Confirmatory Study on Costs and Time Loss from Pre-Anesthetic Consultations for Canceled Surgeries: A Retrospective Analysis at Hannover Medical School, Germany
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Study Groups
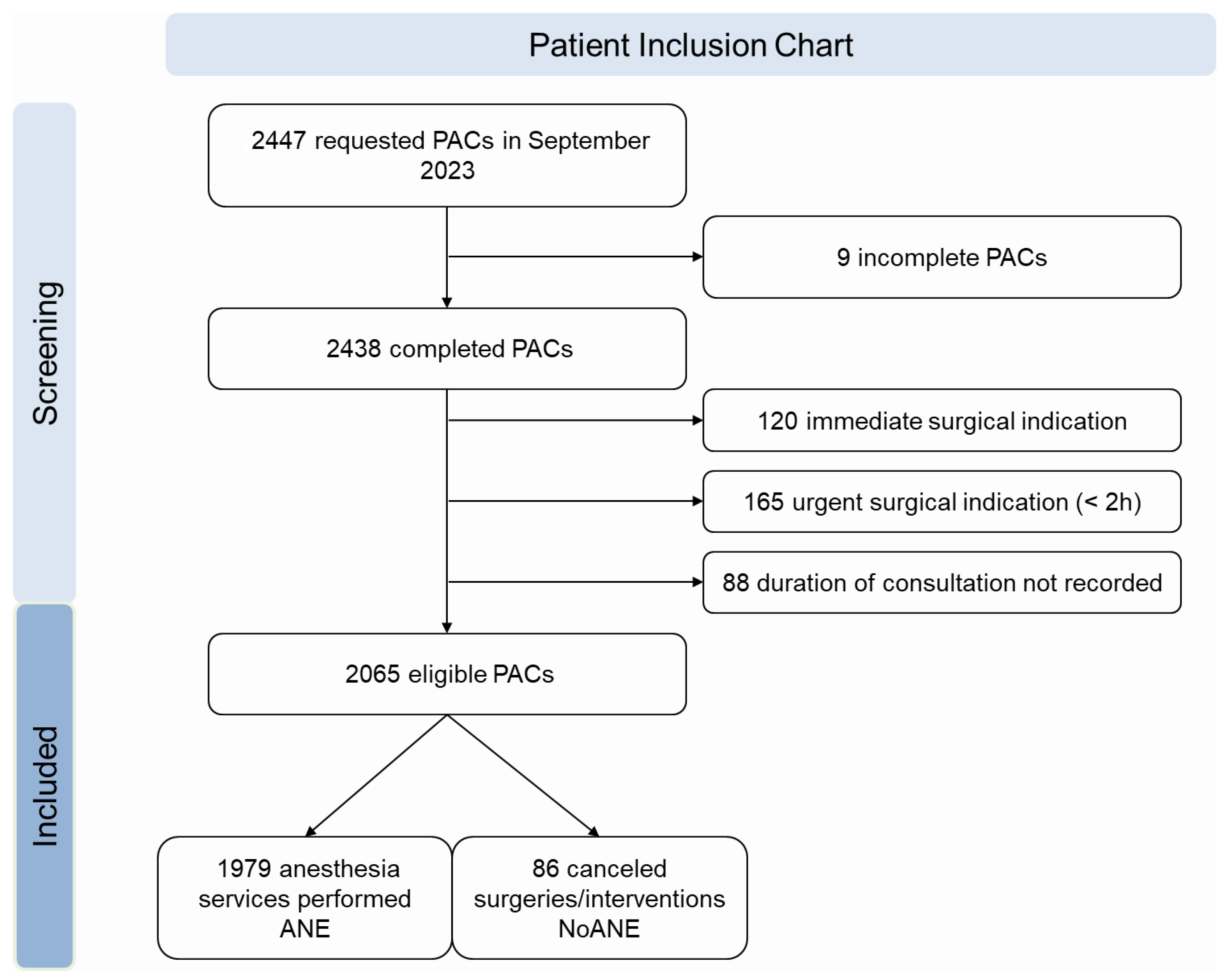
2.3. Inclusion and Exclusion Criteria
