Eyelid Complications in Subciliary Versus Transconjunctival Approaches to Orbital and Zygomaticofacial Fractures: A Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Quality Assessment
2.4. Data Extraction
2.5. Statistical Analysis
3. Results
3.1. Search Results
3.2. Evaluation of the Quality of Included Studies
3.3. Characteristics of the Included Studies
3.4. Outcome Assessment
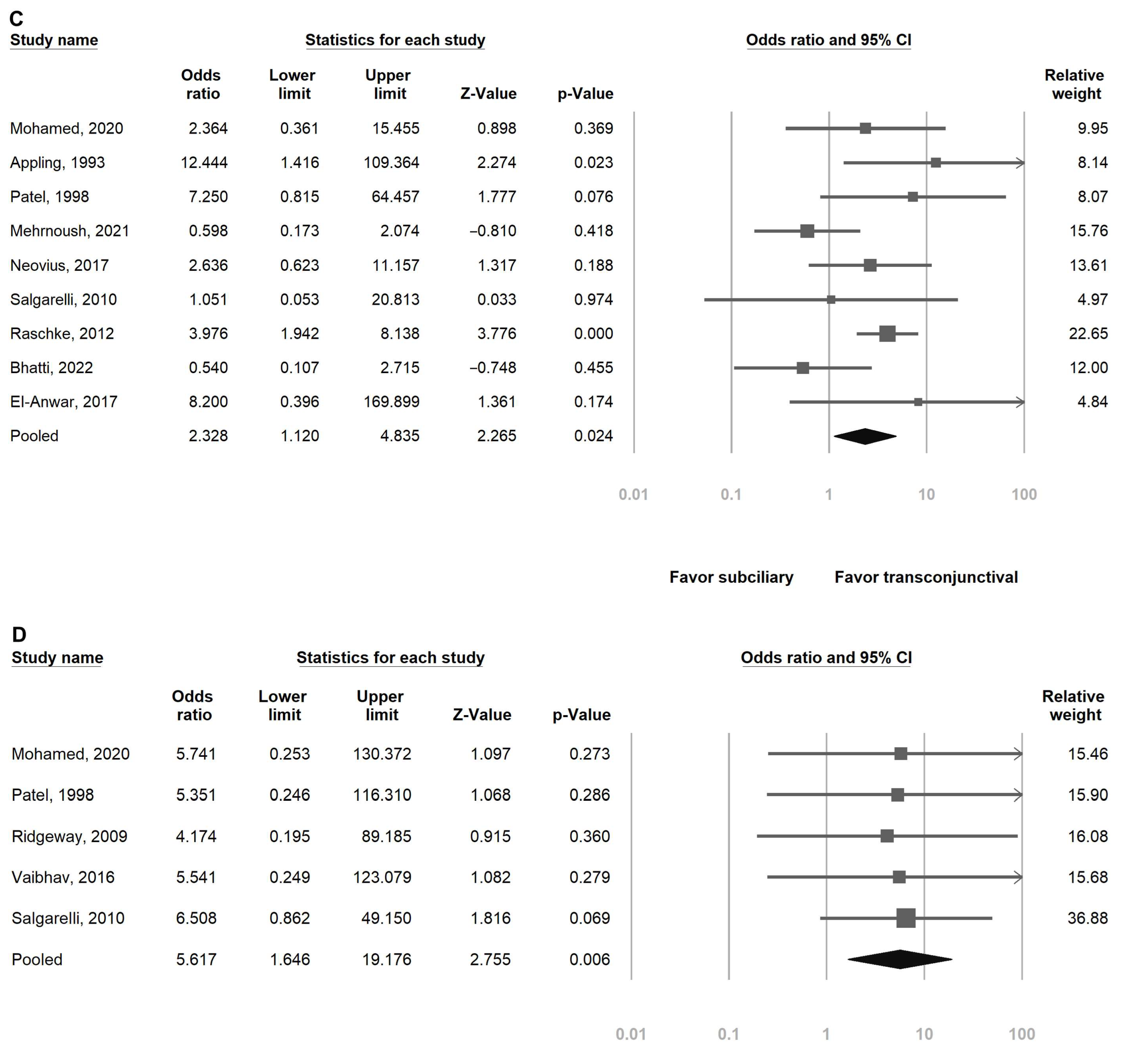
3.4.1. Ectropion
3.4.2. Entropion
3.4.3. Scleral Show
3.4.4. Scar
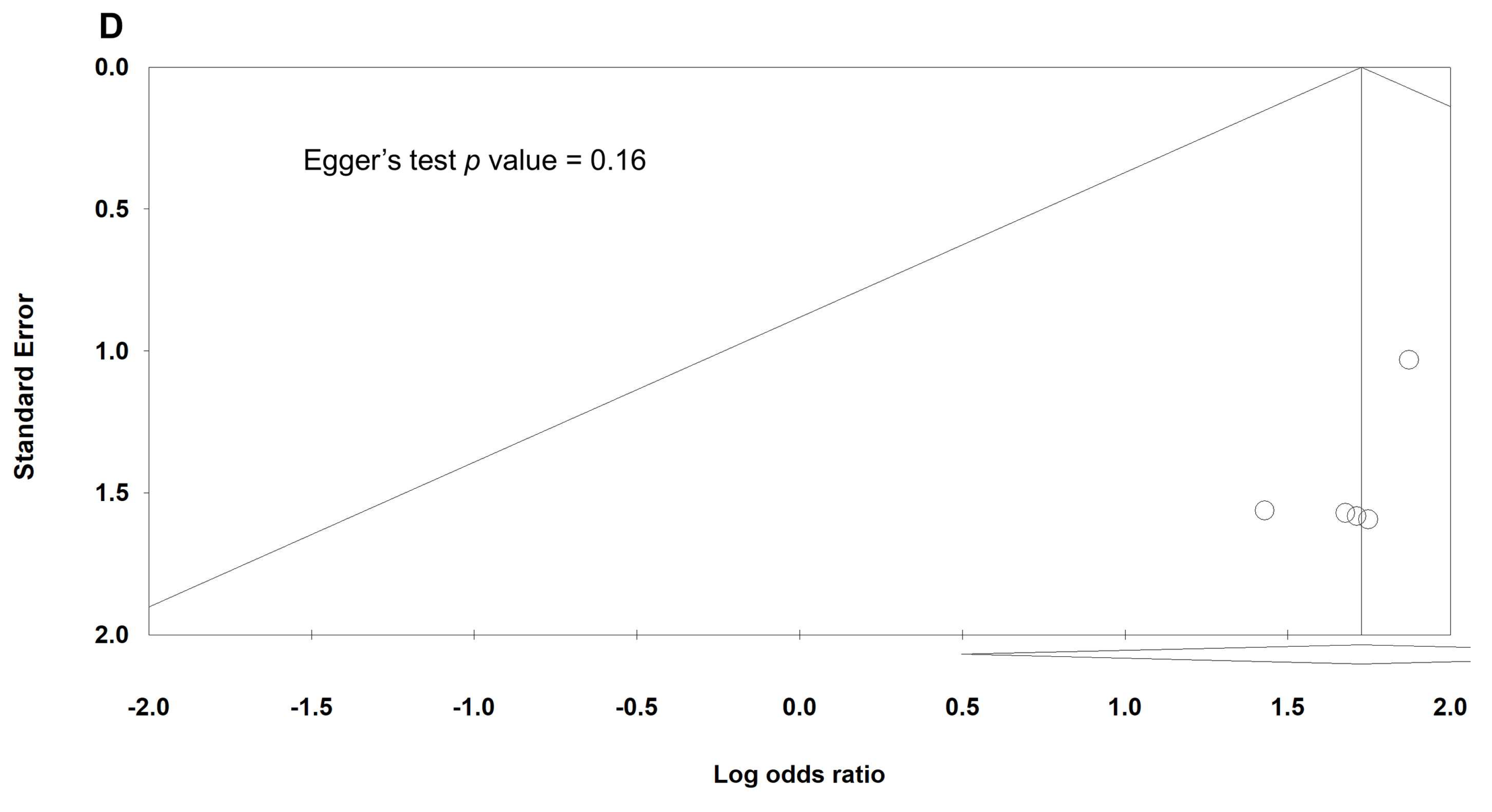
3.5. Heterogeneity and Publication Bias
3.6. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Ors | Odds Ratios |
| Cis | Confidence Intervals |
| VAS | Visual Analog Scale |
References
- Zingg, M.; Chowdhury, K.; Lädrach, K.; Vuillemin, T.; Sutter, F.; Raveh, J. Treatment of 813 zygoma-lateral orbital complex fractures. New aspects. Arch. Otolaryngol.-Head Neck Surg. 1991, 117, 611–620. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Thaller, S.R.; Ellis, E. Subciliary vs. Transconjunctival approach for the management of orbital floor and periorbital fractures: A systematic review and meta-analysis. J. Cranio-Maxillo-Facial Surg. 2017, 45, 1647–1654. [Google Scholar] [CrossRef]
- Patel, P.C.; Sobota, B.T.; Patel, N.M.; Greene, J.S.; Millman, B. Comparison of transconjunctival versus subciliary approaches for orbital fractures: A review of 60 cases. J. Cranio-Maxillofac. Trauma 1998, 4, 17–21. [Google Scholar]
- Gooris, P.J.J.; Jansen, J.; Bergsma, J.E.; Dubois, L. Evidence-based decision making in orbital fractures: Implementation of a clinical protocol. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2021, 29, 109–127. [Google Scholar] [CrossRef]
- Palavalli, M.H.; Huayllani, M.T.; Gokun, Y.; Lu, Y.; Janis, J.E. Surgical approaches to orbital fractures: A practical and systematic review. Plast. Reconstr. Surg. Glob. Open 2023, 11, e4967. [Google Scholar] [CrossRef]
- Ridgway, E.B.; Chen, C.; Lee, B.T. Acquired entropion associated with the transconjunctival incision for facial fracture management. J. Craniofacial Surg. 2009, 20, 1412–1415. [Google Scholar] [CrossRef]
- Liu, S.H.; Chen, Y.Y.; Nurmatov, U.; van Schayck, O.C.P.; Kuo, I.C. Antibiotics versus placebo for acute bacterial conjunctivitis: Findings from a cochrane systematic review. Am. J. Ophthalmol. 2024, 257, 143–153. [Google Scholar] [CrossRef]
- Thevi, T.; Abas, A.L.; Dua, H.S. Amniotic membrane graft (amg) for persistent epithelial defects following infective corneal ulcers and keratitis— A systematic review. Indian J. Ophthalmol. 2025, 73, S361–S368. [Google Scholar] [CrossRef] [PubMed]
