Transpancreatic Sphincterotomy Is a Safe and Effective Pancreatic Guidewire-Assisted Cannulation Method: Real-World Data Analysis of the Hungarian ERCP Registry
Abstract
1. Introduction
2. Materials and Methods
2.1. General Considerations
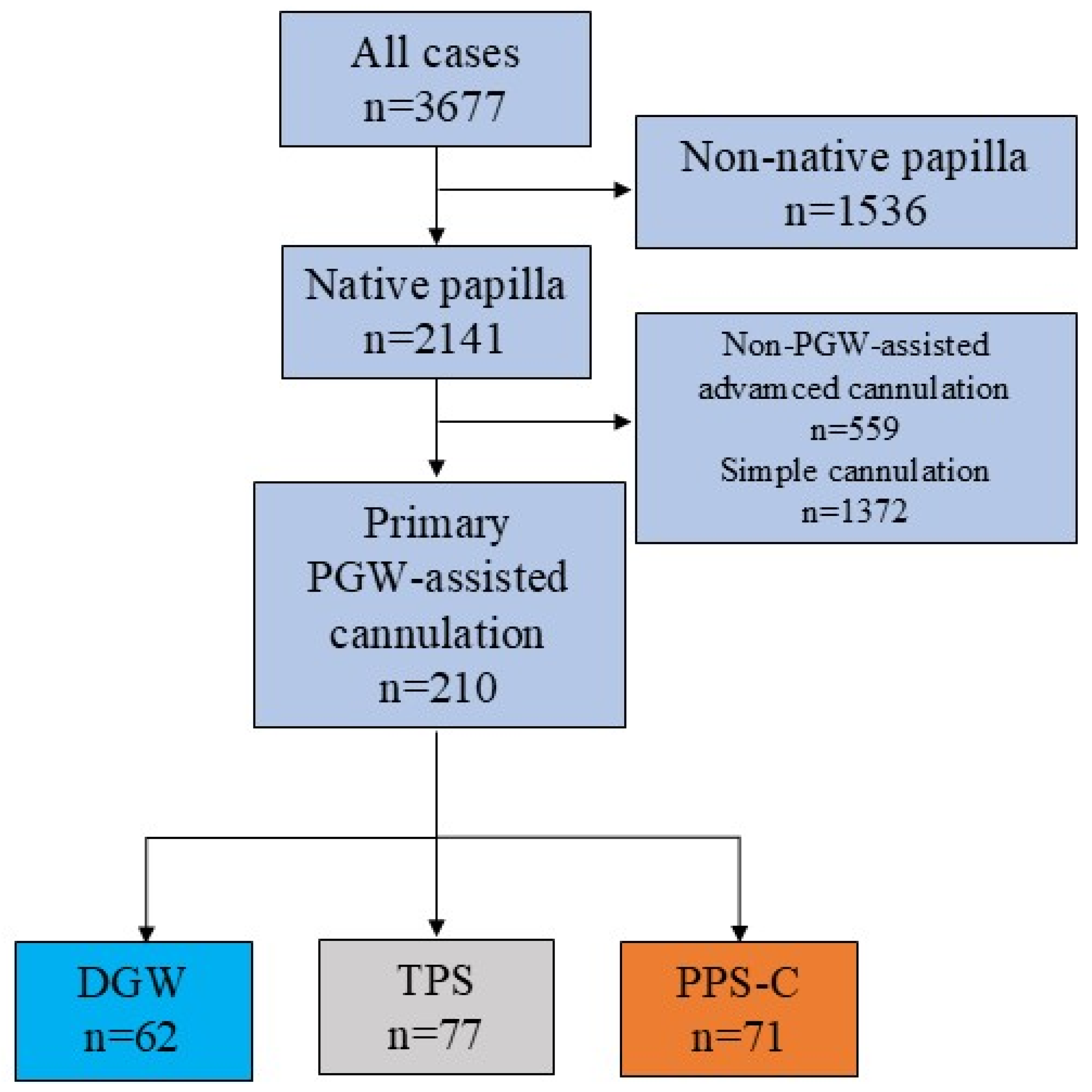
2.2. Inclusion and Exclusion Criteria
2.3. Definitions
2.4. Analyzed Dataset
2.5. Statistical Analysis
3. Results
3.1. General Characteristics of the Cohort
3.2. Indications of ERCP
3.3. Objective Grading of ERCP Difficulty
3.4. Biliary Cannulation Success Rates
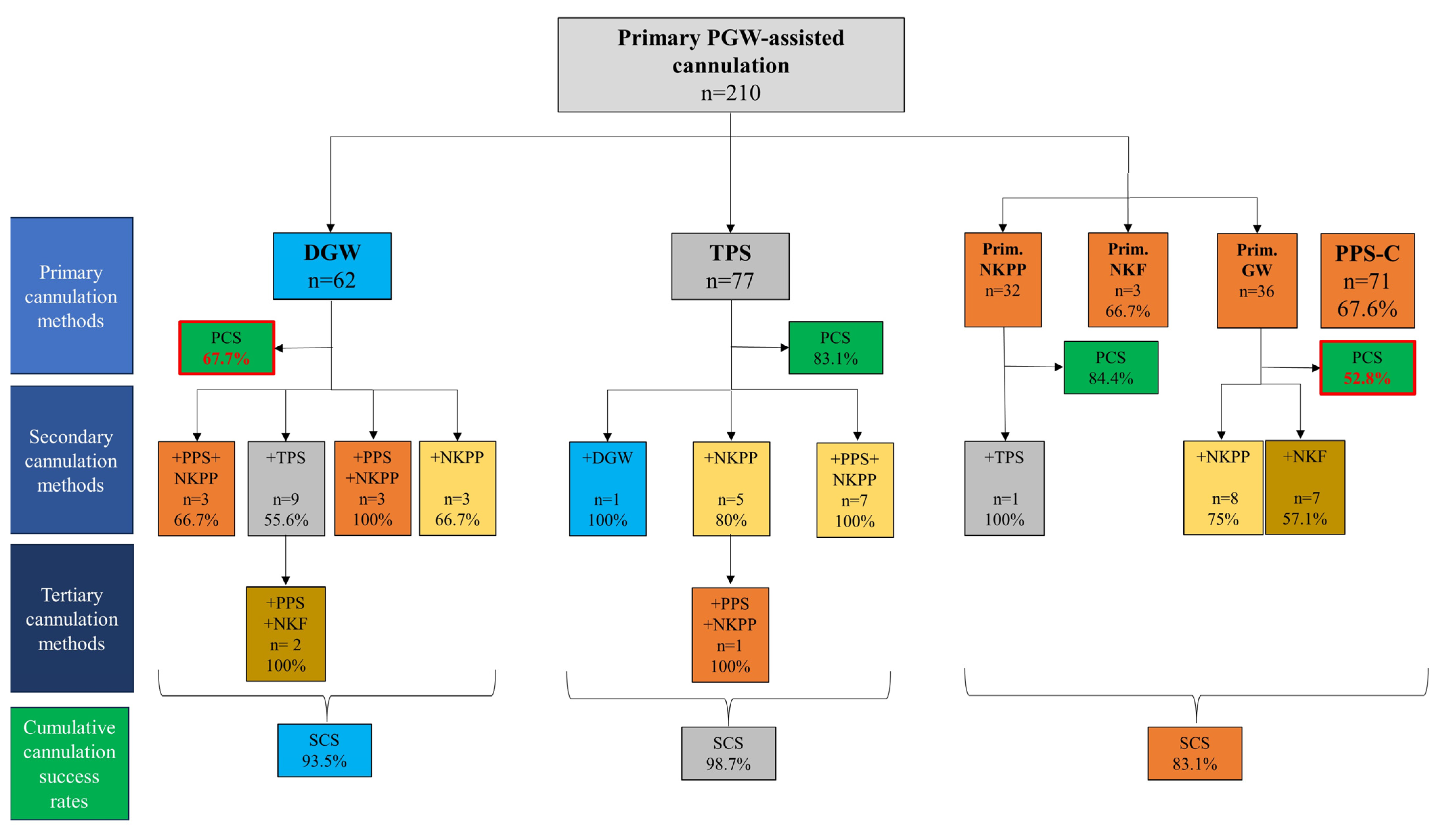
3.5. Salvage Advanced Cannulation Methods Used After Failed PGW-Assisted Cannulation
3.6. Adverse Event Rates
3.7. Post-ERCP Pancreatitis Prophylaxis
3.8. Cannulation and Fluoroscopy Times
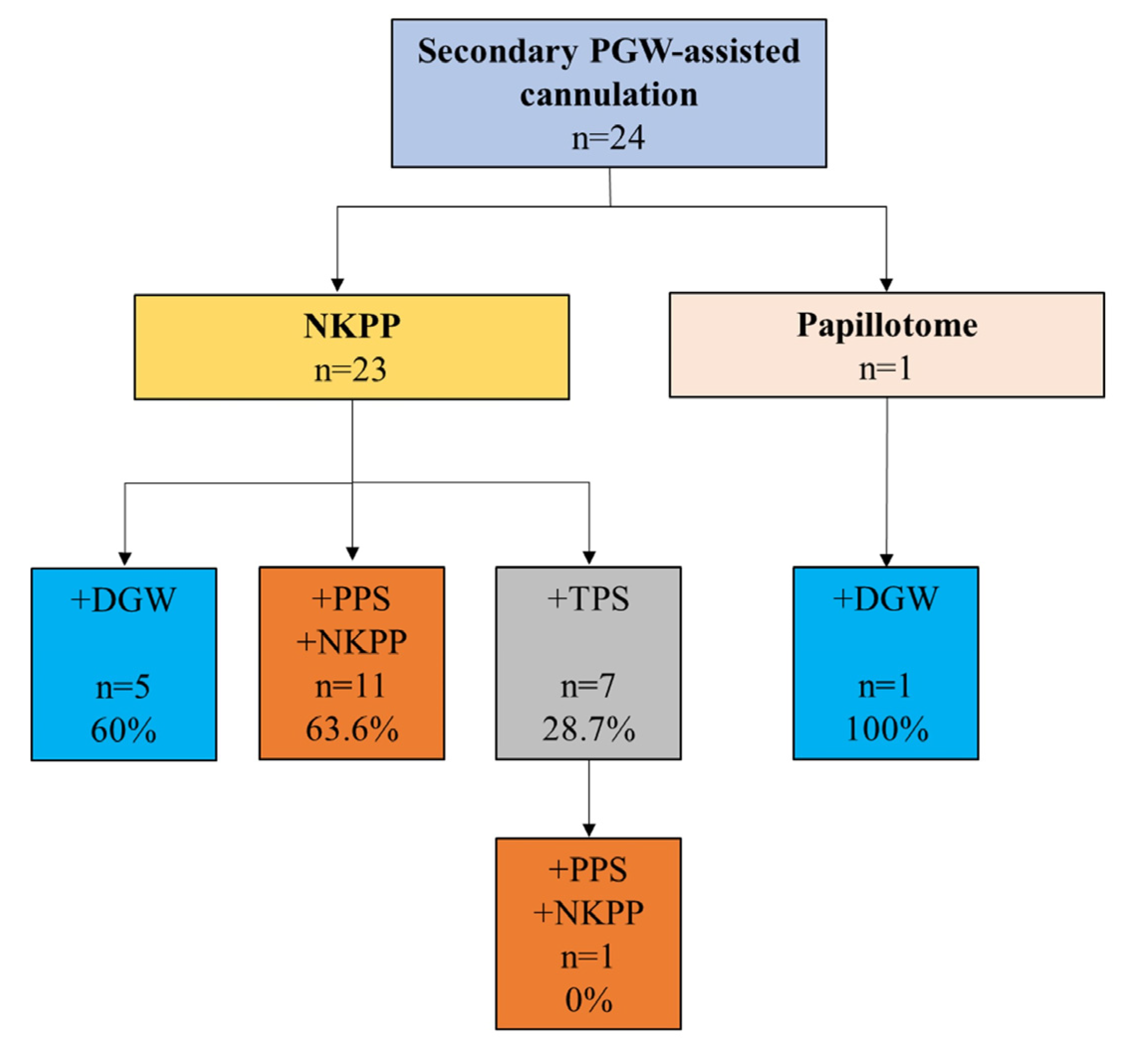
3.9. PGW-Assisted Cannulation Methods as Salvage Advanced Cannulation Techniques
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Practice and Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ABP | acute biliary pancreatitis |
| ASA | American Society of Anesthesiologists |
| ASGE | American Society of Gastrointestinal Endoscopy |
| DGW | double-guidewire technique |
| ERCP | endoscopic retrograde cholangiopancreatography |
| ESGE | European Society of Gastrointestinal Endoscopy |
| IQR | interquartile range |
| NKPP | needle-knife papillotomy |
| PEP | post-ERCP pancreatitis |
| PGW | pancreatic guidewire |
| PPS-C | prophylactic pancreatic stent-assisted cannulation |
| SD | standard deviation |
| TPS | transpancreatic sphincterotomy |
References
- Testoni, P.A.; Mariani, A.; Aabakken, L.; Arvanitakis, M.; Bories, E.; Costamagna, G.; Devière, J.; Dinis-Ribeiro, M.; Dumonceau, J.-M.; Giovannini, M.; et al. Papillary Cannulation and Sphincterotomy Techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016, 48, 657–683. [Google Scholar] [CrossRef]
