Cross-Sectional Study of the Changes in Attitudes of Post-Acute Coronary Syndromes Patients Towards Remote Biosignal Monitoring an eHealth Support in a 5-Year Interval
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Questionnaire Description
- Personal Data: Standard demographics such as age, sex, and activity frequency;
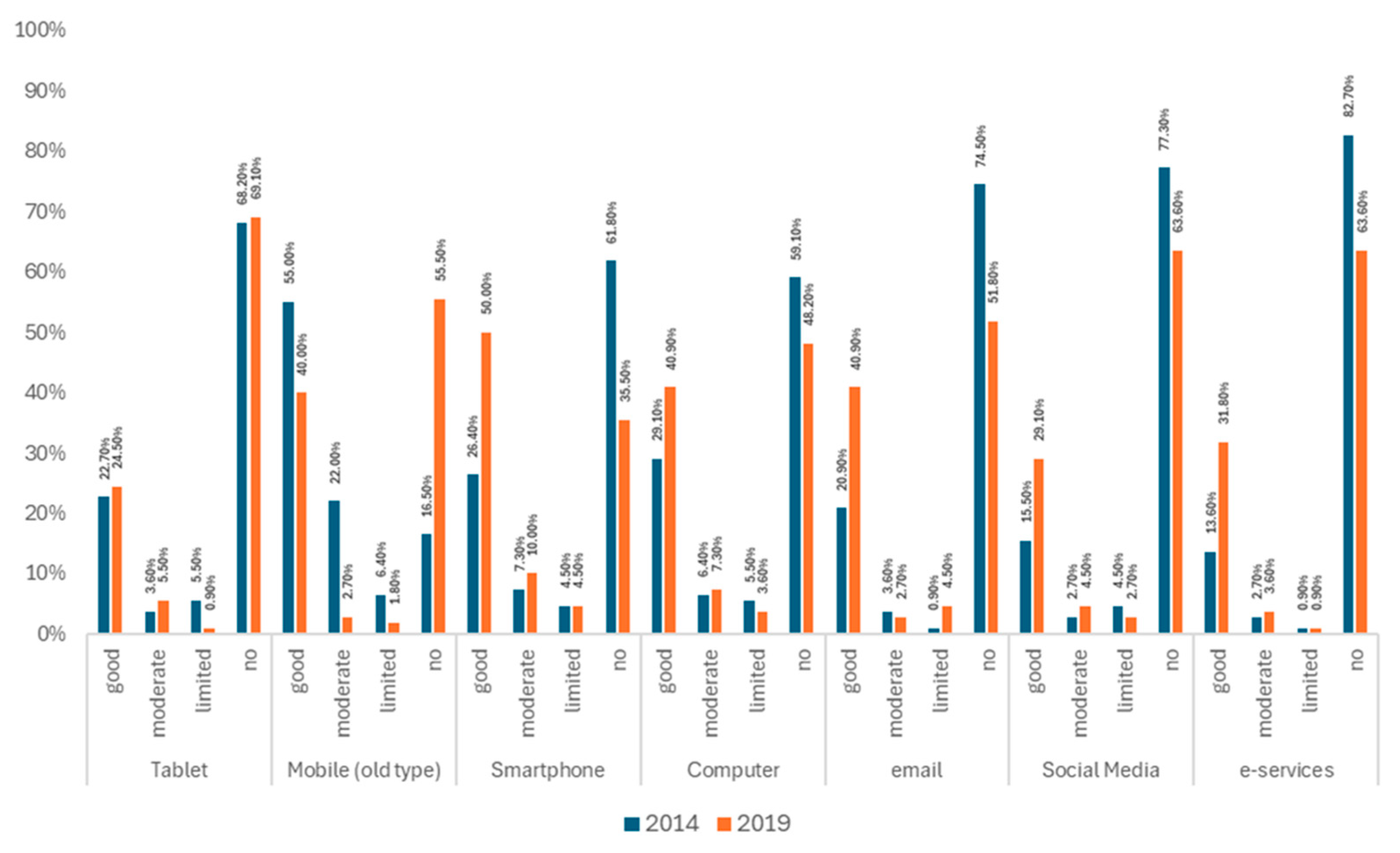
- Technological Literacy: Use of smartphones, internet services, etc.;
- Opinions and Perceptions about eHealth Services and Monitoring;
- Five questions addressed the inconvenience/annoyance of using a body-attached mobile recording device;
- Eight questions focused on the patient’s willingness to be observed for medical or activity monitoring.
