Tooth Autotransplantation in Contemporary Dentistry: A Narrative Review of Its Clinical Applications and Biological Basis
Abstract
1. Introduction
2. Methods
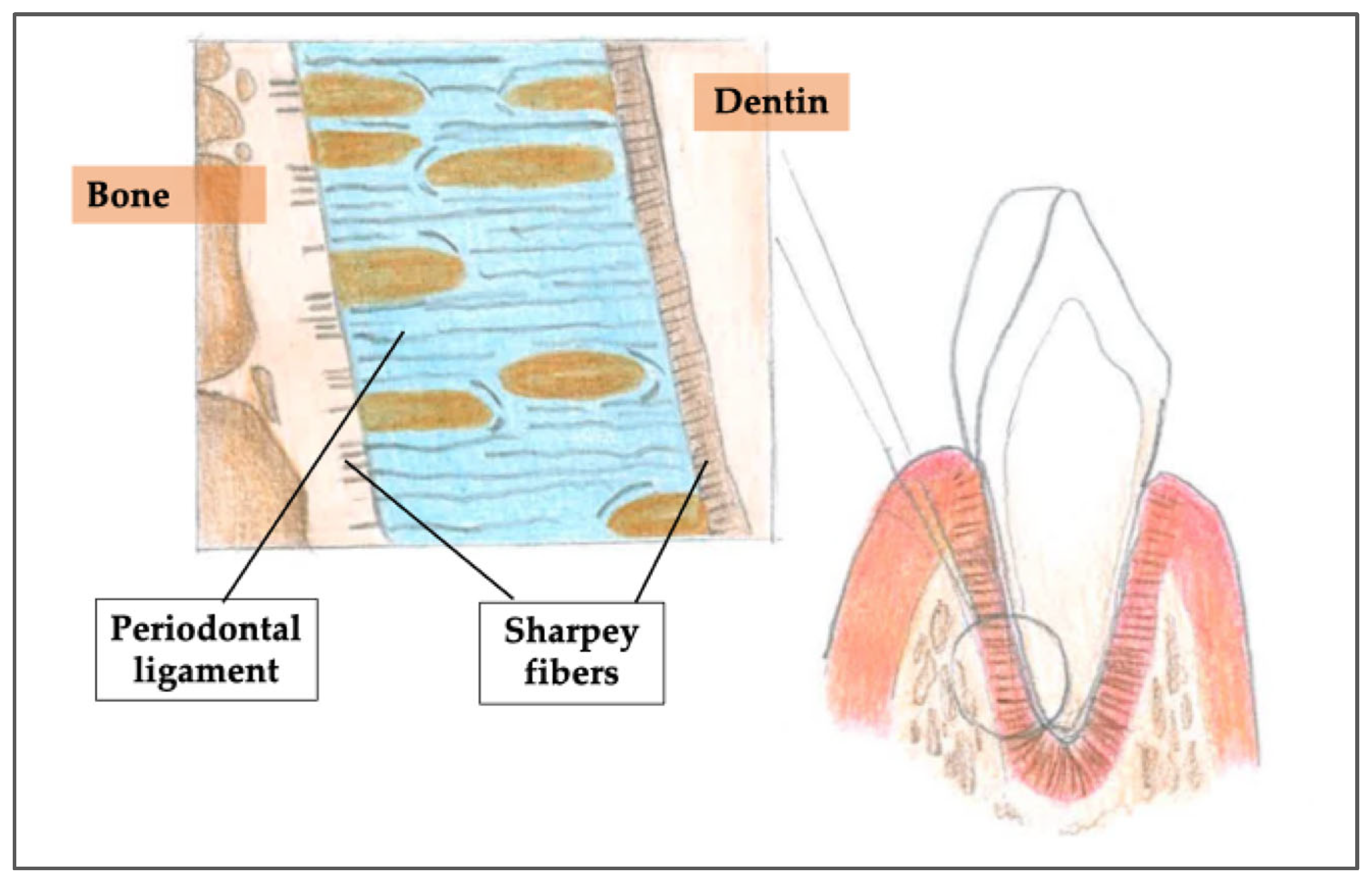
3. Biological Basis and Histological Mechanisms of Tooth Autotransplantation
4. Root Resorption in Tooth Autotransplantation
4.1. Types of External Root Resorption: Autotransplantation-Related and Its Pathophysiology
4.1.1. Surface Resorption
4.1.2. Inflammatory Root Resorption
4.1.3. Replacement Resorption (Ankylosis-Related Resorption)
4.2. Clinical Implications
4.3. Factors Contributing to Root Resorption
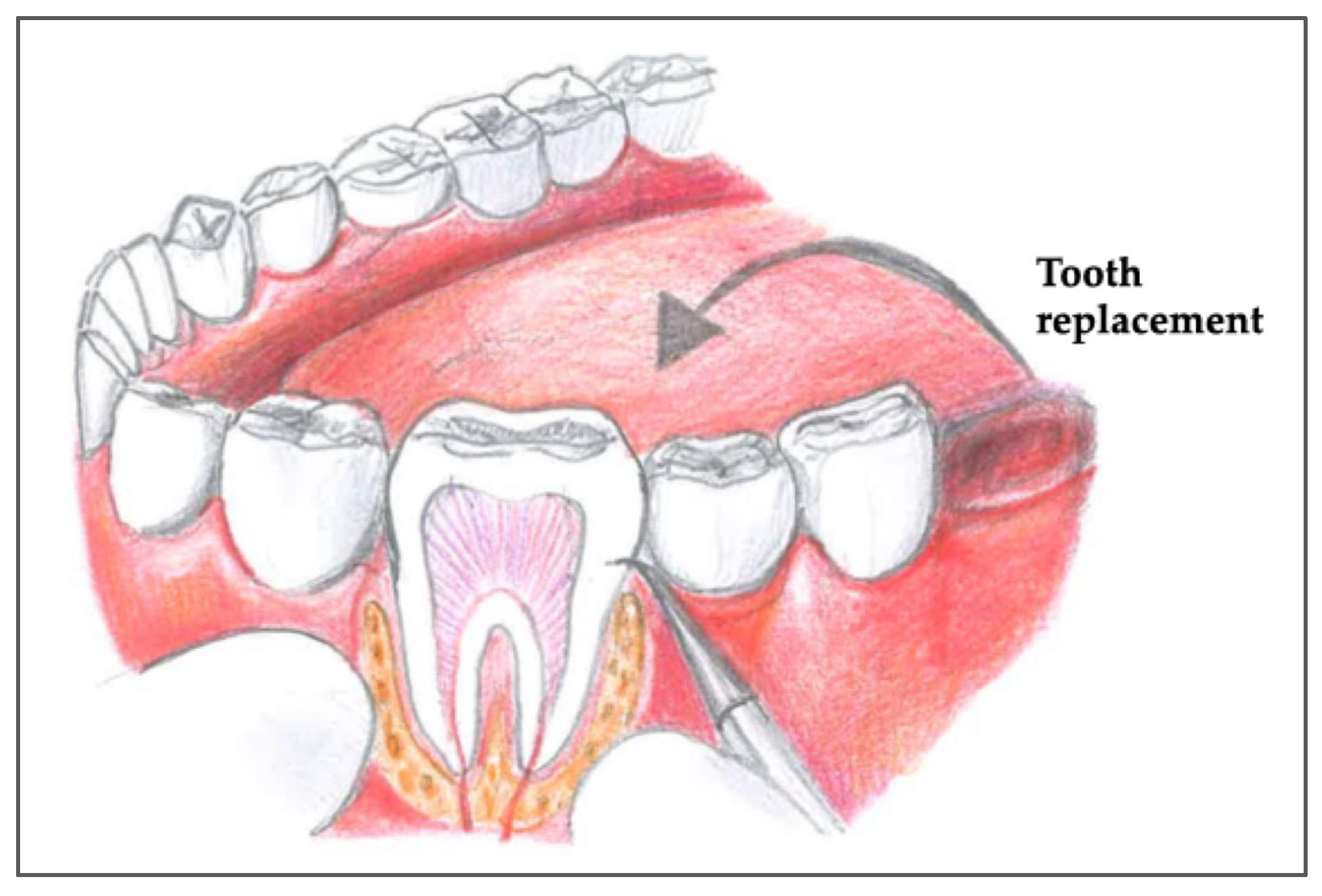
5. A Step-by-Step Surgical Protocol for Tooth Autotransplantation
5.1. Donor Tooth Selection
5.2. Preparation of the Recipient Site
5.3. Atraumatic Explantation of the Donor Tooth
5.4. Insertion and Stabilization of the Donor Tooth
5.5. Patient and Case Selection for Optimal Outcomes
- (A)
- Pediatric-Specific Indications
- Traumatic Tooth Loss: Frequently observed in children and adolescents, especially in anterior regions. Autotransplantation of premolars can restore function and esthetics while preserving alveolar bone growth.
- Congenitally Missing Teeth: Commonly involving lateral incisors or second premolars. Premolar autotransplantation serves as a viable alternative to implants, which are contraindicated during skeletal growth.
- Ectopic and Impacted Teeth: Impacted canines and other teeth can be surgically repositioned using autotransplantation, particularly when orthodontic traction is not feasible or would require prolonged treatment.
- (B)
- Surgical Protocol Considerations
- Immature Roots with Open Apices (>1 mm): Preferred because they enhance revascularization and pulpal healing.
- Minimal Extraoral Time and Atraumatic Extraction: Essential for maintaining PDL viability and supporting continued root development.
- Avoidance of Rigid Fixation: Semi-rigid splinting is recommended to allow for physiological mobility and prevent ankylosis, which is particularly detrimental in growing patients.
