1. Introduction
In fixed prosthodontics, tooth preparation design is a key determinant for the long-term success, esthetic integration, and periodontal stability of restorations. The configuration and position of the finishing line critically determine how the interaction between restorations with gingival and peri-implant soft tissues.
Traditionally, two preparation categories have been described: horizontal preparations, such as chamfer and shoulder, and vertical preparations, including feather-edge techniques [
1,
2,
3,
4,
5,
6,
7]. Horizontal finishing lines are predictable and widely taught, but evidence indicates they may predispose to plaque accumulation, inflammation, and marginal recession particularly when extended subgingivally [
8,
9,
10].
To address these limitations, the Biologically Oriented Preparation Technique (BOPT) introduced by Ignacio Loi in 2008 [
11] proposed a vertical, edgeless concept. This vertical preparation concept eliminates the pre-existing emergence profile and uses immediate temporization to guide gingival adaptation, promoting increased soft tissue thickness, stable probing depths, and long-term margin stability [
12,
13,
14]. Clinical studies have demonstrated its ability to promote soft tissue thickening, stable probing depths, and long-term margin stability, with prospective trials confirming favorable outcomes after up to 10 years [
12,
13,
14].
Advances in digital dentistry have further enhanced the applicability of vertical preparations. Intraoral scanning, CAD/CAM workflows, and virtual gingiva modeling enable precise reproduction of the emergence profile and more predictable transfer from provisional to definitive restorations [
15,
16,
17,
18].
Clinically, the choice between chamfer, shoulder, and BOPT should be individualized: while BOPT offers advantages in thin gingival biotypes and esthetically demanding anterior regions, horizontal designs remain reliable in posterior areas with lower esthetic demands and greater biomechanical requirements [
8,
12,
19].
This review synthesizes clinical, histological, and experimental evidence to critically compare horizontal and vertical preparations, with particular emphasis on BOPT, evaluating their biological, mechanical, and esthetic implications in contemporary prosthodontics.
Objective
The primary objective of this review is to critically assess and compare the biological, clinical, and esthetic outcomes of conventional horizontal preparations (chamfer and shoulder) with vertical approaches such as the Biologically Oriented Preparation Technique (BOPT). Special emphasis is placed on periodontal health parameters—including probing depth, gingival inflammation, margin stability, and soft tissue thickness—that have been highlighted in prospective clinical trials and systematic reviews as crucial indicators of long-term success [
6,
17,
18].
Another important objective is to evaluate the contribution of analog and digital workflows in shaping the emergence profile of BOPT restorations, with recent studies demonstrating the growing reliability of intraoral scanning and CAD/CAM systems in managing subgingival contours [
8,
19,
20]. The review also considers the mechanical implications of preparation design, including tooth structure reduction [
3] and stress distribution in endodontically treated teeth restored with zirconia crowns [
7].
Finally, the review explores clinical outcomes of BOPT in implant-supported restorations, particularly with convergent collar implants and customized healing abutments, which have shown favorable effects on peri-implant tissues [
21,
22,
23,
24,
25,
26]. It also addresses the level of professional awareness and adoption of vertical preparation techniques, identifying barriers to broader implementation and underscoring the relevance of the prosthetic adaptation profile as a novel framework for achieving predictable long-term rehabilitation [
14,
16].
2. Materials and Methods
This paper was designed as a narrative review, with elements of structured searching and study selection similar to a scoping review. A formal systematic review was not attempted, as the heterogeneity of study designs and outcomes precluded meta-analysis. This review was conducted as a narrative synthesis of the available evidence on the influence of tooth preparation designs on periodontal health and long-term stability. A comprehensive literature search was performed between September 2023 and January 2025 using four electronic databases: PubMed/MEDLINE, Scopus, Web of Science, and Google Scholar.
The search strategy combined keywords and Boolean operators related to preparation design and periodontal outcomes, including “tooth preparation”, “chamfer”, “shoulder”, “Biologically Oriented Preparation Technique”, “BOPT”, “vertical preparation”, “biologic width”, “periodontal health”, “gingival stability”, and “emergence profile”. Reference lists of systematic reviews and relevant clinical studies were also screened manually to identify additional eligible publications.
Inclusion criteria were as follows: (a) studies published in English between January 2000 and January 2025; (b) clinical trials, prospective or retrospective studies, systematic or narrative reviews, in vitro investigations, and histological studies; and (c) research addressing conventional horizontal preparations (chamfer, shoulder) or vertical preparations (BOPT, feather-edge).
Exclusion criteria included the following: (a) case reports, conference abstracts, and opinion papers without original data; (b) studies unrelated to full-coverage restorations or periodontal outcomes; and (c) implant studies not specifically evaluating preparation design or emergence profile.
