Prevalence of Knee Pain and Its Relation to Depression, Anxiety, and Health-Related Quality of Life Among Maintenance Hemodialysis Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Sociodemographic Data and Clinical Characteristics
2.3. Knee Pain Screening Tool (KNEST) and Visual Analog Scale (VAS)
2.4. The Western Ontario and McMaster Universities Arthritis Index (WOMAC)
2.5. Hospital Anxiety and Depression Scale (HADS)
2.6. The Kidney Disease Quality of Life-36 (KDQOL-36)
2.7. Blood Sampling and Laboratory Tests
2.8. Statistical Analysis
3. Results
3.1. Sociodemographic Data and Clinical Characteristics
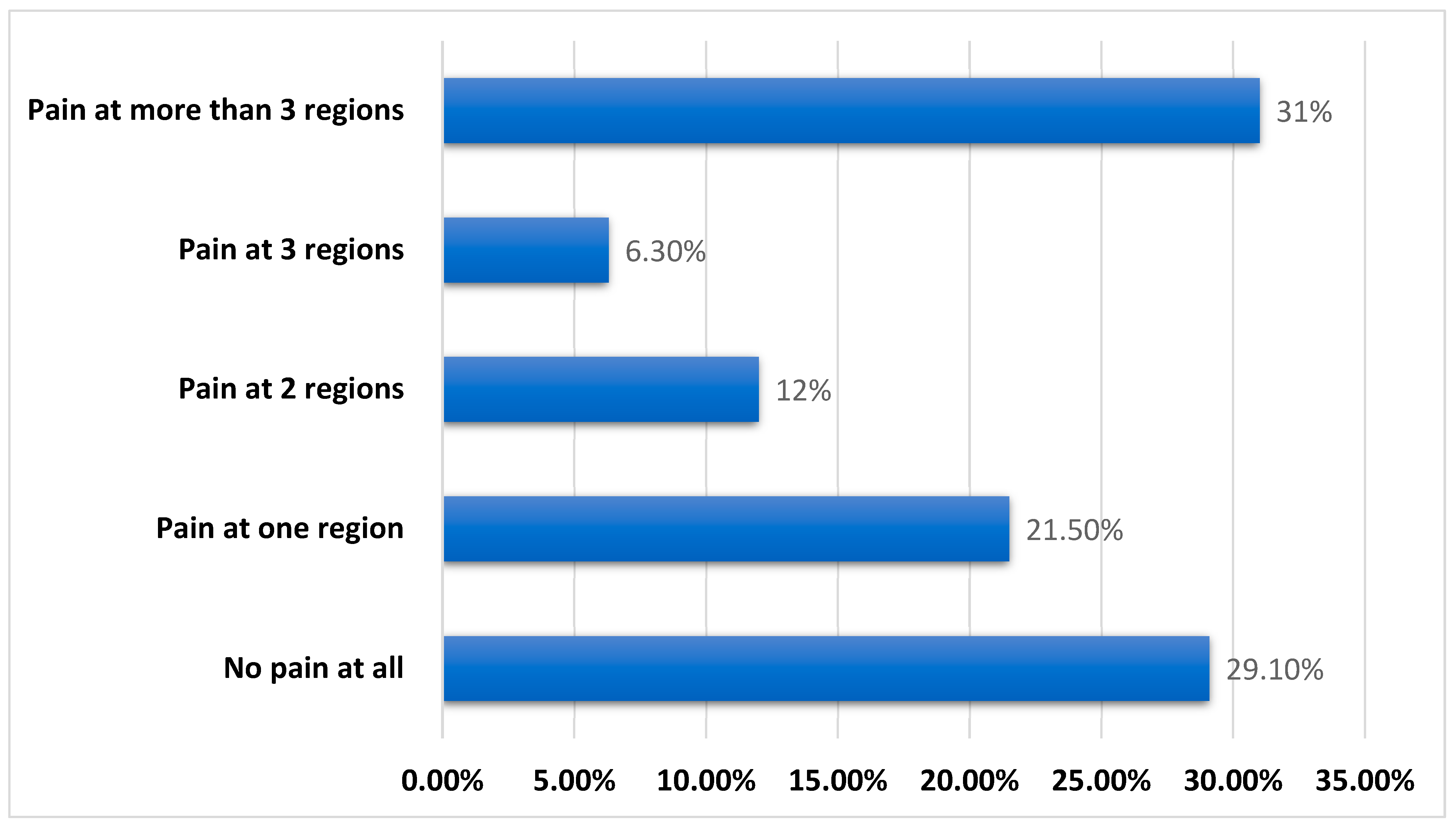
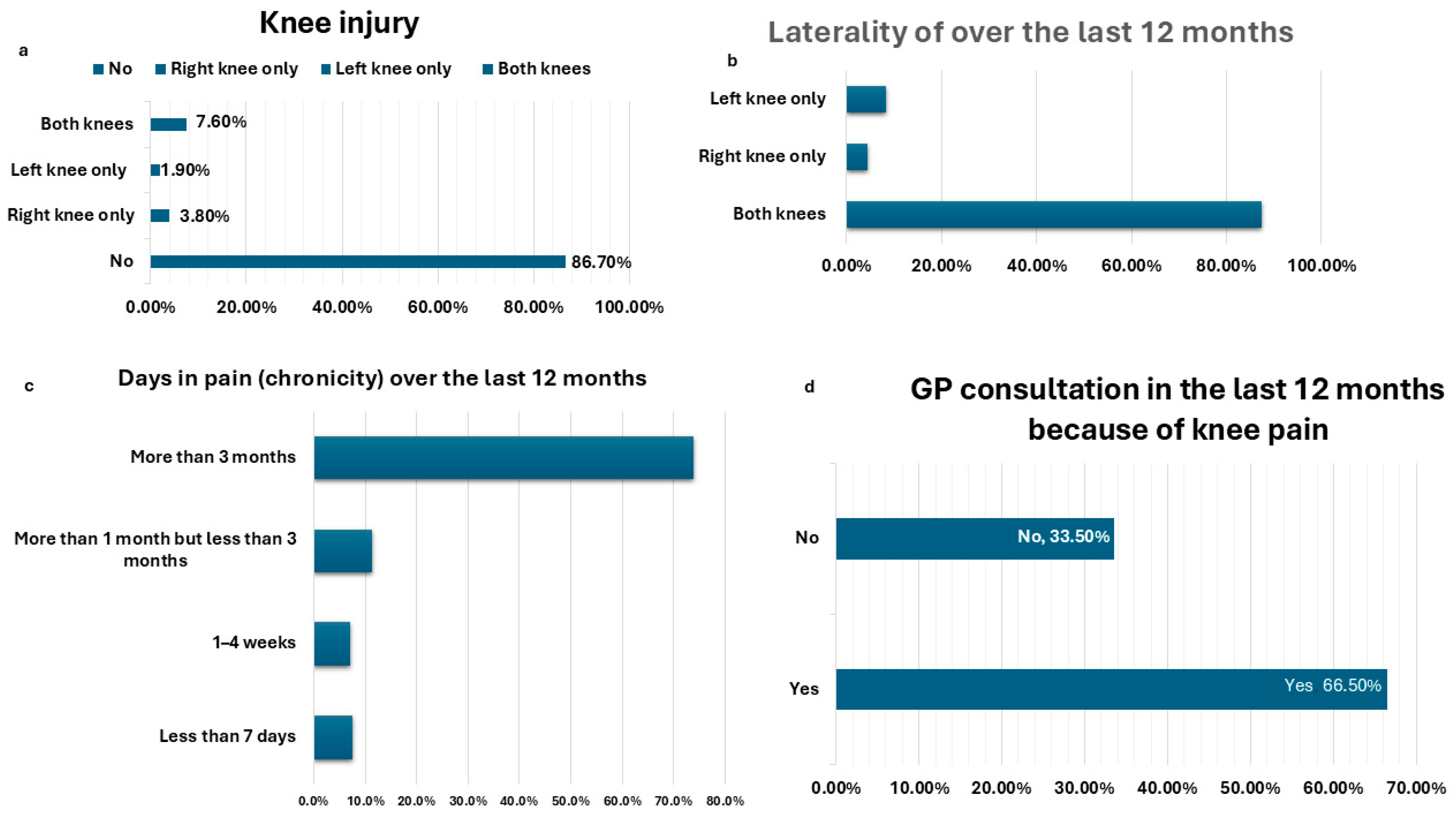
3.2. Knee Pain Screening Tool (KNEST)
3.3. Hospital Anxiety and Depression Scale (HADS) and the Kidney Disease Quality of Life-36 (KDQOL-36)
3.4. The Effect of Pain Severity Among Patients with Knee Pain
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bikbov, B.; Purcell, C.A.; Levey, A.S.; Smith, M.; Abdoli, A.; Abebe, M.; Adebayo, O.M.; Afarideh, M.; Agarwal, S.K.; Agudelo-Botero, M. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef] [PubMed]
- Liyanage, T.; Ninomiya, T.; Jha, V.; Neal, B.; Patrice, H.M.; Okpechi, I.; Zhao, M.-h.; Lv, J.; Garg, A.X.; Knight, J. Worldwide access to treatment for end-stage kidney disease: A systematic review. Lancet 2015, 385, 1975–1982. [Google Scholar] [CrossRef] [PubMed]
- Valderrábano, F.; Jofre, R.; López-Gómez, J.M. Quality of life in end-stage renal disease patients. Am. J. Kidney Dis. 2001, 38, 443–464. [Google Scholar] [CrossRef]
- Hage, S.; Hage, V.; El-Khoury, N.; Azar, H.; Chelala, D.; Ziadé, N. Musculoskeletal disorders in hemodialysis patients: Different disease clustering according to age and dialysis vintage. Clin. Rheumatol. 2020, 39, 533–539. [Google Scholar] [CrossRef]
- Ezzat, S.; Tharwat, S.; Abdelsalam, S.; Eltoraby, E.E. Musculoskeletal Symptoms in Hemodialysis Patients and their Effect on Health-Related Quality of Life. Blood Purif. 2020, 49, 289–294. [Google Scholar] [CrossRef]
- Fidan, F.; Alkan, B.M.; Tosun, A.; Altunoğlu, A.; Ardıçoğlu, Ö. Quality of life and correlation with musculoskeletal problems, hand disability and depression in patients with hemodialysis. Int. J. Rheum. Dis. 2016, 19, 159–166. [Google Scholar] [CrossRef]
- Santoro, D.; Satta, E.; Messina, S.; Costantino, G.; Savica, V.; Bellinghieri, G. Pain in end-stage renal disease: A frequent and neglected clinical problem. Clin. Nephrol. 2013, 79, S2–S11. [Google Scholar] [CrossRef]
