Accuracy of Navigated High-Speed Drill-Assisted Cervical and Upper Thoracic Pedicle Screw Placement—A Single Center Experience with 1112 Pedicle Screws
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CPS | Cervical pedicle screw |
| CT | Computed tomography |
References
- Abumi, K.; Itoh, H.; Taneichi, H.; Kaneda, K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: Description of the techniques and preliminary report. J. Spinal Disord. 1994, 7, 19–28. [Google Scholar] [CrossRef]
- Johnston, T.L.; Karaikovic, E.E.; Lautenschlager, E.P.; Marcu, D. Cervical pedicle screws vs. lateral mass screws: Uniplanar fatigue analysis and residual pullout strengths. Spine J. 2006, 6, 667–672. [Google Scholar] [CrossRef] [PubMed]
- Ito, Z.; Higashino, K.; Kato, S.; Kim, S.S.; Wong, E.; Yoshioka, K.; Hutton, W.C. Pedicle screws can be 4 times stronger than lateral mass screws for insertion in the midcervical spine: A biomechanical study on strength of fixation. J. Spinal Disord. Tech. 2014, 27, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Gan, G.; Kaliya-Perumal, A.K.; Yu, C.S.; Nolan, C.P.; Oh, J.Y. Spinal Navigation for Cervical Pedicle Screws: Surgical Pearls and Pitfalls. Global Spine J. 2021, 11, 196–202. [Google Scholar] [CrossRef]
- Panjabi, M.M.; Duranceau, J.; Goel, V.; Oxland, T.; Takata, K. Cervical human vertebrae. Quantitative three-dimensional anatomy of the middle and lower regions. Spine 1991, 16, 861–869. [Google Scholar] [CrossRef]
- Soliman, M.A.R.; Aguirre, A.O.; Khan, S.; Kuo, C.C.; Ruggiero, N.; Mariotti, B.L.; Fritz, A.G.; Sharma, S.; Nezha, A.; Levy, B.R.; et al. Complications associated with subaxial placement of pedicle screws versus lateral mass screws in the cervical spine (C2–T1): Systematic review and meta-analysis comprising 4165 patients and 16,669 screws. Neurosurg. Rev. 2023, 46, 61. [Google Scholar] [CrossRef]
- Kotani, Y.; Abumi, K.; Ito, M.; Minami, A. Improved accuracy of computer-assisted cervical pedicle screw insertion. J. Neurosurg. 2003, 99, 257–263. [Google Scholar] [CrossRef]
- Tarawneh, A.M.; Haleem, S.; D’Aquino, D.; Quraishi, N. The comparative accuracy and safety of fluoroscopic and navigation-based techniques in cervical pedicle screw fixation: Systematic review and meta-analysis. J. Neurosurg. Spine 2021, 35, 194–201. [Google Scholar] [CrossRef]
- Mahmoud, A.; Shanmuganathan, K.; Rocos, B.; Sedra, F.; Montgomery, A.; Aftab, S. Cervical Spine Pedicle Screw Accuracy in Fluoroscopic, Navigated and Template Guided Systems-A Systematic Review. Tomography 2021, 7, 614–622. [Google Scholar] [CrossRef]
- Gertzbein, S.D.; Robbins, S.E. Accuracy of pedicular screw placement in vivo. Spine 1990, 15, 11–14. [Google Scholar] [CrossRef]
