Radiographic Analysis of Early Changes in Upper Adjacent Segments After Fusion Surgery: OLIF vs. PLIF
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Radiographic Evaluation
2.3. Patient-Reported Outcome Measures
2.4. Surgical Methods
2.5. Statistical Methods
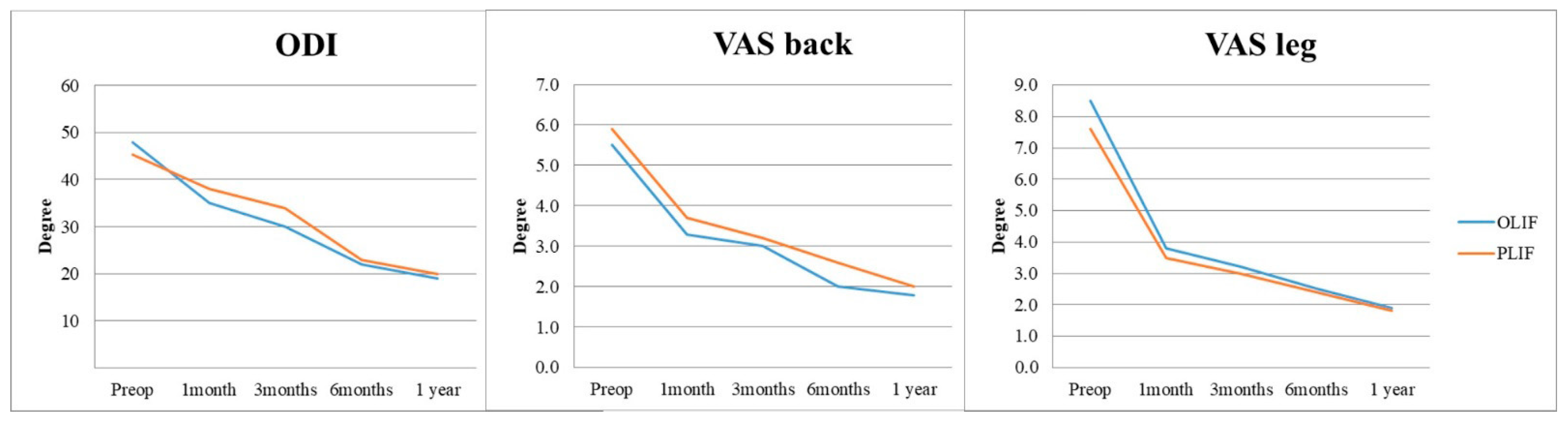
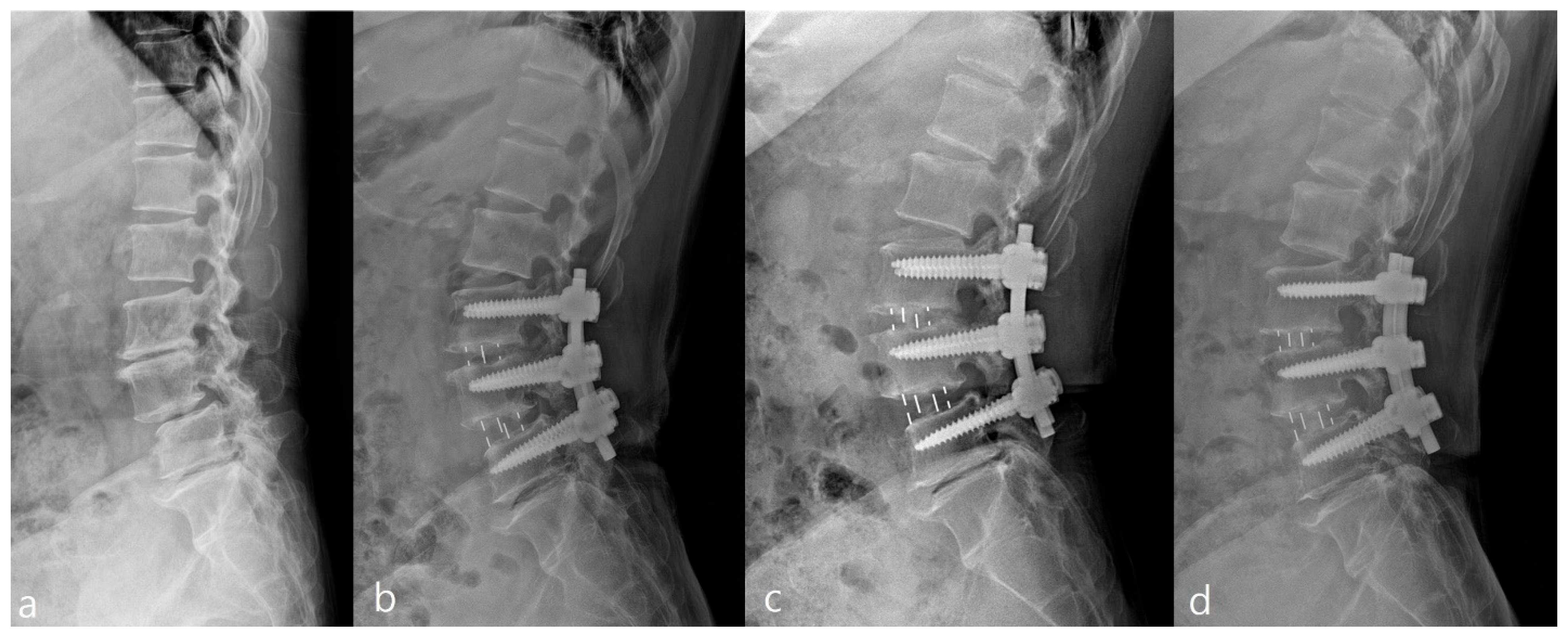
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bono, C.M.; Lee, C.K. Critical analysis of trends in fusion for degenerative disc disease over the past 20 years: Influence of technique on fusion rate and clinical outcome. Spine 2004, 29, 455–463. [Google Scholar] [CrossRef]
- Wei, X.; Yamato, Y.; Hasegawa, T.; Yoshida, G.; Banno, T.; Oe, S.; Arima, H.; Ide, K.; Yamada, T.; Kurosu, K. Adjacent segment degeneration at a minimum 2-year follow-up after posterior lumbar interbody fusion: The impact of sagittal spinal proportion: A retrospective case series. Asian Spine J. 2024, 18, 681–689. [Google Scholar] [CrossRef]
- Cannizzaro, D.; Anania, C.D.; De Robertis, M.; Pizzi, A.; Gionso, M.; Ballabio, C.; Ubezio, M.C.; Frigerio, G.M.; Battaglia, M.; Morenghi, E. The lumbar adjacent-level syndrome: Analysis of clinical, radiological, and surgical parameters in a large single-center series. J. Neurosurg. Spine 2023, 39, 479–489. [Google Scholar] [CrossRef] [PubMed]
- Mobbs, R.J.; Phan, K.; Malham, G.; Seex, K.; Rao, P.J. Lumbar interbody fusion: Techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J. Spine Surg. 2015, 1, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, C.L.; Macwan, K.; Sundararajan, K.; Rampersaud, R.Y. Comparative outcomes of minimally invasive surgery for posterior lumbar fusion: A systematic review. Clin. Orthop. Relat. Res. 2014, 472, 1727–1737. [Google Scholar] [CrossRef]
