The Impact of Virtual-Reality-Based Physiotherapy on Upper Limb Function in Children with Cerebral Palsy
Abstract
1. Introduction
2. Materials and Methods
2.1. Databases and Search Strategy
- PubMed/MEDLINE;
- ScienceDirect;
- Scopus;
- Web of Science;
- ResearchGate;
- Google Scholar.
- “cerebral palsy” or “spastic hemiplegia”;
- “virtual reality” or “VR therapy”;
- “upper limb” or “upper extremity” or “hand function”;
- “rehabilitation” or “physiotherapy”;
- “children” or “pediatrics”.
2.2. Inclusion Criteria
- Availability of full text;
- Language of publication: Polish or English;
- Population: children under 18 with clinically diagnosed cerebral palsy (any type);
- Intervention: physiotherapy/rehabilitation using virtual reality;
- Therapy goal: improvement of upper limb or hand function—muscle strength, range of movement, coordination;
- Type of study: randomized controlled trials (RCTs), quasi-experimental or prospective studies with a control group.
2.3. Exclusion Criteria
- Studies involving only adults;
- Studies involving only the lower limb;
- Studies without the use of virtual reality, e.g., robotics, classic physiotherapy;
- Single case reports or case series;
- Expert opinions without quantitative data and narrative reviews.
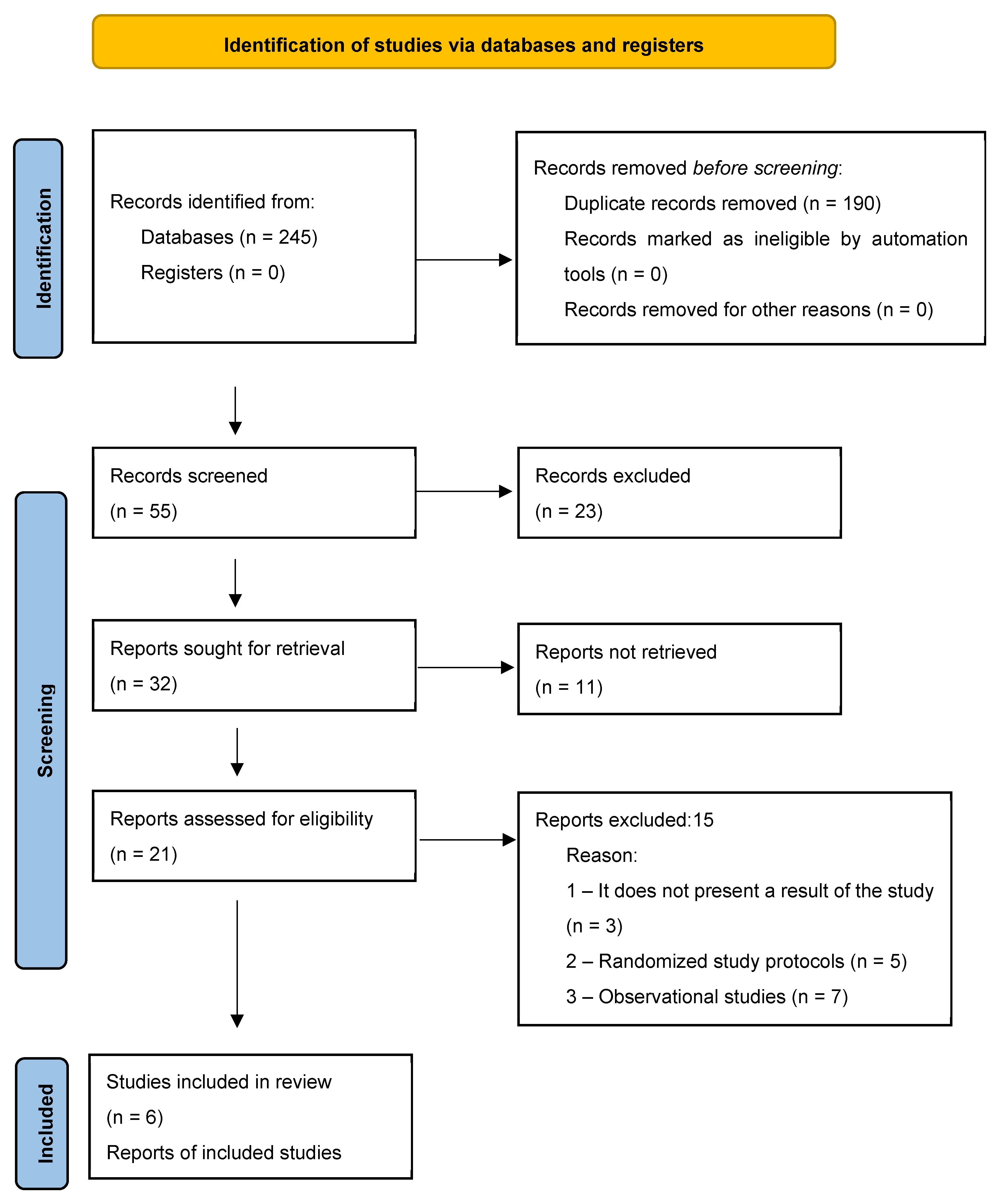
2.4. Selection Process
2.5. Data Extraction and Analysis
2.6. Quality Assessment and Risk Bias
2.6.1. Assessment Results
- Randomization and allocation concealment: In all studies, the randomization process was described; however, detailed information regarding the generation of the random sequence and allocation concealment was incomplete, resulting in a judgment of moderate risk of bias.