- Bronstein, J.A.; Bruce, W.J.; Bakhos, F.; Ishaq, D.; Joyce, C.J.; Cimino, V. Surgical approach to orbital floor fractures: Comparing complication rates between subciliary and subconjunctival approaches. Craniomaxillofacial Trauma Reconstr. 2020, 13, 45–48. [Google Scholar] [CrossRef]
- Mohamed, F.I.; Reda, H.M.; Khalifa, G.A. Anthropometric changes in the morphology of the lower eyelid after using three different approaches in patients with orbital fractures. J. Cranio-Maxillo-Facial Surg. 2020, 48, 985–993. [Google Scholar] [CrossRef] [PubMed]
- Appling, W.D.; Patrinely, J.R.; Salzer, T.A. Transconjunctival approach vs subciliary skin-muscle flap approach for orbital fracture repair. Arch. Otolaryngol.-Head Neck Surg. 1993, 119, 1000–1007. [Google Scholar] [CrossRef]
- Mehrnoush, M.R.; Amir, J.A.; Hamed, Z.; Narges, H. The incidence of common complications, including ectropion and entropion, in transconjunctival and subciliary approaches for treatment of zmc fractures. J. Dent. 2021, 22, 76–81. [Google Scholar]
- Trevisiol, L.; D’Agostino, A.; Gasparini, S.; Bettini, P.; Bersani, M.; Nocini, R.; Favero, V. Transconjunctival and subciliary approach in the treatment of orbital fractures: A study on oculoplastic complication. J. Clin. Med. 2021, 10, 2775. [Google Scholar] [CrossRef]
- Raschke, G.; Djedovic, G.; Peisker, A.; Wohlrath, R.; Rieger, U.; Guentsch, A.; Gomez-Dammeier, M.; Schultze-Mosgau, S. The isolated orbital floor fracture from a transconjunctival or subciliary perspective-a standardized anthropometric evaluation. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e111–e117. [Google Scholar] [CrossRef]
- Pandya, R.P.; Deng, W.; Hodgson, N.M. Current guidelines and opinions in the management of orbital floor fractures. Otolaryngol. Clin. N. Am. 2023, 56, 1101–1112. [Google Scholar] [CrossRef]
- Ridgway, E.B.; Chen, C.; Colakoglu, S.; Gautam, S.; Lee, B.T. The incidence of lower eyelid malposition after facial fracture repair: A retrospective study and meta-analysis comparing subtarsal, subciliary, and transconjunctival incisions. Plast. Reconstr. Surg. 2009, 124, 1578–1586. [Google Scholar] [CrossRef]
- Zhang, J.; He, X.; Qi, Y.; Zhou, P. The better surgical timing and approach for orbital fracture: A systematic review and meta-analysis. Ann. Transl. Med. 2022, 10, 564. [Google Scholar] [CrossRef]
- Vaibhav, N.; Keerthi, R.; Nanjappa, M.; Ashwin, D.P.; Reyazulla, M.A.; Gopinath, A.L.; Ghosh, A. Comparison of ‘sutureless’ transconjunctival and subciliary approach for treatment of infraorbital rim fractures: A clinical study. J. Maxillofac. Oral Surg. 2016, 15, 355–362. [Google Scholar] [CrossRef]