After duplicate removal and eligibility screening, 112 articles were included in the final synthesis. Selection was performed independently by two authors, with disagreements resolved through discussion until consensus was achieved. Extracted data were categorized into domains covering periodontal parameters, preparation geometry, analogical versus digital workflows, esthetic outcomes, survival and complication rates, and long-term stability.
Given the heterogeneity of study designs and outcomes, direct quantitative comparison or meta-analysis was not feasible. As this is a narrative review, no formal risk of bias tool was applied; however, study selection and data extraction were performed independently by two authors to enhance transparency.
No formal risk of bias or quality appraisal tool was applied, which is consistent with the scope of a narrative review. However, heterogeneity in study designs and sample sizes was acknowledged and considered in the interpretation of findings.
3. Results
A total of 112 studies met the inclusion criteria and were synthesized in this review. The findings are presented according to periodontal, mechanical, esthetic, and digital domains.
3.1. Periodontal Parameters
Long-term prospective studies (sample sizes ranging from 40 to 85 patients; follow-up periods of 6–10 years) reported that BOPT maintained stable probing depths (mean variation <0.2 mm) and significantly increased gingival thickness compared with horizontal designs [
9,
17,
18]. One 10-year trial involving 77 restorations confirmed superior periodontal stability and gingival volume preservation in BOPT compared with chamfer and shoulder preparations [
17]. By contrast, chamfer and shoulder preparations, though predictable in the short term, have been linked to progressive gingival recession and papilla loss, particularly in anterior esthetic regions [
7,
8,
23].
3.2. Gingival Inflammation
Clinical investigations with sample sizes between 30 and 60 patients demonstrated that subgingival chamfer or shoulder margins were associated with higher plaque indices and bleeding on probing (BOP > 25%) after 2–3 years [
8,
23]. In contrast, BOPT restorations showed significantly lower BOP scores (<10%) and reduced plaque accumulation over comparable follow-up periods [
9,
17,
18].
3.3. Tooth Reduction and Biomechanics
In vitro analysis has demonstrated that preparation geometry directly influences the extent of tooth reduction. A recent study by Real-Voltas et al. (2025) showed that BOPT and its modification (BOPTm) preserve more dental structure in anterior teeth compared to chamfer and shoulder, while still ensuring functional retention [
3]. Finite element analysis confirmed that marginal design affects stress concentration in both teeth and restorations, with BOPT showing slightly higher marginal stress values but remaining within clinically acceptable limits [
7].
3.4. Esthetic Outcomes and Patient Satisfaction
Prospective clinical trials (
n = 45–80 patients; follow-up 6–10 years) reported higher esthetic scores for BOPT restorations compared with horizontal designs, particularly in anterior teeth (mean satisfaction score >90% vs. ~75%) [
9,
17,
18]. One 10-year study further confirmed stable gingival margins and high esthetic predictability, with >95% of patients rating their restorations as satisfactory or highly satisfactory [
17]. In contrast, chamfer and shoulder preparations provide initially acceptable esthetics, but satisfaction scores tend to decrease over time as marginal recession develops [
23].
3.5. Implant-Supported Restorations
Clinical evidence supports the application of BOPT principles in implant prosthodontics. Studies with convergent collar implants and customized healing abutments reported improved peri-implant soft tissue stability and keratinized mucosa width compared with conventional implant protocols [
21,
25,
26].
3.6. Digital Workflows
Multiple studies demonstrated the successful integration of digital workflows into vertical preparation protocols. Intraoral scanning and CAD/CAM technologies enable precise reproduction of the emergence profile and facilitate accurate transfer of provisional contours to definitive restorations [
8,
10,
11,
19,
20]. This improved accuracy in reproducing the emergence profile has been associated with reduced plaque accumulation and lower bleeding on probing scores, as well as more stable probing depths and gingival margins in BOPT cases compared with conventional workflows [
8,
19,
20]. Recent digital protocols also incorporate virtual gingiva modeling and finish line identification, which improve the transfer of provisional contours to definitive restorations. These advances contribute to clinically relevant endpoints such as reduced plaque accumulation, lower bleeding on probing, stable probing depths, and improved margin stability in BOPT cases [
11,
20].
