Impact of Obesity on Hospitalization Burden of Urolithiasis in Spain Between 1997 and 2021
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
3.1. Demographic and Basal Characteristics
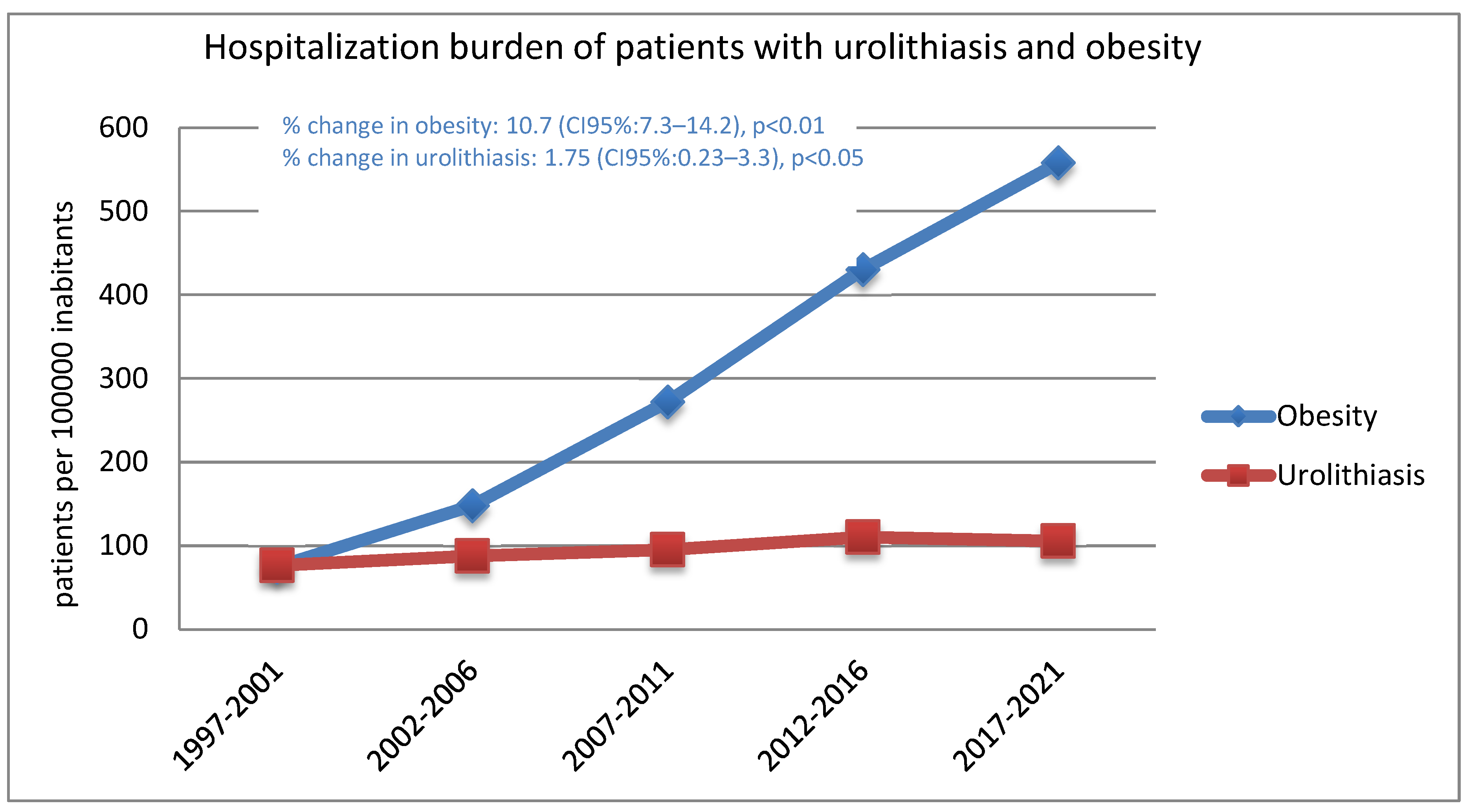
3.2. Trends of Lithiasis and Obesity in Spanish Hospitalizations
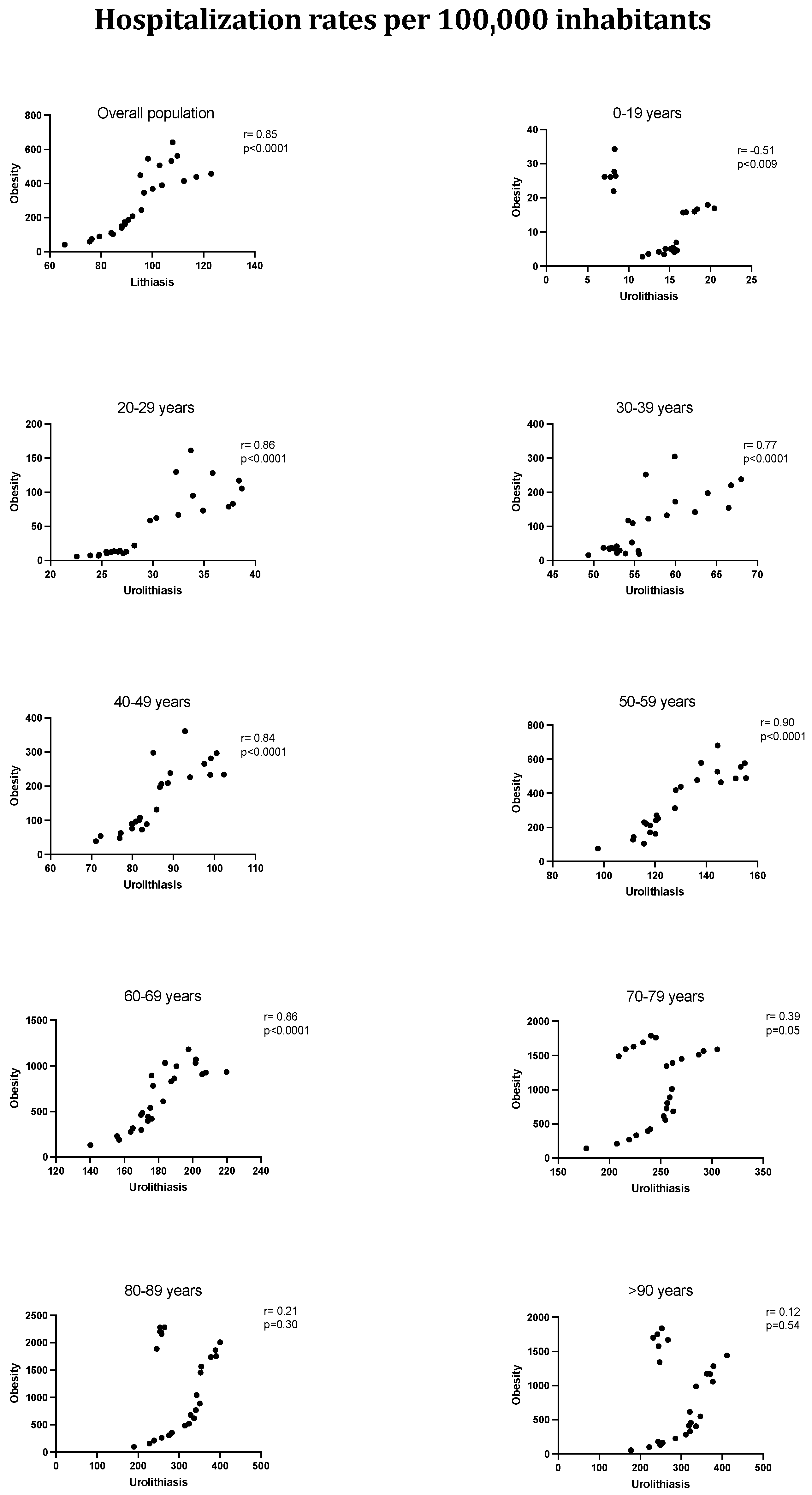
3.3. Hospitalized Lithiasis Incidence in the General and Obese Populations
3.4. Influence of Obesity on Mortality, Length of Stay, and Costs of Hospitalized Lithiasis Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ramello, A.; Vitale, C.; Marangella, M. Epidemiology of nephrolithiasis. J. Nephrol. 2000, 13 (Suppl. S3), S45–S50. [Google Scholar] [PubMed]
- Trinchieri, A. Epidemiology of urolithiasis: An update. Clin. Cases Miner. Bone Metab. 2008, 5, 101–106. [Google Scholar] [PubMed]
- Romero, V.; Akpinar, H.; Assimos, D.G. Kidney stones: A global picture of prevalence, incidence, and associated risk factors. Rev. Urol. 2010, 12, e86–e96. [Google Scholar]
- Di Cesare, M.; NCD Risk Factor Collaboration. Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef]
- Taylor, E.N.; Fung, T.T.; Curhan, G.C. DASH-style diet associates with reduced risk for kidney stones. J. Am. Soc. Nephrol. 2009, 20, 2253–2259. [Google Scholar] [CrossRef]