- Berry, R.; Han, J.Y.; Tabibian, J.H. Difficult Biliary Cannulation: Historical Perspective, Practical Updates, and Guide for the Endoscopist. World J. Gastrointest. Endosc. 2019, 11, 5–21. [Google Scholar] [CrossRef] [PubMed]
- Gyökeres, T.; Duhl, J.; Varsányi, M.; Schwab, R.; Burai, M.; Pap, A. Double Guide Wire Placement for Endoscopic Pancreaticobiliary Procedures. Endoscopy 2003, 35, 95–96. [Google Scholar] [CrossRef] [PubMed]
- Goff, J.S. Long-Term Experience with the Transpancreatic Sphincter Pre-Cut Approach to Biliary Sphincterotomy. Gastrointest. Endosc. 1999, 50, 642–645. [Google Scholar] [CrossRef] [PubMed]
- Coté, G.A.; Mullady, D.K.; Jonnalagadda, S.S.; Keswani, R.N.; Wani, S.B.; Hovis, C.E.; Ammar, T.; Al-Lehibi, A.; Edmundowicz, S.A.; Komanduri, S.; et al. Use of a Pancreatic Duct Stent or Guidewire Facilitates Bile Duct Access with Low Rates of Precut Sphincterotomy: A Randomized Clinical Trial. Dig. Dis. Sci. 2012, 57, 3271–3278. [Google Scholar] [CrossRef]
- Pécsi, D.; Farkas, N.; Hegyi, P.; Varjú, P.; Szakács, Z.; Fábián, A.; Varga, G.; Rakonczay, Z.; Bálint, E.R.; Erőss, B.; et al. Transpancreatic Sphincterotomy Is Effective and Safe in Expert Hands on the Short Term. Dig. Dis. Sci. 2019, 64, 2429–2444. [Google Scholar] [CrossRef]
- Pécsi, D.; Farkas, N.; Hegyi, P.; Balaskó, M.; Czimmer, J.; Garami, A.; Illés, A.; Mosztbacher, D.; Pár, G.; Párniczky, A.; et al. Transpancreatic Sphincterotomy Has a Higher Cannulation Success Rate than Needle-Knife Precut Papillotomy—A Meta-Analysis. Endoscopy 2017, 49, 874–887. [Google Scholar] [CrossRef]
- Facciorusso, A.; Ramai, D.; Gkolfakis, P.; Khan, S.R.; Papanikolaou, I.S.; Triantafyllou, K.; Tringali, A.; Chandan, S.; Mohan, B.P.; Adler, D.G. Comparative Efficacy of Different Methods for Difficult Biliary Cannulation in ERCP: Systematic Review and Network Meta-Analysis. Gastrointest. Endosc. 2022, 95, 60–71.e12. [Google Scholar] [CrossRef]