5.6. Prevention and Management
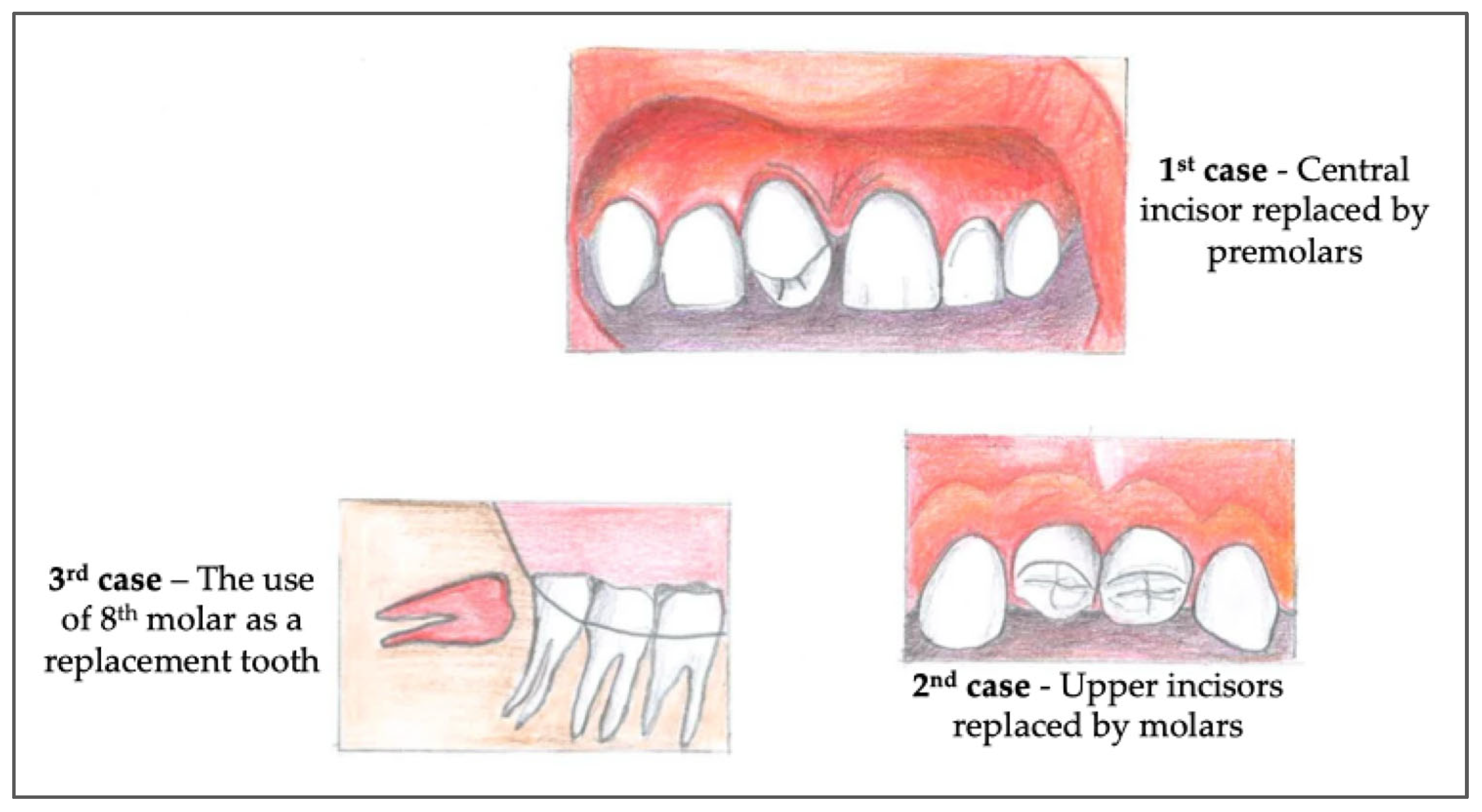
6. Types of Cases in Tooth Autotransplantation
6.1. Replacement of Missing or Extracted Teeth
6.2. Management of Traumatic Tooth Loss
6.3. Treatment of Congenitally Missing Teeth
6.4. Orthodontic Space Closure and Malocclusion Management
6.5. Replacement of Non-Restorable Teeth
6.6. Adjunct to Regenerative Procedures
6.7. Management of Impacted or Ectopically Positioned Teeth
7. Clinical Decision-Making Approach for Case Selection
7.1. Classification and Timing of Dental Autotransplantation
- Immediate autotransplantation is performed directly following tooth extraction or avulsion, before significant alveolar remodeling has occurred.
- Delayed autotransplantation typically takes place within 15 to 20 days post-extraction, allowing initial healing while maintaining socket architecture.
- Late autotransplantation involves transplanting a tooth after complete healing of the recipient site. In such cases, the socket must be surgically reconstructed (alveoloplasty), often supplemented by orthodontic splinting to ensure stability and alignment.
- Dry environment: ~18 min of viability;
- Saline: <2 h;
- Milk: up to 3 h;
- HBSS: up to 24 h (considered the gold standard in the United States).
- 1.
- Donor Tooth Selection: A detailed evaluation of both the receiving site and the donor tooth anatomy is performed to assess anatomical compatibility and identify any contraindications.
- 2.
- Explantation: A gentle explantation is mandatory, avoiding PDL damage; an orthodontic pre-treatment should be performed to simplify the procedure because it causes tooth mobility.
- 3.
- Tooth Repositioning and Splinting: The tooth is reinserted into the socket with minimal pressure and stabilized using a semi-rigid splint. It is crucial that the splint permits slight physiological mobility and does not exert tension on the tooth, which could disrupt reattachment. The recommended duration of splinting varies:
- ○
- One week, as per Andreasen’s protocol.
- ○
- Two–three weeks according to Tsukiboshi’s guidelines.
During this period, pulp vitality and signs of healing are closely monitored. - 4.
- Gingival Suturing: Soft tissue margins are approximated and sutured to reestablish mucogingival continuity and protect the surgical site.
- 5.
- Post-Operative Radiography: A periapical radiograph is obtained immediately after reimplantation to confirm accurate repositioning and stabilization.
- 6.
- Pharmacologic Support: Post-operative management includes topical antiseptics (0.2% chlorhexidine mouthwash for 30 days) and systemic antibiotics for 7 days to minimize infection risk and support periodontal healing.