- Saenz-Medina, J.; Muñoz, M.; Rodriguez, C.; Contreras, C.; Sánchez, A.; Coronado, M.J.; Ramil, E.; Santos, M.; Carballido, J.; Prieto, D. Hyperoxaluria Induces Endothelial Dysfunction in Preglomerular Arteries: Involvement of Oxidative Stress. Cells 2022, 11, 2306. [Google Scholar] [CrossRef]
- Saenz-Medina, J.; Muñoz, M.; Rodriguez, C.; Contreras, C.; Sánchez, A.; Coronado, M.J.; Ramil, E.; Santos, M.; Carballido, J.; Prieto, D. Comorbidity and sociodemographic factors associated with renal lithiasis in persons aged 40 to 65: A cross-sectional study. Med. Clin. 2017, 149, 383–390. [Google Scholar] [CrossRef]
- Sánchez-Martín, F.M.; Martínez-Rodríguez, R. Incidence and prevalence of published studies about urolithiasis in Spain. A review. Actas Urol. Esp. 2007, 31, 511–520. [Google Scholar] [CrossRef]
- De Lorenzo, A.; Gratteri, S.; Gualtieri, P.; Cammarano, A.; Bertucci, P.; Di Renzo, L. Why primary obesity is a disease? J. Transl. Med. 2019, 17, 169. [Google Scholar] [CrossRef]
- Grases, F. Epidemiology of renal lithiasis and associated factors. Med. Clin. 2017, 149, 397–398. [Google Scholar] [CrossRef]
- Sorokin, I.; Mamoulakis, C.; Miyazawa, K.; Rodgers, A.; Talati, J.; Lotan, Y. Epidemiology of stone disease across the world. World J. Urol. 2017, 35, 1301–1320. [Google Scholar] [CrossRef] [PubMed]
- Levy, D.T.; Mabry, P.L.; Wang, Y.C.; Gortmaker, S.; Huang, T.K.; Marsh, T.; Moodie, M.; Swinburn, B. Simulation models of obesity: A review of the literature and implications for research and policy. Obes. Rev. 2011, 12, 378–394. [Google Scholar] [CrossRef] [PubMed]