- Sugiyama, H.; Tsuyuguchi, T.; Sakai, Y.; Mikata, R.; Yasui, S.; Watanabe, Y.; Sakamoto, D.; Nakamura, M.; Nishikawa, T. Transpancreatic Precut Papillotomy versus Double-Guidewire Technique in Difficult Biliary Cannulation: Prospective Randomized Study. Endoscopy 2018, 50, 33–39. [Google Scholar] [CrossRef]
- Kylänpää, L.; Koskensalo, V.; Saarela, A.; Ejstrud, P.; Udd, M.; Lindström, O.; Rainio, M.; Tenca, A.; Halttunen, J.; Qvigstad, G.; et al. Transpancreatic Biliary Sphincterotomy versus Double Guidewire in Difficult Biliary Cannulation: A Randomized Controlled Trial. Endoscopy 2021, 53, 1011–1019. [Google Scholar] [CrossRef]
- Pécsi, D.; Hegyi, P.; Szentesi, A.; Gódi, S.; Pakodi, F.; Vincze, Á. [The role of endoscopy registries in quality health care. The first data from the Hungarian Endoscopic Retrograde Cholangiopancreatography (ERCP) Registry]. Orv. Hetil. 2018, 159, 1506–1515. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Dumonceau, J.-M.; Kapral, C.; Aabakken, L.; Papanikolaou, I.S.; Tringali, A.; Vanbiervliet, G.; Beyna, T.; Dinis-Ribeiro, M.; Hritz, I.; Mariani, A.; et al. ERCP-Related Adverse Events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2020, 52, 127–149. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekhara, V.; Khashab, M.A.; Muthusamy, V.R.; Acosta, R.D.; Agrawal, D.; Bruining, D.H.; Eloubeidi, M.A.; Fanelli, R.D.; Faulx, A.L.; Gurudu, S.R.; et al. Adverse Events Associated with ERCP. Gastrointest. Endosc. 2017, 85, 32–47. [Google Scholar] [CrossRef]
- Cotton, P.B.; Eisen, G.; Romagnuolo, J.; Vargo, J.; Baron, T.; Tarnasky, P.; Schutz, S.; Jacobson, B.; Bott, C.; Petersen, B. Grading the Complexity of Endoscopic Procedures: Results of an ASGE Working Party. Gastrointest. Endosc. 2011, 73, 868–874. [Google Scholar] [CrossRef]