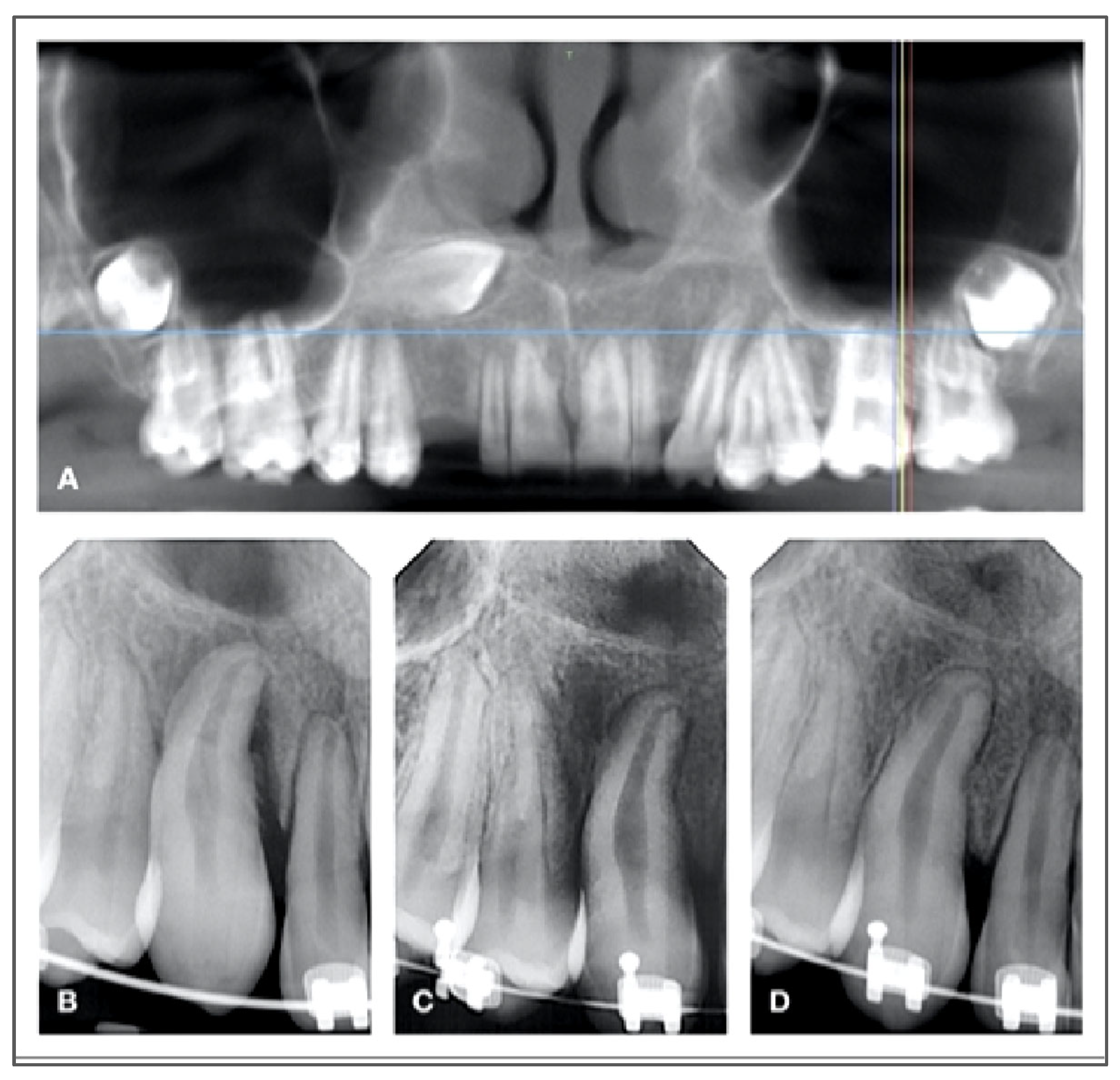
7.2. Endodontic Considerations and Healing Dynamics
- Teeth with complete root development typically require root canal therapy within two weeks post-reimplantation. This is often accompanied by the placement of an interim calcium hydroxide dressing, which promotes an antimicrobial environment and aids in monitoring periodontal healing. To delay the root canal treatment, waiting for a better stabilization of the transplanted tooth, an extraoral apicoectomy has been suggested during the surgery, because it is a fast technique that allows an immediate seal of the canals [42]. New trends propose not to treat mature transplanted teeth, suggesting potential healing [30,31].
- Teeth with incomplete root formation (open apex) are monitored for signs of pulp revascularization. If reinnervation fails to occur or if clinical or radiographic indicators of inflammatory root resorption develop, endodontic treatment becomes necessary to preserve the tooth and surrounding structures.
7.3. Age-Dependent Risk of Root Resorption
7.4. PDL Healing: Reattachment vs. New Attachment
- Reattachment involves the realignment of existing PDL fibers on the root surface with those in the alveolar socket. This process can occur rapidly, within two weeks, and restores up to two-thirds of the original biomechanical integrity of the periodontium. This type of healing is possible in cases of post-extraction transplantation in the areas of the recipient site that do not require remodeling and if there is proximity between the socket wall and the root surface.
- New attachment takes place when PDL remnants are only partially viable. In such cases, regenerative healing is required, characterized by the formation of new cementum and PDL fibers to restore attachment. This healing is slower and more vulnerable to disruption.