- Manzoor, M.A.P.; Agrawal, A.K.; Singh, B.; Mujeeburahiman, M.; Rekha, P.-D. Morphological characteristics and microstructure of kidney stones using synchrotron radiation μCT reveal the mechanism of crystal growth and aggregation in mixed stones. PLoS ONE 2019, 14, e0214003. [Google Scholar] [CrossRef]
- Grases, F.; Costa-Bauzá, A.; Prieto, R.M. May renal lithiasis be really prevented? New trends and therapeutic tools. Arch. Esp. Urol. 2017, 70, 91–102. [Google Scholar]
- Khan, S.R.; Pearle, M.S.; Robertson, W.G.; Gambaro, G.; Canales, B.K.; Doizi, S.; Traxer, O.; Tiselius, H.G. Kidney stones. Nat. Rev. Dis. Primers 2016, 2, 16008. [Google Scholar] [CrossRef]
- Arbelaez, M.C.S.; Nackeeran, S.; Shah, K.; Blachman-Braun, R.; Bronson, I.; Towe, M.; Bhat, A.; Marcovich, R.; Ramasamy, R.; Shah, H.N. Association between body mass index, metabolic syndrome and common urologic conditions: A cross-sectional study using a large multi-institutional database from the United States. Ann. Med. 2023, 55, 2197293. [Google Scholar] [CrossRef]
- West, B.; Luke, A.; Durazo-Arvizu, R.A.; Cao, G.; Shoham, D.; Kramer, H. Metabolic syndrome and self-reported history of kidney stones: The National Health and Nutrition Examination Survey (NHANES III) 1988-1994. Am. J. Kidney Dis. 2008, 51, 741–747. [Google Scholar] [CrossRef]
