Endo-Periodontal Lesions Without Root Damage: Recommendations for Clinical Management
Abstract
1. Introduction
2. Methods
3. Results
3.1. EPL Diagnosis
3.2. Management of EPLs Without Root Damage
3.2.1. EPLs in the Periodontitis Patient (Figure 1)
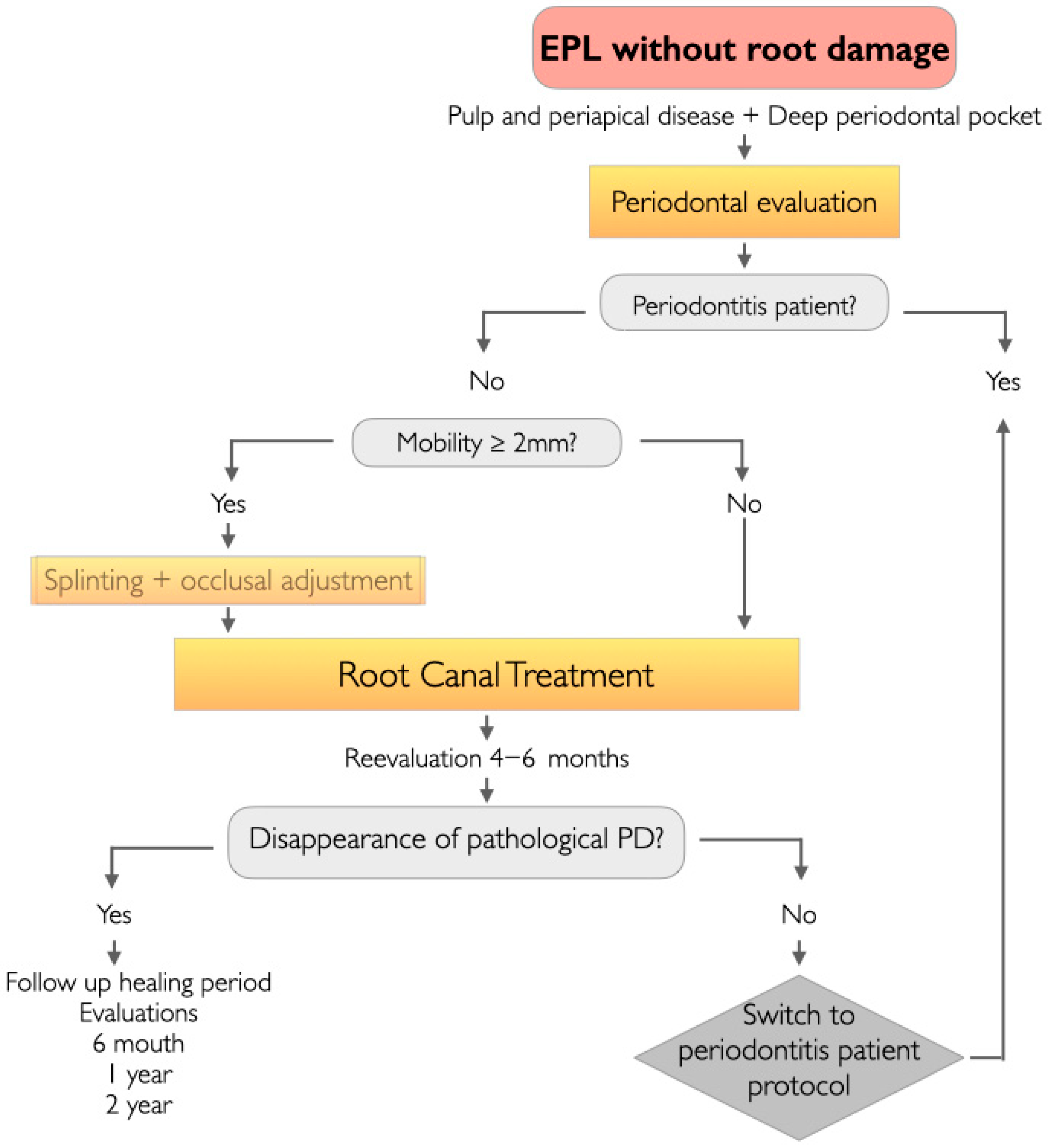
3.2.2. EPLs in the Non-Periodontitis Patient (Figure 2)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| EPL | Endo-periodontal lesion |
| PD | Probing depth |
| CAL | Clinical attachment level |
| SPT | supportive periodontal therapy |
References
- Kinaia, B.M.; Chogle, S.M.; Kinaia, A.M.; Goodis, H.E. Regenerative therapy: A periodontal-endodontic perspective. Dent. Clin. N. Am. 2012, 56, 537–547. [Google Scholar] [CrossRef] [PubMed]
- Herrera, D.; Retamal-Valdes, B.; Alonso, B.; Feres, M. Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo-periodontal lesions. J. Periodontol. 2018, 89 (Suppl. S1), S85–S102. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, J.C.; Walter, C.; Amato, M.; Weiger, R. Treatment of periodontal-endodontic lesions—A systematic review. J. Clin. Periodontol. 2014, 41, 779–790. [Google Scholar] [CrossRef] [PubMed]
- Rotstein, I. Interaction between endodontics and periodontics. Periodontol. 2000 2017, 74, 11–39. [Google Scholar] [CrossRef]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89 (Suppl. S1), S173–S182. [Google Scholar]
- Gambin, D.J.; Vitali, F.C.; Casanova, K.A.S.; DE Carli, J.P.; Mazzon, R.R.; Gomes, B.; Trentin, M.S.; Duque, T.M. Prevalence of species of yellow, purple and green microbial complexes in endo-perio lesions: A systematic review. Braz. Oral. Res. 2024, 38, e048. [Google Scholar] [CrossRef]
- Oh, S.L.; Fouad, A.F.; Park, S.H. Treatment strategy for guided tissue regeneration in combined endodontic-periodontal lesions: Case report and review. J. Endod. 2009, 35, 1331–1336. [Google Scholar] [CrossRef]
- Shenoy, N.; Shenoy, A. Endo-perio lesions: Diagnosis and clinical considerations. Indian. J. Dent. Res. 2010, 21, 579–585. [Google Scholar] [CrossRef]
- Jivoinovici, R.; Suciu, I.; Dimitriu, B.; Perlea, P.; Bartok, R.; Malita, M.; Ionescu, C. Endo-periodontal lesion—Endodontic approach. J. Med. Life 2014, 7, 542–544. [Google Scholar]
- Simon, J.H.; Glick, D.H.; Frank, A.L. The relationship of endodontic-periodontic lesions. J. Periodontol. 1972, 43, 202–208. [Google Scholar] [CrossRef]
- Torabinejad, M.W.R. Endodontics Principles and Practice; Mc-Graw Hill Interameriana: Mexico City, Mexico, 1996. [Google Scholar]
- Special Committee to Revise the Joint AAE/AAOMR Position Statement on Use of CBCT in Endodontics. AAE and AAOMR Joint Position Statement: Use of Cone Beam Computed Tomography in Endodontics 2015 Update. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2015, 120, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Woelber, J.P.; Fleiner, J.; Rau, J.; Ratka-Krüger, P.; Hannig, C. Accuracy and Usefulness of CBCT in Periodontology: A Systematic Review of the Literature. Int. J. Periodontics Restor. Dent. 2018, 38, 289–297. [Google Scholar] [CrossRef]