- Hero, N.; Topolovec, M. Comparative analysis of combined (first anterior, then posterior) versus only posterior approach for treating severe scoliosis: A mean follow up of 8.5 years. Spine 2017, 42, 831–837. [Google Scholar] [CrossRef] [PubMed]
- Ricciardi, L.; Piazza, A.; Capobianco, M.; Della Pepa, G.M.; Miscusi, M.; Raco, A.; Scerrati, A.; Somma, T.; Lofrese, G.; Sturiale, C.L. Lumbar interbody fusion using oblique (OLIF) and lateral (LLIF) approaches for degenerative spine disorders: A meta-analysis of the comparative studies. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 1–7. [Google Scholar] [CrossRef]
- Seaton, M.P.C.; Hirshman, B.R.; Kim, T.Y.; Pham, M.H. Radiological outcomes of static and expandable cage placement in minimally invasive oblique lumbar interbody fusion: A retrospective study. Asian Spine J. 2025. [Google Scholar] [CrossRef]
- Stoll, T.M.; Dubois, G.; Schwarzenbach, O. The dynamic neutralization system for the spine: A multi-center study of a novel non-fusion system. Eur. Spine J. 2002, 11, S170–S178. [Google Scholar] [CrossRef]
- Du, C.-F.; Cai, X.-Y.; Gui, W.; Sun, M.-S.; Liu, Z.-X.; Liu, C.-J.; Zhang, C.-Q.; Huang, Y.-P. Does oblique lumbar interbody fusion promote adjacent degeneration in degenerative disc disease: A finite element analysis. Comput. Biol. Med. 2021, 128, 104122. [Google Scholar] [CrossRef]
- Koslosky, E.; Gendelberg, D. Classification in brief: The Meyerding classification system of spondylolisthesis. Clin. Orthop. Relat. Res. 2020, 478, 1125–1130. [Google Scholar] [CrossRef]
- Lee, S.; Lee, J.W.; Yeom, J.S.; Kim, K.-J.; Kim, H.-J.; Chung, S.K.; Kang, H.S. A Practical MRI Grading System for Lumbar Foraminal Stenosis. Am. J. Roentgenol. 2010, 194, 1095–1098. [Google Scholar] [CrossRef]