- Carbone, A.; Al Salhi, Y.; Tasca, A.; Palleschi, G.; Fuschi, A.; De Nunzio, C.; Bozzini, G.; Mazzaferro, S.; Pastore, A.L. Obesity and kidney stone disease: A systematic review. Minerva Urol. Nefrol. 2018, 70, 393–400. [Google Scholar] [CrossRef]
- Taylor, E.N.; Stampfer, M.J.; Curhan, G.C. Diabetes mellitus and the risk of nephrolithiasis. Kidney Int. 2005, 68, 1230–1235. [Google Scholar] [CrossRef]
- Domingos, F.; Serra, A. Nephrolithiasis is associated with an increased prevalence of cardiovascular disease. Nephrol. Dial. Transplant. 2011, 26, 864–868. [Google Scholar] [CrossRef]
- Saenz, J. Murine model for the evaluation of hyperoxaluria on metabolic syndrome patients. Eur. Urol. Suppl. 2016, 3, e916–e916a. [Google Scholar] [CrossRef]
- Sáenz-Medina, J.; Muñoz, M.; Sanchez, A.; Rodriguez, C.; Jorge, E.; Corbacho, C.; Izquierdo, D.; Santos, M.; Donoso, E.; Virumbrales, E.; et al. Nox1-derived oxidative stress as a common pathogenic link between obesity and hyperoxaluria-related kidney injury. Urolithiasis 2019, 48, 481–492. [Google Scholar] [CrossRef] [PubMed]
- Pearle, M.S.; Calhoun, E.A.; Curhan, G.C.; Urologic Diseases of America Project. Urologic diseases in America project: Urolithiasis. J. Urol. 2005, 173, 848–857. [Google Scholar] [CrossRef]
- World Bank Open Data. Available online: https://data.worldbank.org (accessed on 13 August 2024).