- Blinding: None of the studies implemented full blinding of participants or therapists, which increases the risk of placebo effects and subjective outcome assessment (moderate to high risk of bias).
- Completeness of data: Most studies reported complete outcome data; however, due to the small sample sizes (10–41 participants), even minimal dropout could have influenced the results (moderate risk of bias).
- Selective reporting: No clear evidence of selective reporting was identified; nevertheless, the absence of preregistered protocols limited the certainty of this assessment (low to moderate risk of bias).
- Other sources of bias: The main limitation was the heterogeneity of interventions (different VR systems, duration and frequency of sessions), which hinders comparability of results and may introduce confounding.
2.6.2. Summary
3. Results
3.1. Characteristics of the Included Studies
3.2. Type of Interventions
- Classic VR therapeutic protocols with interactive biofeedback [24];
- VR task-oriented training with fine motor elements [25];
- Gamified VR with motivational educational apps [26];
- Immersive VR therapy based on 3D environments with motion control [27];
- In-home VR therapy supported by sensors and remote monitoring [28].
3.3. Assessment Tools and Results
- Assisting Hand Assessment (AHA);
- Quality of Upper Extremity Skills Test (QUEST);
- ABILHAND-Kids;
- Melbourne Assessment 2 (MA2);
- Biomechanical measurements: ROM, grip strength, task time.