- Poleshuck, E.L.; Bair, M.J.; Kroenke, K.; Damush, T.M.; Tu, W.; Wu, J.; Krebs, E.E.; Giles, D.E. Psychosocial stress and anxiety in musculoskeletal pain patients with and without depression. Gen. Hosp. Psychiatry 2009, 31, 116–122. [Google Scholar] [CrossRef]
- Kii, S.; Sonohata, M.; Hashimoto, A.; Nakashima, T.; Kawaguchi, A.; Matsumura, Y.; Shimazaki, T.; Nagamine, S.; Mawatari, M. Mid-term clinical outcomes and complications of primary total knee arthroplasty in hemodialysis patients: A retrospective comparative cohort study. BMC Musculoskelet. Disord. 2021, 22, 927. [Google Scholar] [CrossRef]
- Revicki, D.A. Health-related quality of life in the evaluation of medical therapy for chronic illness. J. Fam. Pract. 1989, 29, 377–380. [Google Scholar]
- Hill, C.L.; Parsons, J.; Taylor, A.; Leach, G. Health related quality of life in a population sample with arthritis. J. Rheumatol. 1999, 26, 2029–2035. [Google Scholar] [PubMed]
- Muraki, S.; Akune, T.; Oka, H.; En-yo, Y.; Yoshida, M.; Saika, A.; Suzuki, T.; Yoshida, H.; Ishibashi, H.; Tokimura, F. Association of radiographic and symptomatic knee osteoarthritis with health-related quality of life in a population-based cohort study in Japan: The ROAD study. Osteoarthr. Cartil. 2010, 18, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Phyomaung, P.P.; Dubowitz, J.; Cicuttini, F.M.; Fernando, S.; Wluka, A.E.; Raaijmaakers, P.; Wang, Y.; Urquhart, D.M. Are depression, anxiety and poor mental health risk factors for knee pain? A systematic review. BMC Musculoskelet. Disord. 2014, 15, 10. [Google Scholar] [CrossRef]
- de Rooij, M.; van der Leeden, M.; Heymans, M.W.; Holla, J.F.; Häkkinen, A.; Lems, W.F.; Roorda, L.D.; Veenhof, C.; Sanchez-Ramirez, D.C.; de Vet, H.C.; et al. Prognosis of pain and physical functioning in patients with knee osteoarthritis: A systematic review and meta-analysis. Arthritis Care Res. 2016, 68, 481–492. [Google Scholar] [CrossRef]
- Binik, Y.M.; Baker, A.G.; Kalogeropoulos, D.; Devins, G.M.; Guttmann, R.D.; Hollomby, D.J.; Barré, P.E.; Hutchison, T.; Prud’Homme, M.; McMullen, L. Pain, control over treatment, and compliance in dialysis and transplant patients. Kidney Int. 1982, 21, 840–848. [Google Scholar] [CrossRef]
- Li, X.; Pan, F.; Zhu, R.; Ge, L.; Zhang, X.; Wen, X.; Zhou, J.; Cheng, J.; Pan, F.; Cai, G. Cross-Sectional and Longitudinal Associations of Comorbidities with Knee Symptoms and Radiographic Abnormalities of Osteoarthritis. Rheumatol. Ther. 2024, 11, 129–142. [Google Scholar] [CrossRef]