- Raynal, G.; Merlet, B.; Traxer, O. In-hospital stays for urolithiasis: Analysis of French national data. Prog. Urol. 2011, 21, 459–462. [Google Scholar] [CrossRef]
- Trinchieri, A.; Croppi, E.; Montanari, E. Obesity and urolithiasis: Evidence of regional influences. Urolithiasis 2017, 45, 271–278. [Google Scholar] [CrossRef]
- Cano-Castiñeira, R.; Carrasco-Valiente, J.; Pérula-de-Torres, L.A.; Jiménez-García, C.; Olaya-Caro, I.; Criado-Larumbe, M.; Requena-Tapia, M.J. Prevalence of renal stones in Andalusian population: Results of PreLiRenA study. Actas Urol. Esp. 2015, 39, 26–31. [Google Scholar] [CrossRef]
- Sáenz, J.; Páez, A.; Alarcón, R.O.; Casas, J.M.; Sánchez, A.; Pereira, E.; Cáncer, E.; Alvarez, M.; Rendón, D.; Durán, M. Obesity as risk factor for lithiasic recurrence. Actas Urol. Esp. 2012, 36, 228–233. [Google Scholar] [CrossRef]
- Bahia, L.; Coutinho, E.S.F.; Barufaldi, L.A.; de Azevedo Abreu, G.; Malhão, T.A.; Ribeiro de Souza, C.P.; Araujo, D.V. The costs of overweight and obesity-related diseases in the Brazilian public health system: Cross-sectional study. BMC Public Health 2012, 12, 440. [Google Scholar] [CrossRef]
- Allender, S.; Rayner, M. The burden of overweight and obesity-related ill health in the UK. Obes. Rev. 2007, 8, 467–473. [Google Scholar] [CrossRef]
- Destri, K.; Henriques, A.R.; Mendonça, N.; Alves, J.; Barcelos, A.; Dias, S.S.; Gregório, M.J.; Canhão, H.; Rodrigues, A.M. Hospitalization costs in Portugal among people with obesity: Results from a nationwide population-based cohort 2011 to 2021. Front. Public Health 2024, 12, 1380690. [Google Scholar] [CrossRef]
- Javaid, S.; Frasier, K.; Chaudhary, A.J. Impact of obesity on in-hospital mortality and morbidity among patients admitted for antineoplastic chemotherapy: A nationwide analysis. Clin. Transl. Oncol. 2024, 26, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Bhanot, R.; Pietropaolo, A.; Tokas, T.; Kallidonis, P.; Skolarikos, A.; Keller, E.X.; De Coninck, V.; Traxer, O.; Gozen, A.; Sarica, K.; et al. Predictors and Strategies to Avoid Mortality Following Ureteroscopy for Stone Disease: A Systematic Review from European Association of Urologists Sections of Urolithiasis (EULIS) and Uro-technology (ESUT). Eur. Urol. Focus. 2022, 8, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Kim, F.; Pham, M.; Maloney, E.; Rizzo, N.O.; Morton, G.J.; Wisse, B.E.; Kirk, E.A.; Chait, A.; Schwartz, M.W. Vascular inflammation, insulin resistance, and reduced nitric oxide production precede the onset of peripheral insulin resistance. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 1982–1988. [Google Scholar] [CrossRef] [PubMed]