- Patel, S.; Brown, J.; Pimentel, T.; Kelly, R.D.; Abella, F.; Durack, C. Cone beam computed tomography in Endodontics—A review of the literature. Int. Endod. J. 2019, 52, 1138–1152. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Clin. Periodontol. 2018, 45 (Suppl. S20), S149–S161. [Google Scholar] [CrossRef]
- Pico-Blanco, A.; Castelo-Baz, P.; Caneiro-Queija, L.; Liñares-González, A.; Martin-Lancharro, P.; Blanco-Carrión, J. Saving Single-rooted Teeth with Combined Endodontic-periodontal Lesions. J. Endod. 2016, 42, 1859–1864. [Google Scholar] [CrossRef]
- Fan, J.; Caton, J.G. Occlusal trauma and excessive occlusal forces: Narrative review, case definitions, and diagnostic considerations. J. Clin. Periodontol. 2018, 45 (Suppl. S20), S199–S206. [Google Scholar] [CrossRef]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A new classification scheme for periodontal and peri-implant diseases and conditions—Introduction and key changes from the 1999 classification. J. Periodontol. 2018, 89 (Suppl. S1), S1–S8. [Google Scholar] [CrossRef]
- Graziani, F.; Karapetsa, D.; Alonso, B.; Herrera, D. Nonsurgical and surgical treatment of periodontitis: How many options for one disease? Periodontol 2000 2017, 75, 152–188. [Google Scholar] [CrossRef]
- Cortellini, P.; Stalpers, G.; Mollo, A.; Tonetti, M.S. Periodontal regeneration versus extraction and dental implant or prosthetic replacement of teeth severely compromised by attachment loss to the apex: A randomized controlled clinical trial reporting 10-year outcomes, survival analysis and mean cumulative cost of recurrence. J. Clin. Periodontol. 2020, 47, 768–776. [Google Scholar] [PubMed]
- Cortellini, P.; Tonetti, M.S. Clinical concepts for regenerative therapy in intrabony defects. Periodontol 2000 2015, 68, 282–307. [Google Scholar] [CrossRef] [PubMed]
- Cortellini, P.; Tonetti, M.S. Clinical performance of a regenerative strategy for intrabony defects: Scientific evidence and clinical experience. J. Periodontol. 2005, 76, 341–350. [Google Scholar] [CrossRef]
- Zhang, M.M.; Liang, Y.H.; Gao, X.J.; Jiang, L.; van der Sluis, L.; Wu, M.K. Management of Apical Periodontitis: Healing of Post-treatment Periapical Lesions Present 1 Year after Endodontic Treatment. J. Endod. 2015, 41, 1020–1025. [Google Scholar] [CrossRef]
- Abbott, P.V.; Salgado, J.C. Strategies for the endodontic management of concurrent endodontic and periodontal diseases. Aust. Dent. J. 2009, 54 (Suppl. S1), S70–S85. [Google Scholar] [CrossRef] [PubMed]
- Ruetters, M.; Kim, T.S.; Krisam, J.; El-Sayed, S.; ElSayed, N. Effect of endodontic treatment on periodontal healing of grade 3 endo-periodontal lesions without root damage in periodontally compromised patients-a retrospective pilot study. Clin. Oral. Investig. 2021, 25, 2373–2380. [Google Scholar] [CrossRef]