2.3. Survey
2.4. Ethics
2.5. Statistical Methods
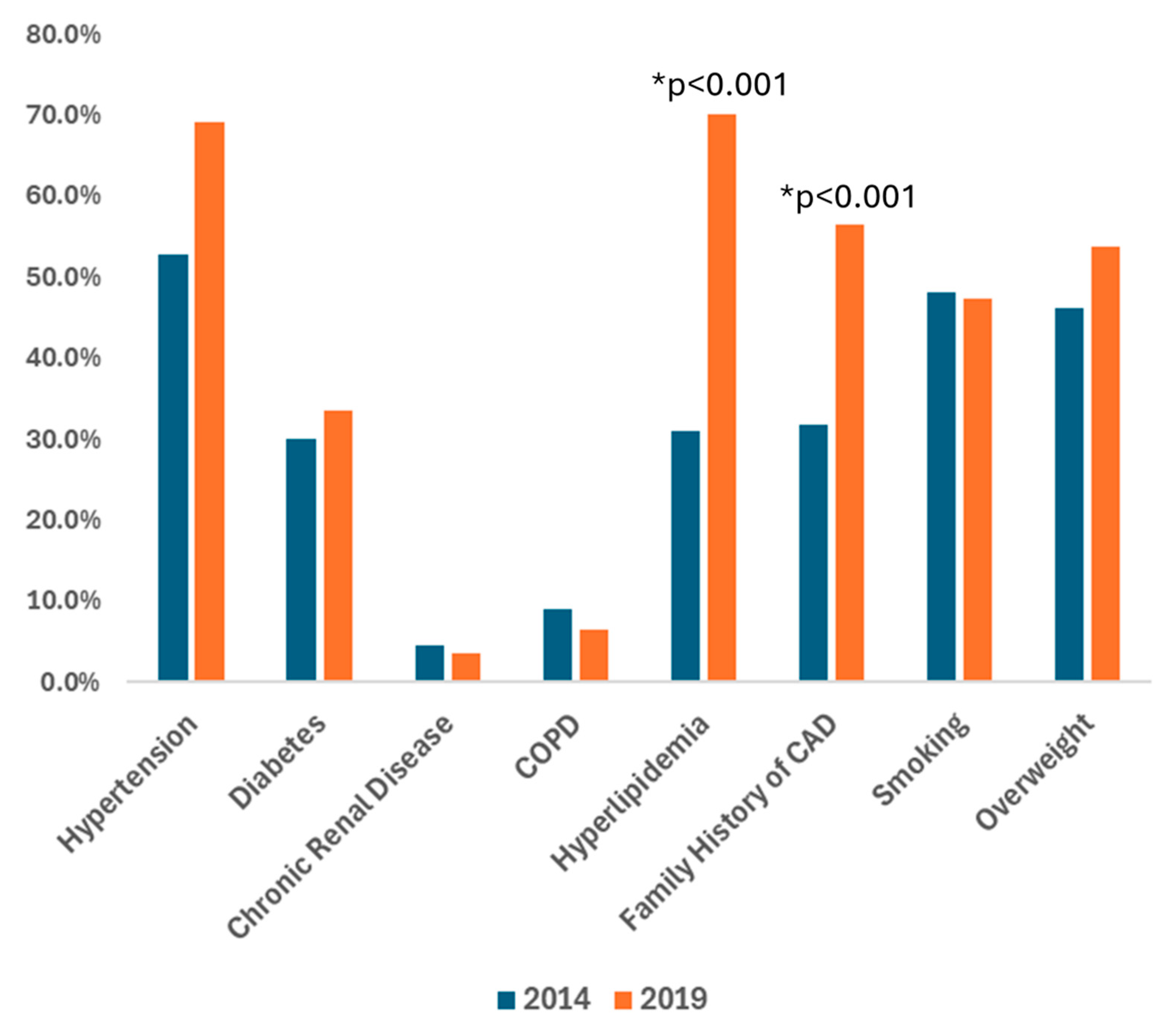
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Timmis, A.; Kazakiewicz, D.; Townsend, N.; Huculeci, R.; Aboyans, V.; Vardas, P. Global Epidemiology of Acute Coronary Syndromes. Nat. Rev. Cardiol. 2023, 20, 778–788. [Google Scholar] [CrossRef] [PubMed]
- Hamida, S.T.-B.; Hamida, E.B.; Ahmed, B. A New mHealth Communication Framework for Use in Wearable WBANs and Mobile Technologies. Sensors 2015, 15, 3379–3408. [Google Scholar] [CrossRef]
- Triberti, S.; Barello, S. The Quest for Engaging AmI: Patient Engagement and Experience Design Tools to Promote Effective Assisted Living. J. Biomed. Inform. 2016, 63, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Konstantinidis, E.I.; Bamparopoulos, G.; Billis, A.; Bamidis, P.D. Internet of Things for An Age-Friendly Healthcare. Stud. Health Technol. Inform. 2015, 210, 587–591. [Google Scholar]
- Scherr, D.; Kastner, P.; Kollmann, A.; Hallas, A.; Auer, J.; Krappinger, H.; Schuchlenz, H.; Stark, G.; Grander, W.; Jakl, G.; et al. Effect of Home-Based Telemonitoring Using Mobile Phone Technology on the Outcome of Heart Failure Patients after an Episode of Acute Decompensation: Randomized Controlled Trial. J. Med. Internet Res. 2009, 11, e34. [Google Scholar] [CrossRef]
- Amadi-Obi, A.; Gilligan, P.; Owens, N.; O’Donnell, C. Telemedicine in Pre-Hospital Care: A Review of Telemedicine Applications in the Pre-Hospital Environment. Int. J. Emerg. Med. 2014, 7, 29. [Google Scholar] [CrossRef] [PubMed]
