Clinical Outcomes of Radial Collateral Ligament Repair in Recalcitrant Lateral Epicondylitis with Mild Elbow Instability Following Repeated Steroid Injections
Abstract
1. Introduction
1.1. Study Design and Patient Selection
- -
- Age between 30 and 70 years.
- -
- Clinical and radiologic diagnosis of chronic lateral epicondylitis.
- -
- Failure of ≥1 year of conservative management.
- -
- Availability of complete medical records and ≥12 months follow-up.
- -
- Prior fracture or dislocation around the elbow.
- -
- Systemic inflammatory diseases (e.g., rheumatoid arthritis).
- -
- Full-thickness tears of the common extensor origin on MRI.
- -
- Workers’ compensation or ongoing legal disputes related to the elbow.
1.2. Evaluation of Instability
- Lateral joint line tenderness and pain during the varus stress test on physical examination. This apparent discrepancy with normal CSRA in some cases reflects the possibility of symptomatic minor instability detectable only under anesthesia or dynamic testing.
- Increased T2-weighted signal intensity of the lateral ligament complex on MRI.
- Positive intraoperative fluoroscopic varus stress test under anesthesia.
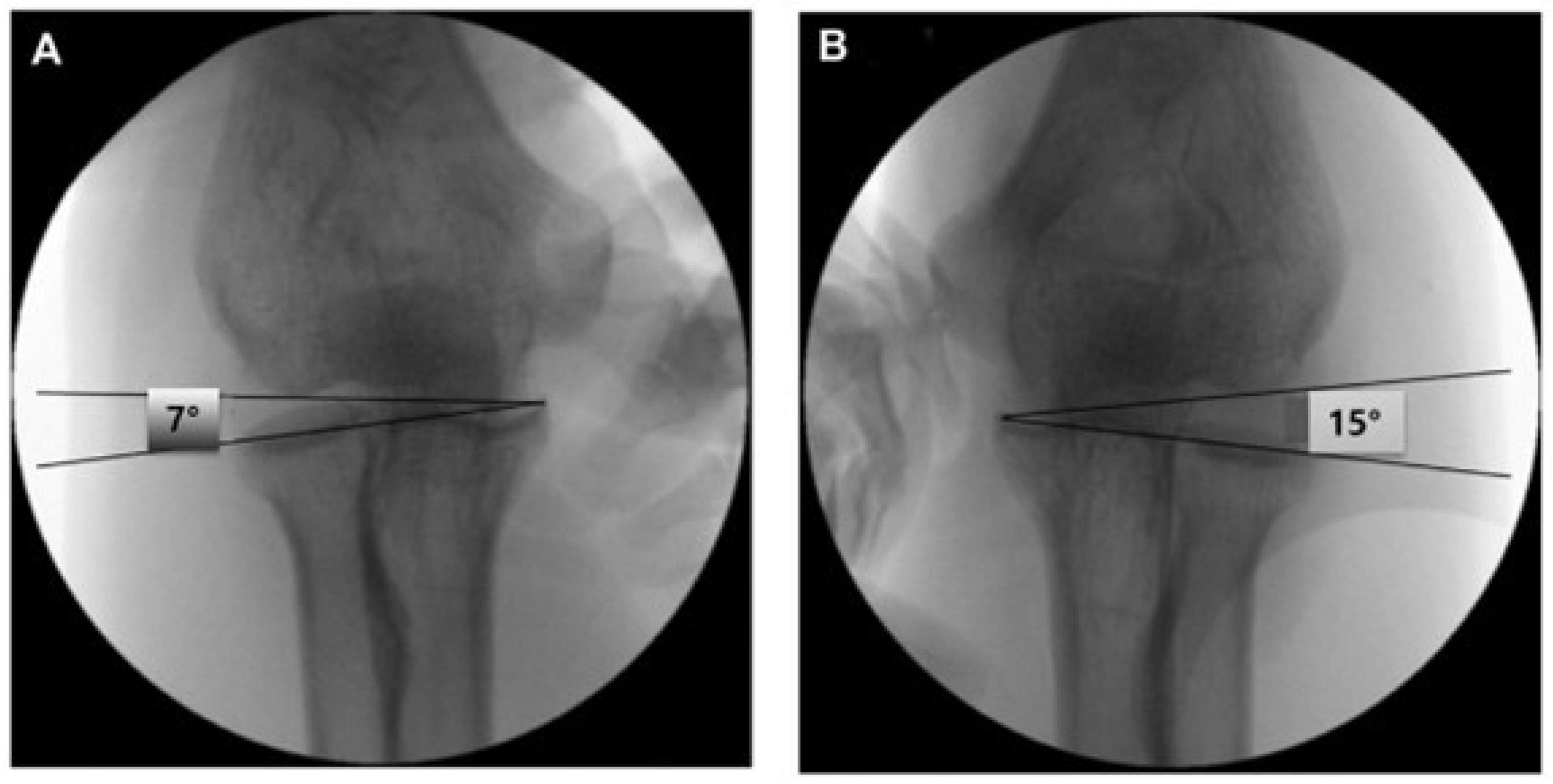
- A capitellum–sublime tubercle–radial head angle (CSRA) greater than 5° compared with the contralateral side. (Figure 2) This threshold was adopted based on previous studies that demonstrated its diagnostic utility in detecting subtle lateral elbow instability [13]. The CSRA measurement reflects subtle changes in joint alignment, aiding diagnosis of minor instability in this population.