2.4. Cost and Time Calculations
2.5. Statistical Analysis
3. Results
3.1. Patient Inclusion and Exclusion Criteria
3.2. Patient Demographics and Clinical Characteristics
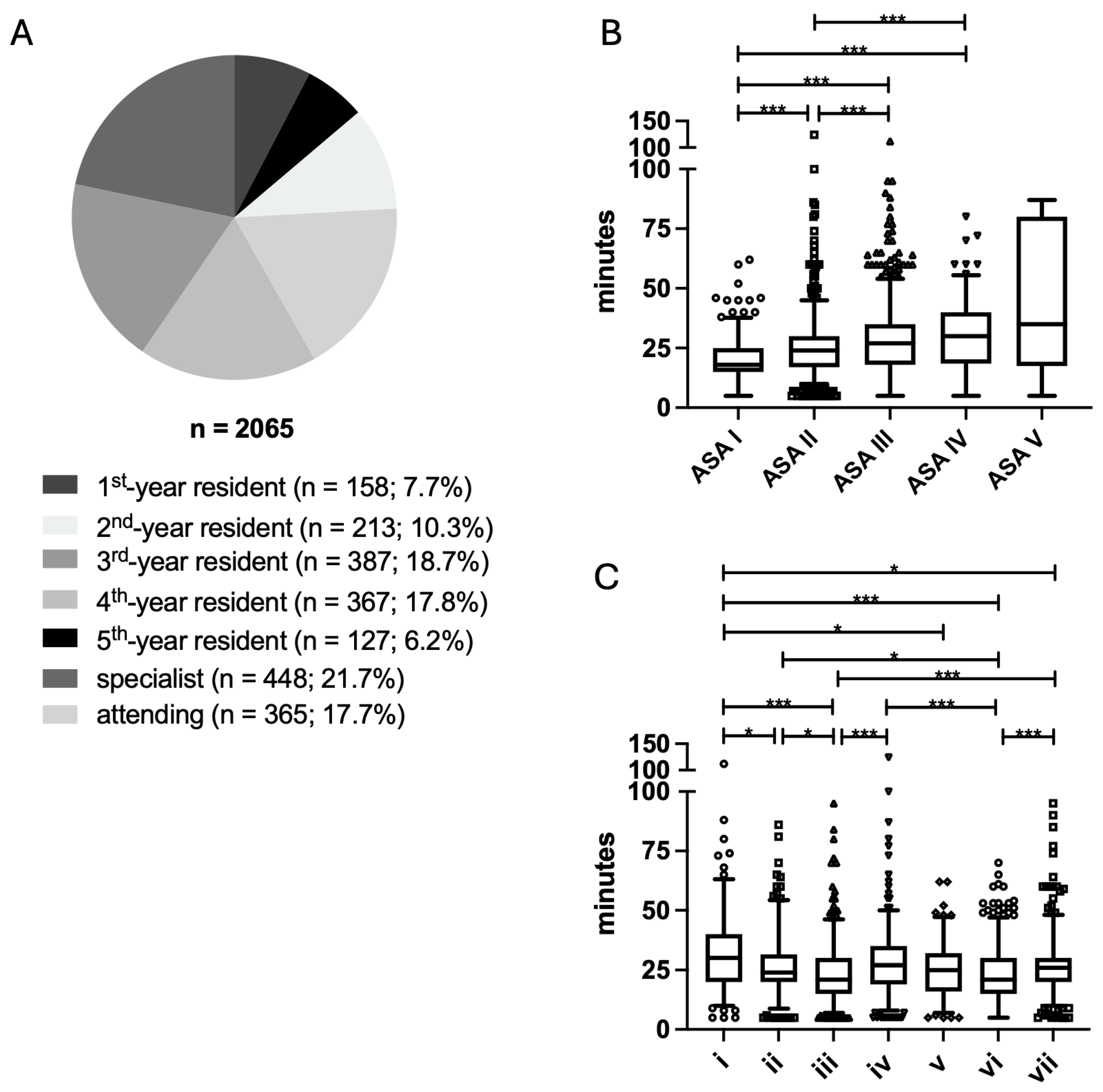
3.3. Training Levels of Anesthesiologists and Duration of PACs