3.7. Summary of Comparative Outcomes
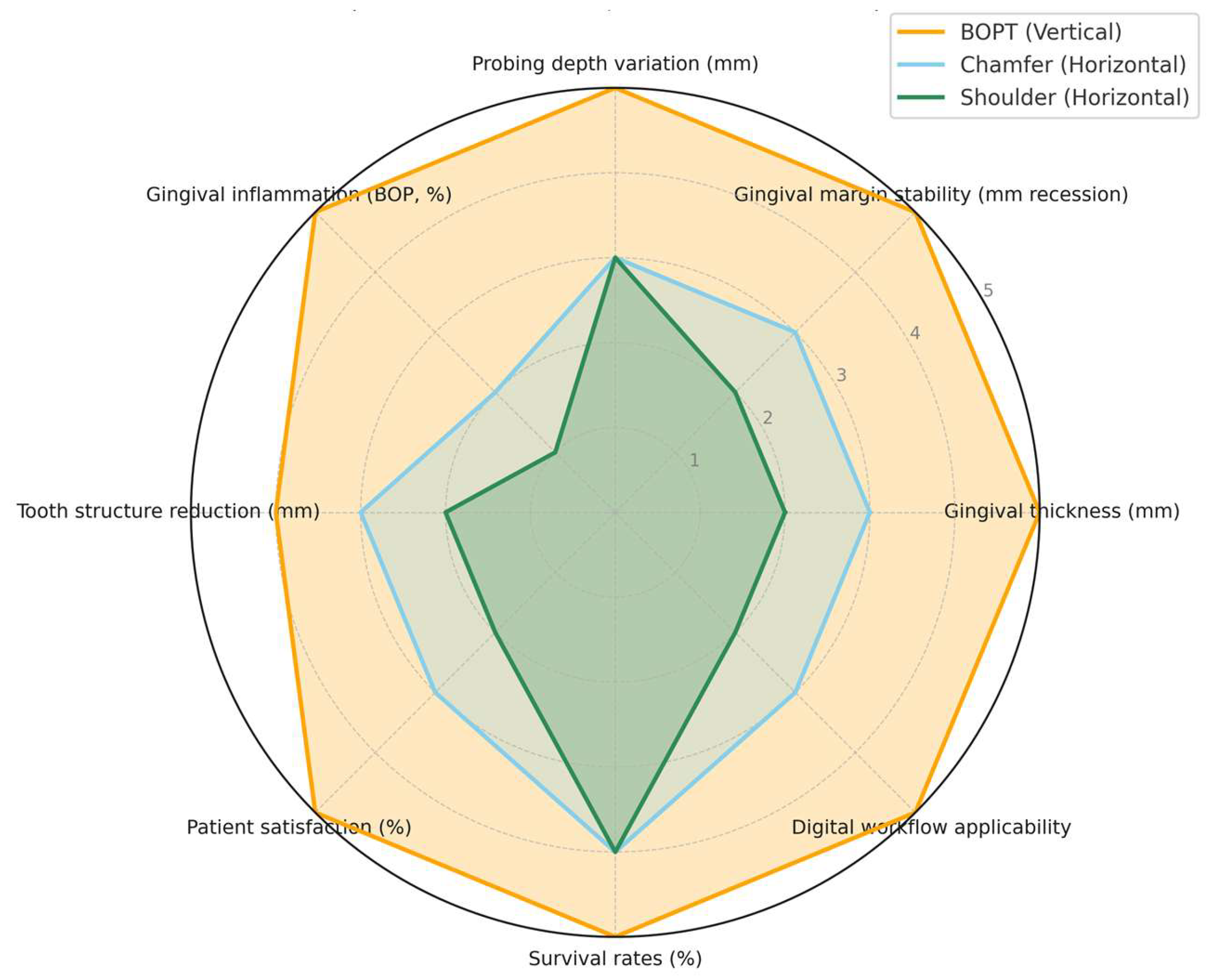
The comparative performance of BOPT, chamfer, and shoulder preparations across periodontal, biological, and esthetic parameters is synthesized in
Table 1 and illustrated in
Figure 1, highlighting the superior stability and clinical predictability of BOPT.
The table summarizes findings from prospective clinical trials, in vitro investigations, and systematic reviews, focusing on gingival thickness, margin stability, probing depth, inflammation, tooth structure reduction, esthetic outcomes, survival rates, and digital workflow integration [
3,
7,
8,
9,
12,
13,
19,
20,
21,
22].
The figure compares eight parameters: gingival thickness, margin stability, probing depth, gingival inflammation/bleeding on probing, tooth reduction, esthetic outcomes, survival rates, and digital workflow applicability. Data were synthesized from key clinical and laboratory studies [
3,
7,
8,
9,
10,
17,
18,
19,
20,
23]. BOPT consistently demonstrates superior periodontal and esthetic outcomes compared with conventional horizontal preparations.