- Improved bilateral coordination;
- Increased movement precision;
| Authors (Year) | Assessment Tools | Results and Effects | |
|---|---|---|---|
| 1 | Menekseoglu et al. (2023) [15] | Assisting Hand Assessment (AHA), ABILHAND-Kids, Quality of Upper Extremity Skills Test (QUEST), KINDL and active range of motion. |
|
| 2 | Choi et al. (2023) [16] | Melbourne Assessment of Unilateral Upper Limb Function v2 (MA2), ULPRS, PEDI-CAT, 3D movement analysis, satisfaction questionnaires. |
|
| 3 | Goyal et al. (2022) [17] | ABILHAND-Kids, WeeFIM, 9HPT, BBT |
|
| 4 | Metin Ökmen et al. (2019) [18] | Bimanual Fine Motor Function (BFMF), FMS |
|
| 5 | Daliri et al. (2025) [19] | Spoon use time—daily activity, knife use time—daily activity, range of motion (ROM) and grip strength. |
|
| 6 | Saussez et al. (2023) [20] | Assisting Hand Assessment (AHA), BBT-MA, BBT-LA, JTTHF-MA hand, JTTHF-LA hand, MFPT-MA hand, MFPT-LA hand, 6MWT, ABILHAND-Kids, ACTIVLIM-CP, PEDI, ABILOCO-Kids, COPM perf, COPM sat |
|
| 7 | Baillet et al. (2024) [21] | Movement Assessment Battery for Children 2 (MABC-2), range of motion (ROM) assessment, |
|
| 8 | Avcil et al. (2021) [22] | Minnesota Manual Dexterity Test (MMDT), Childhood Health Assessment Questionnaire (CHAQ), Duruoz Hand Index (DHI), dynamometer. |
|
| 9 | Golomb et al. (2010) [23] | Assessment of finger range of motion (ROM) using a sensor glove, dual-energy X-ray absorptiometry (DXA), peripheral quantitative computed tomography (pQCT) and functional magnetic resonance imaging (MRI). |
|
3.4. Heterogeneity and Limitations
4. Discussion
5. Conclusions
- Virtual reality has a positive effect on neuroplasticity in children with cerebral palsy by activating multi-level brain pathways responsible for movement planning and control.
- VR therapy can be a safe and effective tool to support traditional physiotherapy approaches in children with cerebral palsy, particularly in improving muscle strength, range of motion, coordination and grip.
- Virtual reality is beneficial for patients with mild to moderate impairments (GMFCS I–III), while patients with more severe impairments require integration with assistive technologies (exoskeletons, robotics).
- Remote therapy using VR can be a valuable alternative for families with limited access to specialist care.
- Both immersive and non-immersive systems have therapeutic potential, but their selection should be tailored to the individual sensory and motor profile of the child.
- Large-scale randomized clinical trials with long-term follow-up and clearly defined treatment protocols are necessary.
- It is recommended to use standardized tools for assessing upper limb function (AHA, MA2, QUEST) and to analyze secondary effects (PEDI-CAT, quality of life).
- There is evidence of the transfer of skills developed in a virtual reality environment to the activities of daily living. However, this evidence is inconclusive and requires confirmation in further scientific research.
- The mechanisms of virtual reality effectiveness include: active patient participation, an engaging multisensory environment, increased repetition and intensification of exercises.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child. Neurol. Suppl. 2007, 109, 8–14. [Google Scholar] [PubMed]
- Himmelmann, K.; Uvebrant, P. The panorama of cerebral palsy in Sweden. Part XI. Changing patterns in the birth-year period 2003–2006. Acta Paediatr. 2014, 103, 618–624. [Google Scholar] [CrossRef]