- Salgarelli, A.C.; Bellini, P.; Landini, B.; Multinu, A.; Consolo, U. A comparative study of different approaches in the treatment of orbital trauma: An experience based on 274 cases. Oral Maxillofac. Surg. 2010, 14, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Raschke, G.; Rieger, U.; Bader, R.D.; Schaefer, O.; Guentsch, A.; Schultze-Mosgau, S. Outcomes analysis of eyelid deformities using photograph-assisted standardized anthropometry in 311 patients after orbital fracture treatment. J. Trauma Acute Care Surg. 2012, 73, 1319–1325. [Google Scholar] [CrossRef] [PubMed]
- Pausch, N.C.; Sirintawat, N.; Wagner, R.; Halama, D.; Dhanuthai, K. Lower eyelid complications associated with transconjunctival versus subciliary approaches to orbital floor fractures. Oral Maxillofac. Surg. 2016, 20, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Neovius, E.; Clarliden, S.; Farnebo, F.; Lundgren, T.K. Lower eyelid complications in facial fracture surgery. J. Craniofacial Surg. 2017, 28, 391–393. [Google Scholar] [CrossRef]
- Kesselring, A.G.; Promes, P.; Strabbing, E.M.; van der Wal, K.G.; Koudstaal, M.J. Lower eyelid malposition following orbital fracture surgery: A retrospective analysis based on 198 surgeries. Craniomaxillofacial Trauma Reconstr. 2016, 9, 109–112. [Google Scholar] [CrossRef]
- Ishida, K. Evolution of the surgical approach to the orbitozygomatic fracture: From a subciliary to a transconjunctival and to a novel extended transconjunctival approach without skin incisions. J. Plast. Reconstr. Aesthetic Surg. 2016, 69, 497–505. [Google Scholar] [CrossRef]
- Haghighat, A.; Moaddabi, A.; Soltani, P. Comparison of subciliary, subtarsal and transconjunctival approaches for management of zygomaticoorbital fractures. Br. J. Med. Med. Res. 2017, 20, 1–9. [Google Scholar] [CrossRef]
- Giraddi, G.B.; Syed, M.K. Preseptal transconjunctival vs. Subciliary approach in treatment of infraorbital rim and floor fractures. Ann. Maxillofac. Surg. 2012, 2, 136–140. [Google Scholar] [CrossRef]
- Bhatti, M.A.; Riaz, E.; Razi, A.; Ahmed, S.; Ahsan, F.; Nadeem, R. Incidence of complication of ectropion and entropion in transconjunctival and subciliary approach for treatment of zmc fracture. Pak. J. Med. Health Sci. 2022, 16, 693–695. [Google Scholar] [CrossRef]
- Subramanian, B.; Krishnamurthy, S.; Suresh Kumar, P.; Saravanan, B.; Padhmanabhan, M. Comparison of various approaches for exposure of infraorbital rim fractures of zygoma. J. Maxillofac. Oral Surg. 2009, 8, 99–102. [Google Scholar] [CrossRef] [PubMed]
- El-Anwar, M.W.; Elsheikh, E.; Hussein, A.M.; Tantawy, A.A.; Abdelbaki, Y.M. Transconjunctival versus subciliary approach to the infraorbital margin for open reduction of zygomaticomaxillary complex fractures: A randomized feasibility study. Oral Maxillofac. Surg. 2017, 21, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.; Elsharkawy, A.; Al-Tairi, N.; Farhan, A.; Abotaleb, B.; Alsharaee, Y.; Oginni, F.O.; Al-Zabidi, A. What surgical approach has the lowest risk of the lower lid complications in the treatment of orbital floor and periorbital fractures? A frequentist network meta-analysis. J. Cranio-Maxillo-Facial Surg. 2018, 46, 2164–2175. [Google Scholar] [CrossRef]