- Martin, J.A. Transpancreatic Sphincterotomy: “I Don’t Get No Respect. ” Dig. Dis. Sci. 2021, 66, 657–659. [Google Scholar] [CrossRef]
- Barakat, M.T.; Girotra, M.; Huang, R.J.; Choudhary, A.; Thosani, N.C.; Kothari, S.; Sethi, S.; Banerjee, S. Goff Septotomy Is a Safe and Effective Salvage Biliary Access Technique Following Failed Cannulation at ERCP. Dig. Dis. Sci. 2021, 66, 866–872. [Google Scholar] [CrossRef]
- Sadeghi, A.; Arabpour, E.; Rastegar, R.; Hosseinzadeh, E.; Tape, P.M.K.; Zali, M.R. Pancreatic Guidewire-Assisted Fistulotomy versus Transpancreatic Biliary Sphincterotomy in Difficult Biliary Cannulation with Unintentional Pancreatic Duct Cannulation: A Randomized Clinical Trial. Indian J. Gastroenterol. Off. J. Indian Soc. Gastroenterol. 2025. [Google Scholar] [CrossRef]
- Tse, F.; Yuan, Y.; Moayyedi, P.; Leontiadis, G.I.; Barkun, A.N. Double-Guidewire Technique in Difficult Biliary Cannulation for the Prevention of Post-ERCP Pancreatitis: A Systematic Review and Meta-Analysis. Endoscopy 2017, 49, 15–26. [Google Scholar] [CrossRef]
- Han, S.; Zhang, J.; Durkalski-Mauldin, V.; Foster, L.D.; Serrano, J.; Coté, G.A.; Bang, J.Y.; Varadarajulu, S.; Singh, V.K.; Khashab, M.; et al. Impact of Difficult Biliary Cannulation on Post-ERCP Pancreatitis: Secondary Analysis of the Stent versus Indomethacin Trial Dataset. Gastrointest. Endosc. 2025, 101, 617–628. [Google Scholar] [CrossRef]
- Pécsi, D.; Gódi, S.; Hegyi, P.; Hanák, L.; Szentesi, A.; Altorjay, I.; Bakucz, T.; Czakó, L.; Kovács, G.; Orbán-Szilágyi, Á.; et al. ERCP Is More Challenging in Cases of Acute Biliary Pancreatitis than in Acute Cholangitis—Analysis of the Hungarian ERCP Registry Data. Pancreatol. Off. J. Int. Assoc. Pancreatol. IAP Al 2021, 21, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Dubravcsik, Z.; Szepes, A.; Hritz, I.; Madácsy, L. Small-Caliber Rescue Pancreatic Stenting for Severe Post-ERCP Pancreatitis: A Useful Tool to Pull the Pancreas out of the Fire. Endoscopy 2015, 47, 467–468. [Google Scholar] [CrossRef] [PubMed]