- Jinks, C.; Jordan, K.; Ong, B.; Croft, P. A brief screening tool for knee pain in primary care (KNEST). 2. Results from a survey in the general population aged 50 and over. Rheumatology 2004, 43, 55–61. [Google Scholar] [CrossRef]
- Von Korff, M.; Ormel, J.; Keefe, F.J.; Dworkin, S.F. Grading the severity of chronic pain. Pain 1992, 50, 133–149. [Google Scholar] [CrossRef]
- Jinks, C.; Lewis, M.; Ong, B.; Croft, P. A brief screening tool for knee pain in primary care. 1. Validity and reliability. Rheumatology 2001, 40, 528–536. [Google Scholar] [CrossRef]
- Cavalcante, R.; Arruda, J.; Zaccariotti, V.; Marques, R.; Santos, V.; Fernandes, Y. Evaluation between the SINS Score, VAS, and neurological status for spinal metastatic tumors. Glob. Spine J. 2016, 6, s-0036. [Google Scholar] [CrossRef]
- Alghadir, A.; Anwer, S.; Iqbal, Z.A.; Alsanawi, H.A. Cross-cultural adaptation, reliability and validity of the Arabic version of the reduced Western Ontario and McMaster Universities Osteoarthritis index in patients with knee osteoarthritis. Disabil. Rehabil. 2016, 38, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Faik, A.; Benbouazza, K.; Amine, B.; Maaroufi, H.; Bahiri, R.; Lazrak, N.; Aboukal, R.; Hajjaj-Hassouni, N. Translation and validation of Moroccan Western Ontario and Mc Master Universities (WOMAC) osteoarthritis index in knee osteoarthritis. Rheumatol. Int. 2008, 28, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Jinks, C.; Jordan, K.; Croft, P. Measuring the population impact of knee pain and disability with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Pain 2002, 100, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Terkawi, A.S.; Tsang, S.; AlKahtani, G.J.; Al-Mousa, S.H.; Al Musaed, S.; AlZoraigi, U.S.; Alasfar, E.M.; Doais, K.S.; Abdulrahman, A.; Altirkawi, K.A. Development and validation of Arabic version of the Hospital Anxiety and Depression Scale. Saudi J. Anaesth. 2017, 11, S11–S18. [Google Scholar] [CrossRef]
- Mykletun, A.; Stordal, E.; Dahl, A.A. Hospital Anxiety and Depression (HAD) scale: Factor structure, item analyses and internal consistency in a large population. Br. J. Psychiatry 2001, 179, 540–544. [Google Scholar] [CrossRef]
- Albatineh, A.N.; Al-Taiar, A.; Al-Sabah, R.; Zogheib, B. Psychometric properties of the Arabic version of the Hospital Anxiety and Depression Scale in hemodialysis patients. Psychol. Health Med. 2024, 29, 1664–1679. [Google Scholar] [CrossRef]
- Chao, S.; Yen, M.; Lin, T.-C.; Sung, J.-M.; Wang, M.-C.; Hung, S.-Y. Psychometric properties of the kidney disease quality of life–36 questionnaire (KDQOL-36™). West. J. Nurs. Res. 2016, 38, 1067–1082. [Google Scholar] [CrossRef]