7.5. Surgical Techniques
7.6. Technological Advancements
8. Success Rates of Tooth Autotransplantation vs. Dental Implants
8.1. Success Rates of Tooth Autotransplantation
8.2. Success Rates of Dental Implants
8.3. Comparison of Success Rates
8.4. Cost-Effectiveness
9. Limitations and Future Outcomes of Tooth Autotransplantation
9.1. Limitations
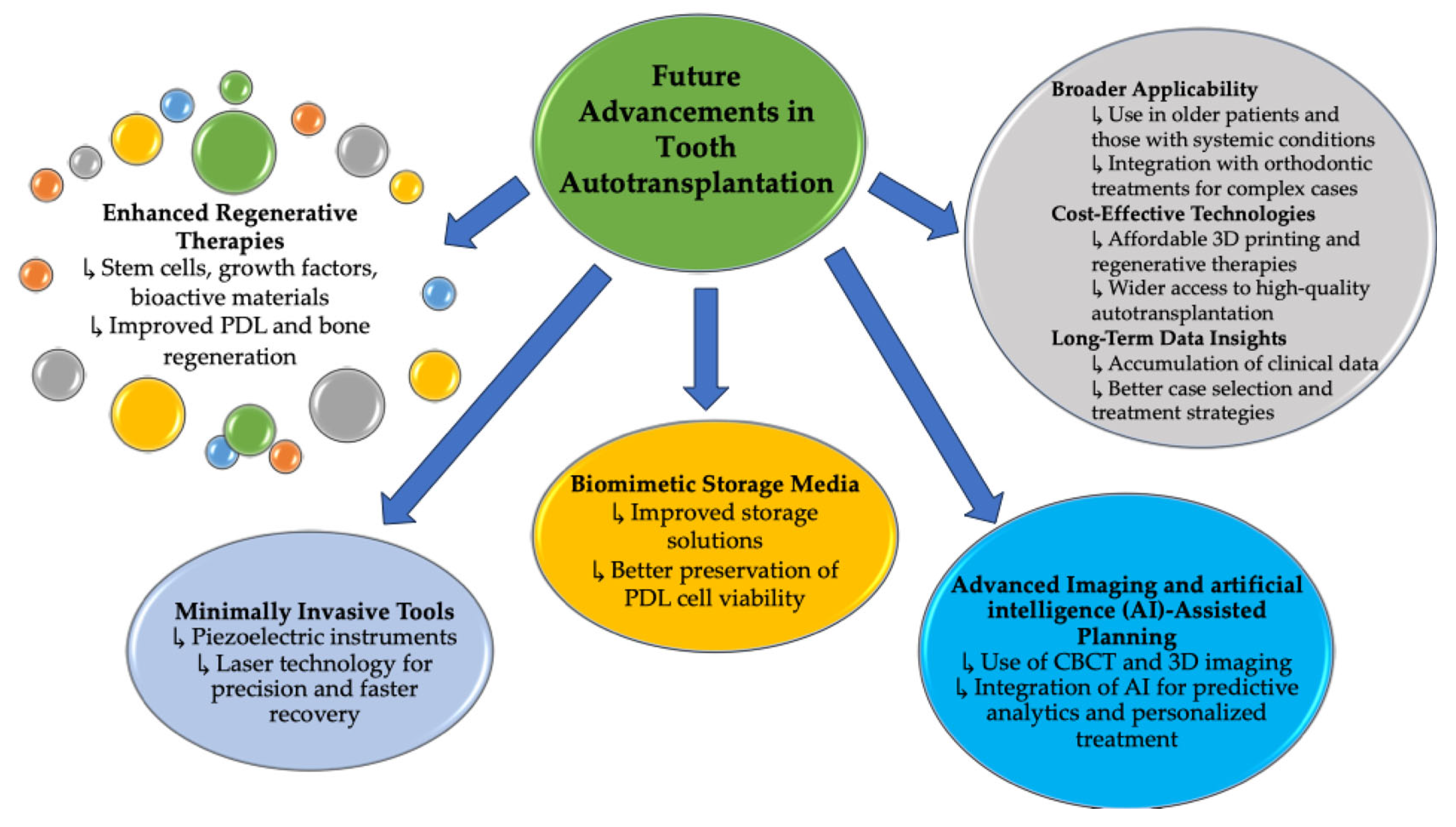
9.2. Future Advancements
10. Discussion
11. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Nimčenko, T.; Omerca, G.; Varinauskas, V.; Bramanti, E.; Signorino, F.; Cicciù, M. Tooth auto-transplantation as an alternative treatment option: A literature review. Dent. Res. J. 2013, 10, 1–6. [Google Scholar] [CrossRef]
- Doomen, R.; Barendregt, D.; Temmerman, L.; De Roo, N.; De Pauw, G. Premolar Autotransplantation to the Anterior Maxilla Region-Aesthetic Outcome and Patient Satisfaction. Dent. Traumatol. 2025; Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Krupp, J.; Petrakakis, P.; Jost-Brinkmann, P.G.; Meinzer, S.; Widbiller, M.; Niederle, C.; Geserick, M.; Nolte, D. Survival of retained permanent canines after autotransplantation: A retrospective cohort study. Am. J. Orthod. Dentofacial Orthop. 2024, 165, 533–545. [Google Scholar] [CrossRef] [PubMed]
- Guerini, V. A History of Dentistry from the Most Ancient Times Until the End of the Eighteenth Century; Lea & Febiger: New York, NY, USA; Philadelphia, PA, USA, 1909; p. 355. Available online: https://catalog.lib.unc.edu/catalog/UNCb1905784 (accessed on 15 February 2024).