- Dubravcsik, Z.; Madácsy, L.; Gyökeres, T.; Vincze, Á.; Szepes, Z.; Hegyi, P.; Hritz, I.; Szepes, A. Hungarian Pancreatic Study Group Preventive Pancreatic Stents in the Management of Acute Biliary Pancreatitis (PREPAST Trial): Pre-Study Protocol for a Multicenter, Prospective, Randomized, Interventional, Controlled Trial. Pancreatol. Off. J. Int. Assoc. Pancreatol. IAP Al 2015, 15, 115–123. [Google Scholar] [CrossRef]
- Guzmán-Calderón, E.; Martinez-Moreno, B.; Casellas, J.A.; Aparicio, J.R. Transpancreatic Precut Papillotomy versus Double-Guidewire Technique in Difficult Biliary Cannulation: A Systematic Review and Meta-Analysis. Endosc. Int. Open 2021, 9, E1758–E1767. [Google Scholar] [CrossRef]
- Su, W.-C.; Wang, C.-C.; Hsiao, T.-H.; Chen, H.-D.; Chen, J.-H. The Impact of Transpancreatic Precut Sphincterotomy on the Quality of ERCP in a Low-Volume Setting. Gastrointest. Endosc. 2024, 99, 747–755. [Google Scholar] [CrossRef]
- Koskensalo, V.; Udd, M.; Rainio, M.; Halttunen, J.; Sipilä, M.; Lindström, O.; Kylänpää, L. Transpancreatic Biliary Sphincterotomy for Biliary Access Is Safe Also on a Long-Term Scale. Surg. Endosc. 2021, 35, 104–112. [Google Scholar] [CrossRef]
- Chen, Y.-P.; Liao, Y.-J.; Peng, Y.-C.; Tung, C.-F.; Tsai, H.-J.; Yang, S.-S.; Chen, C.-C. Impact of Duodenal Papilla Morphology on the Success of Transpancreatic Precut Sphincterotomy. J. Clin. Med. 2024, 13, 6940. [Google Scholar] [CrossRef]