- Kruse, G.; Park, E.R.; Shahid, N.N.; Abroms, L.; Haberer, J.E.; Rigotti, N.A. Combining Real-Time Ratings with Qualitative Interviews to Develop a Smoking Cessation Text Messaging Program for Primary Care Patients. JMIR Mhealth Uhealth 2019, 7, e11498. [Google Scholar] [CrossRef]
- Podina, I.R.; Fodor, L.A.; Cosmoiu, A.; Boian, R. An Evidence-Based Gamified mHealth Intervention for Overweight Young Adults with Maladaptive Eating Habits: Study Protocol for a Randomized Controlled Trial. Trials 2017, 18, 592. [Google Scholar] [CrossRef]
- Chung, S.-C.; Gedeborg, R.; Nicholas, O.; James, S.; Jeppsson, A.; Wolfe, C.; Heuschmann, P.; Wallentin, L.; Deanfield, J.; Timmis, A.; et al. Acute Myocardial Infarction: A Comparison of Short-Term Survival in National Outcome Registries in Sweden and the UK. Lancet 2014, 383, 1305–1312. [Google Scholar] [CrossRef]
- Chen, S.; Gong, E.; Kazi, D.S.; Gates, A.B.; Bai, R.; Fu, H.; Peng, W.; De La Cruz, G.; Chen, L.; Liu, X.; et al. Using Mobile Health Intervention to Improve Secondary Prevention of Coronary Heart Diseases in China: Mixed-Methods Feasibility Study. JMIR Mhealth Uhealth 2018, 6, e9. [Google Scholar] [CrossRef]
- Role of Technology in Promoting Heart Healthy Behavior Change to Increase Equity in Optimal Cardiovascular Health: A Scientific Statement from the American Heart Association. PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/40190270/ (accessed on 23 August 2025).
