.41 | −378.044 | −368.149 |
| Kyphosis angle ICT-ITL (max) (°) | 160 | 44.748 | 9.388 | 44.98 | 20.98 | 70.05 | 43.278 | 46.219 |
| Kyphosis angle VP-ITL (°) | 160 | 41.708 | 9.935 | 42.82 | 11.48 | 64.22 | 40.152 | 43.265 |
| Lordosis angle ITL-ITS (max) (°) | 160 | 38.827 | 9.241 | 39.17 | 9.44 | 60.66 | 37.380 | 40.275 |
| Lordosis angle ITL-DM (°) | 160 | 35.322 | 9.102 | 34.87 | 7.55 | 56.21 | 33.896 | 36.748 |
| Body Posture Variables | X Girls | X Boys | Student’s t | df | p | N Girls | N Boys | SD Girls | SD Boys | F Quotient of Variance | p of Variance | Cohen’s d |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Inflexion point ICT (mm) | 1.562 | −1.678 | 2.852 | 301 | 0.00464 | 143 | 160 | 9.922 | 9.764 | 1.033 | 0.84257 | 0.0114 |
| Kyphotic apex KA (VPDM) (mm) | −126.348 | −136.233 | 3.120 | 301 | 0.00198 | 143 | 160 | 30.352 | 24.543 | 1.529 | 0.00952 | 0.1499 |
| Inflexion point ITL (mm) | −228.560 | −237.133 | 1.981 | 301 | 0.04847 | 143 | 160 | 37.802 | 37.172 | 1.034 | 0.83535 | 0.01195 |
| Lordosis apex LA (VPDM) (mm) | −304.258 | −309.838 | 1.452 | 301 | 0.14766 | 143 | 160 | 34.162 | 32.506 | 1.104 | 0.54248 | 0.0350 |
| Inflexion point ILS (mm) | −371.211 | −373.096 | 0.502 | 301 | 0.61587 | 143 | 160 | 33.523 | 31.583 | 1.127 | 0.46539 | 0.04199 |
| Kyphosis angle ICT-ITL (max) (°) | 41.781 | 44.748 | −2.762 | 301 | 0.00610 | 143 | 160 | 9.210 | 9.388 | 1.039 | 0.81778 | 0.0132 |
| Kyphosis angle VP-ITL (°) | 38.757 | 41.708 | −2.647 | 301 | 0.00855 | 143 | 160 | 9.332 | 9.935 | 1.133 | 0.44823 | 0.0436 |
| Lordosis angle ITL-ITS (max) (°) | 41.870 | 38.827 | 2.861 | 301 | 0.00453 | 143 | 160 | 9.177 | 9.241 | 1.014 | 0.93518 | 0.0046 |
| Lordosis angle ITL-DM (°) | 38.145 | 35.322 | 2.696 | 301 | 0.00742 | 143 | 160 | 9.032 | 9.102 | 1.016 | 0.92698 | 0.00527 |
| No. | Variable | Thoracic Kyphosis Angle | Lumbar Lordosis Angle | Kyphosis and Lordosis Angles |
|---|---|---|---|---|
| 1 | Reduced kyphosis, reduced lordosis | <42° | <33° | K < 42°; L < 33° |
| 2 | Reduced kyphosis, normal lordosis | <42° | 33–47° | K < 42°; 33° ≤ L ≤ 47° |
| 3 | Reduced kyphosis, Increased lordosis | <42° | >47° | K < 42°; L > 47° |
| 4 | Normal kyphosis, reduced lordosis | 42–55° | <33° | 42° ≤ K ≤ 55°; L < 33° |
| 5 | Normal kyphosis, normal lordosis | 42–55° | 33–47° | 42° ≤ K ≤ 55°; 33° ≤ L ≤ 47° |
| 6 | Normal kyphosis, increased lordosis | 42–55° | >47° | 42° ≤ K ≤ 55°; L > 47° |
| 7 | Increased kyphosis, reduced lordosis | >55° | <33° | K > 55°; L < 33° |
| 8 | Increased kyphosis, normal lordosis | >55° | 33–47° | K > 55°; 33° ≤ L ≤ 47° |
| 9 | Increased kyphosis, increased lordosis | >55° | >47° | K > 55°; L > 47° |
| Variable | Girls | Boys | Total | Structure p-Index Test | Cohen’s d | |||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |||
| Reduced kyphosis, reduced lordosis | 22 | 15.49 | 26 | 16.35 | 48 | 15.95 | 0.83893 | 0.01168 |
| Reduced kyphosis, normal lordosis | 41 | 28.87 | 26 | 16.35 | 67 | 22.26 | 0.00914 | 0.1507 |
| Reduced kyphosis, increased lordosis | 12 | 8.45 | 2 | 1.26 | 14 | 4.65 | 0.00309 | 0.17135 |
| Normal kyphosis, reduced lordosis | 1 | 0.7 | 16 | 10.06 | 17 | 5.65 | 0.00045 | 0.2038 |
| Posture with normal physiological curvatures of spine | 36 | 25.35 | 51 | 32.08 | 87 | 28.9 | 0.19896 | 0.07395 |
| Normal kyphosis, increased lordosis | 18 | 12.68 | 17 | 10.69 | 35 | 11.63 | 0.59189 | 0.03083 |
| Increased kyphosis, reduced lordosis | 1 | 0.7 | 1 | 1.60 | 2 | 0.66 | 0.87637 | 0.00894 |
| Increased kyphosis, normal lordosis | 2 | 1.41 | 10 | 6.29 | 12 | 3.99 | 0.03072 | 0.12471 |
| Increased kyphosis, increased lordosis | 10 | 7.04 | 11 | 6.92 | 21 | 6.98 | 0.96637 | 0.0024 |
| Total | 143 | 47.18 | 160 | 52.82 | 303 | 100 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilczyński, J. Own Typology of Body Posture Based on Research Using the Diers Formetric III 4D System. J. Clin. Med. 2025, 14, 501. https://doi.org/10.3390/jcm14020501
Wilczyński J. Own Typology of Body Posture Based on Research Using the Diers Formetric III 4D System. Journal of Clinical Medicine. 2025; 14(2):501. https://doi.org/10.3390/jcm14020501
Chicago/Turabian StyleWilczyński, Jacek. 2025. "Own Typology of Body Posture Based on Research Using the Diers Formetric III 4D System" Journal of Clinical Medicine 14, no. 2: 501. https://doi.org/10.3390/jcm14020501
APA StyleWilczyński, J. (2025). Own Typology of Body Posture Based on Research Using the Diers Formetric III 4D System. Journal of Clinical Medicine, 14(2), 501. https://doi.org/10.3390/jcm14020501