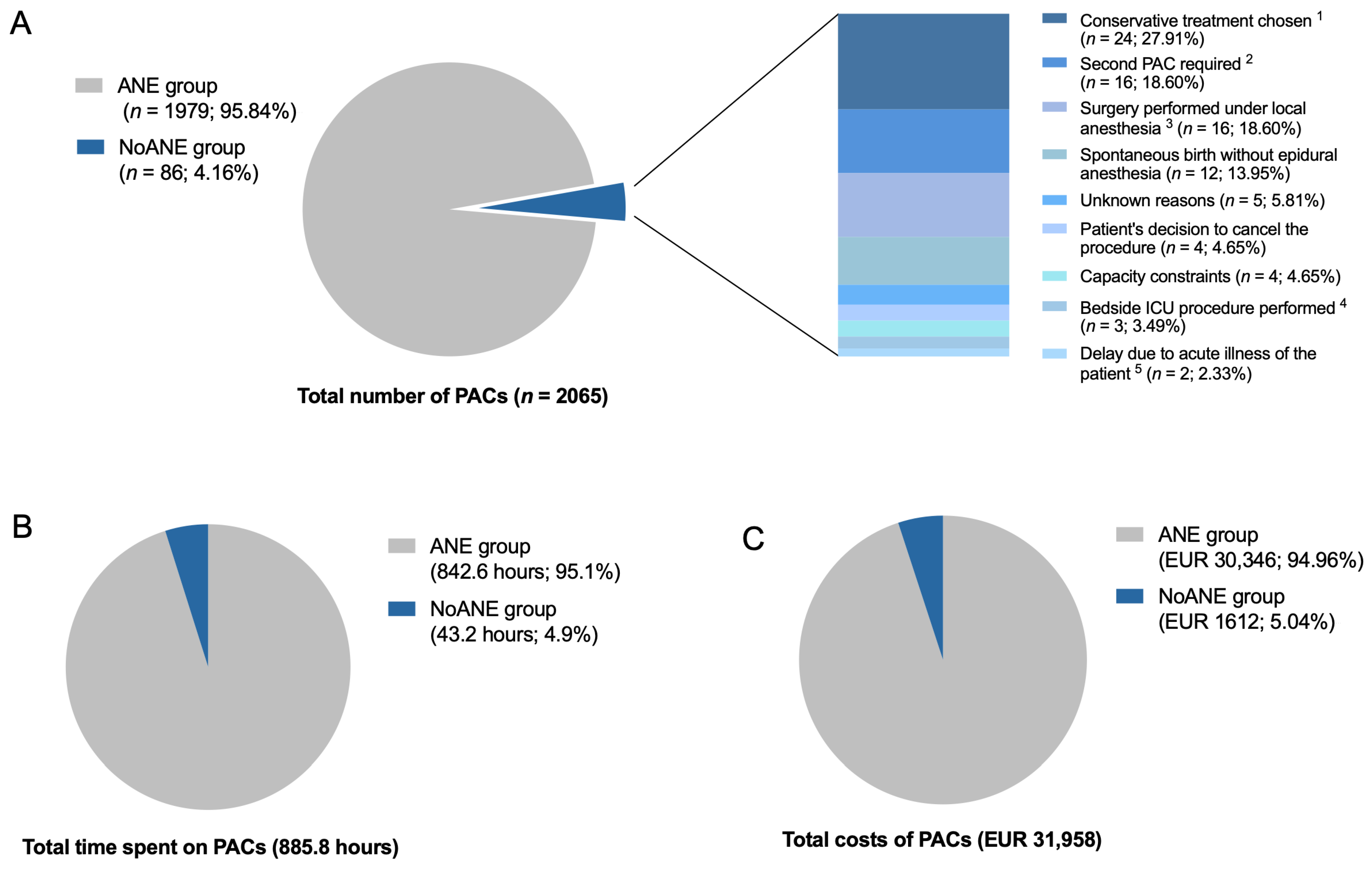
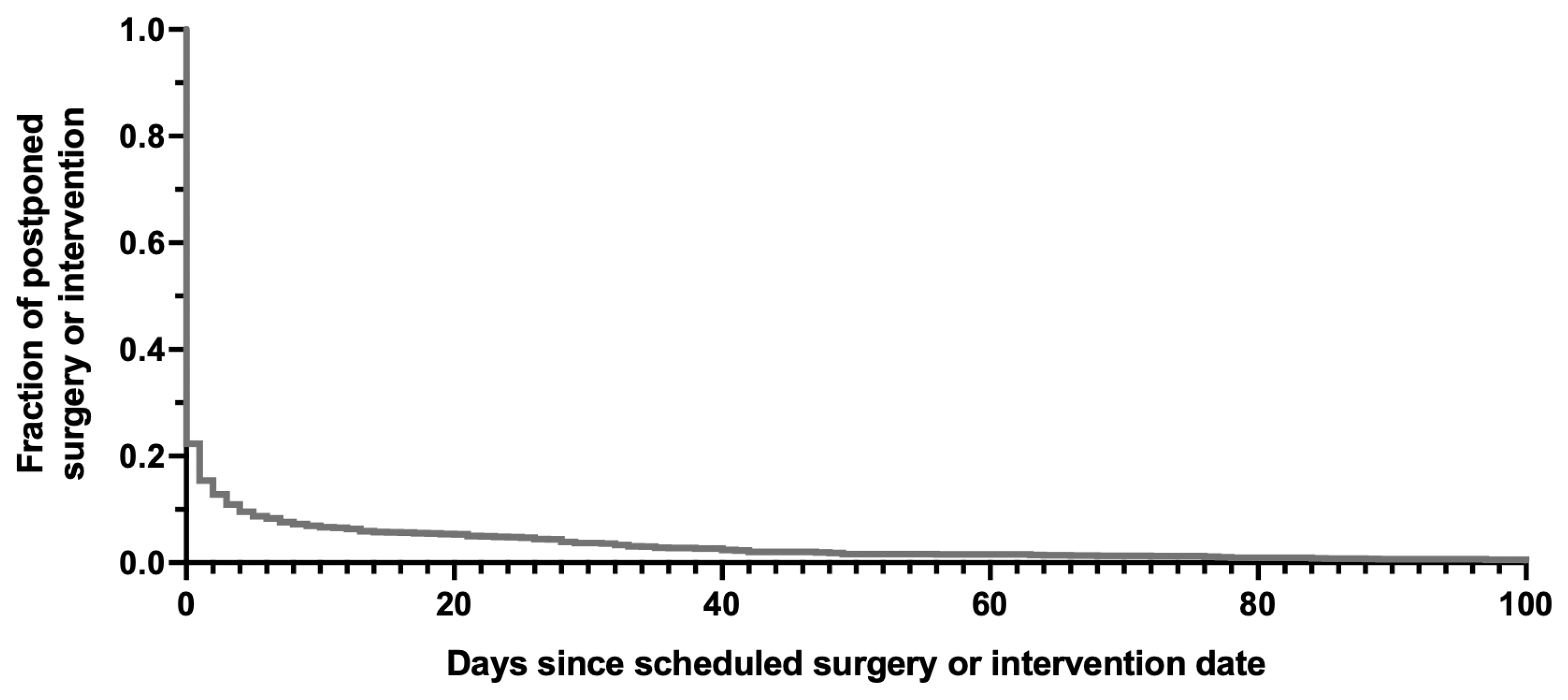
3.4. Overall Duration and Costs of PACs
3.5. Missing Test Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PAC | Pre-anesthetic consultation |
| ASA | American Society of Anesthesiology |
| ECG | Electrocardiogram |
| TTE | Transthoracic echocardiography |
| TEE | Transesophageal echocardiography |
References
- Die 20 Häufigsten Operationen Insgesamt (5). Statistisches Bundesamt. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Krankenhauser/Tabellen/drg-operationen-insgesamt.html (accessed on 24 May 2025).