4. Discussion
The design of tooth preparation is a decisive factor in preserving periodontal health and ensuring the long-term success of fixed prosthodontic restorations. The location and geometry of the finishing line directly influence marginal adaptation, plaque retention, and gingival response.
Evidence shows that CAD/CAM-fabricated zirconia restorations provide superior marginal fit and reduced gingival inflammation compared with conventionally fabricated metal–ceramic prostheses [
27]. The smoother surfaces and more precise emergence profiles achieved through digital workflows contribute to plaque control and enhance periodontal stability. These findings highlight the importance of both material selection and fabrication technology in reducing biological complications.
Importantly, digital workflows are not only a matter of technical precision but have direct biological implications. By enabling accurate transfer of the provisional emergence profile, intraoral scanning and CAD/CAM systems facilitate a harmonious prosthesis–gingiva interface [
28]. This translates into lower gingival inflammation, more stable probing depths, and reduced risk of marginal recession compared with conventional workflows. The vertical position of restoration margins is equally critical. Studies have consistently demonstrated that subgingival margins are associated with increased inflammation due to plaque retention and marginal misfit, whereas supragingival margins are more favorable for periodontal health and facilitate maintenance [
9]. Preservation of the biologic width and respect for the supracrestal tissue attachment remain essential principles in restorative dentistry.
Long-term studies confirm that BOPT maintains stable soft tissue conditions with minimal recession and high patient satisfaction [
4,
19,
20,
29]. By contrast, conventional preparations such as chamfer and shoulder, although predictable and widely adopted, have been linked to progressive gingival recession and loss of papillary height over time, particularly in the anterior esthetic zone [
7,
8]. Recent in vitro data further suggest that horizontal preparations require greater tooth reduction in anterior teeth compared with BOPT, while BOPT achieves comparable retention with more conservative tissue removal [
3]. A 10-year prospective trial also confirmed that restorations performed with BOPT maintain superior soft tissue stability compared to horizontal designs, reinforcing its clinical relevance [
19].
Clinically, preparation design should be individualized: BOPT offers advantages for thin gingival biotypes and anterior esthetic cases, while chamfer and shoulder remain reliable in posterior regions with lower esthetic demands [
4,
8]. In high-risk patients, supragingival margins and minimally invasive designs are preferable [
7,
8,
9,
30]. The integration of digital workflows is also pivotal, as intraoral scanning and CAD/CAM technologies increase accuracy and reproducibility, particularly in BOPT cases where the exact transfer of the provisional emergence profile is crucial [
21,
22]. Beyond technical precision, this transferability directly impacts clinical outcomes: accurate reproduction of provisional contours contributes to lower gingival inflammation, maintenance of stable probing depths, and improved long-term margin stability [
31]. Digital workflows therefore play not only a technical but also a biological role in supporting periodontal health.
Most available studies are prospective cohorts or case series with limited sample sizes, and heterogeneity in design and outcomes makes direct comparison difficult. This underscores the need for well-designed randomized controlled trials with long-term follow-up. In summary, while chamfer and shoulder preparations remain reliable and widely practiced, BOPT offers distinctive biological and esthetic benefits, especially in high-risk and esthetically demanding situations. The available evidence suggests that BOPT may offer biological and esthetic advantages in selected cases, but the heterogeneity and limited scale of current studies prevent definitive conclusions. Widespread adoption should await further clinician training supported by robust randomized trials and long-term data [
4,
7,
8,
19,
20].
Additional contributions support the relevance of preparation design: Hategan et al. linked finish line geometry with periodontal health [
32], while Petrescu et al. emphasized the biological determinants of esthetic outcomes in non-metallic prostheses [
33]. Novel diagnostic methods such as optical coherence tomography [
34] and micro-CT [
35] may refine the evaluation of restorative interfaces. Furthermore, advances in smart biomaterials, including magnetorheological elastomers [
36], illustrate potential future directions, although their direct application to tooth preparation design remains exploratory.
Recent advances in CAD/CAM technologies, both subtractive and additive, have enhanced the clinical relevance of preparation design by enabling precise finishing line reproduction, virtual gingiva modeling, and accurate transfer of provisional contours to definitive restorations [
10,
19,
20]. These digital workflows contribute to improved marginal adaptation and emergence profile control, thus supporting periodontal stability and esthetic integration [
11,
21]. Nevertheless, long-term outcomes remain closely dependent on respecting the supracrestal tissue attachment and ensuring patient-related factors such as post-restorative care and adequate oral hygiene [
7,
8,
9]. This is particularly relevant in patients with advanced periodontal disease, where restorative strategies must be carefully balanced with periodontal stability to achieve long-term success [
37,
38,
39,
40,
41].