- Saenz-Medina, J.; Muñoz, M.; Rodriguez, C.; Sanchez, A.; Contreras, C.; Carballido-Rodríguez, J.; Prieto, D. Endothelial Dysfunction: An Intermediate Clinical Feature between Urolithiasis and Cardiovascular Diseases. Int. J. Mol. Sci. 2022, 23, 912. [Google Scholar] [CrossRef]
| Age | 1997–2001 | 2002–2006 | 2007–2011 | 2012–2016 | 2017–2021 | Overall 1997–2021 | % Change | p |
|---|---|---|---|---|---|---|---|---|
| <20 years | 13.3 (13–13.6) | 15.5 (15.1–15.8) | 16.2 (15.8–16.5) | 16.9 (16.6–17.3) | 8 (7.7–8.2) | 14 (13.8–14.1) | −1.84 | ns |
| 20–29 years | 24.6 (24–25.1) | 26.1 (25.6–26.6) | 28.2 (27.7–28.8) | 35.3 (34.5–36) | 35.8 (35–36.5) | 29.4 (29.1–29.6) | 2.12 (0.8–3.5) | <0.05 |
| 30–39 years | 53.5 (52.7–54.3) | 52.1 (51.4–52.7) | 53.7 (53–54.5) | 60.8 (60–61.6) | 63 (62.2–64) | 56.5 (56.2–56.9) | 0.97 (0.06–1.9) | <0.05 |
| 40–49 years | 76.1 (75–77.1) | 80.9 (79.9–81.9) | 85 (84.1–86) | 94.4 (93.4–95.4) | 95 (94–96) | 87.24 (86.8–87.7) | 1.2 (0.8–1.6) | <0.05 |
| 50–59 years | 111.5 (110.1–112.9) | 117.8 (116.4–119.1) | 125.6 (124.3–127) | 143.9 (142.6–145.2) | 147 (145.7–148.3) | 131.4 (130.8–132) | 1.5 (1–2) | <0.05 |
| 60–69 years | 157.1 (155.4–158.9) | 171.7 (169.8–173.5) | 178.8 (177–180.6) | 199.7 (197.9–201.5) | 195.2 (193.5–196.9) | 181.9 (181.1–182.7) | 1.2 (0.5–1.8) | <0.05 |
| 70–79 years | 214.3 (211.2–216.7) | 253.1 (250.7–255.5) | 258.5 (256.1–260.9) | 272.3 (269.8–274.8) | 231.5 (229.4–233.7) | 246.5 (245.5–247.6) | 0.5 (−0.8–1.7) | ns |
| 80–89 years | 238.8 (234.8–242.9) | 318.3 (314.1–322.5) | 348.3 (344.4–352.3) | 359.2 (355.6–362.9) | 257.1 (254.1–260.2) | 307.9 (306.3–309.6) | 0.5 (−1.7–2.8) | ns |
| >89 years | 231.1 (220.3–242.2) | 315.1 (304–326.5) | 342 (331.7–352.5) | 351.6 (342.9–360.6) | 246.3 (239.9–252.8) | 297.2 (293.1–301.2) | 0.48 (−1.8–2.8) | ns |
| Total | 76.4 (76–76.8) | 87.8 (87.4–88.2) | 95.2 (94.8–95.6) | 110.3 (109.9–110.8) | 105.3 (104.9–105.7) | 95.6 (95.4–95.8) | 1.8 (0.2–3.3) | <0.05 |
| Age | 1997–2001 | 2002–2006 | 2007–2011 | 2012–2016 | 2017–2021 | Overall 1997–2021 | % Change | p |
|---|---|---|---|---|---|---|---|---|
| <20 years | 3.8 (3.6–4) | 4.6 (4.4–4.8) | 9.7 (9.4–10) | 17.9 (17.5–18.3) | 28 (27.6–28.5) | 12.9 (12.8–13.1) | 11.3 (8.5–14.1) | <0.01 |
| 20–29 years | 7.7 (7.5–8) | 12.3 (11.9–12.7) | 32.8 (32.1–33.3) | 78.8 (77.7–79.9) | 128.2 (126.8–129.6) | 45.9 (45.5–46.2) | 16.1 (11.4–20.9) | <0.001 |
| 30–39 years | 21 (20.5–21.5) | 34.1 (33.5–34.7) | 71.5 (70.7–72.3) | 143.8 (142.5–145) | 240.9 (239.2–242.6) | 100.3 (99.8–100.8) | 13.5 (11.7–15.2) | <0.001 |