- Goldfarb, M.J.; Saylor, M.A.; Bozkurt, B.; Code, J.; Di Palo, K.E.; Durante, A.; Flanary, K.; Masterson Creber, R.; Ogunniyi, M.O.; Rodriguez, F.; et al. Patient-Centered Adult Cardiovascular Care: A Scientific Statement from the American Heart Association. Circulation 2024, 149, e1176–e1188. [Google Scholar] [CrossRef]
- Halldorsdottir, H.; Thoroddsen, A.; Ingadottir, B. Impact of Technology-Based Patient Education on Modifiable Cardiovascular Risk Factors of People with Coronary Heart Disease: A Systematic Review. Patient Educ. Couns. 2020, 103, 2018–2028. [Google Scholar] [CrossRef]
- Wang, W.; Jiao, M.; Zhao, X.; Chen, C.; Jiang, W.; Zhang, X. Assessment of eHealth Literacy among Cardiovascular Disease Patients and Analysis of Influencing Factors. Front. Public Health 2025, 13, 1587163. [Google Scholar] [CrossRef]
- Qi, Y.; Mohamad, E.; Azlan, A.A.; Zhang, C.; Ma, Y.; Wu, A. Digital Health Solutions for Cardiovascular Disease Prevention: Systematic Review. J. Med. Internet Res. 2025, 27, e64981. [Google Scholar] [CrossRef]
- Terschüren, C.; Mensing, M.; Mekel, O.C.L. Is Telemonitoring an Option against Shortage of Physicians in Rural Regions? Attitude towards Telemedical Devices in the North Rhine-Westphalian Health Survey, Germany. BMC Health Serv. Res. 2012, 12, 95. [Google Scholar] [CrossRef]
- Wang, H.; Paulson, K.R.; Pease, S.A.; Watson, S.; Comfort, H.; Zheng, P.; Aravkin, A.Y.; Bisignano, C.; Barber, R.M.; Alam, T.; et al. Estimating Excess Mortality Due to the COVID-19 Pandemic: A Systematic Analysis of COVID-19-Related Mortality, 2020–21. Lancet 2022, 399, 1513–1536. [Google Scholar] [CrossRef] [PubMed]
- Canizares, M.; Badley, E.M. Generational Differences in Patterns of Physical Activities over Time in the Canadian Population: An Age-Period-Cohort Analysis. BMC Public Health 2018, 18, 304. [Google Scholar] [CrossRef] [PubMed]
- Van Oostrom, S.H.; Slobbe, L.C.J.; Van Den Berg, S.W.; Verschuren, W.M.M.; Picavet, H.S.J. Do Generations Differ in Sports Participation and Physical Activity over the Life Course? Evidence from Multiple Datasets. Eur. J. Sport Sci. 2019, 19, 1395–1403. [Google Scholar] [CrossRef]
- Sahlqvist, S.; Song, Y.; Ogilvie, D. Is Active Travel Associated with Greater Physical Activity? The Contribution of Commuting and Non-Commuting Active Travel to Total Physical Activity in Adults. Prev. Med. 2012, 55, 206–211. [Google Scholar] [CrossRef] [PubMed]
- Foti, K.; Wang, D.; Appel, L.J.; Selvin, E. Hypertension Awareness, Treatment, and Control in US Adults: Trends in the Hypertension Control Cascade by Population Subgroup (National Health and Nutrition Examination Survey, 1999–2016). Am. J. Epidemiol. 2019, 188, 2165–2174. [Google Scholar] [CrossRef]
- Chew, N.W.S.; Ng, C.H.; Tan, D.J.H.; Kong, G.; Lin, C.; Chin, Y.H.; Lim, W.H.; Huang, D.Q.; Quek, J.; Fu, C.E.; et al. The Global Burden of Metabolic Disease: Data from 2000 to 2019. Cell Metab. 2023, 35, 414–428.e3. [Google Scholar] [CrossRef]