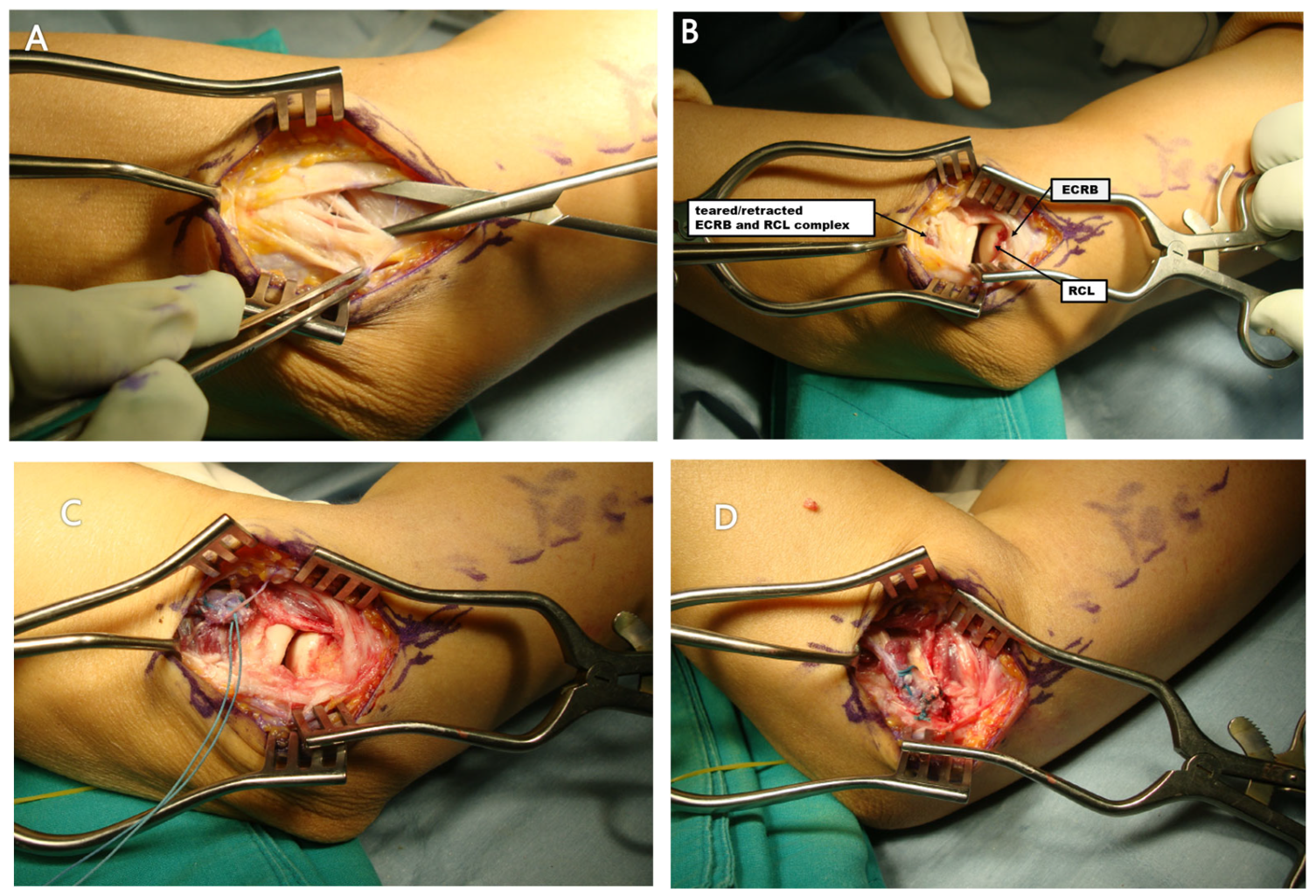
1.3. Operative Technique
- -
- Unstable Group
- -
- Stable group
1.4. Postoperative Rehabilitation
1.5. Clinical Outcome Measures
- -
- Visual Analog Scale (VAS) for pain.