- Pakula, A.T.; Van Naarden Braun, K.; Yeargin-Allsopp, M. Cerebral palsy: Classification and epidemiology. Phys. Med. Rehabil. Clin. N. Am. 2009, 20, 425–452. [Google Scholar] [CrossRef] [PubMed]
- Oskoui, M.; Coutinho, F.; Dykeman, J.; Jetté, N.; Pringsheim, T. An update on the prevalence of cerebral palsy: A systematic review and meta-analysis. Dev. Med. Child. Neurol. 2013, 55, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Odding, E.; Roebroeck, M.E.; Stam, H.J. The epidemiology of cerebral palsy: Incidence, impairments and risk factors. Disabil. Rehabil. 2006, 28, 183–191. [Google Scholar] [CrossRef]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Valentine, J.; Walker, K.; White, R.; Badawi, N.; et al. Early, accurate diagnosis and early intervention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef]
- Eliasson, A.C.; Krumlinde-Sundholm, L.; Rösblad, B.; Beckung, E.; Arner, M.; Ohrvall, A.M.; Rosenbaum, P. The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Dev. Med. Child. Neurol. 2006, 48, 549–554. [Google Scholar] [CrossRef]
- Novak, I.; Morgan, C.; Fahey, M.; Finch-Edmondson, M.; Galea, C.; Hines, A.; Langdon, K.; Mc Namara, M.; Paton, M.C.; Popat, H.; et al. State of the evidence traffic lights 2019: Systematic review of interventions for preventing and treating children with cerebral palsy. Curr. Neurol. Neurosci. Rep. 2020, 20, 3. [Google Scholar] [CrossRef]
- Ravi, D.K.; Kumar, N.; Singhi, P. Effectiveness of virtual reality rehabilitation for children and adolescents with cerebral palsy: An updated evidence-based systematic review. Physiotherapy 2017, 103, 245–258. [Google Scholar] [CrossRef]
- Levin, M.F.; Weiss, P.L.; Keshner, E.A. Emergence of virtual reality as a tool for upper limb rehabilitation: Incorporation of motor control and motor learning principles. Phys. Ther. 2015, 95, 415–425. [Google Scholar] [CrossRef]
- Howard, M.C. A meta-analysis and systematic literature review of virtual reality rehabilitation programs. Comput. Human. Behav. 2017, 70, 317–327. [Google Scholar] [CrossRef]
- Chen, Y.P.; Lee, S.Y.; Howard, A.M. Effect of virtual reality on upper extremity function in children with cerebral palsy: A meta-analysis. Pediatr. Phys. Ther. 2014, 26, 289–300. [Google Scholar] [CrossRef]
- Alrashidi, M.; Wadey, C.A.; Tomlinson, R.J.; Buckingham, G.; Williams, C.A. The efficacy of virtual reality interventions compared with conventional physiotherapy in improving the upper limb motor function of children with cerebral palsy: A systematic review of randomised controlled trials. Disabil. Rehabil. 2023, 45, 1773–1783. [Google Scholar] [CrossRef] [PubMed]
- Fandim, J.V.; Saragiotto, B.T.; Porfírio, G.J.M.; Santana, R.F. Effectiveness of virtual reality in children and young adults with cerebral palsy: A systematic review of randomized controlled trials. Braz. J. Phys. Ther. 2021, 25, 369–386. [Google Scholar] [CrossRef] [PubMed]
- Menekseoglu, A.K.; Capan, N.; Arman, S.; Aydin, A.R. Effect of a Virtual Reality-Mediated Gamified Rehabilitation Program on Upper Limb Functions in Children with Hemiplegic Cerebral Palsy: A Prospective, Randomized Controlled Study. Am. J. Phys. Med. Rehabil. 2023, 102, 198–205. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Yi, S.H.; Ao, L.; Yoo, B.; Park, E.S.; Rha, D.-W. Home-based virtual reality-enhanced upper limb training system in children with brain injury: A randomized controlled trial. Front. Pediatr. 2023, 11, 1131573. [Google Scholar] [CrossRef]