- Wahrenberg, A.; Magnusson, P.K.; Discacciati, A.; Ljung, L.; Jernberg, T.; Frick, M.; Linder, R.; Svensson, P. Family History of Coronary Artery Disease Is Associated with Acute Coronary Syndrome in 28,188 Chest Pain Patients. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 741–747. [Google Scholar] [CrossRef]
- Yeşilyurt, E.; Vezne, R. Digital Literacy, Technological Literacy, and Internet Literacy as Predictors of Attitude toward Applying Computer-Supported Education. Educ. Inf. Technol. 2023, 28, 9885–9911. [Google Scholar] [CrossRef]
- Park, H.; Choi, B.; Joo, S.; Kim, Y.-M.; Kim, H.K. Digital Technology Use and Intergenerational Integration: The Mediating Role of Digital Literacy. Innov. Aging 2022, 6, 579. [Google Scholar] [CrossRef]
- Hearn, J.; Pham, Q.; Schwartz, J.I.; Ssinabulya, I.; Akiteng, A.R.; Ross, H.J.; Cafazzo, J.A. Lived Experiences and Technological Literacy of Heart Failure Patients and Clinicians at a Cardiac Care Centre in Uganda. Ann. Glob. Health 2020, 86, 85. [Google Scholar] [CrossRef] [PubMed]
- Taha, J.; Czaja, S.J.; Sharit, J.; Morrow, D.G. Factors Affecting Usage of a Personal Health Record (PHR) to Manage Health. Psychol. Aging 2013, 28, 1124–1139. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, P.J. Improving Health Literacy Using the Power of Digital Communications to Achieve Better Health Outcomes for Patients and Practitioners. Front. Digit. Health 2023, 5, 1264780. [Google Scholar] [CrossRef]
- Spatz, E.S.; Ginsburg, G.S.; Rumsfeld, J.S.; Turakhia, M.P.; Friend, S.H.; Picard, R.W.; Drazen, J.M. Wearable Digital Health Technologies for Monitoring in Cardiovascular Medicine. N. Engl. J. Med. 2024, 390, 346–356. [Google Scholar] [CrossRef]
- DeWyer, A.; Scheel, A.; Kamarembo, J.; Akech, R.; Asiimwe, A.; Beaton, A.; Bobson, B.; Canales, L.; DeStigter, K.; Kazi, D.S.; et al. Establishment of a Cardiac Telehealth Program to Support Cardiovascular Diagnosis and Care in a Remote, Resource-Poor Setting in Uganda. PLoS ONE 2021, 16, e0255918. [Google Scholar] [CrossRef]
- Ghali, H.; El Hraiech, A.; Ben Souda, H.; Karray, M.; Pavy, B.; Zedini, C.; Çalık, E.S. Therapeutic Education of Patients with Coronary Heart Disease: Impact of Digital Platform Monitoring in Preventing Major Cardiovascular Events in Tunisia: Study Protocol. PLoS ONE 2024, 19, e0300250. [Google Scholar] [CrossRef]
- Gleason, A.W. mHealth—Opportunities for Transforming Global Health Care and Barriers to Adoption. J. Electron. Resour. Med. Libr. 2015, 12, 114–125. [Google Scholar] [CrossRef]
- Cajita, M.I.; Hodgson, N.A.; Budhathoki, C.; Han, H.-R. Intention to Use mHealth in Older Adults with Heart Failure. J. Cardiovasc. Nurs. 2017, 32, E1–E7. [Google Scholar] [CrossRef]
- Mackert, M.; Mabry-Flynn, A.; Champlin, S.; Donovan, E.E.; Pounders, K. Health Literacy and Health Information Technology Adoption: The Potential for a New Digital Divide. J. Med. Internet Res. 2016, 18, e6349. [Google Scholar] [CrossRef] [PubMed]