- -
- Mayo Elbow Performance Score (MEPS).
- -
- Disabilities of the Arm, Shoulder and Hand (DASH) score.
- -
- Range of motion (ROM) in flexion and extension.
1.6. Statistical Analysis
2. Results
2.1. Patient Demographics
2.2. Trauma and Functional Impairment
2.3. Clinical Outcomes
2.4. Complications and Reoperation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Park, H.B.; Kam, M.; Gwark, J.Y. Association of steroid injection with soft-tissue calcification in lateral epicondylitis. J. Shoulder Elb. Surg. 2019, 28, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Cho, B.-K.; Kim, Y.-M.; Kim, D.-S.; Choi, E.-S.; Shon, H.-C.; Park, K.-J.; Lee, E.-M. Mini-open muscle resection procedure under local anesthesia for lateral and medial epicondylitis. Clin. Orthop. Surg. 2009, 1, 123–127. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nirschl, R.P.; Pettrone, F.A. Tennis elbow. The surgical treatment of lateral epicondylitis. J. Bone Jt. Surg. 1979, 61, 832–839. [Google Scholar] [CrossRef]
- Mi, B.; Liu, G.; Zhou, W.; Lv, H.; Liu, Y.; Wu, Q.; Liu, J. Platelet rich plasma versus steroid on lateral epicondylitis: Meta-analysis of randomized clinical trials. Physician Sportsmed. 2017, 45, 97–104. [Google Scholar] [CrossRef]
- Arirachakaran, A.; Sukthuayat, A.; Sisayanarane, T.; Laoratanavoraphong, S.; Kanchanatawan, W.; Kongtharvonskul, J. Platelet-rich plasma versus autologous blood versus steroid injection in lateral epicondylitis: Systematic review and network meta-analysis. J. Orthop. Traumatol. 2016, 17, 101–112. [Google Scholar] [CrossRef]
- Smidt, N.; van der Windt, D.A.; Assendelft, W.J.; Deville, W.L.; Korthals-de Bos, I.B.; Bouter, L.M. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: A randomised controlled trial. Lancet 2002, 359, 657–662. [Google Scholar] [CrossRef]
- Takigawa, N.; Ryu, J.; Kish, V.L.; Kinoshita, M.; Abe, M. Functional anatomy of the lateral collateral ligament complex of the elbow: Morphology and strain. J. Hand Surg. 2005, 30, 143–147. [Google Scholar] [CrossRef]
- Park, C.H.; Kim, B.S.; Lee, J.H.; Chung, S.G. Optimal Elbow Positions for Identification of the Radial Collateral Ligament Using Ultrasonography. PM R 2019, 12, 671–678. [Google Scholar] [CrossRef]
- Cohen, M.S. Lateral collateral ligament instability of the elbow. Hand Clin. 2008, 24, 69–77. [Google Scholar] [CrossRef]
- Zoner, C.S.; Buck, F.M.; Cardoso, F.N.; Gheno, R.; Trudell, D.J.; Randall, T.D.; Resnick, D. Detailed MRI-anatomic study of the lateral epicondyle of the elbow and its tendinous and ligamentous attachments in cadavers. Am. J. Roentgenol. 2010, 195, 629–636. [Google Scholar] [CrossRef]
- Park, J.Y.; Bang, J.Y. Spontaneous Rupture of the Extensor Carpi Radialis Brevis and Radial Collateral Ligament of the Elbow in a Recreational Golfer: Surgical Experience of Repair of a Chronic Retracted Tendon and Ligament. Clin. Shoulder Elb. 2016, 19, 39–42. [Google Scholar] [CrossRef][Green Version]