| 40–49 years | 55.5 (55–56.4) | 88.2 (87.1–89.2) | 150.4 (149.1–151.7) | 227.9 (226.4–229.4) | 300.8 (299–302.5) | 176.2 (175.5–176.8) | 9 (6.2–12) | <0.001 |
| 50–59 years | 123.8 (122.3–125.3) | 215 (213.2–216.9) | 340.4 (338.3–342.6) | 471.4 (469–473.8) | 583.7 (581.2–586.3) | 373.8 (372.7–374.8) | 8.1 (5.8–10.4) | <0.01 |
| 60–69 years | 222.6 (220.5–224.7) | 407.7 (404.9–410.5) | 655.26 (651.8–658.7) | 905.6 (901.7–909.4) | 1064.7 (1060.8–1068.7) | 681.8 (680.3–683.4) | 8.2 (5.6–10.8) | <0.01 |
| 70–79 years | 273.49 (270.8–276.2) | 602.7 (598.9–606.4) | 1084.7 (1079.8–1089.6) | 1522.4 (1516.5–1528.3) | 1695.7 (1689.8–1701.6) | 1070.5 (1068.3–1072.7) | 9.6 (5.4–13.8) | =0.01 |
| 80–89 years | 208.4 (204.7–212.2) | 538 (532.5–543.5) | 1162.1 (1154.9–1169.3) | 1853.8 (1845.5–1862.2) | 2223.5 (2214.7–2232.4) | 1374.2 (1370.7–1377.7) | 12.7 (6.8–18.7) | <0.01 |
| >89 years | 128.2 (120.2–136.6) | 335.5 (324–347.2) | 751.4 (736.1–767) | 1287.8 (1270.9–1304.8) | 1708.5 (1691.6–1725.5) | 1075.5 (1067.8–1083.3) | 13.9 (8.6–19.4) | <0.01 |
| Total | 74.5 (74.1–74.9) | 147.8 (147.3–148.3) | 271.58 (270.8–272.1) | 430.2 (429.3–431) | 557.9 (557–558.9) | 305.2 (304.9–305.5) | 10.7 (7.3–14.2) | <0.01 |
| Age | Lithiasis in General Population | Lithiasis in Obesity Population | Odds Ratio | p |
|---|---|---|---|---|
| <20 years | 12.3 (12.2–12.5) | 569.2 (488–660.1) | 46.4 (39.9–53.8) | p < 0.0001 |
| 20–29 years | 25.9 (25.7–26.2) | 691.6 (631.2–756.2) | 26.9 (24.5–29.4) | p < 0.0001 |
| 30–39 years | 51.4 (51.1–51.7) | 1126.9 (1078.4–1177) | 22.2 (21.2–23.2) | p < 0.0001 |
| 40–49 years | 80.3 (79.9–80.7) | 1712 (1665.7–1759.1) | 21.7 (21.1–22.3) | p < 0.0001 |
| 50–59 years | 120.8 (120.2–121.3) | 1730.5 (1695.2–1766.3) | 14.6 (14.3–14.9) | p < 0.0001 |
| 60–69 years | 163.8 (163.1–164.5) | 1523.4 (1496–1551.2) | 9.42 (9.3–9.6) | p < 0.0001 |
| 70–79 years | 225.8 (224.8–226.7) | 1213.6 (1191.1–1236.3) | 5.4 (5.3–5.5) | p < 0.0001 |
| 80–89 years | 286.6 (285–288.1) | 975.1 (950–1000.7) | 3.4 (3.3–3.5) | p < 0.0001 |
| >89 years | 282.9 (279.1–286.8) | 639.9 (583.1–698.6) | 2.3 (2.1–2.5) | p < 0.0001 |
| Total | 86.4 (86.2–86.6) | 1330.5 (1318.8–1342.7) | 15.6 (15.4–15.7) | p < 0.0001 |
| Age | Length of Stay (95% CI) Days | Mortality % (95% CI) | Cost (95% CI) EUR | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Normal Weight | Obesity | p | Normal Weight | Obesity | p | Normal Weight | Obesity | p | |
| <20 years | 7 (6.9–7.1) | 7.3 (5.5–9.1) | ns | 0.3 (0.3–0.4) | 0.6 (0.01–3.2) | ns | 3379 (3267–3490) | 3540 (3117–3964) | ns |