- Einrichtungen, Betten und Patientenbewegung. Statistisches Bundesamt. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Krankenhauser/Tabellen/gd-krankenhaeuser-jahre.html (accessed on 24 May 2025).
- Bundesärztekammer. 2024. Available online: https://www.bundesaerztekammer.de/baek/ueber-uns/aerztestatistik/2024 (accessed on 1 June 2025).
- Ellinger, E.; Meybohm, P.; Röder, D. Perioperative Anesthesiologic Management: Risk Assessment and Preoperative Improvement of Patient Conditions. Anasthesiol. Intensiv. Notfallmed Schmerzther 2021, 56, 159–173. [Google Scholar]
- Ferschl, M.B.; Tung, A.; Sweitzer, B.; Huo, D.; Glick, D.B. Preoperative clinic visits reduce operating room cancellations and delays. Anesthesiology 2005, 103, 855–859. [Google Scholar] [CrossRef]
- Blitz, J.D.; Kendale, S.M.; Jain, S.K.; Cuff, G.E.; Kim, J.T.; Rosenberg, A.D. Preoperative Evaluation Clinic Visit Is Associated with Decreased Risk of In-hospital Postoperative Mortality. Anesthesiology 2016, 125, 280–294. [Google Scholar] [CrossRef]
- Cañón Pérez, A.; Marti-Scharfhausen Sánchez, M.D.L.R.; Sevilla Ureba, A.; Hernández Magaña, E.Z.; Viscasillas Monteagudo, J.; Martínez Albiñana, A.; Redondo, J.I. Influence of Comprehensive Pre-Anaesthetic Assessment on ASA Classification and Surgical Cancellations in Dogs and Cats: A Retrospective Observational Study. Vet. Sci. 2025, 12, 612. [Google Scholar] [CrossRef]
- van Klei, W.A.; Moons, K.G.; Rutten, C.L.; Schuurhuis, A.; Knape, J.T.; Kalkman, C.J.; Grobbee, D.E. The effect of outpatient preoperative evaluation of hospital inpatients on cancellation of surgery and length of hospital stay. Anesth. Analg. 2002, 94, 644–649. [Google Scholar] [CrossRef]
- Lee, A.; Chui, P.T.; Chiu, C.H.; Gin, T.; Ho, A.M. The cost-effectiveness of an outpatient anesthesia consultation clinic before surgery: A matched Hong Kong cohort study. Perioper. Med. 2012, 1, 3. [Google Scholar] [CrossRef][Green Version]
- Schuster, M.; Standl, T.; Wagner, J.A.; Berger, J.; Reimann, H.; Am Esch, J.S. Effect of different cost drivers on cost per anesthesia minute in different anesthesia subspecialties. Anesthesiology 2004, 101, 1435–1443. [Google Scholar] [CrossRef] [PubMed]
- Epstein, R.H.; Dexter, F. Management implications for the perioperative surgical home related to inpatient case cancellations and add-on case scheduling on the day of surgery. Anesth. Analg. 2015, 121, 206–218. [Google Scholar] [CrossRef] [PubMed]
- Simons, J.A.; Wiegand, S.B.; Thiehoff, L.; Winnersbach, P.; Schälte, G.; Fischbach, A. Costs and Time Loss from Pre-Anesthesia Consultations for Canceled Surgeries: A Retrospective Study at Aachen University Hospital in Germany. Anesth. Res. 2025, 2, 2. [Google Scholar] [CrossRef]