- Griffith, J.F.; Wang, Y.-X.J.; Antonio, G.E.; Choi, K.C.; Yu, A.; Ahuja, A.T.; Leung, P.C. Modified Pfirrmann grading system for lumbar intervertebral disc degeneration. Spine 2007, 32, E708–E712. [Google Scholar] [CrossRef]
- Weishaupt, D.; Zanetti, M.; Boos, N.; Hodler, J. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skelet. Radiol. 1999, 28, 215–219. [Google Scholar] [CrossRef]
- Chang, M.C.; Kim, G.-U.; Choo, Y.J.; Lee, G.W. Transforaminal lumbar interbody fusion (TLIF) versus oblique lumbar interbody fusion (OLIF) in interbody fusion technique for degenerative spondylolisthesis: A systematic review and meta-analysis. Life 2021, 11, 696. [Google Scholar] [CrossRef] [PubMed]
- An, B.; Ren, B.; Han, Z.; Mao, K.; Liu, J. Comparison between oblique lumbar interbody fusion and posterior lumbar interbody fusion for the treatment of lumbar degenerative diseases: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2023, 18, 856. [Google Scholar] [CrossRef] [PubMed]
- Woods, K.R.; Billys, J.B.; Hynes, R.A. Technical description of oblique lateral interbody fusion at L1–L5 (OLIF25) and at L5–S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. 2017, 17, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, H.; Abbasi, A. Oblique Lateral Lumbar Interbody Fusion (OLLIF): Technical Notes and Early Results of a Single Surgeon Comparative Study. Cureus 2015, 7, e351. [Google Scholar] [CrossRef]
- Wong, A.X.J.; Tang, D.H.; Kaliya-Perumal, A.K.; Oh, J.Y. The Evolution of Lateral Lumbar Interbody Fusion: A Journey from Past to Present. Medicina 2024, 60, 378. [Google Scholar] [CrossRef]
- Antonacci, C.L.; Zeng, F.; Jackson, C.; Wellington, I.J.; Patel, S.M.; Esmende, S.M. Lateral interbody fusion for adjacent segment disease: A narrative review. J. Spine Surg. 2024, 10, 286–294. [Google Scholar] [CrossRef]