Limitations and Clinical Implications
Most of the available evidence regarding tooth preparation design is derived from prospective cohort studies and case series, often with relatively small sample sizes and heterogeneous methodologies. A 10-year prospective study confirmed the long-term stability of BOPT restorations [
19], but randomized controlled trials are still lacking. Previous findings have also shown that subgingival margins increase inflammatory risk compared to supragingival designs [
9], highlighting the importance of respecting biological width and tissue health. Furthermore, recent investigations demonstrate that margin design and restorative material directly influence mechanical integrity and periodontal outcomes, emphasizing the need for well-structured comparative trials [
27].
Clinically, preparation design should always be individualized according to the patient’s gingival biotype, esthetic requirements, and periodontal risk profile, ensuring that restorative strategies are tailored to both biological principles and patient-specific needs [
8,
19].
The reliability of conclusions is limited by the absence of a formal risk of bias assessment, as well as by heterogeneity in the included studies regarding design, follow-up periods, and clinical outcomes. These factors should be taken into account when interpreting the findings.
5. Conclusions
The preservation of periodontal health and stability is closely dependent on tooth preparation design. Respecting the biologic width, maintaining supragingival margins whenever possible, and ensuring a harmonious interaction between the restoration and soft tissues remain fundamental principles for long-term clinical success [
7,
9]. Conventional horizontal designs such as chamfer and shoulder remain predictable and widely used, but may predispose to inflammation and recession, especially in esthetic areas [
8].
The Biologically Oriented Preparation Technique (BOPT) represents an alternative concept by promoting gingival adaptation to the restoration rather than obliging the prosthesis to conform to pre-existing contours. Long-term evidence demonstrates gingival thickening, stable probing depths, and improved margin stability with BOPT [
4,
19,
20].
Nevertheless, the choice of preparation design should be individualized according to gingival biotype, esthetic requirements, and periodontal risk profile, to optimize both biological and functional outcomes. Clinically, preparation design should be individualized based on gingival biotype, esthetic requirements, and periodontal risk profile, balancing biological preservation with functional demands.
In summary, while BOPT demonstrates encouraging results regarding gingival stability and esthetic integration, its advantages over conventional preparations remain to be validated in large, well-designed clinical trials. Until such evidence is available, BOPT should be considered a promising but not yet proven alternative within the prosthodontic armamentarium.
Author Contributions
Conceptualization, T.H., G.D.C. and I.V.; methodology, I.V., M.R. and M.D.; software, T.H. and M.D.; validation, M.R., T.H. and M.D.; formal analysis, T.H., G.D.C. and M.D.; investigation, G.D.C., T.H. and M.D.; resources, T.H.; data curation, T.H. and M.R.; writing—original draft preparation, T.H., G.D.C., I.V. and M.R.; writing—review and editing I.V., T.H., G.D.C., T.H. and M.R.; visualization, M.R.; supervision, G.D.C. and M.R.; project administration, T.H.; funding acquisition, T.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received funding from “Victor Babes” University of Medicine and Pharmacy in Timisoara, Romania, for the publication fee.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| BOPT | Biologically Oriented Preparation Technique |
| CAD/CAM | Computer-aided design/computer-aided manufacturing |
References