- Winter, V.; Schreyögg, J.; Thiel, A. Hospital staff shortages: Environmental and organizational determinants and implications for patient satisfaction. Health Policy 2020, 124, 380–388. [Google Scholar] [CrossRef]
- Glance, L.G.; Lustik, S.J.; Hannan, E.L.; Osler, T.M.; Mukamel, D.B.; Qian, F.; Dick, A.W. The Surgical Mortality Probability Model: Derivation and validation of a simple risk prediction rule for noncardiac surgery. Ann. Surg. 2012, 255, 696–702. [Google Scholar] [CrossRef]
- Broadway, P.J.; Jones, J.G. A method of costing anaesthetic practice. Anaesthesia 1995, 50, 56–63. [Google Scholar] [CrossRef]
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J.; et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inf. Assoc. 2020, 27, 957–962. [Google Scholar] [CrossRef]
- Johnsen, T.M.; Norberg, B.L.; Kristiansen, E.; Zanaboni, P.; Austad, B.; Krogh, F.H.; Getz, L. Suitability of Video Consultations During the COVID-19 Pandemic Lockdown: Cross-sectional Survey Among Norwegian General Practitioners. J. Med. Internet Res. 2021, 23, e26433. [Google Scholar] [CrossRef]
- Kornelsen, J.; Taylor, M.; Ebert, S.; Skinner, T.; Stoll, K. Rural patients’ experiences with anesthesia and surgical consultations in British Columbia: A survey-based comparison between virtual and in-person modalities. Digit. Health 2024, 10, 20552076241242667. [Google Scholar] [CrossRef]
- Aldawoodi, N.N.; Turner, K.; Patel, K.; Coughlin, E.; Mhaskar, R.; Streitmatter, C.; Hoffman, M.S.; Pow-Sang, J.M.; Ackerman, R.S. A Randomized Controlled Trial Comparing pre-anesthesia Evaluation via Telemedicine to In-Person at an NCI-Designated Comprehensive Cancer Center. Telemed. J. E Health 2025. [Google Scholar] [CrossRef]
- Grüßer, L.; Bayram, B.; Ziemann, S.; Wallqvist, J.; Wienhold, J.; Rossaint, R.; Derwall, M.; Follmann, A. Teleconsultation for Preoperative Anesthesia Evaluation: Identifying Environmental Potentials by Life Cycle Assessment. Telemed. J. E Health 2024, 30, e2050-8. [Google Scholar] [CrossRef] [PubMed]
- Kagerbauer, S.M.; Wißler, J.; Blobner, M.; Biegert, F.; Andonov, D.I.; Schneider, G.; Podtschaske, A.H.; Ulm, B.; Jungwirth, B. Anaesthesiologists’ guideline adherence in pre-operative evaluation: A retrospective observational study. Perioper. Med. 2024, 13, 64. [Google Scholar] [CrossRef]
- Mendes, F.F.; Mathias, L.A.d.S.T.; Duval Neto, G.F.; Birck, A.R. Impact of preoperative outpatient evaluation clinic on performance indicators. Rev. Bras. Anestesiol. 2005, 55, 175–187. [Google Scholar] [PubMed]
- Farasatkish, R.; Aghdaii, N.; Azarfarin, R.; Yazdanian, F. Can preoperative anesthesia consultation clinic help to reduce operating room cancellation rate of cardiac surgery on the day of surgery? Middle East. J. Anaesthesiol. 2009, 20, 93–96. [Google Scholar] [PubMed]