- Maragkos, G.A.; Atesok, K.; Papavassiliou, E. Prognostic factors for adjacent segment disease after L4–L5 lumbar fusion. Neurosurgery 2020, 86, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Yee, T.J.; Terman, S.W.; La Marca, F.; Park, P. Comparison of adjacent segment disease after minimally invasive or open transforaminal lumbar interbody fusion. J. Clin. Neurosci. 2014, 21, 1796–1801. [Google Scholar] [CrossRef]
- Tan, L.; Du, X.; Tang, R.; Rong, L.; Zhang, L. Preoperative Adjacent Facet Joint Osteoarthritis Is Associated with the Incidence of Adjacent Segment Degeneration and Low Back Pain after Lumbar Interbody Fusion. Asian Spine J 2024, 18, 21–31. [Google Scholar] [CrossRef]
- Nakajima, H.; Watanabe, S.; Honjoh, K.; Kubota, A.; Matsumine, A. Risk factors for early-onset adjacent segment degeneration after one-segment posterior lumbar interbody fusion. Sci. Rep. 2024, 14, 9145. [Google Scholar] [CrossRef]
- Anandjiwala, J.; Seo, J.-Y.; Ha, K.-Y.; Oh, I.-S.; Shin, D.-C. Adjacent segment degeneration after instrumented posterolateral lumbar fusion: A prospective cohort study with a minimum five-year follow-up. Eur. Spine J. 2011, 20, 1951–1960. [Google Scholar] [CrossRef] [PubMed]
- Toivonen, L.A.; Mäntymäki, H.; Benneker, L.M.; Kautiainen, H.; Neva, M.H. Effect of Baseline Adjacent Segment Degeneration on Clinical Outcomes After Lumbar Fusion. Glob. Spine J. 2025, 15, 3093–3100. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, F. Correlation between Peripheric Blood Markers and Surgical Invasiveness During Humeral Shaft Fracture Osteosynthesis in Young and Middle-Aged Patients. Diagnostics 2024, 14, 1112. [Google Scholar] [CrossRef] [PubMed]

| Group O (n = 95) | Group P (n = 141) | p-Value | |
|---|---|---|---|