- Bredow, J.; Oppermann, J.; Kraus, B.; Schiller, P.; Schiffer, G.; Sobottke, R.; Eysel, P.; Koy, T. The accuracy of 3D fluoroscopy-navigated screw insertion in the upper and subaxial cervical spine. Eur. Spine J. 2015, 24, 2967–2976. [Google Scholar] [CrossRef]
- Rienmüller, A.; Buchmann, N.; Kirschke, J.S.; Meyer, E.L.; Gempt, J.; Lehmberg, J.; Meyer, B.; Ryang, Y.M. Accuracy of CT-navigated pedicle screw positioning in the cervical and upper thoracic region with and without prior anterior surgery and ventral plating. Bone Jt. J. 2017, 99-B, 1373–1380. [Google Scholar] [CrossRef] [PubMed]
- Shree Kumar, D.; Ampar, N.; Wee Lim, L. Accuracy and reliability of spinal navigation: An analysis of over 1000 pedicle screws. J. Orthop. 2020, 18, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Bindels, B.J.J.; Dronkers, B.E.G.; Smits, M.L.J.; Verlaan, J.J. Accurate Placement and Revisions for Cervical Pedicle Screws Placed with or Without Navigation: A Systematic Review and Meta-Analysis. Glob. Spine J. 2024, 14, 1018–1037. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Cardozo, M.A.; Barot, K.; Brehm, S.; Bui, T.; Joseph, K.; Kann, M.R.; Trevino, G.; Olufawo, M.; Singh, S.; Yahanda, A.T.; et al. Pedicle screw placement in the cervical vertebrae using augmented reality-head mounted displays: A cadaveric proof-of-concept study. Spine J. 2024, 24, 2417–2427. [Google Scholar] [CrossRef]
- Ryu, S.; Ha, B.J.; Yoon, S.; Lee, C.K.; Shin, D.A.; Kim, K.N.; Yi, S. Feasibility and safety report on robotic assistance for cervical pedicle screw fixation: A cadaveric study. Sci. Rep. 2024, 14, 10881. [Google Scholar] [CrossRef]
- Ito, H.; Neo, M.; Yoshida, M.; Fujibayashi, S.; Yoshitomi, H.; Nakamura, T. Efficacy of computer-assisted pedicle screw insertion for cervical instability in RA patients. Rheumatol. Int. 2007, 27, 567–574. [Google Scholar] [CrossRef]
- Richter, M.; Mattes, T.; Cakir, B. Computer-assisted posterior instrumentation of the cervical and cervico-thoracic spine. Eur. Spine J. 2004, 13, 50–59. [Google Scholar] [CrossRef]
- Scheufler, K.M.; Franke, J.; Eckardt, A.; Dohmen, H. Accuracy of image-guided pedicle screw placement using intraoperative computed tomography-based navigation with automated referencing, part I: Cervicothoracic spine. Neurosurgery 2011, 69, 782–795; discussion 795. [Google Scholar] [CrossRef]
- Wu, J.; Fan, M.; He, D.; Wei, Y.; Duan, F.; Jiang, X.; Tian, W. Accuracy and clinical characteristics of robot-assisted cervical spine surgery: A systematic review and meta-analysis. Int. Orthop. 2024, 48, 1903–1914. [Google Scholar] [CrossRef]
