What Imaging Technique Correlates Best with Surgical Findings in Gluteus Medius Tendon Tears?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
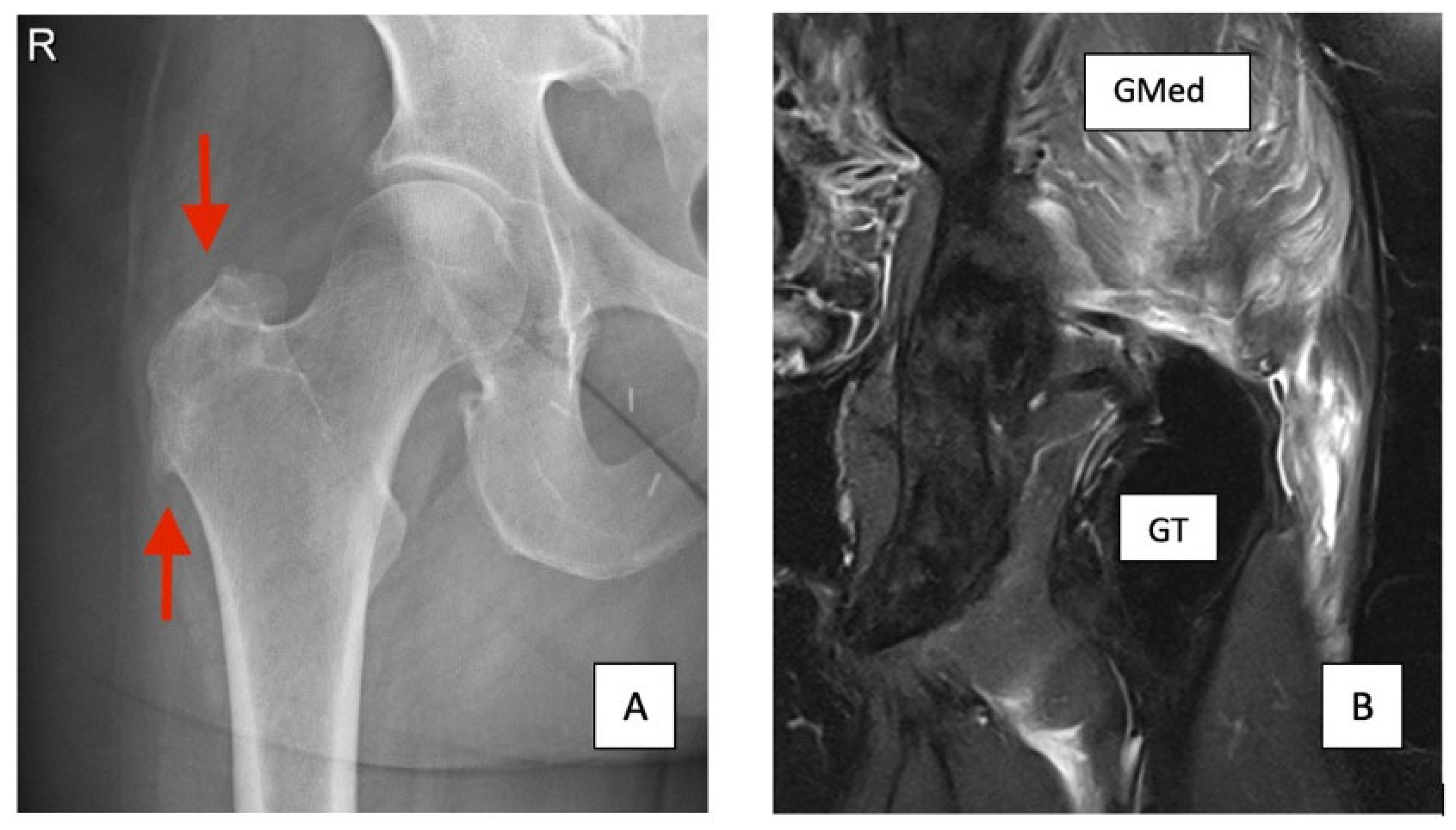
3.1. X-Ray
3.2. Ultrasound
3.3. MRI
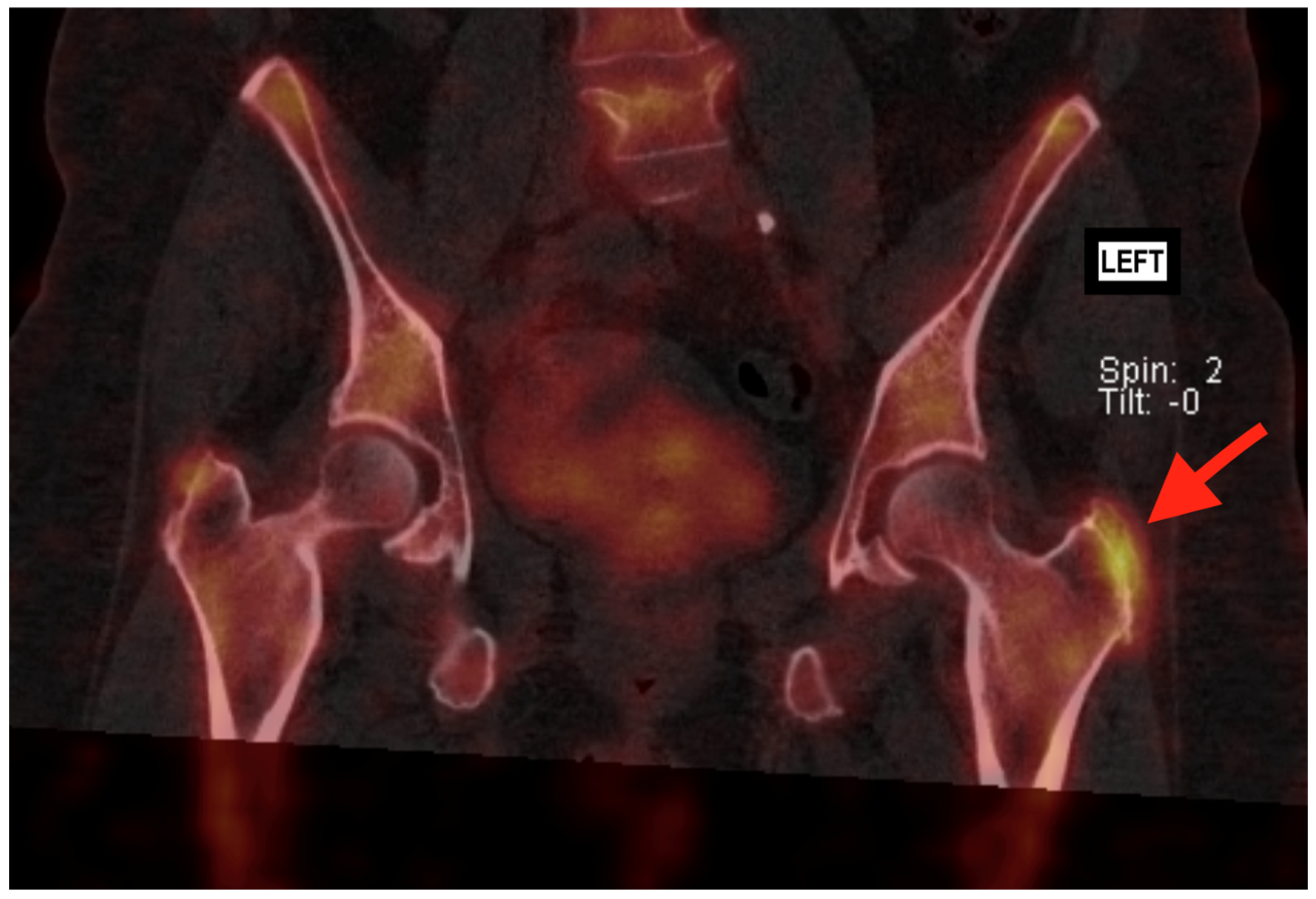
3.4. Bone Scan—SPECT/CT
3.5. Comparative Analysis
3.6. Diagnostic Imaging Combinations and Predictive Accuracy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fearon, A.M.; Cook, J.L.; Scarvell, J.M.; Neeman, T.; Cormick, W.; Smith, P.N. Greater trochanteric pain syndrome negatively affects work, physical activity and quality of life: A case control study. J. Arthroplast. 2014, 29, 383–386. [Google Scholar] [CrossRef] [PubMed]
- Arvesen, J.; McCallum, J.; Pill, S.G.; Cannady, H.; Adams, K.J.; Jackson, I.; Wienke, J.R.; Folk, J. Prevalence of Contralateral Hip Abductor Tears and Factors Associated with Symptomatic Progression. Am. J. Sports Med. 2022, 50, 1603–1608. [Google Scholar] [CrossRef] [PubMed]
- Bartolotta, R.J.; Ha, A.S.; Bateni, C.P.; Chen, K.C.; Dvorzhinskiy, A.; Flug, J.; Geannette, C.S.; Karagulle Kendi, A.T.; Laur, O.; Levenson, R.B.; et al. ACR Appropriateness Criteria® Acute Hip Pain 2024 Update. J. Am. Coll. Radiol. 2025, 22, S3–S13. [Google Scholar] [CrossRef] [PubMed]
- Cvitanic, O.; Henzie, G.; Skezas, N.; Lyons, J.; Minter, J. MRI diagnosis of tears of the hip abductor tendons (gluteus medius and gluteus minimus). AJR Am. J. Roentgenol. 2004, 182, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Docking, S.I.; Cook, J.; Chen, S.; Scarvell, J.; Cormick, W.; Smith, P.; Fearon, A. Identification and differentiation of gluteus medius tendon pathology using ultrasound and magnetic resonance imaging. Musculoskelet. Sci. Pract. 2019, 41, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Hartigan, D.E.; Perets, I.; Walsh, J.P.; Mohr, M.R.; Chaharbakhshi, E.O.; Yuen, L.C.; Domb, B.G. Radiographic Risk Factors and Signs of Abductor Tears in the Hip. Arthroscopy 2018, 34, 2389–2397. [Google Scholar] [CrossRef] [PubMed]