| Age | 65.07 ± 8.22 | 63.41 ± 7.68 | 0.133 |
| Sex | 0.614 | ||
| male | 26 | 41 | |
| female | 69 | 100 | |
| Smoking | 0.880 | ||
| Non-smoker | 43 | 67 | |
| smoker | 52 | 74 | |
| Level | 0.997 | ||
| L3-4 | 29 | 46 | |
| L4-5 | 55 | 83 | |
| L3-4-5 | 11 | 12 | |
| Lumbar Lordosis | 50.75 ± 8.23 | 48.35 ± 12.78 | 0.502 |
| Pelvic Incidence | 53.47 ± 10.70 | 51.83 ± 10.64 | 0.216 |
| Disc height (mm) | 7.80 ± 3.16 | 7.91 ± 2.44 | 0.487 |
| Upper Segment Radiological Parameter | |||
| Foraminal height (mm) | 19.53 ± 2.05 | 20.1 ± 3.01 | 0.194 |
| Segmental Lordosis (°) | 8.15 ± 3.18 | 7.75 ± 3.88 | 0.379 |
| Flexibility (°) | 7.64 ± 2.05 | 7.49 ± 3.88 | 0.515 |
| Disc degeneration (Pfirrmann Gr.) | 2.33 ± 0.062 | 2.44 ± 0.59 | 0.267 |
| Facet sagitallization (°) | 69.16 ± 9.04 | 71.19 ± 12.62 | 0.259 |
| Facet degeneration (Weishaupt Gr.) | 2.16 ± 0.69 | 2.36 ± 0.48 | 0.085 |
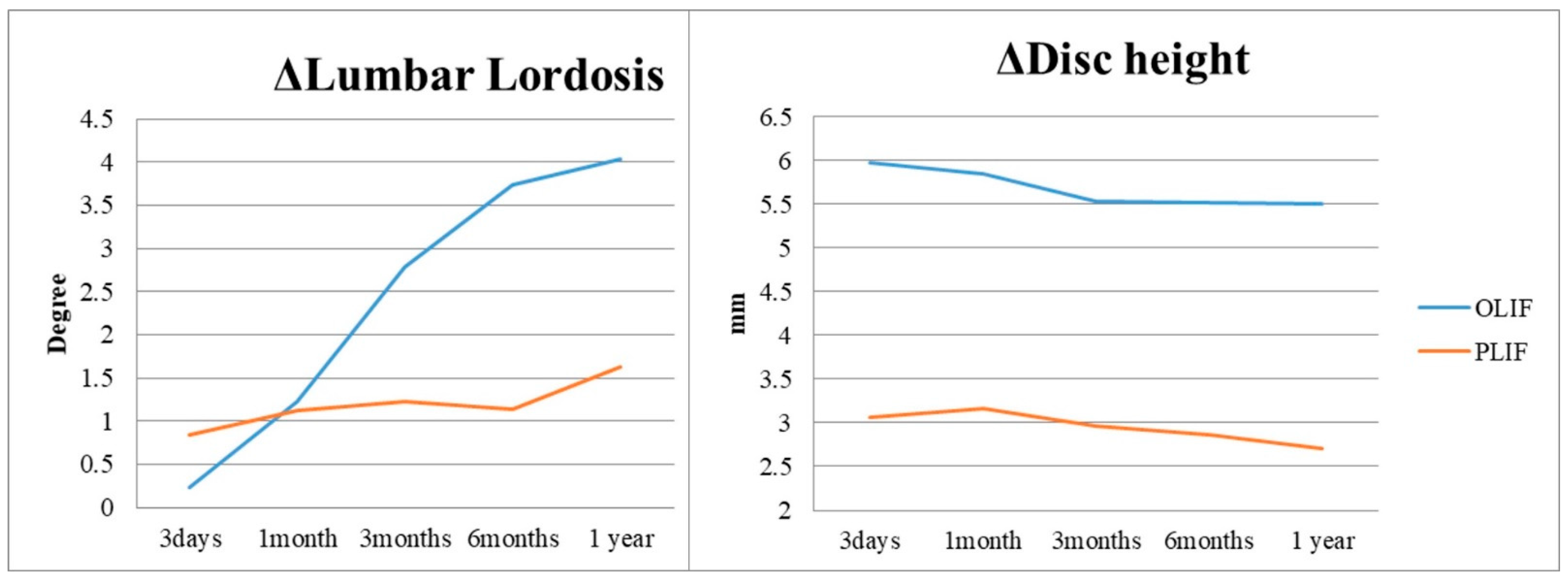
| 3 Days | 1 Month | 3 Months | 6 Months | 1 Year | |
|---|---|---|---|---|---|
| ΔLL(°) | |||||
| Group O | 0.23 ± 4.11 | 1.23 ± 4.26 | 2.78 ± 4.32 | 3.74. ± 4.13 | 4.03 ± 4.38 |
| Group P | 0.84 ± 6.70 | 1.13 ± 4.87 | 1.23 ± 5.71 | 1.14 ± 5.06 | 1.63 ± 5.11 |
| p-value | 0.609 | 0.495 | 0.036 * | <0.000 * | 0.001 * |
| ΔDisc height (mm) | |||||
| Group O | 5.97 ± 3.14 | 5.84 ± 3.07 | 5.53 ± 3.53 | 5.52 ± 3.45 | 5.50 ± 3.39 |
| Group P | 3.07 ± 2.20 | 3.16 ± 2.23 | 2.96 ± 2.32 | 2.87 ± 2.33 | 2.71 ± 2.18 |
| p-value | <0.000 * | <0.000 * | <0.000 * | <0.000 * | <0.000 * |
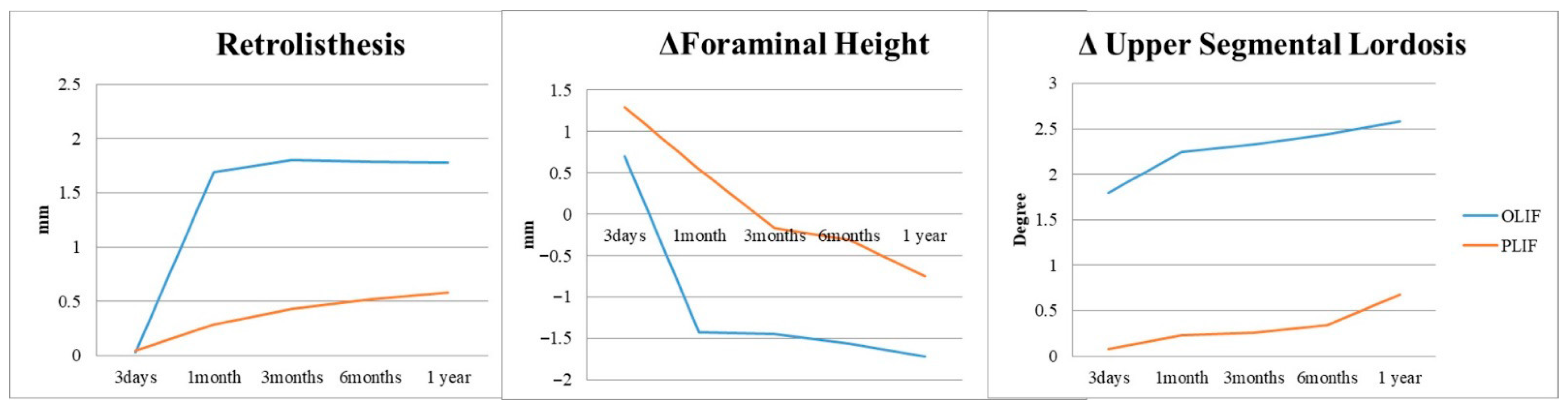
| ΔUpper seg. Retro-incidence (%) | |||||
| Group O | 6.1 | 76.9 | 80 | 83.1 | 83.1 |
| Group P | 2.9 | 24.6 | 29.8 | 31.3 | 34.3 |
| p-value | 0.12 | <0.000 * | <0.000 * | <0.000 * | <0.000 * |
| ΔUpper seg. Retrolisthesis (mm) | |||||