- Beyer, R.S.; Nguyen, A.; Brown, N.J.; Gendreau, J.L.; Hatter, M.J.; Pooladzandi, O.; Pham, M.H. Spinal robotics in cervical spine surgery: A systematic review with key concepts and technical considerations. J. Neurosurg. Spine 2023, 38, 66–74. [Google Scholar] [CrossRef]
- Bydon, M.; Xu, R.; Amin, A.G.; Macki, M.; Kaloostian, P.; Sciubba, D.M.; Wolinsky, J.P.; Bydon, A.; Gokaslan, Z.L.; Witham, T.F. Safety and efficacy of pedicle screw placement using intraoperative computed tomography: Consecutive series of 1148 pedicle screws. J. Neurosurg. Spine 2014, 21, 320–328. [Google Scholar] [CrossRef]
- Faghih-Jouibari, M.; Moazzeni, K.; Amini-Navai, A.; Hanaei, S.; Abdollahzadeh, S.; Khanmohammadi, R. Anatomical considerations for insertion of pedicular screw in cervicothoracic junction. Iran. J. Neurol. 2016, 15, 228–231. [Google Scholar]
- Charles, Y.P.; Al Ansari, R.; Collinet, A.; De Marini, P.; Schwartz, J.; Nachabe, R.; Schäfer, D.; Brendel, B.; Gangi, A.; Cazzato, R.L. Accuracy Assessment of Percutaneous Pedicle Screw Placement Using Cone Beam Computed Tomography with Metal Artifact Reduction. Sensors 2022, 22, 4615. [Google Scholar] [CrossRef]
- Haleem, A.; Chiang, H.Y.; Vodela, R.; Behan, A.; Pottinger, J.M.; Smucker, J.; Greenlee, J.D.; Clark, C.; Herwaldt, L.A. Risk Factors for Surgical Site Infections Following Adult Spine Operations. Infect. Control Hosp. Epidemiol. 2016, 37, 1458–1467. [Google Scholar] [CrossRef]


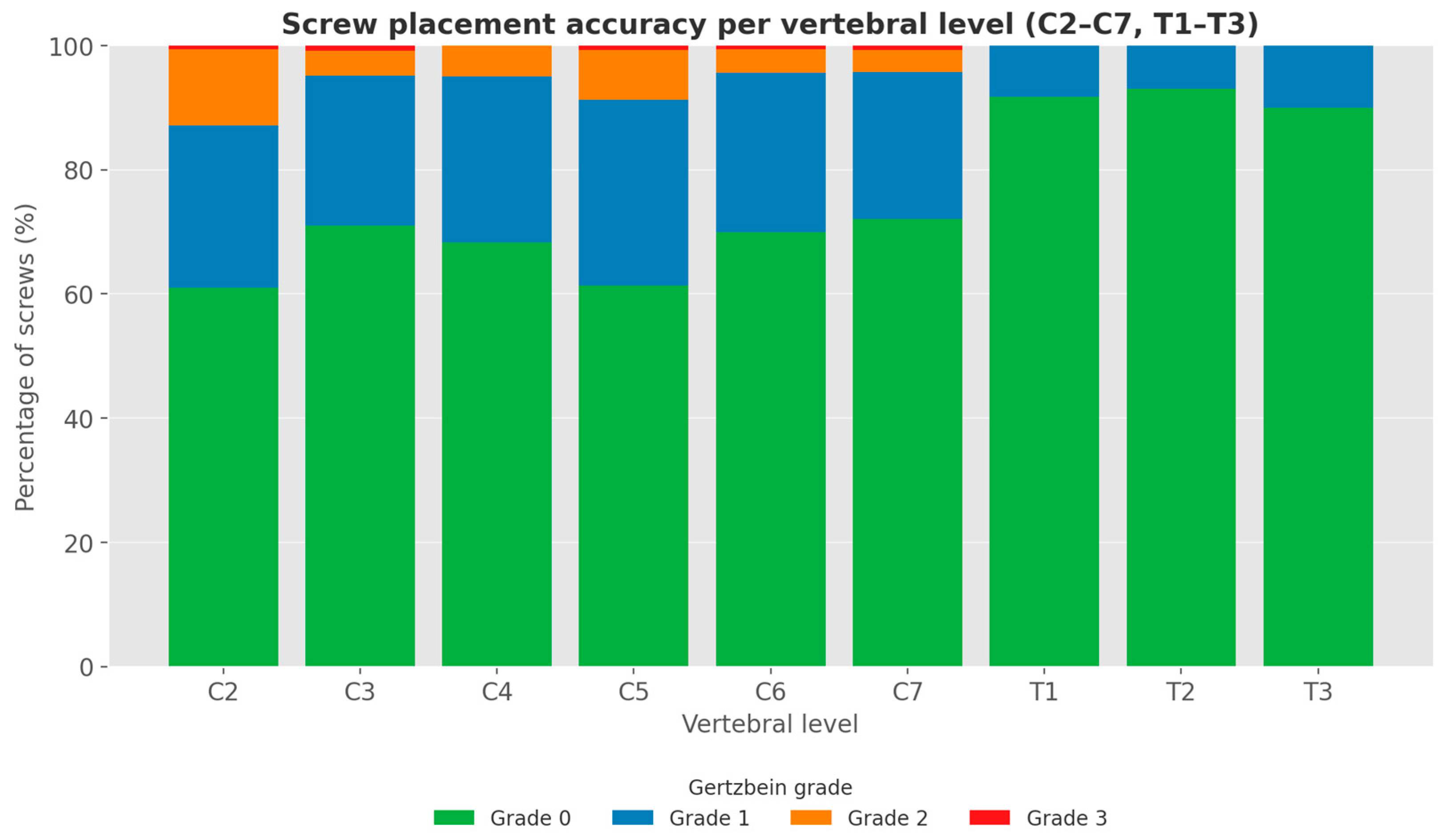

| Grade 0 (n) | Grade 1 (n) | Grade 2 (n) | Grade 3 (n) | Total | Grade 0 (%) | Grade 1 (%) | Grade 2 (%) | Grade 3 (%) | |
|---|---|---|---|---|---|---|---|---|---|
| C2 R | 56 | 22 | 10 | 0 | 88 | 63.6 | 25.0 | 11.4 | 0.0 |
| C2 L | 49 | 23 | 11 | 1 | 84 | 58.3 | 27.4 | 13.1 | 1.2 |
| C2 T | 105 | 45 | 21 | 1 | 172 | 61.0 | 26.2 | 12.2 | 0.6 |
| C3 R | 43 | 16 | 3 | 0 | 62 | 69.4 | 25.8 | 4.8 | 0.0 |
| C3 L | 45 | 14 | 2 | 1 | 62 | 72.6 | 22.6 | 3.2 | 1.6 |
| C3 T | 88 | 30 | 5 | 1 | 124 | 71.0 | 24.2 | 4.0 | 0.8 |
| C4 R | 51 | 20 | 2 | 0 | 73 | 69.9 | 27.4 | 2.7 | 0.0 |
| C4 L | 46 | 18 | 5 | 0 | 69 | 66.7 | 26.1 | 7.2 | 0.0 |
| C4 T | 97 | 38 | 7 | 0 | 142 | 68.3 | 26.8 | 4.9 | 0.0 |
| C5 R | 48 | 20 | 8 | 0 | 76 | 63.2 | 26.3 | 10.5 | 0.0 |
| C5 L | 44 | 25 | 4 | 1 | 74 | 59.5 | 33.8 | 5.4 | 1.4 |
| C5 T | 92 | 45 | 12 | 1 | 150 | 61.3 | 30.0 | 8.0 | 0.7 |
| C6 R | 58 | 17 | 4 | 1 | 80 | 72.5 | 21.2 | 5.0 | 1.2 |
| C6 L | 54 | 24 | 2 | 0 | 80 | 67.5 | 30.0 | 2.5 | 0.0 |
| C6 T | 112 | 41 | 6 | 1 | 160 | 70.0 | 25.6 | 3.8 | 0.6 |
| C7 R | 53 | 12 | 4 | 1 | 70 | 75.7 | 17.1 | 5.7 | 1.4 |
| C7 L | 48 | 21 | 1 | 0 | 70 | 68.6 | 30.0 | 1.4 | 0.0 |