- Natiella, J.R.; Armitage, J.E.; Greene, G.W. The replantation and transplantation of teeth. A review. Oral. Surg. Oral. Med. Oral. Pathol. 1970, 29, 397–419. [Google Scholar] [CrossRef]
- Andersson, L.; Bakland, L.K.; Heithersay, G.S.; Lauridsen, E. Jens Ove Andreasen, 1935–2020 Father of Dental Traumatology. Dent. Traumatol. 2021, 37, 4–16. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Hjorting-Hansen, E.; Jolst, O. A clinical and radiographic study of 76 autotransplanted third molars. Scand. J. Dent. Res. 1970, 78, 512–523. [Google Scholar] [CrossRef]
- Cross, D.; El-Angbawi, A.; McLaughlin, P.; Keightley, A.; Brocklebank, L.; Whitters, J.; McKerlie, R.; Cross, L.; Welbury, R. Developments in autotransplantation of teeth. Surgeon 2013, 11, 49–55. [Google Scholar] [CrossRef]
- Pasqualini, U.; Pasqualini, M.E. Treatise of Implant Dentistry: The Italian Tribute to Modern Implantology; Ariesdue: Carimate, Italy, 2009. [Google Scholar] [PubMed]
- Clokie, C.M.; Yau, D.M.; Chano, L. Autogenous tooth transplantation: An alternative to dental implant placement? J. Can. Dent. Assoc. 2001, 67, 92–96. [Google Scholar]
- Akhlef, Y.; Hosseini, M.; Schwartz, O.; Andreasen, J.O.; Gerds, T.A.; Jensen, S.S. Autotransplantation of Premolars to the Anterior Maxilla: A Long-Term Retrospective Cohort Study of Survival, Success, Esthetic, and Patient-Reported Outcome With up to 38-Year Follow-Up. Dent. Traumatol. 2025, 41, 322–337. [Google Scholar] [CrossRef]
- Kakde, K.K.R. Tooth Autotransplantation as an Alternative Biological Treatment: A Literature Review. Cureus 2022, 14, e30491. [Google Scholar] [CrossRef]
- Ong, D.; Itskovich, Y.; Dance, G. Autotransplantation: A viable treatment option for adolescent patients with significantly compromised teeth. Aust. Dent. J. 2016, 61, 396–407. [Google Scholar] [CrossRef]
- Jiang, N.; Guo, W.; Chen, M.; Zheng, Y.; Zhou, J.; Kim, S.G.; Embree, M.C.; Songhee Song, K.; Marao, H.F.; Mao, J.J. Periodontal Ligament and Alveolar Bone in Health and Adaptation: Tooth Movement. Front. Oral Biol. 2016, 18, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Algubeal, H.M.; Alanazi, A.F.; Arafat, A.S.; Fatani, B.; Al-Omar, A. Autotransplantation of the Lower Posterior Teeth: A Comprehensive Review. Cureus 2022, 14, e27875. [Google Scholar] [CrossRef] [PubMed]
- Zeichner-David, M.; Oishi, K.; Su, Z.; Zakartchenko, V.; Chen, L.S.; Arzate, H.; Bringas, P., Jr. Role of Hertwig’s epithelial root sheath cells in tooth root development. Dev. Dyn. 2003, 228, 651–663. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Tai, K.; Hayashi, D. Tooth autotransplantation as a treatment option: A review. J. Clin. Pediatr. Dent. 2010, 35, 129–135. [Google Scholar] [CrossRef]
- Thalakiriyawa, D.S.; Dissanayaka, W.L. Advances in Regenerative Dentistry Approaches: An Update. Int. Dent. J. 2024, 74, 25–34. [Google Scholar] [CrossRef]
- Abbott, P.V.; Lin, S. Tooth resorption-Part 2: A clinical classification. Dent. Traumatol. 2022, 38, 267–285. [Google Scholar] [CrossRef]
- Tsukiboshi, M.; Yamauchi, N.; Tsukiboshi, Y. Long-term outcomes of autotransplantation of teeth: A case series. Dent. Traumatol. 2019, 35, 358–367. [Google Scholar] [CrossRef]
- Lin, S.; Marvidou, A.M.; Novak, R.; Moreinos, D.; Abbott, P.V.; Rotstein, I. Pathogenesis of non-infection related inflammatory root resorption in permanent teeth: A narrative review. Int. Endod. J. 2023, 56, 1432–1445. [Google Scholar] [CrossRef]
- Trope, M. Root resorption of dental and traumatic origin: Classification based on etiology. Pract. Periodontics Aesthet. Dent. 1998, 10, 515–522. [Google Scholar]
- Fuss, Z.; Tsesis, I.; Lin, S. Root resorption—Diagnosis, classification and treatment choices based on stimulation factors. Dent. Traumatol. 2003, 19, 175–182. [Google Scholar] [CrossRef]
- Asgary, S.; Dianat, O. Invasive Cervical Root Resorption: A Comprehensive Review on Pathogenesis, Diagnosis, and Treatment. Iran. Endod. J. 2024, 19, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Kitaura, H.; Marahleh, A.; Ohori, F.; Noguchi, T.; Shen, W.R.; Qi, J.; Nara, Y.; Pramusita, A.; Kinjo, R.; Mizoguchi, I. Osteocyte-Related Cytokines Regulate Osteoclast Formation and Bone Resorption. Int. J. Mol. Sci. 2020, 21, 5169. [Google Scholar] [CrossRef]
- Tsukiboshi, M.; Tsukiboshi, C.; Levin, L. A step-by step guide for autotransplantation of teeth. Dent. Traumatol. 2023, 39, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Dokova, A.F.; Lee, J.Y.; Mason, M.; Moretti, A.; Reside, G.; Christensen, J. Advancements in tooth autotransplantation. J. Am. Dent. Assoc. 2024, 155, 475–483. [Google Scholar] [CrossRef]
- Pini Prato, G.; Franceschi, D.; Pace, R.; Di Gianfilippo, R. Translational approach to tooth autotransplantation: A 27-year case study. Clin. Adv. Periodontics 2024, 14, 165–171. [Google Scholar] [CrossRef]
- Ajay, S.V.; Vishnani, R. From Concept to Clinical Practice: A Review of Autotransplantation Techniques and Their Impact on Dentistry. Cureus 2024, 16, e66904. [Google Scholar] [CrossRef]
- Murtadha, L.; Kwok, J. Do Autotransplanted Teeth Require Elective Root Canal Therapy? A Long-Term Follow-Up Case Series. J. Oral. Maxillofac. Surg. 2017, 75, 1817–1826. [Google Scholar] [CrossRef]