- Wongtangman, K.; Azimaraghi, O.; Freda, J.; Ganz-Lord, F.; Shamamian, P.; Bastien, A.; Mirhaji, P.; Himes, C.P.; Rupp, S.; Green-Lorenzen, S.; et al. Incidence and predictors of case cancellation within 24 h in patients scheduled for elective surgical procedures. J. Clin. Anesth. 2022, 83, 110987. [Google Scholar] [CrossRef] [PubMed]
- Nouvellon, E.; Cuvillon, P.; Ripart, J.; Riou, B. Regional Anesthesia and Eye Surgery. Anesthesiology 2010, 113, 1236. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | All Patients n = 2065 | ANE Group n = 1979 | NoANE Group n = 86 | p-Value |
|---|---|---|---|---|
| Age, years | 50 (31;70) | 50 (31;69) | 53 (35;76) | 0.359 |
| Sex assigned at birth (female/male) | 1001/1064 (48.5%/51.5%) | 952/1027 (48.1%/51.9%) | 49/37 (57.0%/42.0%) | 0.107 |
| ASA Score | 2 (2;3) | 2 (2;3) | 3 (2;3) | 0.174 |
| ASA I | 246 (11.9%) | 236 (11.9) | 10 (11.6%) | 0.934 |
| ASA II | 893 (43.2%) | 860 (43.5%) | 33 (38.4%) | 0.352 |
| ASA III | 772 (37.4%) | 742 (37.5%) | 30 (34.9%) | 0.624 |
| ASA IV | 149 (7.2%) | 136 (6.9%) | 13 (15.1%) | 0.004 |
| ASA V | 5 (0.2%) | 5 (0.3%) | 0 (0.0%) | >0.999 |
| Interval between PAC and initially scheduled surgery date, days | 1 (1;3) | 1 (1;3) | 3 (1;10) | <0.001 |
| Current PAC is a follow-up visit | 185 (9.0%) | 176 (8.9%) | 9 (10.5%) | 0.050 |
| 2nd anesthesiologist involved in PAC | 100 (4.8%) | 87 (4.4%) | 13 (15.1%) | <0.001 |
| Cardiac risk score [14] | low (low; medium) | low (low; medium) | medium (low; medium) | 0.303 |
| Low | 1048 (50.8%) | 1011 (51.1%) | 37 (43.0%) | 0.143 |
| Medium | 921 (44.6%) | 873 (44.1%) | 48 (55.8%) | 0.033 |
| High | 96 (4.6%) | 95 (4.8%) | 1 (1.2%) | 0.183 |
| Elective vs. non-elective surgery or intervention (24 h) | 1707/360 (82.7%/17.3%) | 1698/281 (85.8%/14.2%) | 9/79 (10.5%/89.5%) | 0.150 |
| Specialty | All Patients n = 2065 | Duration of PAC [min/Case] | Cost of PAC [EUR/Case] ± SD |
|---|---|---|---|
| Thoracic Surgery | 36 (1.7%) | 30.6 ± 13.5 | 20.00 ± 7.89 |
| Dentistry/Maxillofacial Surgery | 114 (5.5%) | 29.4 ± 14.5 | 19.20 ± 10.80 |
| Vascular Surgery | 17 (0.8%) | 29.2 ± 16.9 | 19.86 ± 12.92 |
| Gynecology | 269 (13.0%) | 26.6 ± 10.9 | 19.79 ± 9.13 |
| Internal Medicine | 74 (3.6%) | 30.4 ± 14.3 | 18.98 ± 8.55 |
| Cardiac Surgery | 168 (8.1%) | 28.2 ± 12.7 | 18.91 ± 8.14 |
| Neurosurgery | 138 (6.7%) | 30.0 ± 16.6 | 17.19 ± 9.50 |
| Urology | 134 (6.5%) | 26.3 ± 11.4 | 16.35 ± 7.97 |
| Trauma Surgery | 223 (10.8%) | 26.9 ± 16.7 | 15.68 ± 10.02 |
| General Surgery | 182 (8.8%) | 25.4 ± 15.1 | 15.66 ± 9.46 |
| Neurology | 4 (0.1%) | 25.8 ± 5.9 | 15.25 ± 3.34 |
| Plastic Surgery | 99 (4.8%) | 24.5 ± 13.0 | 14.97 ± 9.40 |
| Otorhinolaryngology | 166 (8.0%) | 24.0 ± 10.5 | 14.16 ± 6.35 |