- Wagh, R.D.; Naik, M.; Bothra, N.; Singh, S. Lower eyelid entropion following transconjunctival orbital fracture repair: Case series and literature review. Saudi J. Ophthalmol. 2023, 37, 154–157. [Google Scholar] [CrossRef] [PubMed]
- Hasan, M.Z.; Rabbani, F.; Hasnat, A.; Imam, F.; Saddam, M.M.R. Aesthetic Outcome of Transconjunctival versus Subciliary Approach for Infra-Orbital Rim and Orbital Floor Fractures. J. Dent. Allied Sci. 2025, 7, 19–25. [Google Scholar] [CrossRef]



| Study | Selection | Comparability | Outcomes | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Representativeness of Cohort | Selection of Nonexposed Cohort | Ascertainment of Exposure | Outcome Lacking at the Beginning | Main Factor | Additional Factor | Outcome Assessment | Sufficient Follow-Up Time | Follow Up Adequacy | Score a | |
| Bronstein [9] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Mohamed [10] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 9 |
| Appling [11] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Patel [3] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Mehrnoush [12] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 9 |
| Ridgeway [16] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Trevisiol [13] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Neovius [22] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Giraddi [26] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 9 |
| Haghighat [25] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Vaibhav [18] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 9 |
| Pausch [21] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Kesselring [23] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Ishida [24] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Salgarelli [19] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Raschke [20] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Bhatti [27] | ★ | ★ | ★ | ★ | ★ | ☆ | ★ | ★ | ★ | 8 |
| Subramanian [28] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 9 |
| EI-Anwar [29] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 9 |
| Authors | Year | Study Design | Age | Groups | Number of Pts | Follow-Up |
|---|---|---|---|---|---|---|
| Bronstein et al. [9] | 2020 | Retrospective | 34.8 ± 12.4 | Subciliary | 82 | at least 6 months |
| 35.3 ± 11.9 | Transconjunctival | 102 | ||||