- Sezer, B.; Şen Yavuz, B.; Korkut, B.; Menteş, A. Nine-year Follow-up of Autotransplantation in the Maxillary Anterior Region: Replacing a Fused Incisor with a Supernumerary Tooth. J. Endod. 2025, 51, 781–787. [Google Scholar] [CrossRef]
- Ji, H.; Ren, L.; Han, J.; Wang, Q.; Xu, C.; Fan, Y.; Zhang, W.; Ge, X.; Meng, X.; Yu, F. Tooth autotransplantation gives teeth a second chance at life: A case series. Heliyon 2023, 9, e15336. [Google Scholar] [CrossRef]
- Dixit, A.; Randhawa, R.K.; Randhawa, G.S.; Nimavat, A.; Patel, T.; Jani, Y. Autogenic Molar Transplantation of Third Molar with Complete Root Formation Versus Incomplete Root Formation: A Prospective Clinical Study. J. Pharm. Bioallied Sci. 2024, 16, S2168–S2171. [Google Scholar] [CrossRef]
- Hasan, M.R.; Takebe, H.; Shalehin, N.; Obara, N.; Saito, T.; Irie, K. Effects of tooth storage media on periodontal ligament preservation. Dent. Traumatol. 2017, 33, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Fagundes, N.C.F.; Bittencourt, L.O.; Magno, M.B.; Marques, M.M.; Maia, L.C.; Lima, R.R. Efficacy of Hank’s balanced salt solution compared to other solutions in the preservation of the periodontal ligament. A systematic review and meta-analysis. PLoS ONE 2018, 13, e0200467. [Google Scholar] [CrossRef]
- Casaroto, A.R.; Hidalgo, M.M.; Sell, A.M.; Franco, S.L.; Cuman, R.K.; Moreschi, E.; Victorino, F.R.; Steffens, V.A.; Bersani-Amado, C.A. Study of the effectiveness of propolis extract as a storage medium for avulsed teeth. Dent. Traumatol. 2010, 26, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Baxmann, M.; Huth, K.C.; Kárpáti, K.; Baráth, Z. Autogenous Transplantation of Teeth Across Clinical Indications: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 5126. [Google Scholar] [CrossRef]
- Chhana, A.A.; Moretti, A.J.; Lietzan, A.D.; Christensen, J.R.; Miguez, P.A. A Narrative and Case-Illustrated Review on Dental Autotransplantation Identifying Current Gaps in Knowledge. J. Clin. Med. 2025, 14, 17. [Google Scholar] [CrossRef]
- Kaur, I.P.; Kumar, A.; Kumar, M.; Jha, K. Successful outcome of permanent maxillary incisor reimplanted after 30 hours of extra-oral time-a case report with 5-year follow-up. Clin. Case Rep. 2023, 11, e7721. [Google Scholar] [CrossRef]
- Lin, Z.; Huang, D.; Huang, S.; Chen, Z.; Yu, Q.; Hou, B.; Qiu, L.; Chen, W.; Li, J.; Wang, X.; et al. Expert consensus on intentional tooth replantation. Int. J. Oral. Sci. 2025, 17, 16. [Google Scholar] [CrossRef]
- Aksel, H.; Zhu, X.; Gauthier, P.; Zhang, W.; Azim, A.A.; Huang, G.T. A new direction in managing avulsed teeth: Stem cell-based de novo PDL regeneration. Stem Cell Res. Ther. 2022, 13, 34. [Google Scholar] [CrossRef]
- Ainiwaer, A.; Wang, L. Immediate Autotransplantation of Mature Third Molars to Bilateral Mandibular First Molars With Large Periapical Lesions: A Case Report. Clin. Case Rep. 2025, 13, e70581. [Google Scholar] [CrossRef]
- Walch, B.; Gaggl, A.; Zeman-Kuhnert, K.; Brandtner, C. Autotransplantation of Impacted Third Molars to DCIA Free Flap in Adolescent Patient: A Case Report. Children 2025, 12, 370. [Google Scholar] [CrossRef]
- Sartoretto, S.C.; Shibli, J.A.; Javid, K.; Cotrim, K.; Canabarro, A.; Louro, R.S.; Lowenstein, A.; Mourão, C.F.; Moraschini, V. Comparing the Long-Term Success Rates of Tooth Preservation and Dental Implants: A Critical Review. J. Funct. Biomater. 2023, 14, 142. [Google Scholar] [CrossRef]
- Lejnieks, M.; Akota, I.; Jākobsone, G.; Neimane, L.; Uribe, S.E. Clinical Efficacy of CBCT and 3D-Printed Replicas in Molar Autotransplantation: A Controlled Clinical Trial. Dent. Traumatol. 2025, 41, 161–170. [Google Scholar] [CrossRef]
- Im, J.; Kim, J.Y.; Yu, H.S.; Lee, K.J.; Choi, S.H.; Kim, J.H.; Ahn, H.K.; Cha, J.Y. Accuracy and efficiency of automatic tooth segmentation in digital dental models using deep learning. Sci. Rep. 2022, 12, 9429. [Google Scholar] [CrossRef]
- Adamska, P.; Pylińska-Dąbrowska, D.; Stasiak, M.; Sobczak-Zagalska, H.; Jusyk, A.; Zedler, A.; Studniarek, M. Tooth Autotransplantation, Autogenous Dentin Graft, and Growth Factors Application: A Method for Preserving the Alveolar Ridge in Cases of Severe Infraocclusion—A Case Report and Literature Review. J. Clin. Med. 2024, 13, 3902. [Google Scholar] [CrossRef] [PubMed]



| Factors | Impact on Root Resorption |
|---|---|
| Extraoral Time | Prolonged exposure leads to PDL cell death, increasing the risk of resorption. Immediate transplantation or storing the tooth in HBSS or saline during the surgery protects the PDL and reduces this risk. |
| Explantation Trauma | Using excessive force or improper techniques can damage the PDL and cementum, exposing the root and increasing the risk of resorption. Gentle, atraumatic extraction helps protect these structures. |
| Recipient Site Conditions | Infections, lack of bone support, or poor socket preparation cause inflammation, raising the risk of resorption. Maintaining aseptic conditions, shaping the socket properly, and ensuring adequate bone volume help prevent this. |