- Noh, Y.M.; Kong, G.M.; Moon, S.W.; Jang, H.S.; Kim, S.; Bak, G.G.; Kim, Y. Lateral ulnar collateral ligament (LUCL) reconstruction for the treatment of recalcitrant lateral epicondylitis of the elbow: A comparison with open debridement of the extensor origin. JSES Int. 2021, 5, 578–587. [Google Scholar] [CrossRef] [PubMed]
- Morrey, B.F.; An, K.N. Functional anatomy of the ligaments of the elbow. Clin. Orthop. Relat. Res. 1985, 201, 84–90. [Google Scholar] [CrossRef]
- Solheim, E.; Hegna, J.; Øyen, J.; Inderhaug, E. Arthroscopic versus open surgical release for lateral epicondylitis: 5-year results of a randomized controlled trial. J. Shoulder Elb. Surg. 2013, 22, e11–e15. [Google Scholar] [CrossRef]
- Dzugan, S.S.; Savoie, F.H.; Field, L.D., 3rd; O’Brien, M.J.; You, Z. Acute radial ulno-humeral ligament injury in patients with chronic lateral epicondylitis: An observational report. J. Shoulder Elb. Surg. 2012, 21, 1651–1655. [Google Scholar] [CrossRef]
- Kalainov, D.M.; Cohen, M.S. Posterolateral rotatory instability of the elbow in association with lateral epicondylitis. A report of three cases. J. Bone Jt. Surg. 2005, 87, 1120–1125. [Google Scholar] [CrossRef]
- Shim, J.W.; Yoo, S.H.; Park, M.J. Surgical management of lateral epicondylitis combined with ligament insufficiency. J. Shoulder Elb. Surg. 2018, 27, 1907–1912. [Google Scholar] [CrossRef]
- Moritomo, H.; Murase, T.; Arimitsu, S.; Oka, K.; Yoshikawa, H.; Sugamoto, K. The in vivo isometric point of the lateral ligament of the elbow. J. Bone Jt. Surg. 2007, 89, 2011–2017. [Google Scholar] [CrossRef]
- Arrigoni, P.; Cucchi, D.; Luceri, F.; Menon, A.; Zaolino, C.; Zagarella, A.; Catapano, M.; Radici, M.; Migliaccio, N.; Polli, D.; et al. Lateral Elbow Laxity Is Affected by the Integrity of the Radial Band of the Lateral Collateral Ligament Complex: A Cadaveric Model With Sequential Releases and Varus Stress Simulating Everyday Activities. Am. J. Sports Med. 2021, 49, 2332–2340. [Google Scholar] [CrossRef]
- Arrigoni, P.; Cucchi, D.; D’aMbrosi, R.; Butt, U.; Safran, M.R.; Denard, P.; Randelli, P. Intra-articular findings in symptomatic minor instability of the lateral elbow (SMILE). Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2255–2263. [Google Scholar] [CrossRef]
- Degen, R.M.; Cancienne, J.M.; Camp, C.L.; Altchek, D.W.; Dines, J.S.; Werner, B.C. Three or more preoperative injections is the most significant risk factor for revision surgery after operative treatment of lateral epicondylitis: An analysis of 3863 patients. J. Shoulder Elb. Surg. 2017, 26, 704–709. [Google Scholar] [CrossRef]
- Tempfer, H.; Gehwolf, R.; Lehner, C.; Wagner, A.; Mtsariashvili, M.; Bauer, H.-C.; Resch, H.; Tauber, M. Effects of crystalline glucocorticoid triamcinolone acetonide on cultered human supraspinatus tendon cells. Acta Orthop. 2009, 80, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Hugate, R.; Pennypacker, J.; Saunders, M.; Juliano, P. The effects of intratendinous and retrocalcaneal intrabursal injections of corticosteroid on the biomechanical properties of rabbit Achilles tendons. J. Bone Jt. Surg. 2004, 86, 794–801. [Google Scholar] [CrossRef] [PubMed]