- Goyal, C.; Vardhan, V.; Naqvi, W. Non-Immersive Virtual Reality as an Intervention for Improving Hand Function and Functional Independence in Children with Unilateral Cerebral Palsy: A Feasibility Study. Cureus 2022, 14, e26085. [Google Scholar] [CrossRef]
- Metin Ökmen, B.; Doğan Aslan, M.; Nakipoğlu Yüzer, G.F.; Özgirgin, N. Effect of virtual reality therapy on functional development in children with cerebral palsy: A single-blind, prospective, randomized-controlled study. Turk. J. Phys. Med. Rehabil. 2019, 65, 371–378. [Google Scholar] [CrossRef]
- Daliri, M.; Salehi Nasab, F.; Fatorehchy, S.; Farzad, M.; Moradi, A. Impact of Virtual Reality Task-Oriented Training on Upper Extremity Motor Function in Children with Cerebral Palsy: A Randomised Controlled Trial. Pediatr. Neurol. 2025, 163, 85–92. [Google Scholar] [CrossRef]
- Saussez, G.; Bailly, R.; Araneda, R.; Paradis, J.; Ebner-Karestinos, D.; Klöcker, A.; Sogbossi, E.S.; Riquelme, I.; Brochard, S.; Bleyenheuft, Y. Efficacy of integrating a semi-immersive virtual device in the HABIT-ILE intervention for children with unilateral cerebral palsy: A non-inferiority randomized controlled trial. J. Neuroeng. Rehabil. 2023, 20, 98. [Google Scholar] [CrossRef]
- Burin-Chu, S.; Baillet, H.; Leconte, P.; Lejeune, L.; Thouvarecq, R.; Benguigui, N. Effectiveness of virtual reality interventions of the upper limb in children and young adults with cerebral palsy: A systematic review with meta-analysis. Clin. Rehabil. 2024, 38, 15–33. [Google Scholar] [CrossRef] [PubMed]
- Avcil, E.; Tarakci, D.; Arman, N.; Tarakci, E. Upper extremity rehabilitation using Leap Motion controller for children with hemiplegic cerebral palsy: A randomized controlled trial. J. Hand Ther. 2021, 34, 234–241. [Google Scholar]
- Golomb, M.R.; McDonald, B.C.; Warden, S.J.; Yonkman, J.; Saykin, A.J.; Shirley, B.; Huber, M.; Rabin, B.; AbdelBaky, M.; Warner, J.; et al. In-home virtual reality videogame telerehabilitation in adolescents with hemiplegic cerebral palsy. Arch. Phys. Med. Rehabil. 2010, 91, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Liu, N.; Liu, S.; Gao, Y. Effects of nonimmersive virtual reality intervention on children with spastic cerebral palsy: A meta-analysis and systematic review. Am. J. Phys. Med. Rehabil. 2023, 102, 1130–1138. [Google Scholar] [CrossRef]
- Liu, W.; Hu, Y.; Li, J.; Chang, J. Effect of virtual reality on balance function in children with cerebral palsy: A systematic review and meta-analysis. Front. Public Health 2022, 10, 865474. [Google Scholar] [CrossRef]
- Chang, H.J.; Ku, K.H.; Park, Y.S.; Park, J.G.; Cho, E.S.; Seo, J.S.; Kim, C.W.; Se Hwi, O. Effects of virtual reality-based rehabilitation on upper extremity function among children with cerebral palsy. Healthcare 2020, 8, 391. [Google Scholar] [CrossRef]
- Bell, J.; Decker, B.; Eichmann, A.; Palkovich, C.; Reji, C. Effectiveness of virtual reality for upper extremity function and motor performance of children with cerebral palsy: A systematic review. Am. J. Occup. Ther. 2024, 78, 7802180180. [Google Scholar] [CrossRef]
- Jha, R.; Singh, A.; Ranjan, R.; Karthikbabu, S. Virtual reality gaming with physiotherapy improves balance in children with bilateral cerebral palsy: A randomized controlled trial. J. Pediatr. Rehabil. Med. 2021, 14, 213–220. [Google Scholar]
- You, S.H.; Jang, S.H.; Kim, Y.H.; Hallett, M.; Ahn, S.H.; Kwon, Y.H.; Lee, M.Y.; Kim, J.H. Virtual reality-induced cortical reorganization and associated locomotor recovery in chronic stroke: An experimenter-blind randomized study. Stroke 2005, 36, 1166–1171. [Google Scholar] [CrossRef]