- Schatell, D.; Witten, B. Measuring dialysis patients’ health-related Quality of life with the KDQOL-36™. Med. Educ. Inst. 2008, 608, 833–8033. [Google Scholar]
- Pagana, K.D.; Pagana, T.J. Mosby’s Manual of Diagnostic and Laboratory Tests-E-Book: Mosby’s Manual of Diagnostic and Laboratory Tests-E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2017. [Google Scholar]
- Jhun, H.-J.; Sung, N.-J.; Kim, S.Y. Knee pain and its severity in elderly Koreans: Prevalence, risk factors and impact on quality of life. J. Korean Med. Sci. 2013, 28, 1807–1813. [Google Scholar] [CrossRef]
- Song, Q.; Shen, P.; Mao, M.; Sun, W.; Zhang, C.; Li, L. Proprioceptive neuromuscular facilitation improves pain and descending mechanics among elderly with knee osteoarthritis. Scand. J. Med. Sci. Sports 2020, 30, 1655–1663. [Google Scholar] [CrossRef]
- Ganji, R.; Pakniat, A.; Armat, M.R.; Tabatabaeichehr, M.; Mortazavi, H. The effect of self-management educational program on pain intensity in elderly patients with knee osteoarthritis: A randomized clinical trial. Open Access Maced. J. Med. Sci. 2018, 6, 1062. [Google Scholar] [CrossRef] [PubMed]
- Zempo, H.; Miyamoto-Mikami, E.; Kikuchi, N.; Fuku, N.; Miyachi, M.; Murakami, H. Heritability estimates of muscle strength-related phenotypes: A systematic review and meta-analysis. Scand. J. Med. Sci. Sports 2017, 27, 1537–1546. [Google Scholar] [CrossRef] [PubMed]
- Glass, N.; Torner, J.; Law, L.F.; Wang, K.; Yang, T.; Nevitt, M.; Felson, D.; Lewis, C.; Segal, N.A. The relationship between quadriceps muscle weakness and worsening of knee pain in the MOST cohort: A 5-year longitudinal study. Osteoarthr. Cartil. 2013, 21, 1154–1159. [Google Scholar] [CrossRef] [PubMed]
- Akasbi, N.; Houssaini, T.S.; Tahiri, L.; Hachimi, H.; Maaroufi, C.E.; Youbi, R.E.; Arrayhani, M.; Harzy, T. Rheumatic complications of long term treatment with hemodialysis. Rheumatol. Int. 2012, 32, 1161–1163. [Google Scholar] [CrossRef]
- Hurton, S.; Embil, J.M.; Reda, A.; Smallwood, S.; Wall, C.; Thomson, L.; Zacharias, J.; Dascal, M.; Trepman, E.; Koulack, J. Upper extremity complications in patients with chronic renal failure receiving haemodialysis. J. Ren. Care 2010, 36, 203–211. [Google Scholar] [CrossRef]
- Sulkova, S.; Fortova, M.; Valek, M.; Svara, F. Renal bone disease. Vnitr Lek. 2003, 49, 403–408. [Google Scholar]
- Burston, J.J.; Valdes, A.M.; Woodhams, S.G.; Mapp, P.I.; Stocks, J.; Watson, D.J.G.; Gowler, P.R.W.; Xu, L.; Sagar, D.R.; Fernandes, G.; et al. The impact of anxiety on chronic musculoskeletal pain and the role of astrocyte activation. Pain 2019, 160, 658–669. [Google Scholar] [CrossRef]