| Dermatology | 10 (0.5%) | 24.2 ± 12.1 | 13.94 ± 6.07 |
| Ophthalmology | 264 (12.8%) | 22.5 ± 11.4 | 13.81 ± 7.53 |
| Pediatrics | 130 (6.3%) | 19.1 ± 8.6 | 13.49 ± 6.39 |
| Nuclear Medicine/Radiology | 16 (0.8%) | 19.3 ± 12.5 | 12.51 ± 8.08 |
| Psychiatry | 21 (1.0%) | 13.8 ± 14.4 | 9.13 ± 7.78 |
| Overall | 2065 (100%) | 25.74 ± 13.5 | 16.45 ± 8.97 |
| p-Value | <0.001 | <0.001 |
| Type of Outstanding Preoperative Test Results | All Patients n = 2065 | ANE n = 1979 | No ANE n = 86 | p-Value |
|---|---|---|---|---|
| Total | 226 (10.9%) | 210 (10.6%) | 16 (18.6%) | 0.020 |
| Lab test results | 134 (6.5%) | 126 (6.3%) | 8 (9.3%) | 0.263 |
| ECG | 89 (4.3%) | 81 (4.1%) | 8 (9.3%) | 0.029 |
| TTE/TEE | 11 (0.5%) | 10 (0.5%) | 1 (1.2%) | 0.374 |
| X-ray/CT scan | 2 (0.1%) | 2 (0.1%) | 0 (0%) | >0.999 |
| Cardiology consultation | 9 (0.4%) | 7 (0.3%) | 2 (2.3%) | 0.051 |
| Pulmonary function tests | 4 (0.2%) | 4 (0.2%) | 0 (0%) | >0.999 |
| Other specialty consultations | 9 (0.4%) | 9 (0.5%) | 0 (0%) | >0.999 |
| Characteristic | OR (95% CI) | p-Value | Adjusted p-Value Bonferoni Holm |
|---|---|---|---|
| 2nd anesthesiologist involved in the PAC | 3.823 (2.035 to 7.182) | <0.001 | 0.003 |
| Medium cardiac risk score | 1.585 (1.022 to 2.456) | 0.039 | 0.078 |
| 2nd PAC required 1 | 1.316 (0.644 to 2.689) | 0.451 | 0.451 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wiegand, S.B.; Heinemann, A.S.; Harries, D.; Bürger, D.; Thiehoff, L.; Fischbach, A. Confirmatory Study on Costs and Time Loss from Pre-Anesthetic Consultations for Canceled Surgeries: A Retrospective Analysis at Hannover Medical School, Germany. J. Clin. Med. 2025, 14, 6454. https://doi.org/10.3390/jcm14186454
Wiegand SB, Heinemann AS, Harries D, Bürger D, Thiehoff L, Fischbach A. Confirmatory Study on Costs and Time Loss from Pre-Anesthetic Consultations for Canceled Surgeries: A Retrospective Analysis at Hannover Medical School, Germany. Journal of Clinical Medicine. 2025; 14(18):6454. https://doi.org/10.3390/jcm14186454
Chicago/Turabian StyleWiegand, Steffen B., Anna S. Heinemann, Dennis Harries, David Bürger, Lisa Thiehoff, and Anna Fischbach. 2025. "Confirmatory Study on Costs and Time Loss from Pre-Anesthetic Consultations for Canceled Surgeries: A Retrospective Analysis at Hannover Medical School, Germany" Journal of Clinical Medicine 14, no. 18: 6454. https://doi.org/10.3390/jcm14186454
APA StyleWiegand, S. B., Heinemann, A. S., Harries, D., Bürger, D., Thiehoff, L., & Fischbach, A. (2025). Confirmatory Study on Costs and Time Loss from Pre-Anesthetic Consultations for Canceled Surgeries: A Retrospective Analysis at Hannover Medical School, Germany. Journal of Clinical Medicine, 14(18), 6454. https://doi.org/10.3390/jcm14186454