- Tobaiqi, M.A.; Albadawi, E.A.; Fadlalmola, H.A.; Albadrani, M.S. Application of Virtual Reality-Assisted Exergaming on the Rehabilitation of Children with Cerebral Palsy: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 7091. [Google Scholar] [CrossRef]
- Mezaraupa, M.; Jamonte, L. i Ceire, Ureality as a training tool impact on upper extremity function in children with cerebral palsy: A systematic review. Educ. Inf. Technol. 2024, 29, 7937. [Google Scholar]
- Levac, D.; Huber, M.E.; Sternad, D. Learning and transfer of complex motor skills in virtual reality: A perspective review. J. Neuroeng. Rehabil. 2019, 16, 121. [Google Scholar] [CrossRef] [PubMed]
- Warnier, N.; Lambregts, S.; Van De Port, I. Effect of virtual reality therapy on balance and walking in children with cerebral palsy: A systematic review. Dev. Neurorehabil. 2020, 23, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.P.; Kang, L.-J.; Chuang, T.-Y.; Doong, J.-L.; Lee, S.-J.; Tsai, M.-W.; Jeng, S.-F.; Sung, W.-H. Use of virtual reality to improve upper-extremity control in children with cerebral palsy: A single-subject design. Phys. Ther. 2007, 87, 1441–1457. [Google Scholar] [CrossRef]
- Liu, C.; Wang, X.; Chen, R.; Zhang, J. The effects of virtual reality training on balance, gross motor function, and daily living ability in children with cerebral palsy: Systematic review and meta-analysis. JMIR Serious Games 2022, 10, e37910. [Google Scholar] [CrossRef] [PubMed]
- Proffitt, R.; Glegg, S.; Levac, D.; Lange, B. End-user involvement in rehabilitation virtual reality implementation research. J. Enabling Technol. 2019, 13, 65–75. [Google Scholar] [CrossRef]
- Levin, M.F.; Snir, O.; Liebermann, D.G.; Weingarden, H.; Weiss, P.L. Virtual reality versus conventional treatment of reaching ability in chronic stroke: Clinical feasibility study. Neurol. Ther. 2012, 1, 3. [Google Scholar] [CrossRef]
- Bleyenheuft, Y.; Gordon, A.M. Precision grip control, sensory impairments and their interactions in children with hemiplegic cerebral palsy: A systematic review. Res. Dev. Disabil. 2013, 34, 301–321. [Google Scholar] [CrossRef]
- Chen, Y.P.; Pope, S.; Tyler, D.; Warren, G.L. Effectiveness of constraint-induced movement therapy on upper-extremity function in children with cerebral palsy: A systematic review and meta-analysis of randomized controlled trials. Clin. Rehabil. 2014, 28, 939–953. [Google Scholar] [CrossRef]
- Chen, Y.P.; Howard, A.M. Effects of robotic therapy on upper-extremity function in children with cerebral palsy: A systematic review. Dev. Neurorehabil. 2016, 19, 64–71. [Google Scholar] [CrossRef]
- Bryanton, C.; Bosse, J.; Brien, M.; McLean, J.; McCormick, A.; Sveistrup, H. Feasibility, motivation, and selective motor control: Virtual reality compared to conventional home exercise in children with cerebral palsy. Cyberpsychol. Behav. 2006, 9, 123–128. [Google Scholar] [CrossRef]
- Fluet, G.G.; Qiu, Q.; Kelly, D.; Parikh, H.D.; Ramirez, D.; Saleh, S.; Adamovich, S.V. Interfacing a haptic robotic system with complex virtual environments to treat impaired upper extremity motor function in children with cerebral palsy. Dev. Neurorehabil. 2010, 13, 335–345. [Google Scholar] [CrossRef] [PubMed]
- Green, D.; Wilson, P.H. Use of virtual reality in rehabilitation of movement in children with hemiplegia—A multiple case study evaluation. Disabil. Rehabil. 2012, 34, 593–604. [Google Scholar] [CrossRef] [PubMed]