- Leeuw, M.; Goossens, M.E.; Linton, S.J.; Crombez, G.; Boersma, K.; Vlaeyen, J.W. The fear-avoidance model of musculoskeletal pain: Current state of scientific evidence. J. Behav. Med. 2007, 30, 77–94. [Google Scholar] [CrossRef]
- Thompson, T.; Keogh, E.; French, C.C.; Davis, R. Anxiety sensitivity and pain: Generalisability across noxious stimuli. Pain 2008, 134, 187–196. [Google Scholar] [CrossRef]
- De Heer, E.W.; Ten Have, M.; Van Marwijk, H.W.; Dekker, J.; De Graaf, R.; Beekman, A.T.; Van Der Feltz-Cornelis, C.M. Pain as a risk factor for common mental disorders. Results from the Netherlands Mental Health Survey and Incidence Study-2: A longitudinal, population-based study. Pain 2018, 159, 712–718. [Google Scholar] [CrossRef]
- Kimmel, P.L.; Patel, S.S. Quality of life in patients with chronic kidney disease: Focus on end-stage renal disease treated with hemodialysis. In Seminars in Nephrology; Elsevier: Amsterdam, The Netherlands, 2006; pp. 68–79. [Google Scholar]
- Davison, S.N.; Jhangri, G.S. The impact of chronic pain on depression, sleep, and the desire to withdraw from dialysis in hemodialysis patients. J. Pain Symptom Manag. 2005, 30, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Belayev, L.Y.; Mor, M.K.; Sevick, M.A.; Shields, A.M.; Rollman, B.L.; Palevsky, P.M.; Arnold, R.M.; Fine, M.J.; Weisbord, S.D. Longitudinal associations of depressive symptoms and pain with quality of life in patients receiving chronic hemodialysis. Hemodial. Int. 2015, 19, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Weisbord, S.D.; Mor, M.K.; Green, J.A.; Sevick, M.A.; Shields, A.M.; Zhao, X.; Rollman, B.L.; Palevsky, P.M.; Arnold, R.M.; Fine, M.J. Comparison of symptom management strategies for pain, erectile dysfunction, and depression in patients receiving chronic hemodialysis: A cluster randomized effectiveness trial. Clin. J. Am. Soc. Nephrol. 2013, 8, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Kiadaliri, A.A.; Lamm, C.J.; de Verdier, M.G.; Engström, G.; Turkiewicz, A.; Lohmander, L.S.; Englund, M. Association of knee pain and different definitions of knee osteoarthritis with health-related quality of life: A population-based cohort study in southern Sweden. Health Qual. Life Outcomes 2016, 14, 1–7. [Google Scholar] [CrossRef]
- Bindawas, S.M.; Vennu, V.; Auais, M. Health-related quality of life in older adults with bilateral knee pain and back pain: Data from the Osteoarthritis Initiative. Rheumatol. Int. 2015, 35, 2095–2101. [Google Scholar] [CrossRef]