| Mohamed et al. [10] | 2020 | Randomized clinical study | 30.9 ± 12.6 | Subciliary | 15 | 6 months |
| 37.4 ± 9.0 | Transconjunctival | 15 | ||||
| Appling et al. [11] | 1993 | Retrospective | 11–60 | Subciliary | 25 | 6 weeks–5 years |
| Transconjunctival | 33 | |||||
| Patel et al. [3] | 1998 | Retrospective | 12–63 | Subciliary | 30 | at least 8 months |
| Transconjunctival | ||||||
| Mehrnoush et al. [12] | 2021 | Randomized clinical study | 34.6 ± 14.2 | Subciliary | 42 | 5 months |
| 29.0 ± 9.0 | Transconjunctival | 38 | ||||
| Ridgeway et al. [16] | 2009 | Retrospective | 39 | Subciliary | 56 | 6 weeks |
| Transconjunctival | 45 | |||||
| Trevisiol et al. [13] | 2021 | Retrospective | 44 | Subciliary | 36 | 12–74 months |
| Transconjunctival | 33 | |||||
| Neovius et al. [22] | 2017 | Retrospective | 41 | Subciliary | 37 | at least 6 months |
| Transconjunctival | 91 | |||||
| Giraddi et al. [26] | 2012 | Randomized clinical study | 28.4 | Subciliary | 10 | 3 months |
| Transconjunctival | 10 | |||||
| Haghighat et al. [25] | 2010 | Prospective clinical study | 26.7 ± 6.5 | Subciliary | 17 | 4 weeks |
| Transconjunctival | 17 | |||||
| Vaibhav et al. [18] | 2016 | Randomized clinical study | 20–60 | Subciliary | 20 | 3 months |
| Transconjunctival | 20 | |||||
| Pausch et al. [21] | 2016 | Retrospective | 42.7 ± 21.1 | Subciliary | 225 | 6 months |
| Transconjunctival | 121 | |||||
| Kesselring et al. [23] | 2016 | Retrospective | 37.5 | Subciliary | 47 | NR |
| Transconjunctival | 26 | |||||
| Ishida et al. [24] | 2016 | Retrospective | NR | Subciliary | 29 | 6 weeks–6.8 years |
| Transconjunctival | 179 | |||||
| Salgarelli et al. [19] | 2010 | Retrospective | 37.1 | Subciliary | 219 | 6–48 months |
| Transconjunctival | 32 | |||||
| Raschke et al. [20] | 2012 | Retrospective | 43.3 ± 19.0 | Subciliary | 114 | 9 months |
| Transconjunctival | 197 | |||||
| Bhatti et al. [27] | 2022 | Prospective clinical study | 32.8 | Subciliary | 28 | 5 months |
| Transconjunctival | 22 | |||||
| Subramanian [28] | 2009 | Randomized clinical study | NR | Subciliary | 10 | at least 6 months |
| Transconjunctival | 10 | |||||
| EI-Anwar et al. [29] | 2017 | Randomized clinical study | 31.3 ± 9.2 | Subciliary | 20 | 6 weeks |
| 31.6 ± 7.7 | Transconjunctival | 20 |
| Study | Groups | Num of pts | Orbital Floor Reconstruction | Types of Complication (%) |
|---|---|---|---|---|
| Bronstein, 2020 [9] | Sub ciliary | 82 | Yes | ectropion (2.4), entropion (1.2), lagophthalmos (1.2), corneal injury (7.3), keratoconjunctivitis sicca (3.7) |
| Transconjunctival | 102 | ectropion (2.0), entropion (3.9), lagophthalmos (1.0), corneal injury (6.9), keratoconjunctivitis sicca (3.9) | ||