- Angsuwatcharakon, P.; Thongsuwan, C.; Ridtitid, W.; Piyachaturawat, P.; Kulpatcharapong, S.; Kongkam, P.; Rerknimitr, R. Morphology of the Major Duodenal Papilla for the Selection of Advanced Cannulation Techniques in Difficult Biliary Cannulation. Surg. Endosc. 2023, 37, 5807–5815. [Google Scholar] [CrossRef]
| Primary Cannulation Method | TPS (n = 77) | DGW (n = 62) | PPS-C (n = 71) | p-Value |
|---|---|---|---|---|
| Primary cannulation success rate | 64 (83.1%) | 42 (67.7%) | 48 (67.6%) | <0.001 |
| Secondary cannulation success rate | 76 (98.7%) | 58 (93.5%) | 59 (83.1%) | 0.006 |
| TPS (n = 77) | DGW (n = 62) | PPS-C (n = 71) | p-Value | |
|---|---|---|---|---|
| Post-ERCP pancreatitis (ABP cases excluded) | 3/59 (5.0%) | 3/54 (5.6%) | 2/51 (3.9%) | 0.923 |
| Clinically significant bleeding | 1 (1.3%) | 0 (0.0%) | 2 (2.8%) | 0.838 |
| Immediate bleeding | 8 (11%) | 12 (19.4%) | 15 (21.1%) | 0.184 |
| Perforation | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | N/A |
| Cholangitis | 1 (1.3%) | 0 (0.0%) | 3 (4.2%) | 0.267 |
| Cholecystitis | 0 (0.0%) | 1 (1.6%) | 0 (0.0%) | 0.293 |
| TPS (n = 77) | DGW (n = 62) | PPS-C (n = 71) | p-Value | |
|---|---|---|---|---|
| Indomethacin suppository use | 41 (53.2%) | 58 (93.5%) | 24 (33.8%) | <0.001 |
| PPS use | 47 (61.0%) | 35 (56.5%) | 71 (100.0%) | <0.001 |
| No PEP prophylaxis used | 25 (32.5%) | 0 (0%) | 0 (0%) | <0.001 |
| Post-ERCP Pancreatitis Cases by Groups | n | PPS | Indomethacin Suppository | |
|---|---|---|---|---|
| Primary PGW-assisted groups | DGW | 3 | 0/3 (0%) | 3/3 (100%) |
| PPS + GW | 1 | 1/1 (100%) | 1/1 (100%) | |
| PPS + NKPP | 1 | 1/1 (100%) | 0/1 (0%) | |
| TPS | 2 | 1/2 (50%) | 0/2 (0%) | |
| TPS + DGW | 1 | 0/1 (0%) | 0/1 (0%) | |
| Salvage PGW-assisted groups | NKPP + TPS | 1 | 0/1 (0%) | 1/1 (100%) |
| NKPP + PPS + NKPP | 1 | 1/1 (100%) | 1/1 (100%) | |
| TPS (n = 77) | DGW (n = 62) | PPS-C (n = 71) | p-Value | |
|---|---|---|---|---|