- Bindawas, S.M.; Vennu, V.; Al Snih, S. Differences in health-related quality of life among subjects with frequent bilateral or unilateral knee pain: Data from the Osteoarthritis Initiative study. J. Orthop. Sports Phys. Ther. 2015, 45, 128–136. [Google Scholar] [CrossRef]
- Smith, B.W.; Zautra, A.J. The effects of anxiety and depression on weekly pain in women with arthritis. Pain 2008, 138, 354–361. [Google Scholar] [CrossRef]
- Wise, R.G.; Lujan, B.J.; Schweinhardt, P.; Peskett, G.D.; Rogers, R.; Tracey, I. The anxiolytic effects of midazolam during anticipation to pain revealed using fMRI. Magn. Reson. Imaging 2007, 25, 801–810. [Google Scholar] [CrossRef]
| Variables Mean ± SD, Median (IQR), n (%) | Patients Without Knee Pain (n = 113) | Patients with Knee Pain (n = 158) | p Value | Effect Size # | 95% CI of Difference |
|---|---|---|---|---|---|
| Age (years) | 48 (20.50) | 53 (22) | 0.013 * | 0.357 | −7.50, −1.1 |
| Sex | |||||
| Male | 81 (71.7) | 79 (50) | <0.001 * | - | - |
| Female | 32 (28.3) | 79 (50) | |||
| Marital status | |||||
| Single/divorced/widowed | 27 (23.9) | 47 (29.7) | 0.286 | - | - |
| Married | 86 (76.1) | 111 (70.3) | |||
| Residence | |||||
| Rural | 66 (58.4) | 77 (48.7) | 0.116 | - | - |
| Urban | 47 (41.6) | 81 (51.3) | |||
| Education | |||||
| Not educated | 21 (18.6) | 52 (32.9) | |||
| Low School | 13 (11.5) | 18 (11.4) | |||
| Middle School | 12 (10.6) | 12 (7.6) | 0.136 | - | - |
| High School | 45 (39.8) | 57 (36.1) | |||
| College degree | 20 (17.7) | 17 (10.8) | |||
| Post-graduate | 2 (1.8) | 2 (1.3) | |||
| Socioeconomic status | |||||
| Low | 50 (44.2) | 73 (46.2) | |||
| Average | 61 (54) | 82 (51.9) | 0.944 | - | - |
| High | 2(1.8) | 3 (1.9) | |||
| Smoking | |||||
| Never | 59 (52.2) | 87 (55.1) | |||
| Former smoker | 35 (31) | 47 (29.7) | 0.886 | - | - |
| Current smoker | 19 (16.8) | 24 (15.2) |
| Variables | Patients Without Knee Pain (n = 113) | Patients with Knee Pain (n = 158) | p Value | Effect Size # | 95% CI of Difference |
|---|---|---|---|---|---|
| Duration of hemodialysis (years) | 4 (6.00) | 7 (8.00) | 0.004 * | 0.30 | −2.7, −0.29 |
| Associated comorbidities | |||||
| Diabetes | 16 (14.2) | 23 (14.6) | 0.927 | ||
| Hypertension | 71 (62.8) | 112 (70.9) | 0.163 | ||
| Chronic respiratory disease | 1 (0.9) | 3 (1.9) | 0.495 | - | - |
| Psychiatric disorder | 0 | 9 (5.7) | - | ||
| Ischemic heart disease | 10 (8.8) | 6 (3.8) | 0.082 | ||
| Therapeutic data | |||||