- Van Quickenborne, D.; Van Der Straeten, C.; Burssens, A.; Audenaert, E. Surgical technique for the open repair of grade 3–4 tears of the gluteus medius tendon of the hip: Technical note and case series. Int. J. Surg. Case Rep. 2025, 129, 111191. [Google Scholar] [CrossRef] [PubMed]
- Weissman, B.N.; Palestro, C.J.; Fox, M.G.; Bell, A.M.; Blankenbaker, D.G.; Frick, M.A.; Jawetz, S.T.; Kuo, P.H.; Said, N.; Stensby, J.D.; et al. ACR Appropriateness Criteria® Imaging After Total Hip Arthroplasty. J. Am. Coll. Radiol. 2023, 20, S413–S432. [Google Scholar] [CrossRef] [PubMed]
- Van Quickenborne, D.; Van Der Straeten, C.; Burssens, A.; Audenaert, E. Victorian Institute of Sport Assessment questionnaire specifically tailored for greater trochanteric pain syndrome for the Dutch population. J. Hip Preserv. Surg. 2024, 11, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Fearon, A.M.; Scarvell, J.M.; Cook, J.L.; Smith, P.N. Does ultrasound correlate with surgical or histologic findings in greater trochanteric pain syndrome? A pilot study. Clin. Orthop. Relat. Res. 2010, 468, 1838–1844. [Google Scholar] [CrossRef] [PubMed]
- Connell, D.A.; Bass, C.; Sykes, C.A.; Young, D.; Edwards, E. Sonographic evaluation of gluteus medius and minimus tendinopathy. Eur. Radiol. 2003, 13, 1339–1347. [Google Scholar] [CrossRef] [PubMed]
- Şirolu, S.; Hamid, R.; Arman, G.M.; Karagöz, S.H.; Salt, V.; Alçiçek, M.N.; Akgün, K.; Kalyoncu Uçar, A.; Adaletli, İ. An appraisal and comparative analysis of superb microvascular imaging with conventional ultrasound and MRI for greater trochanteric pain syndrome management. Medicine 2024, 103, e38622. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Grimaldi, A.; Nasser, A.; Mellor, R.; Vicenzino, B. An examination of imaging findings in patients with clinically diagnosed gluteal tendinopathy: A secondary analysis of a randomised clinical trial. Arch. Orthop. Trauma Surg. 2025, 145, 347. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Sex (F/M) | 41 (91.1%)/4 |