| Cannulation time (median—IQR) in seconds | 420 (120, 627) | 335 (240, 602) | 300 (120, 606) | 0.179 |
| Fluoroscopy time (median—IQR) in seconds | 100 (80, 143) | 185 (108, 256) | 110 (65, 172) | 0.047 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pécsi, D.; Farkas, N.; Gódi, S.; Hegyi, P.; Szentesi, A.; Altorjay, I.; Bakucz, T.; Orbán-Szilágyi, Á.; Szepes, Z.; Czakó, L.; et al. Transpancreatic Sphincterotomy Is a Safe and Effective Pancreatic Guidewire-Assisted Cannulation Method: Real-World Data Analysis of the Hungarian ERCP Registry. J. Clin. Med. 2025, 14, 7118. https://doi.org/10.3390/jcm14197118
Pécsi D, Farkas N, Gódi S, Hegyi P, Szentesi A, Altorjay I, Bakucz T, Orbán-Szilágyi Á, Szepes Z, Czakó L, et al. Transpancreatic Sphincterotomy Is a Safe and Effective Pancreatic Guidewire-Assisted Cannulation Method: Real-World Data Analysis of the Hungarian ERCP Registry. Journal of Clinical Medicine. 2025; 14(19):7118. https://doi.org/10.3390/jcm14197118
Chicago/Turabian StylePécsi, Dániel, Nelli Farkas, Szilárd Gódi, Péter Hegyi, Andrea Szentesi, István Altorjay, Tamás Bakucz, Ákos Orbán-Szilágyi, Zoltán Szepes, László Czakó, and et al. 2025. "Transpancreatic Sphincterotomy Is a Safe and Effective Pancreatic Guidewire-Assisted Cannulation Method: Real-World Data Analysis of the Hungarian ERCP Registry" Journal of Clinical Medicine 14, no. 19: 7118. https://doi.org/10.3390/jcm14197118
APA StylePécsi, D., Farkas, N., Gódi, S., Hegyi, P., Szentesi, A., Altorjay, I., Bakucz, T., Orbán-Szilágyi, Á., Szepes, Z., Czakó, L., Patai, Á., Gyökeres, T., Fejes, R., Dubravcsik, Z., & Vincze, Á. (2025). Transpancreatic Sphincterotomy Is a Safe and Effective Pancreatic Guidewire-Assisted Cannulation Method: Real-World Data Analysis of the Hungarian ERCP Registry. Journal of Clinical Medicine, 14(19), 7118. https://doi.org/10.3390/jcm14197118