| Mohamed, 2020 [10] | Subciliary | 15 | Yes | ectropion (20), entropion (0), scleral show (26.7), visible scar (13.3) a |
| Transconjunctival | 15 | ectropion (6.7), entropion (20), scleral show (13.3), visible scar (0) a | ||
| Appling, 1993 [11] | Subciliary | 25 | Yes | ectropion (12.0), scleral show (28.0), canthal malposition (0) |
| Transconjunctival | 33 | ectropion (0), scleral show (3.0), canthal malposition (9.1) | ||
| Patel, 1998 [3] | Subciliary | 30 | Yes | ectropion (6.7), entropion (0), scleral show (20), visible scar (6.7) b |
| Transconjunctival | 30 | ectropion (0), entropion (0), scleral show (3.3), visible scar (0) b | ||
| Mehrnoush, 2021 [12] | Subciliary | 42 | Yes | ectropion (2.4), entropion (0), epiphora (7.1), scleral show (11.9) |
| Transconjunctival | 38 | ectropion (13.2), entropion (5.3), epiphora (23.7), scleral show (18.4) | ||
| Ridgeway, 2009 [16] | Subciliary | 56 | Yes | Ectropion (12.5), entropion (0), scar (3.6) c, lid edema (8.9) |
| Transconjunctival | 45 | Ectropion (0), entropion (4.4), scar (0) c, lid edema (0) | ||
| Trevisiol, 2021 [13] | Subciliary | 36 | Yes | ectropion (8.3), entropion (0) |
| Transconjunctival | 33 | ectropion (0), entropion (0) | ||
| Neovius, 2017 [22] | Subciliary | 37 | Yes | ectropion (8.1), entropion (0), scleral show (11.0), canthal malposition (0) |
| Transconjunctival | 91 | ectropion (2.2), entropion (0), scleral show (4.4), canthal malposition (2.2) | ||
| Giraddi, 2012 [26] | Subciliary | 10 | Yes | ectropion (30.0), entropion (0), laceration of tarsal plate (0), buttonhole laceration of lower eyelid (10.0) |
| Transconjunctival | 10 | ectropion (10.0), entropion (30.0), laceration of tarsal plate (10.0), buttonhole laceration of lower eyelid (0) | ||
| Haghighat, 2017 [25] | Subciliary | 17 | Yes | ectropion (17.6), scar (3.7 ± 0.6) d |
| Transconjunctival | 17 | ectropion (0), scar (0.0 ± 0.0) d | ||
| Vaibhav, 2016 [18] | Subciliary | 20 | No | ectropion (0), entropion (0), unsatisfactory scar (10) e |
| Transconjunctival | 20 | ectropion (0), entropion (5), unsatisfactory scar (0) e | ||
| Pausch, 2016 [21] | Subciliary | 225 | Yes | ectropion (3.6), entropion (0), eyelid retraction (0) |
| Transconjunctival | 121 | ectropion (0), entropion (2.5), eyelid retraction (0) | ||
| Kesselring, 2016 [23] | Subciliary | 47 | Yes | ectropion (2.1), entropion (0) |
| Transconjunctival | 26 | ectropion (0), entropion (0) | ||
| Ishida, 2016 [24] | Subciliary | 29 | Yes | ectropion (6.9), scleral show (6.9) |
| Transconjunctival | 179 | ectropion (0.6), entropion (3.4), symblepharon (1.7), trichiasis (1.1), lacrimal canaliculus avulsion (1.1), conjunctival granulation (2.2), canthal malposition (0.6) | ||