| 20–29 years | 5.2 (5.1–5.3) | 5 (4.4–5.5) | ns | 0.2 (0.1–0.2) | 0.6 (0.1–0.2) | ns | 3085 (3040–3129) | 3638 (3387–3890) | p < 0.0001 |
| 30–39 years | 5.24 (5.1–5.4) | 5.7 (5.3–6) | ns | 0.4 (0.3–0.4) | 0.3 (0.1–0.6) | ns | 3128 (3098–3157) | 3963 (3760–4166) | p < 0.0001 |
| 40–49 years | 5.6 (5.4–5.8) | 5.7 (5.5–5.9) | ns | 0.7 (0.6–0.7) | 0.8 (0.6–1.1) | ns | 3383 (3357–3408) | 4344 (4176–4511) | p < 0.0001 |
| 50–59 years | 6.2 (6.1–6.2) | 6.4 (6.2–6.6) | 0.01 | 1.3 (1.2–1.4) | 0.9 (0.8–1.2) | p = 0.005 | 3831 (3800–3862) | 4721 (4601–4841) | p < 0.0001 |
| 60–69 years | 7.7 (7.7–7.8) | 7.3 (7.1–7.5) | <0.001 | 2.4 (2.4–2.5) | 1.7 (1.5–2) | p < 0.0001 | 4318 (4282–4354) | 5070 (4950–5190) | p < 0.0001 |
| 70–79 years | 9.5 (9.4–9.5) | 8.7 (8.5–8.9) | <0.001 | 4.6 (4.5–4.7) | 3.8 (3.4–4.1) | p < 0.0001 | 4760 (4719–4801) | 5100 (4971–5228) | p < 0.0001 |
| 80–89 years | 10 (10–10.1) | 9.3 (9.1–9.5) | <0.001 | 9 (8.8–9.1) | 6.7 (6–7.3) | p < 0.0001 | 4763 (4717–4807) | 4860 (4709–5010) | ns |
| >89 years | 9.6 (9.4–9.7) | 9.2 (8.5–9.9) | ns | 14.9 (14.4–15.3) | 13.4 (10.5–16.8) | ns | 4628 (4544–4712) | 4856 (4376–5337) | ns |
| Total | 7.4 (7.4–7.5) | 7.5 (7.4–7.6) | ns | 3 (3–3.1) | 2.6 (2.4–2.7) | p < 0.001 | 4015 (4002–4030) | 4789 (4732–4846) | p < 0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Monsalve, M.; Durán-Poveda, M.; Gómez Dos Santos, V.; Burgos Revilla, J.; García-Criado, E.; Prieto, D.; Gil de Miguel, Á.; Sáenz-Medina, J. Impact of Obesity on Hospitalization Burden of Urolithiasis in Spain Between 1997 and 2021. J. Clin. Med. 2025, 14, 381. https://doi.org/10.3390/jcm14020381
Rodríguez-Monsalve M, Durán-Poveda M, Gómez Dos Santos V, Burgos Revilla J, García-Criado E, Prieto D, Gil de Miguel Á, Sáenz-Medina J. Impact of Obesity on Hospitalization Burden of Urolithiasis in Spain Between 1997 and 2021. Journal of Clinical Medicine. 2025; 14(2):381. https://doi.org/10.3390/jcm14020381
Chicago/Turabian StyleRodríguez-Monsalve, María, Manuel Durán-Poveda, Victoria Gómez Dos Santos, Javier Burgos Revilla, Elena García-Criado, Dolores Prieto, Ángel Gil de Miguel, and Javier Sáenz-Medina. 2025. "Impact of Obesity on Hospitalization Burden of Urolithiasis in Spain Between 1997 and 2021" Journal of Clinical Medicine 14, no. 2: 381. https://doi.org/10.3390/jcm14020381
APA StyleRodríguez-Monsalve, M., Durán-Poveda, M., Gómez Dos Santos, V., Burgos Revilla, J., García-Criado, E., Prieto, D., Gil de Miguel, Á., & Sáenz-Medina, J. (2025). Impact of Obesity on Hospitalization Burden of Urolithiasis in Spain Between 1997 and 2021. Journal of Clinical Medicine, 14(2), 381. https://doi.org/10.3390/jcm14020381