| Age (years) | 63.0 ± 10.6 (range 36–83) |
| BMI (kg/m2) | 26.0 ± 3.3 (range 21.7–36.5) |
| Affected side (L/R) | 19/26 |
| Preoperative VISA-G (0–100) | 42.6 ± 7.9 (range 26–56) |
| Modality | Cases | TP | TN | FP | FN | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|---|---|---|
| X-ray | 45 | 9 | 4 | 0 | 32 | Limited | Perfect (100%) | 100% | 11.1% |
| Ultrasound | 45 | 40 | 0 | 4 | 1 | Excellent | Limited (0%) | 90.9% | 0% |
| MRI | 45 | 41 | 0 | 4 | 0 | Perfect (100%) | Limited (0%) | 91.1% | 0% |
| Bone Scan (SPECT/CT) | 38 | 16 | 4 | 0 | 25 | Limited | Perfect (100%) | 100% | 13.8% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Quickenborne, D.; Van Der Straeten, C.; Burssens, A.; Audenaert, E. What Imaging Technique Correlates Best with Surgical Findings in Gluteus Medius Tendon Tears? J. Clin. Med. 2025, 14, 6714. https://doi.org/10.3390/jcm14196714
Van Quickenborne D, Van Der Straeten C, Burssens A, Audenaert E. What Imaging Technique Correlates Best with Surgical Findings in Gluteus Medius Tendon Tears? Journal of Clinical Medicine. 2025; 14(19):6714. https://doi.org/10.3390/jcm14196714
Chicago/Turabian StyleVan Quickenborne, Damien, Catherine Van Der Straeten, Arne Burssens, and Emmanuel Audenaert. 2025. "What Imaging Technique Correlates Best with Surgical Findings in Gluteus Medius Tendon Tears?" Journal of Clinical Medicine 14, no. 19: 6714. https://doi.org/10.3390/jcm14196714
APA StyleVan Quickenborne, D., Van Der Straeten, C., Burssens, A., & Audenaert, E. (2025). What Imaging Technique Correlates Best with Surgical Findings in Gluteus Medius Tendon Tears? Journal of Clinical Medicine, 14(19), 6714. https://doi.org/10.3390/jcm14196714