| Salgarelli, 2010 [19] | Subciliary | 219 | Yes | ectropion (0), visible scar (17.5) f, scleral show (1.3) |
| Transconjunctival | 32 | ectropion (0), visible scar (3) f, scleral show (0) | ||
| Raschke, 2012 [20] | Subciliary | 114 | Yes | ectropion (5.3), entropion (0), scleral show (21.8) |
| Transconjunctival | 197 | ectropion (1.0), entropion (1.0), scleral show (6.6) | ||
| Bhatti, 2022 [27] | Subciliary | 28 | No | ectropion (14.2), entropion (0), scleral show (11.0), epiphora (21.0) |
| Transconjunctival | 22 | ectropion (13.5), entropion (9.1), scleral show (17.0), epiphora (20.0) | ||
| Subramanian, 2009 [28] | Subciliary | 10 | No | ectropion (0), scar (1.55) g |
| Transconjunctival | 10 | ectropion (10), scar (1.00) g, prolonged edema (20) | ||
| EI-Anwar, 2017 [29] | Subciliary | 20 | No | ectropion (10), entropion (0), scleral show (15), intolerable pain (10) |
| Transconjunctival | 20 | ectropion (0), entropion (20), scleral show (0), intolerable pain (15) |
| Study | Scar Assessment Method | Score Range |
|---|---|---|
| Mohamed, 2020 [10] | Feldman scar esthetic score | 0–4 (0 = Scar not visible, 1 = Barely visible, 2 = Noticeable, 3 = Very noticeable, 4 = Extremely noticeable |
| Patel, 1998 [3] | visible scar scale (binary) | yes/no |
| Ridgway, 2009 [16] | hypertrophic (or visible) scar scale | yes/no |
| Vaibhav, 2016 [18] | patient-reported satisfaction scale (binary) | satisfactory/unsatisfactory |
| Salgarelli, 2010 [19] | visible scar scale (binary) | yes/no |
| Subramanian, 2009 [28] | VAS (3-point visibility score) | custom; 1 = invisible, 2 = barely visible, 3 = visible |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.-Y.; Lai, Y.-J.; Chen, T.-Y.; Yen, Y.-F. Eyelid Complications in Subciliary Versus Transconjunctival Approaches to Orbital and Zygomaticofacial Fractures: A Meta-Analysis. J. Clin. Med. 2025, 14, 6431. https://doi.org/10.3390/jcm14186431
Chen Y-Y, Lai Y-J, Chen T-Y, Yen Y-F. Eyelid Complications in Subciliary Versus Transconjunctival Approaches to Orbital and Zygomaticofacial Fractures: A Meta-Analysis. Journal of Clinical Medicine. 2025; 14(18):6431. https://doi.org/10.3390/jcm14186431
Chicago/Turabian StyleChen, Yu-Yen, Yun-Ju Lai, Tai-Yuan Chen, and Yung-Feng Yen. 2025. "Eyelid Complications in Subciliary Versus Transconjunctival Approaches to Orbital and Zygomaticofacial Fractures: A Meta-Analysis" Journal of Clinical Medicine 14, no. 18: 6431. https://doi.org/10.3390/jcm14186431
APA StyleChen, Y.-Y., Lai, Y.-J., Chen, T.-Y., & Yen, Y.-F. (2025). Eyelid Complications in Subciliary Versus Transconjunctival Approaches to Orbital and Zygomaticofacial Fractures: A Meta-Analysis. Journal of Clinical Medicine, 14(18), 6431. https://doi.org/10.3390/jcm14186431