| Stability of the Recipient Site | Strong stabilization prevents PDL reattachment, while excessive mobility delays healing, increasing the risk of ankylosis or resorption. Proper stabilization ensures successful transplantation. |
| Criteria | Recommendation | Description |
|---|---|---|
| Patient Age | Ideal ≤ 20 years | Younger patients have better healing and bone remodeling capacity |
| Donor Tooth Type | Canine, premolars, or third molars | Must have similar root morphology to recipient site |
| Root Development | Better incomplete apex (>1 mm open) | Allows revascularization and continued development |
| Recipient Site | Non-infected, sufficient bone | Adequate volume and hygiene are critical |
| Alternatives | Implants, bridges | Consider implants for adults with poor donor options |
| Management Strategies | Prevention Strategies |
|---|---|
| Endodontic Treatment: Use endodontic therapy to remove inflammation and seal defects with biocompatible materials like MTA or calcium hydroxide. | Preservation of the PDL: Use atraumatic techniques and preservation media to maintain PDL viability. |
| Biocompatible Materials: Apply MTA or Biodentine to repair resorptive lesions and support tissue regeneration. | Control of Inflammation: Use anti-inflammatory agents and antibiotics to reduce inflammation and prevent infection. |
| Surgical Interventions: Use surgical repositioning or GBR for severe cases, or tooth extraction if necessary. Regenerative therapies like PRP or stem cells can enhance healing. | Stabilization Techniques: Employ flexible splinting techniques to stabilize the tooth while allowing PDL regeneration. |
| Regular Monitoring: Use radiographs and cone-beam computed tomography (CBCT) to detect resorption early for timely intervention. |
| Estimated Timeframe for Root Resorption | Age Group |
|---|---|
| Within ~2 years | Pre-pubertal patients |
| May extend up to 10 years | Post-pubertal adults |
| Higher risk of complications including infraocclusion and esthetic concerns | Adolescents |
| Benefits | Description | Aspects |
|---|---|---|
| Ensures viability of PDL cells for reattachment and healing. | Gentle removal of the donor tooth to preserve PDL cells. | Atraumatic Extraction |
| Prevents complications like ankylosis and ensures proper occlusion. | Shaping the socket to fit the donor tooth dimensions and orientation. | Recipient Site Preparation |
| Enhances accuracy and minimizes risks to adjacent structures. | 3D imaging for detailed pre-operative planning. | CBCT Imaging |
| Ensures precise socket preparation and donor tooth alignment. | Virtual surgical planning with custom surgical guides. | Computer-Guided Surgery |
| Reduces intra-operative variability and improves efficiency. | Fabrication of patient-specific surgical templates. | 3D Printing |
| Accelerates bone and soft tissue repair, promoting better integration. | Use of PRP and PRF to enhance healing and tissue regeneration. | Adjunctive Regenerative Therapies |
| Enhances long-term outcomes by ensuring continued root development. | Techniques to maintain pulp vitality and support root growth in immature teeth. | Regenerative Endodontics |
| Reduces bleeding, minimizes discomfort, and promotes faster recovery. | Minimally invasive techniques for soft tissue management. | Laser-Assisted Surgery |
| Description | Limitations |
|---|---|
| Limited to patients with suitable donor teeth and adequate recipient site conditions. | Case Selection Constraints |
| Reduced regenerative potential and higher risk of complications in older patients. | Age-Related Challenges |
| Requires high surgical precision and expertise to preserve PDL and ensure proper placement. | Complex Surgical Technique |
| Includes root resorption, pulp necrosis, infection, and ankylosis, especially in mature teeth. | Complications and Risks |
| Lack of extensive studies on outcomes over several decades limits knowledge about durability. | Limited Long-Term Data |
| Advanced techniques and tools may not be available in all clinical settings, restricting their use. | Accessibility of Technology |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meto, A.; Çota, K.; Meto, A.; Bara, S.; Boschini, L. Tooth Autotransplantation in Contemporary Dentistry: A Narrative Review of Its Clinical Applications and Biological Basis. J. Clin. Med. 2025, 14, 6249. https://doi.org/10.3390/jcm14176249
Meto A, Çota K, Meto A, Bara S, Boschini L. Tooth Autotransplantation in Contemporary Dentistry: A Narrative Review of Its Clinical Applications and Biological Basis. Journal of Clinical Medicine. 2025; 14(17):6249. https://doi.org/10.3390/jcm14176249
Chicago/Turabian StyleMeto, Aida, Kreshnik Çota, Agron Meto, Silvana Bara, and Luca Boschini. 2025. "Tooth Autotransplantation in Contemporary Dentistry: A Narrative Review of Its Clinical Applications and Biological Basis" Journal of Clinical Medicine 14, no. 17: 6249. https://doi.org/10.3390/jcm14176249
APA StyleMeto, A., Çota, K., Meto, A., Bara, S., & Boschini, L. (2025). Tooth Autotransplantation in Contemporary Dentistry: A Narrative Review of Its Clinical Applications and Biological Basis. Journal of Clinical Medicine, 14(17), 6249. https://doi.org/10.3390/jcm14176249