| Erythropoietin | 67 (59.3) | 88 (55.7) | 0.555 | ||
| Calcium supplementations | 102 (90.3) | 133 (84.2) | 0.145 | ||
| Iron supplementations | 93 (82.3) | 125 (79.1) | 0.514 | - | - |
| Antihypertensive drugs | 67 (59.3) | 121 (76.6) | 0.002 | ||
| Antidiabetic drugs | 25 (22.1) | 34 (21.5) | 0.905 | ||
| Laboratory data | |||||
| Blood hemoglobin (gm/dL) | 10.67 ± 1.3 | 10.26 ± 1.3 | 0.02 * | 0.32 | 0.063, 0.755 |
| Serum ferritin (ng/mL) | 265.7 (414.15) | 281.3 (237.38) | 0.811 | 0.02 | −154.68, 144.59 |
| TSAT (%) | 20.5 (8.75) | 20.5 (12.25) | 0.895 | 0.08 | −4.87, 3.69 |
| Serum calcium (mg/dL) | 8.4 (0.88) | 8.6 (0.58) | 0.790 | 0.02 | −0.22, 0.276 |
| Serum phosphorus (mg/dL) | 4.6 (2.85) | 4.5 (1.85) | 0.254 | 0.23 | −0.045, 0.66 |
| iPTH (pg/mL) | 405.5 (507) | 371 (564) | 0.666 | 0.07 | −233.72, 166.33 |
| Serum albumin (gm/dL) | 3.95 (0.20) | 4 (0.40) | 0.270 | 0.25 | −0.19, 0.74 |
| Variables Median (IQR), n (%) | Patients Without Knee Pain (n = 113) | Patients with Knee Pain (n = 158) | p Value | Effect Size # | 95% CI of Difference |
|---|---|---|---|---|---|
| Anxiety | |||||
| Normal | 37 (32.7) | 23 (14.6) | |||
| Borderline abnormal | 26 (23) | 47 (29.7) | 0.002 * | ||
| Abnormal | 50 (44.2) | 88 (55.7) | |||
| Depression | |||||
| Normal | 24 (21.2) | 18 (11.4) | |||
| Borderline abnormal | 30 (26.5) | 51 (32.3) | 0.080 | ||
| Abnormal | 59 (52.2) | 89 (56.3) | |||
| Health-related quality of life | |||||
| Symptom/problem list | 75 (20.83) | 66.67 (27.09) | 0.003 * | 0.341 | 1.93–11.6 |
| Effect of kidney disease | 68.75 (25.00) | 65.63 (28.12) | 0.501 | 0.101 | −2.93, 7.13 |
| Burden of kidney disease | 18.75 (31.25) | 12.5 (25.00) | 0.047 * | 0.195 | −0.93, 8.61 |
| PHC | 34.69 (9.57) | 30.65 (8.83) | <0.001 * | 0.503 | 1.80–5.11 |
| MHC | 37.59 (10.80) | 35.6 (7.98) | 0.001 * | 1.04 | 1.74–5.48 |
| Variables Median (IQR), n (%) | Patients with Knee Pain (n = 158) | Effect Size # | 95% CI of Difference | |||
|---|---|---|---|---|---|---|
| Mild (n = 12) | Moderate (n = 95) | Severe (n = 51) | p | |||
| WOMAC | 34.4 (27.60) 1,2 | 55.2 (19.79) 1 | 53.1 (29.17) 2 | 0.009 * | 0.202 | CI1 = −36.69, −12.11 CI2 = −42.63, −17.01 CI3 = −2.37, 13.22 |
| Pain | 5 (4.00) 1,2 | 9 (5.00) 1,3 | 10 (6.00) 2,3 | <0.001 * | 0.23 | CI1 = −7.29, −3.09 CI2 = −9.62, −5.13 CI3 = 0.786, 3.58 |
| Stiffness | 2 (3.50) 1,2 | 4 (3.00) 1,3 | 4 (4.00) 2,3 | <0.001 * | 0.16 | CI1 = −2.57, −0.672 CI2 = −3.66, −1.64 CI3 = 0.391, 1.67 |
| Physical | 25 (27.00) 1,2 | 39 (16.00) 1 | 39 (26.00) 2 | 0.009 * | 0.19 | CI1 = −24.81, −7.77 CI2 = −29.45, −11.65 CI3 = −1.0, 9.56 |