- Jannink, M.J.; van der Wilden, G.J.; Navis, D.W.; Visser, G.; Gussinklo, J.; Ijzerman, M. A low-cost video game applied for training of upper extremity function in children with cerebral palsy: A pilot study. Cyberpsychol. Behav. 2008, 11, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Lam-Damji, S.; Chau, T.; Fehlings, D. The development of a home-based virtual reality therapy system to promote upper extremity movement for children with hemiplegic cerebral palsy. Technol. Disabil. 2009, 21, 107–113. [Google Scholar] [CrossRef]
- Qiu, Q.; Ramirez, D.A.; Saleh, S.; Fluet, G.G.; Parikh, H.D.; Kelly, D.; Adamovich, S.V. The New Jersey Institute of Technology Robot-Assisted Virtual Rehabilitation (NJIT-RAVR) system for children with cerebral palsy: A feasibility study. J. Neuroeng. Rehabil. 2009, 6, 40. [Google Scholar] [CrossRef]
- Reid, D. The influence of virtual reality on playfulness in children with cerebral palsy: A pilot study. Occup. Ther. Int. 2004, 11, 131–144. [Google Scholar] [CrossRef]
- Reid, D.T. The use of virtual reality to improve upper-extremity efficiency skills in children with cerebral palsy: A pilot study. Technol. Disabil. 2002, 14, 53–61. [Google Scholar] [CrossRef]
- Reid, D.T.; Campbell, K. The use of virtual reality with children with cerebral palsy: A pilot randomized trial. Ther. Recreat. J. 2006, 40, 255–268. [Google Scholar]
| Authors (Year) | Study Type | Number of Participants | Age | CP Type | VR | Therapy Duration | |
|---|---|---|---|---|---|---|---|
| 1 | Menekseoglu et al. (2023) [15] | RCT | 36 | 6–12 years | hemiplegia | gamified VR | 6 weeks (3×/week) |
| 2 | Choi et al. (2023) [16] | RCT | 40 | 4–17 years | hemiplegia, diplegia | VR + IMU | 4 weeks (daily) |
| 3 | Goyal et al. (2022) [17] | RCT | 10 | 6–12 years | hemiplegia | VR + IMU | 6 weeks (daily) |
| 4 | Metin Ökmen et al. (2019) [18] | RCT | 41 | 5–15 years | hemiplegia | task-oriented VR | 4 weeks (3×/week) |
| 5 | Daliri et al. (2025) [19] | RCT | 30 | 6–10 years | hemiplegia | task-oriented VR | 8 weeks (2×/week) |
| 6 | Saussez et al. (2023) [20] | RCT | 40 | 5–18 years | hemiplegia | task-oriented VR | 8 weeks (2×/week) |
| 7 | Baillet et al. (2024) [21] | RCT | 20 | 6–12 years | hemiplegia | immersive 3D VR | 5 weeks (3×/week) |
| 8 | Avcil et al. (2021) [22] | RCT | 30 | 8–12 years | hemiplegia | leap Motion | 6 weeks |
| 9 | Golomb et al. (2010) [23] | RCT—in-home VR | 30 | 13–17 years | hemiplegia | VR + telerehabilitation | 6 weeks |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wojtowicz, Z.; Czech, K.; Lechowska, A.; Paprocka, J. The Impact of Virtual-Reality-Based Physiotherapy on Upper Limb Function in Children with Cerebral Palsy. J. Clin. Med. 2025, 14, 7040. https://doi.org/10.3390/jcm14197040
Wojtowicz Z, Czech K, Lechowska A, Paprocka J. The Impact of Virtual-Reality-Based Physiotherapy on Upper Limb Function in Children with Cerebral Palsy. Journal of Clinical Medicine. 2025; 14(19):7040. https://doi.org/10.3390/jcm14197040
Chicago/Turabian StyleWojtowicz, Zuzanna, Katarzyna Czech, Adrianna Lechowska, and Justyna Paprocka. 2025. "The Impact of Virtual-Reality-Based Physiotherapy on Upper Limb Function in Children with Cerebral Palsy" Journal of Clinical Medicine 14, no. 19: 7040. https://doi.org/10.3390/jcm14197040
APA StyleWojtowicz, Z., Czech, K., Lechowska, A., & Paprocka, J. (2025). The Impact of Virtual-Reality-Based Physiotherapy on Upper Limb Function in Children with Cerebral Palsy. Journal of Clinical Medicine, 14(19), 7040. https://doi.org/10.3390/jcm14197040