- Manganello, J.; Gerstner, G.; Pergolino, K.; Graham, Y.; Falisi, A.; Strogatz, D. The Relationship of Health Literacy with Use of Digital Technology for Health Information: Implications for Public Health Practice. J. Public Health Manag. Pract. 2017, 23, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Perlmutter, A.; Benchoufi, M.; Ravaud, P.; Tran, V.-T. Identification of Patient Perceptions That Can Affect the Uptake of Interventions Using Biometric Monitoring Devices: Systematic Review of Randomized Controlled Trials. J. Med. Internet Res. 2020, 22, e18986. [Google Scholar] [CrossRef]
- Yang Meier, D.; Barthelmess, P.; Sun, W.; Liberatore, F. Wearable Technology Acceptance in Health Care Based on National Culture Differences: Cross-Country Analysis Between Chinese and Swiss Consumers. J. Med. Internet Res. 2020, 22, e18801. [Google Scholar] [CrossRef]
- Jiang, J.; Zhu, Q.; Zheng, Y.; Zhu, Y.; Li, Y.; Huo, Y. Perceptions and Acceptance of mHealth in Patients with Cardiovascular Diseases: A Cross-Sectional Study. JMIR Mhealth Uhealth 2019, 7, e10117. [Google Scholar] [CrossRef]
- Jiménez-Zarco, A.; Mateos, S.C.; Bosque-Prous, M.; Espelt, A.; Torrent-Sellens, J.; Adib, K.; Davtyan, K.; Santos, R.D.; Saigí-Rubió, F. Impact of the COVID-19 Pandemic on mHealth Adoption: Identification of the Main Barriers through an International Comparative Analysis. Int. J. Med. Inform. 2025, 195, 105779. [Google Scholar] [CrossRef] [PubMed]
- Getachew, E.; Adebeta, T.; Muzazu, S.G.Y.; Charlie, L.; Said, B.; Tesfahunei, H.A.; Wanjiru, C.L.; Acam, J.; Kajogoo, V.D.; Solomon, S.; et al. Digital Health in the Era of COVID-19: Reshaping the next Generation of Healthcare. Front. Public Health 2023, 11, 942703. [Google Scholar] [CrossRef]
| Cohort | ||||||
|---|---|---|---|---|---|---|
| 2014 | 2019 | |||||
| N | % | N | % | P | ||
| Age groups | ≤45 | 14 | 12.7 | 8 | 7.3 | 0.346 |
| 46–55 | 29 | 26.4 | 21 | 19.1 | ||
| 56–65 | 31 | 28.2 | 38 | 34.5 | ||
| 66–75 | 19 | 17.3 | 25 | 22.7 | ||
| 76+ | 17 | 15.5 | 18 | 16.4 | ||
| Sex | Woman | 29 | 26.4 | 21 | 19.1 | 0.198 |
| Man | 81 | 73.6 | 89 | 80.9 | ||
| Educational Level | Primary | 47 | 42.7 | 34 | 30.9 | 0.070 |
| Secondary | 35 | 31.8 | 33 | 30.0 | ||
| University+ | 28 | 25.5 | 43 | 39.1 | ||
| Working | No | 60 | 54.5 | 50 | 45.5 | 0.178 |
| Yes | 50 | 45.5 | 60 | 54.5 | ||
| Living in | House | 78 | 70.9 | 69 | 62.7 | 0.198 |
| Apartment | 32 | 29.1 | 41 | 37.3 | ||
| Living with other | Yes | 98 | 89.1 | 93 | 84.5 | 0.319 |
| Cohort | ||||||
|---|---|---|---|---|---|---|
| 2014 | 2019 | |||||
| N | % | N | % | P | ||
| Hobbies | Yes | 39 | 35.5 | 46 | 41.8 | 0.332 |
| Hobbies, f | Never | 71 | 64.5 | 64 | 58.2 | 0.798 |
| Rarely | 8 | 7.3 | 9 | 8.2 | ||
| Monthly | 2 | 1.8 | 3 | 2.7 | ||
| 1–2 times/week | 15 | 13.6 | 21 | 19.1 | ||
| Everyday | 14 | 12.7 | 13 | 11.8 | ||
| Travels/Trips | Yes | 75 | 68.2 | 86 | 78.2 | 0.094 |
| Travels/Trips, f | Never | 35 | 31.8 | 24 | 21.8 | 0.011 |
| Rarely | 26 | 23.6 | 39 | 35.5 | ||
| Yearly | 21 | 19.1 | 20 | 18.2 | ||
| Every 2–3 years | 17 | 15.5 | 6 | 5.5 | ||