- Axelsson, P.; Nyström, B.; Lindhe, J. The long-term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. J. Clin. Periodontol. 2004, 31, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, X.; Xu, J.; Zhou, X.; Xie, K. The clinical study on the use of diode laser irradiation in the treatment of periodontal-endodontic combined lesions. Hua Xi Kou Qiang Yi Xue Za Zhi 2012, 30, 161–164+168. [Google Scholar]
- Salehrabi, R.; Rotstein, I. Endodontic treatment outcomes in a large patient population in the USA: An epidemiological study. J. Endod. 2004, 30, 846–850. [Google Scholar] [CrossRef] [PubMed]
- Ng, Y.L.; Mann, V.; Gulabivala, K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health. Int. Endod. J. 2011, 44, 583–609. [Google Scholar] [CrossRef]
- Schulz, A.; Hilgers, R.D.; Niedermeier, W. The effect of splinting of teeth in combination with reconstructive periodontal surgery in humans. Clin. Oral. Investig. 2000, 4, 98–105. [Google Scholar] [CrossRef]
- Kim, E.; Song, J.S.; Jung, I.Y.; Lee, S.J.; Kim, S. Prospective clinical study evaluating endodontic microsurgery outcomes for cases with lesions of endodontic origin compared with cases with lesions of combined periodontal-endodontic origin. J. Endod. 2008, 34, 546–551. [Google Scholar] [CrossRef]
- Song, M.; Kang, M.; Kang, D.R.; Jung, H.I.; Kim, E. Comparison of the effect of endodontic-periodontal combined lesion on the outcome of endodontic microsurgery with that of isolated endodontic lesion: Survival analysis using propensity score analysis. Clin. Oral. Investig. 2018, 22, 1717–1724. [Google Scholar] [CrossRef] [PubMed]
- Rosen, E.; Tsesis, I.; Kavalerchik, E.; Salem, R.; Kahn, A.; Del Fabbro, M.; Taschieri, S.; Corbella, S. Effect of guided tissue regeneration on the success of surgical endodontic treatment of teeth with endodontic-periodontal lesions: A systematic review. Int. Endod. J. 2023, 56, 910–921. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aranda Verdú, S.; Pallarés Sabater, A.; Pallarés Serrano, A.; Rubio Climent, J.; Casino Alegre, A. Endo-Periodontal Lesions Without Root Damage: Recommendations for Clinical Management. J. Clin. Med. 2025, 14, 6655. https://doi.org/10.3390/jcm14186655
Aranda Verdú S, Pallarés Sabater A, Pallarés Serrano A, Rubio Climent J, Casino Alegre A. Endo-Periodontal Lesions Without Root Damage: Recommendations for Clinical Management. Journal of Clinical Medicine. 2025; 14(18):6655. https://doi.org/10.3390/jcm14186655
Chicago/Turabian StyleAranda Verdú, Susana, Antonio Pallarés Sabater, Antonio Pallarés Serrano, Jorge Rubio Climent, and Alberto Casino Alegre. 2025. "Endo-Periodontal Lesions Without Root Damage: Recommendations for Clinical Management" Journal of Clinical Medicine 14, no. 18: 6655. https://doi.org/10.3390/jcm14186655
APA StyleAranda Verdú, S., Pallarés Sabater, A., Pallarés Serrano, A., Rubio Climent, J., & Casino Alegre, A. (2025). Endo-Periodontal Lesions Without Root Damage: Recommendations for Clinical Management. Journal of Clinical Medicine, 14(18), 6655. https://doi.org/10.3390/jcm14186655