| C7 T | 101 | 33 | 5 | 1 | 140 | 72.1 | 23.6 | 3.6 | 0.7 |
| T1 R | 61 | 5 | 0 | 0 | 66 | 92.4 | 7.6 | 0.0 | 0.0 |
| T1 L | 60 | 6 | 0 | 0 | 66 | 90.9 | 9.1 | 0.0 | 0.0 |
| T1 T | 121 | 11 | 0 | 0 | 132 | 91.7 | 8.3 | 0.0 | 0.0 |
| T2 R | 31 | 5 | 0 | 0 | 36 | 86.1 | 13.9 | 0.0 | 0.0 |
| T2 L | 36 | 0 | 0 | 0 | 36 | 100.0 | 0.0 | 0.0 | 0.0 |
| T2 T | 67 | 5 | 0 | 0 | 72 | 93.1 | 6.9 | 0.0 | 0.0 |
| T3 R | 8 | 2 | 0 | 0 | 10 | 80.0 | 20.0 | 0.0 | 0.0 |
| T3 L | 10 | 0 | 0 | 0 | 10 | 100.0 | 0.0 | 0.0 | 0.0 |
| T3 T | 18 | 2 | 0 | 0 | 20 | 90.0 | 10.0 | 0.0 | 0.0 |
| Total | 801 | 250 | 56 | 5 | 1112 | 72.0 | 22.5 | 5.0 | 0.4 |
| Cervical | 595 | 232 | 56 | 5 | 888 | 67.0% | 26.1% | 6.3% | 0.6% |
| Thoracic | 206 | 18 | 0 | 0 | 224 | 92.0% | 8.0% | 0.0 | 0.0 |
| Reason for Revision | n | % (of Cohort) | Time Interval * (Days) | Mean Time Interval (Days) | Note |
|---|---|---|---|---|---|
| Screw loosening | 7 | 3.4% | 28, 61, 97, 135, 152, 163, 233, 302 | 130.1 | In 2 cases, not CPS but lateral mass screw failure led to revision |
| Rebleeding | 6 | 2.9 | 0, 0, 0, 1, 1, 3 | 0.8 | |
| Wound healing disorder | 4 | 2.0 | 11, 28, 21 and 35 | 23.8 | |
| Total | 18 | 8.8 | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aspalter, S.; Stroh-Holly, N.; Höllmüller, K.; Davachi, A.; Rauch, P.; Heisinger, S.; Gruber, A.; Senker, W. Accuracy of Navigated High-Speed Drill-Assisted Cervical and Upper Thoracic Pedicle Screw Placement—A Single Center Experience with 1112 Pedicle Screws. J. Clin. Med. 2025, 14, 6597. https://doi.org/10.3390/jcm14186597
Aspalter S, Stroh-Holly N, Höllmüller K, Davachi A, Rauch P, Heisinger S, Gruber A, Senker W. Accuracy of Navigated High-Speed Drill-Assisted Cervical and Upper Thoracic Pedicle Screw Placement—A Single Center Experience with 1112 Pedicle Screws. Journal of Clinical Medicine. 2025; 14(18):6597. https://doi.org/10.3390/jcm14186597
Chicago/Turabian StyleAspalter, Stefan, Nico Stroh-Holly, Katja Höllmüller, Armin Davachi, Philip Rauch, Stephan Heisinger, Andreas Gruber, and Wolfgang Senker. 2025. "Accuracy of Navigated High-Speed Drill-Assisted Cervical and Upper Thoracic Pedicle Screw Placement—A Single Center Experience with 1112 Pedicle Screws" Journal of Clinical Medicine 14, no. 18: 6597. https://doi.org/10.3390/jcm14186597
APA StyleAspalter, S., Stroh-Holly, N., Höllmüller, K., Davachi, A., Rauch, P., Heisinger, S., Gruber, A., & Senker, W. (2025). Accuracy of Navigated High-Speed Drill-Assisted Cervical and Upper Thoracic Pedicle Screw Placement—A Single Center Experience with 1112 Pedicle Screws. Journal of Clinical Medicine, 14(18), 6597. https://doi.org/10.3390/jcm14186597