- Wiggins, M.E.; Fadale, P.D.; Barrach, H.; Ehrlich, M.G.; Walsh, W.R. Healing characteristics of a type I collagenous structure treated with corticosteroids. Am. J. Sports Med. 1994, 22, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Mikolyzk, D.K.; Wei, A.S.; Tonino, P.; Marra, G.; Williams, D.A.; Himes, R.D.; Wezeman, F.H.; Callaci, J.J. Effect of corticosteroids on the biomechanical strength of rat rotator cuff tendon. J. Bone Jt. Surg. 2009, 91, 1172–1180. [Google Scholar] [CrossRef]
- Tillander, B.; Franzen, L.E.; Karlsson, M.H.; Norlin, R. Effect of steroid injections on the rotator cuff: An experimental study in rats. J. Shoulder Elb. Surg. 1999, 8, 271–274. [Google Scholar] [CrossRef]
- Arslan, I.; Yucel, I.; Ozturk, T.B.; Karahan, N.; Orak, M.M.; Midi, A. The Effects of Corticosteroid Injection in the Healthy and Damaged Achilles Tendon Model: Histopathological and Biomechanical Experimental Study in Rats. Turk. J. Pathol. 2019, 36, 39–47. [Google Scholar] [CrossRef]
- Morrey, B.F. Reoperation for failed surgical treatment of refractory lateral epicondylitis. J. Shoulder Elb. Surg. 1992, 1, 47–55. [Google Scholar] [CrossRef]

| Unstable Group | Stable Group | p-Value | |
|---|---|---|---|
| Sex, men/women | 5/7 | 31/49 | 0.135 |
| Age (mean ± SD), yr | 54 ± 1.8 | 51 ± 0.7 | 0.042 * |
| Involvement of dominant arm, n (%) | 8 (66) | 44 (55) | 0.908 |
| Case with steroid injection history, n (%) | 12 (100) | 62 (78) | 0.306 |
| Case with previous surgery, n (%) | 3 (25) | 0 (0) | 0.037 * |
| No. of steroid injections, mean ± SD | 3.4 ± 0.9 | 1.2 ± 0.7 | 0.024 * |
| Case with trauma history, n (%) | 2 (17) | 3 (3) | 0.097 |
| Preoperative | Postoperative | p-Value | |
| pVAS | 6.8 ± 1.5 | 1.4 ± 0.5 | 0.001 * |
| ROM | |||
| Flexion | 138 ± 9.1 | 143 ± 8.1 | 0.072 |
| Extension | 0.3 ± 3.2 | 1.2 ± 1.5 | 0.413 |
| DASH score | 47.1 ± 10.2 | 13.8 ± 3.8 | 0.001 * |
| MEPS | |||
| Total score | 53.0 ± 10.1 | 91.1 ± 10.7 | 0.001 * |
| Stability | 3.2 ± 1.1 | 10.0 ± 1.5 | 0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moon, S.W.; D’Lima, D.; Bang, J.-Y. Clinical Outcomes of Radial Collateral Ligament Repair in Recalcitrant Lateral Epicondylitis with Mild Elbow Instability Following Repeated Steroid Injections. J. Clin. Med. 2025, 14, 6474. https://doi.org/10.3390/jcm14186474
Moon SW, D’Lima D, Bang J-Y. Clinical Outcomes of Radial Collateral Ligament Repair in Recalcitrant Lateral Epicondylitis with Mild Elbow Instability Following Repeated Steroid Injections. Journal of Clinical Medicine. 2025; 14(18):6474. https://doi.org/10.3390/jcm14186474
Chicago/Turabian StyleMoon, Sang Won, Darryl D’Lima, and Jin-Young Bang. 2025. "Clinical Outcomes of Radial Collateral Ligament Repair in Recalcitrant Lateral Epicondylitis with Mild Elbow Instability Following Repeated Steroid Injections" Journal of Clinical Medicine 14, no. 18: 6474. https://doi.org/10.3390/jcm14186474
APA StyleMoon, S. W., D’Lima, D., & Bang, J.-Y. (2025). Clinical Outcomes of Radial Collateral Ligament Repair in Recalcitrant Lateral Epicondylitis with Mild Elbow Instability Following Repeated Steroid Injections. Journal of Clinical Medicine, 14(18), 6474. https://doi.org/10.3390/jcm14186474