| Anxiety | ||||||
| Normal | 5 (41.6) 1 | 5 (5.3) 1,2 | 13 (25.5) 2 | |||
| Borderline abnormal | 5 (41.6) | 38 (40) | 4 (7.8) | <0.001 * | - | - |
| Abnormal | 2 (16.8) | 52 (54.7) | 34 (66.7) | |||
| Depression | ||||||
| Normal | 4 (33.3) 1 | 5 (5.3) 1,2 | 11 (21.6) 2 | |||
| Borderline abnormal | 1 (8.3) | 32 (33.6) | 15 (29.4) | 0.005 * | - | - |
| Abnormal | 7 (58.4) | 58 (61.1) | 25 (49) | |||
| Health-related quality of life | ||||||
| Symptom/problem list | 83.3 (35.41) | 64.6 (23.96) | 66.7 (30.21) | 0.143 | 0.02 | CI1 = −1.81, 19.55 CI2 = 3.26, 25.91 CI3 = −12.57, 1.14 |
| Effect of kidney disease | 68.7 (28.13) | 65.6 (31.25) | 62.5 (37.50) | 0.582 | 0.012 | CI1 = −6.21, 15.8 CI2 = −7.27, 16.17 CI3 = −6.71, 7.48 |
| Burden of kidney disease | 18.75 (56.25) | 12.5 (25.00) | 6.25 (25.00) | 0.648 | 0.05 | CI1 = 0.491, 21.30 CI2 = −0.356, 21.71 CI3 = −6.46, 6.90 |
| PHC | 35.2 (11.08) 1,2 | 30.2 (7.31) 1 | 29.2 (10.58) 2 | 0.046 * | 0.04 | CI1 = 1.466, 7.96 CI2 = 2.06, 8.95 CI3 = −2.87, 1.29 |
| MHC | 43.9 (9.35) | 35.6 (7.00) | 35.4 (11.19) | 0.058 | 0.04 | CI1 = 0.523, 8.23 CI2 = −0.989, 7.18 CI3 = −1.19, 3.75 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tharwat, S.; Nagy, E.; Elsayed, A.M.; Salem, K.M.; Salah, A.M.; Mohamed, S.Z.; Nassar, M.K. Prevalence of Knee Pain and Its Relation to Depression, Anxiety, and Health-Related Quality of Life Among Maintenance Hemodialysis Patients. J. Clin. Med. 2025, 14, 368. https://doi.org/10.3390/jcm14020368
Tharwat S, Nagy E, Elsayed AM, Salem KM, Salah AM, Mohamed SZ, Nassar MK. Prevalence of Knee Pain and Its Relation to Depression, Anxiety, and Health-Related Quality of Life Among Maintenance Hemodialysis Patients. Journal of Clinical Medicine. 2025; 14(2):368. https://doi.org/10.3390/jcm14020368
Chicago/Turabian StyleTharwat, Samar, Eman Nagy, Abdelrahman Mohammed Elsayed, Karem Mohamed Salem, Ahmed M. Salah, Sherin Zohdy Mohamed, and Mohammed Kamal Nassar. 2025. "Prevalence of Knee Pain and Its Relation to Depression, Anxiety, and Health-Related Quality of Life Among Maintenance Hemodialysis Patients" Journal of Clinical Medicine 14, no. 2: 368. https://doi.org/10.3390/jcm14020368
APA StyleTharwat, S., Nagy, E., Elsayed, A. M., Salem, K. M., Salah, A. M., Mohamed, S. Z., & Nassar, M. K. (2025). Prevalence of Knee Pain and Its Relation to Depression, Anxiety, and Health-Related Quality of Life Among Maintenance Hemodialysis Patients. Journal of Clinical Medicine, 14(2), 368. https://doi.org/10.3390/jcm14020368