- Abad-Coronel, C.; Villacís Manosalvas, J.; Palacio Sarmiento, C.; Esquivel, J.; Loi, I.; Pradíes, G. Clinical outcomes of the biologically oriented preparation technique (BOPT) in fixed dental prostheses: A systematic review. J. Prosthet. Dent. 2024, 132, 502–508. [Google Scholar] [CrossRef]
- Granell-Ruiz, M.; Bertolini, R.; Rech-Ortega, C.; Oteiza-Galdón, B.; Bouazza-Juanes, K. Gingival margin stabilization using the final prosthetic restoration (BOPT). A case report. J. Clin. Exp. Dent. 2024, 16, e1040–e1045. [Google Scholar] [CrossRef]
- Real-Voltas, F.; Galletti, C.; Gelosa, A.S.; Figueras-Alvarez, O.; Flores-Fraile, J.; Cabratosa-Termes, J. In vitro assessment of tooth reduction in incisors, canines, and bicuspids using horizontal (chamfer) and vertical (BOPT and BOPTm) finishing lines. J. Esthet. Restor. Dent. 2025, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Serra-Pastor, B.; Bustamante-Hernández, N.; Fons-Font, A.; Solá-Ruíz, M.F.; Revilla-León, M.; Agustín-Panadero, R. Periodontal behavior and patient satisfaction of anterior teeth restored with single zirconia crowns using a biologically oriented preparation technique: A 6-year prospective clinical study. J. Clin. Med. 2021, 10, 3482. [Google Scholar] [CrossRef] [PubMed]
- Loi, I.; Di Felice, A. Biologically oriented preparation technique (BOPT): A new approach for prosthetic restoration of periodontally healthy teeth. Eur. J. Esthet. Dent. 2013, 8, 10–23. [Google Scholar] [PubMed]
- Al-Haddad, A.; Arsheed, N.A.A.; Yee, A.; Kohli, S. Biological oriented preparation technique (BOPT) for tooth preparation: A systematic review and meta-analysis. Saudi Dent. J. 2024, 36, 11–19. [Google Scholar] [CrossRef]
- Sichi, L.G.B.; Pierre, F.Z.; Arcila, L.V.C.; de Andrade, G.S.; Tribst, J.P.M.; Ausiello, P.; di Lauro, A.E.; Borges, A.L.S. Effect of Biologically Oriented Preparation Technique on the stress concentration of endodontically treated upper central incisor restored with zirconia crown: 3D-FEA. Molecules 2021, 26, 6113. [Google Scholar] [CrossRef]
- Mohammad, A.; Abraham, S.A. Effect of biologically oriented and subgingival horizontal preparation techniques on periodontal health: A randomized controlled clinical trial. Saudi Dent. J. 2023, 35, 727–733. [Google Scholar] [CrossRef]
- Podhorsky, A.; Suchanek, J.; Rihakova, J.; Vanicek, J.; Holeckova, P.; Cermakova, E. Influence of subgingival and supragingival crown margins on periodontal health: A clinical and histological study. Clin. Oral Investig. 2015, 19, 1261–1268. [Google Scholar] [CrossRef]
- Cabanes-Gumbau, G.; Soto-Peñaloza, D.; Peñarrocha-Diago, M.; Peñarrocha-Diago, M. Analogical and digital workflow in the design and preparation of the emergence profile of BOPT crowns over implants in the working model. J. Clin. Med. 2019, 8, 1452. [Google Scholar] [CrossRef]
- Granell-Ruiz, M.; Rech-Ortega, C.; Oteiza-Galdón, B.; Bouazza-Juanes, K. Vertical preparation protocol for veneers: A case report. J. Clin. Exp. Dent. 2023, 15, e346–e350. [Google Scholar] [CrossRef] [PubMed]
- García-Gil, I.; Perez de la Calle, C.; Lopez-Suarez, C.; Pontevedra, P.; Suarez, M.J. Comparative analysis of trueness between conventional and digital impression in dental-supported fixed prosthesis with vertical preparation. J. Clin. Exp. Dent. 2020, 12, e896–e901. [Google Scholar] [CrossRef] [PubMed]
- Morini, C.M.; Franchini, L.; Saratti, C.M. Defining margins and emergence profile in vertical preparations: A digital technique. J. Prosthet. Dent. 2025, 134, 24–27. [Google Scholar] [CrossRef] [PubMed]
- Agustín-Panadero, R.; Ausina-Escrihuela, D.; Fernández-Estevan, L.; Román-Rodríguez, J.L.; Faus-López, J.; Solá-Ruíz, M.F. Dental-gingival remodeling with BOPT no-prep veneers. J. Clin. Exp. Dent. 2017, 9, e1496–e1500. [Google Scholar] [CrossRef]