| Group O | 0.03 ± 0.14 | 1.69 ± 1.09 | 1.80 ± 1.33 | 1.79 ± 1.28 | 1.78 ± 1.10 |
| Group P | 0.05 ± 0.78 | 0.29 ± 0.70 | 0.43 ± 0.75 | 0.52 ± 0.91 | 0.58 ± 0.98 |
| p-value | 0.305 | <0.000 * | <0.000 * | <0.000 * | <0.000 * |
| ΔUpper seg. FH (mm) | |||||
| Group O | 0.70 ± 0.78 | −1.43 ± 2.12 | −1.45 ± 2.82 | −1.56 ± 2.07 | −1.72 ± 1.81 |
| Group P | 1.3 ± 2.72 | 0.54 ± 2.53 | −0.16 ± 2.42 | −0.75 ± 2.72 | −0.75 ± 2.72 |
| p-value | 0.155 | <0.000 * | 0.03 * | 0.037 * | 0.035 * |
| ΔUpper seg. Lordosis (°) | |||||
| Group O | 1.8 ± 4.39 | 2.24 ± 3.55 | 2.33 ± 3.57 | 2.44 ± 3.65 | 2.58 ± 3.17 |
| Group P | 0.08 ± 3.35 | 0.23 ± 3.75 | 0.26 ± 3.17 | 0.34 ± 3.02 | 0.68 ± 2.63 |
| p-value | 0.001 * | <0.000 * | <0.000 * | <0.000 * | 0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Cho, J.; Lee, D.-H.; Hwang, C.; Park, S. Radiographic Analysis of Early Changes in Upper Adjacent Segments After Fusion Surgery: OLIF vs. PLIF. J. Clin. Med. 2025, 14, 6570. https://doi.org/10.3390/jcm14186570
Lee J, Cho J, Lee D-H, Hwang C, Park S. Radiographic Analysis of Early Changes in Upper Adjacent Segments After Fusion Surgery: OLIF vs. PLIF. Journal of Clinical Medicine. 2025; 14(18):6570. https://doi.org/10.3390/jcm14186570
Chicago/Turabian StyleLee, JooYoung, JaeHwan Cho, Dong-Ho Lee, ChangJu Hwang, and SeHan Park. 2025. "Radiographic Analysis of Early Changes in Upper Adjacent Segments After Fusion Surgery: OLIF vs. PLIF" Journal of Clinical Medicine 14, no. 18: 6570. https://doi.org/10.3390/jcm14186570
APA StyleLee, J., Cho, J., Lee, D.-H., Hwang, C., & Park, S. (2025). Radiographic Analysis of Early Changes in Upper Adjacent Segments After Fusion Surgery: OLIF vs. PLIF. Journal of Clinical Medicine, 14(18), 6570. https://doi.org/10.3390/jcm14186570