| Often | 11 | 10.0 | 21 | 19.1 | ||
| Sports | Yes | 70 | 63.6 | 92 | 83.6 | 0.001 |
| Sports, f | Systematic | 27 | 24.5 | 36 | 32.7 | 0.010 |
| Periodically | 19 | 17.3 | 23 | 20.9 | ||
| Rarely | 24 | 21.8 | 33 | 30.0 | ||
| Never | 40 | 36.4 | 18 | 16.4 | ||
| Remotely Recording of Vital Signs | P | |||||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| N | % | N | % | |||
| Cohort | 2014 | 66 | 60.0 | 44 | 40.0 | <0.001 |
| 2019 | 93 | 84.5 | 17 | 15.5 | ||
| Sex | Woman | 34 | 68.0 | 16 | 32.0 | 0.443 |
| Man | 125 | 73.5 | 45 | 26.5 | ||
| Age groups | ≤45 | 19 | 86.4 | 3 | 13.6 | 0.158 |
| 46–55 | 39 | 78.0 | 11 | 22.0 | ||
| 56–65 | 51 | 73.9 | 18 | 26.1 | ||
| 66–75 | 29 | 65.9 | 15 | 34.1 | ||
| 76+ | 21 | 60.0 | 14 | 40.0 | ||
| Working | No | 73 | 66.4 | 37 | 33.6 | 0.050 |
| Yes | 86 | 78.2 | 24 | 21.8 | ||
| Educational Level | Primary | 51 | 63.0 | 30 | 37.0 | 0.062 |
| Secondary | 53 | 77.9 | 15 | 22.1 | ||
| University+ | 55 | 77.5 | 16 | 22.5 | ||
| Hobbies | Yes | 67 | 42.1 | 18 | 29.5 | 0.085 |
| Trips/Travels | Yes | 122 | 75.8 | 37 | 62.7 | 0.055 |
| Score | Cohort | Mean | SD | p* |
|---|---|---|---|---|
| Observation of biosignals | 2014 | 6.5 | 3.9 | 0.969 |
| 2019 | 6.5 | 2.9 | (0.857) | |
| Annoyance/Inconvenience of recording | 2014 | 14.5 | 5.9 | 0.503 |
| 2019 | 14.1 | 4.2 | (0.244) | |
| Technological Literacy | 2014 | 21.2 | 6.7 | 0.026 |
| 2019 | 19.4 | 5.7 | (0.002) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsoumani, N.; Klironomos, I.; Antona, M.; Kampanis, N.; Kochiadakis, G.E.; Stephanidis, C.; Karageorgos, S.; Notas, G. Cross-Sectional Study of the Changes in Attitudes of Post-Acute Coronary Syndromes Patients Towards Remote Biosignal Monitoring an eHealth Support in a 5-Year Interval. J. Clin. Med. 2025, 14, 6272. https://doi.org/10.3390/jcm14176272
Tsoumani N, Klironomos I, Antona M, Kampanis N, Kochiadakis GE, Stephanidis C, Karageorgos S, Notas G. Cross-Sectional Study of the Changes in Attitudes of Post-Acute Coronary Syndromes Patients Towards Remote Biosignal Monitoring an eHealth Support in a 5-Year Interval. Journal of Clinical Medicine. 2025; 14(17):6272. https://doi.org/10.3390/jcm14176272
Chicago/Turabian StyleTsoumani, Natalia, Iosif Klironomos, Margherita Antona, Nikos Kampanis, George E. Kochiadakis, Constantine Stephanidis, Spyridon Karageorgos, and George Notas. 2025. "Cross-Sectional Study of the Changes in Attitudes of Post-Acute Coronary Syndromes Patients Towards Remote Biosignal Monitoring an eHealth Support in a 5-Year Interval" Journal of Clinical Medicine 14, no. 17: 6272. https://doi.org/10.3390/jcm14176272
APA StyleTsoumani, N., Klironomos, I., Antona, M., Kampanis, N., Kochiadakis, G. E., Stephanidis, C., Karageorgos, S., & Notas, G. (2025). Cross-Sectional Study of the Changes in Attitudes of Post-Acute Coronary Syndromes Patients Towards Remote Biosignal Monitoring an eHealth Support in a 5-Year Interval. Journal of Clinical Medicine, 14(17), 6272. https://doi.org/10.3390/jcm14176272