- Morón-Conejo, B.; Gil, A.; Bonfanti-Gris, M.; Salido, M.P.; Martínez-Rus, F. Esthetic and functional rehabilitation: Retreatment of anterior fixed prosthesis with BOPT and digital workflow. J. Esthet. Restor. Dent. 2025, 37, 761–770. [Google Scholar] [CrossRef]
- Alahmari, N.M.; Al-Haboob, M.A.; Gadah, T.S.; Albar, N.H.; Al Moaleem, M.M.; Sayed, M.E.; Alhumaidi, A.M.; Al-Amri, T.M.A.S.; Diaban, S.S.A.; Tajedin, A.A.H.S. Knowledge and practice of dental professionals regarding vertical teeth preparation techniques. BMC Med. Educ. 2024, 24, 1482. [Google Scholar] [CrossRef]
- Mandillo-Alonso, V.; Cascos-Sánchez, R.; Antonaya-Martín, J.L.; Laguna-Martos, M. Soft tissue thickness evaluation in screw-retained crowns by the biologically oriented preparation technique (BOPT). J. Clin. Exp. Dent. 2021, 13, e1209–e1215. [Google Scholar] [CrossRef]
- Di Felice, A.; Abad-Coronel, C.; Giovane, V.; Loi, I.; Pradíes, G. The importance of esthetic integration through laboratory adaptation profiles in the BOPT. Int. J. Esthet. Dent. 2022, 17, 76–87. [Google Scholar] [PubMed]
- Agustín-Panadero, R.; Loi, I.; Fons-Badal, C.; Laguna-Martos, M.; Llobell-Cortell, A.; Serra-Pastor, B. Periodontal behavior of full-coverage restorations using BOPT: A 10-year prospective clinical study. Int. J. Periodontics Restor. Dent. 2025, 1–23. [Google Scholar] [CrossRef]
- Serra-Pastor, B.; Bustamante-Hernández, N.; Fons-Font, A.; Solá-Ruíz, M.F.; Revilla-León, M.; Agustín-Panadero, R. Periodontal outcomes of anterior fixed partial dentures using BOPT: A 6-year prospective trial. J. Prosthet. Dent. 2023, 129, 703–709. [Google Scholar] [CrossRef]
- Agustín-Panadero, R.; Loi, I.; Fernández-Estevan, L.; Chust, C.; Rech-Ortega, C.; Pérez-Barquero, J.A. Digital protocol for creating a virtual gingiva adjacent to teeth with subgingival dental preparations. J. Prosthodont. Res. 2020, 64, 506–514. [Google Scholar] [CrossRef]
- Cabanes-Gumbau, G.; Palma, J.C.; Kois, J.C.; Revilla-León, M. Transferring the preparation finish line on intraoral digital scans to software programs: A technique. J. Prosthet. Dent. 2023, 130, 439–443. [Google Scholar] [CrossRef]
- Canullo, L.; Menini, M.; Covani, U.; Pesce, P. Clinical outcomes of a prosthetic protocol to rehabilitate tissue-level implants with a convergent collar in the esthetic zone: A 3-year prospective study. J. Prosthet. Dent. 2020, 123, 246–251. [Google Scholar] [CrossRef]
- Palombo, D.; Rahmati, M.; Vignoletti, F.; Sanz-Esporrin, J.; Salido, M.P.; Haugen, H.J.; Sanz, M. Hard and soft tissue healing around teeth prepared with BOPT and restored with provisional crowns: An in vivo study. J. Clin. Periodontol. 2023, 50, 1217–1238. [Google Scholar] [CrossRef] [PubMed]
- Agustín-Panadero, R.; Bustamante-Hernández, N.; Labaig-Rueda, C.; Fons-Font, A.; Fernández-Estevan, L.; Solá-Ruíz, M.F. Influence of Biologically Oriented Preparation Technique on Peri-Implant Tissues; Prospective Randomized Clinical Trial with Three-Year Follow-Up. Part II: Soft Tissues. J. Clin. Med. 2019, 8, 2223. [Google Scholar] [CrossRef] [PubMed]
- Crespi, R.; Toti, P.; Covani, U.; Brevi, B.C.; Menchini-Fabris, G.B. Preformed customized healing abutments in BOPT procedures: A 3-year retrospective case-control study. Int. J. Comput. Dent. 2024, 27, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Hajaj, T.; Marian, D.; Zaharia, C.; Niculescu, S.T.; Negru, R.M.; Titihazan, F.; Rominu, M.; Sinescu, C.; Novac, A.C.; Dobrota, G.; et al. Fracture Resistance of CAD/CAM-Fabricated Zirconia and Lithium Disilicate Crowns with Different Margin Designs: Implications for Digital Dentistry. J. Funct. Biomater. 2025, 16, 205. [Google Scholar] [CrossRef]
- Zamparini, F.; Pirani, C.; Chavarria-Bolanos, D.; Gandolfi, M.G.; Prati, C. Rehabilitation of anterior maxilla with a novel hyperbolic profile transmucosal implant in elderly patients. Minerva Stomatol. 2019, 68, 249–258. [Google Scholar] [CrossRef]
- Agustín-Panadero, R.; Martín-de Llano, J.J.; Fons-Font, A.; Carda, C. Histological study of human periodontal tissue following BOPT. J. Clin. Exp. Dent. 2020, 12, e597–e602. [Google Scholar] [CrossRef]
- Carcuac, O.; Yakubova, N. The Concept of Crown Shortening: Combination of Vertical Edgeless Preparation Technique and Modified Coronally Advanced Tunnel. Int. J. Periodontics Restor. Dent. 2025, 1–16. [Google Scholar] [CrossRef]
- Serrano-Belmonte, I.; Roca-Cánovas, N.; Linares-Tovar, E.K.; Martínez-Cánovas, A.; Pérez-Fernández, V. Influence of the thickness of materials for provisionalization in minimally invasive restorations. Materials 2022, 15, 7238. [Google Scholar] [CrossRef]
- Hategan, S.I.; Belea, A.L.; Tanase, A.D.; Gavrilovici, A.M.; Petrescu, E.L.; Marsavina, L.; Sinescu, C.; Negrutiu, M.L.; Manole, M.C. The Evaluation of the Prosthetic Preparations Finish Lines for Provisional Crowns with the Impact on Periodontal Health. Rom. J. Oral Rehabil. 2024, 16, 453–459. [Google Scholar] [CrossRef]
- Petrescu, E.L.; Martu, I.; Sinescu, C.; Romînu, M.; Stoia, A.E.; Onisei, D.; Negrutiu, M.L.; Tanase, A.D.; Pop, D.M. Factors Involved in the Chromatic Failures of Non-Metallic Fixed Dental Prostheses. Rom. J. Oral Rehabil. 2024, 16, 549–556. [Google Scholar] [CrossRef]
- Sinescu, C.; Bradu, A.; Duma, V.-F.; Topala, F.; Negrutiu, M.; Podoleanu, A.G. Effects of Temperature Variations during Sintering of Metal Ceramic Tooth Prostheses Investigated Non-Destructively with Optical Coherence Tomography. Appl. Sci. 2017, 7, 552. [Google Scholar] [CrossRef]
- Zaharia, C.; Duma, V.-F.; Sinescu, C.; Socoliuc, V.; Craciunescu, I.; Turcu, R.P.; Marin, C.N.; Tudor, A.; Rominu, M.; Negrutiu, M.-L. Dental Adhesive Interfaces Reinforced with Magnetic Nanoparticles: Evaluation and Modeling with Micro-CT versus Optical Microscopy. Materials 2020, 13, 3908. [Google Scholar] [CrossRef] [PubMed]
- Gavrilovici, A.M.; Anitas, E.M.; Chirigiu, L.; Bica, I.; Negrutiu, M.L. Magnetodielectric Effects in Magnetorheological Elastomers Based on Polymer Fabric, Silicone Rubber, and Magnetorheological Suspension. Adv. Polym. Technol. 2019, 2019, 1983547. [Google Scholar] [CrossRef]
- Rădulescu, V.; Boariu, M.; Rusu, D.; Boldeanu, C.; Christodorescu, R.; Roman, A.; Surlin, P.; Didilescu, A.C.; Vela, O.; Kardaras, G.; et al. Is the Diagnosis of Generalized Stage IV (Severe) Periodontitis Compatible with the Survival of Extended Stabilizing Prosthetic Restorations? A Medium-Term Retrospective Study. Diagnostics 2022, 12, 3053. [Google Scholar] [CrossRef]
- Ilyes, I.; Rusu, D.; Rădulescu, V.; Vela, O.; Boariu, M.I.; Roman, A.; Surlin, P.; Kardaras, G.; Boia, S.; Chinnici, S.; et al. A Placebo-Controlled Trial to Evaluate Two Locally Delivered Antibiotic Gels (Piperacillin Plus Tazobactam vs. Doxycycline) in Stage III–IV Periodontitis Patients. Medicina 2023, 59, 303. [Google Scholar] [CrossRef]
- Ilyes, I.; Boariu, M.; Rusu, D.; Iorio-Siciliano, V.; Vela, O.; Boia, S.; Kardaras, G.; Șurlin, P.; Calniceanu, H.; Jentsch, H.; et al. A Single Dose of Piperacillin Plus Tazobactam Gel as an Adjunct to Professional Mechanical Plaque Removal (PMPR) in Patients with Peri-Implant Mucositis: A 6-Month Double-Blind Randomized Clinical Trial. Antibiotics 2024, 13, 269. [Google Scholar] [CrossRef]
- Ilyes, I.; Boariu, M.; Rusu, D.; Iorio-Siciliano, V.; Vela, O.; Boia, S.; Radulescu, V.; Șurlin, P.; Jentsch, H.; Lodin, A.; et al. Comparative Study of Systemic vs. Local Antibiotics with Subgingival Instrumentation in Stage III–IV Periodontitis: A Retrospective Analysis. Antibiotics 2024, 13, 430. [Google Scholar] [CrossRef]
- Vela, O.C.; Boariu, M.; Rusu, D.; Iorio-Siciliano, V.; Ramaglia, L.; Boia, S.; Radulescu, V.; Ilyes, I.; Stratul, S.-I. Healing of Periodontal Suprabony Defects following Treatment with Open Flap Debridement with or without Hyaluronic Acid (HA) Application. Medicina 2024, 60, 829. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).