CT Angiography in Patients Referred for Invasive Coronary Angiography: A Single Large-Volume Tertiary Center Experience
Abstract
Highlights
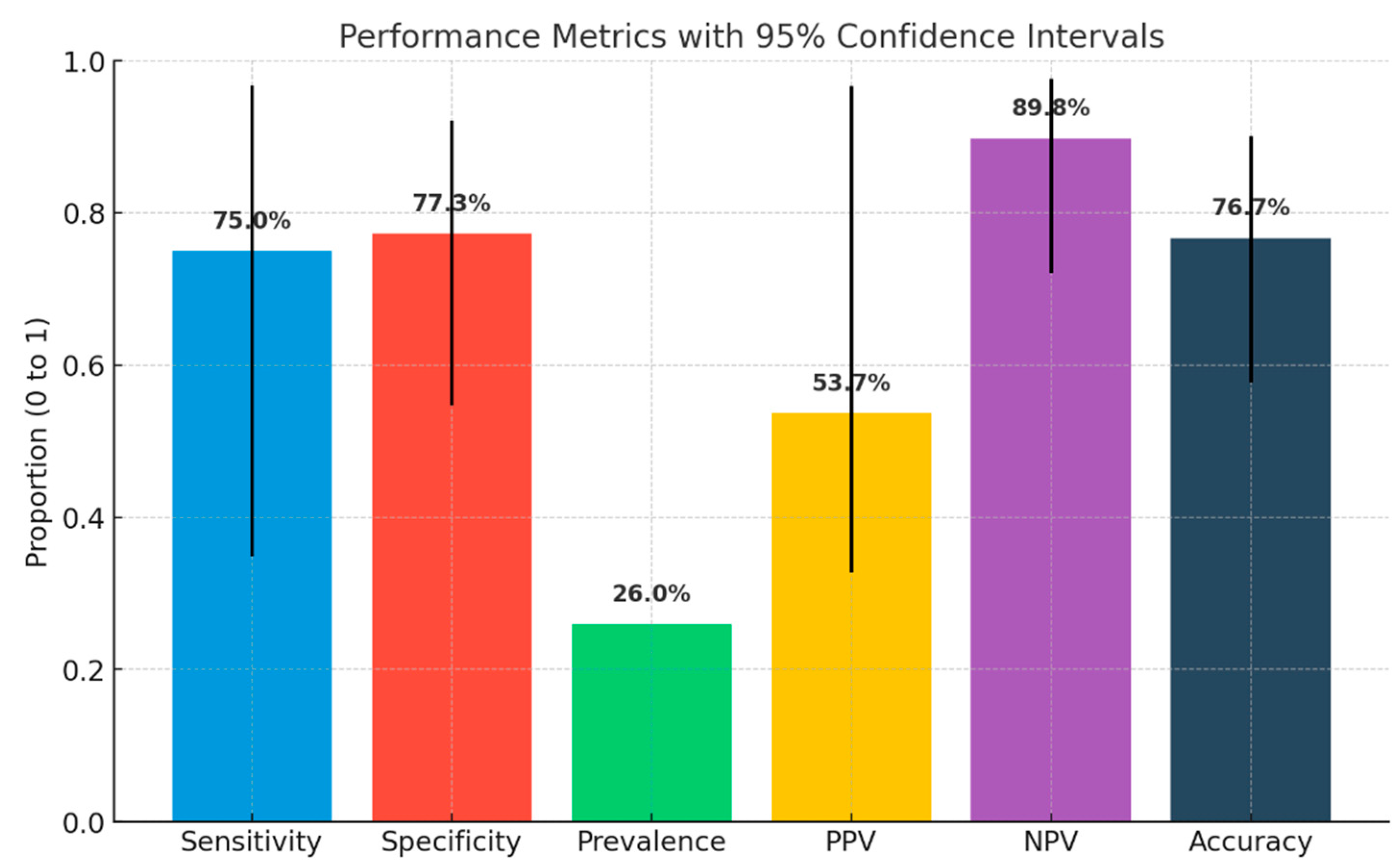
- In a real-world, single-center study, CTCA demonstrated similar long-term clinical outcomes compared to invasive coronary angiography (ICA), with no significant differences in adverse events or functional outcomes assessed by stress echocardiography.
- CTCA demonstrated a high negative predictive value (89%), confirming its reliability in safely ruling out CAD and potentially avoiding unnecessary invasive procedures.
- CTCA significantly reduced diagnostic time and hospital stay compared to ICA (4.7 vs. 20.2 h, p < 0.0001), highlighting its potential for efficient outpatient workflows.
- Despite a higher mean radiation dose in the CTCA group (2.3 mSv vs. 1.5 mSv, p = 0.03), no procedure-related complications occurred in this group, unlike the ICA arm.
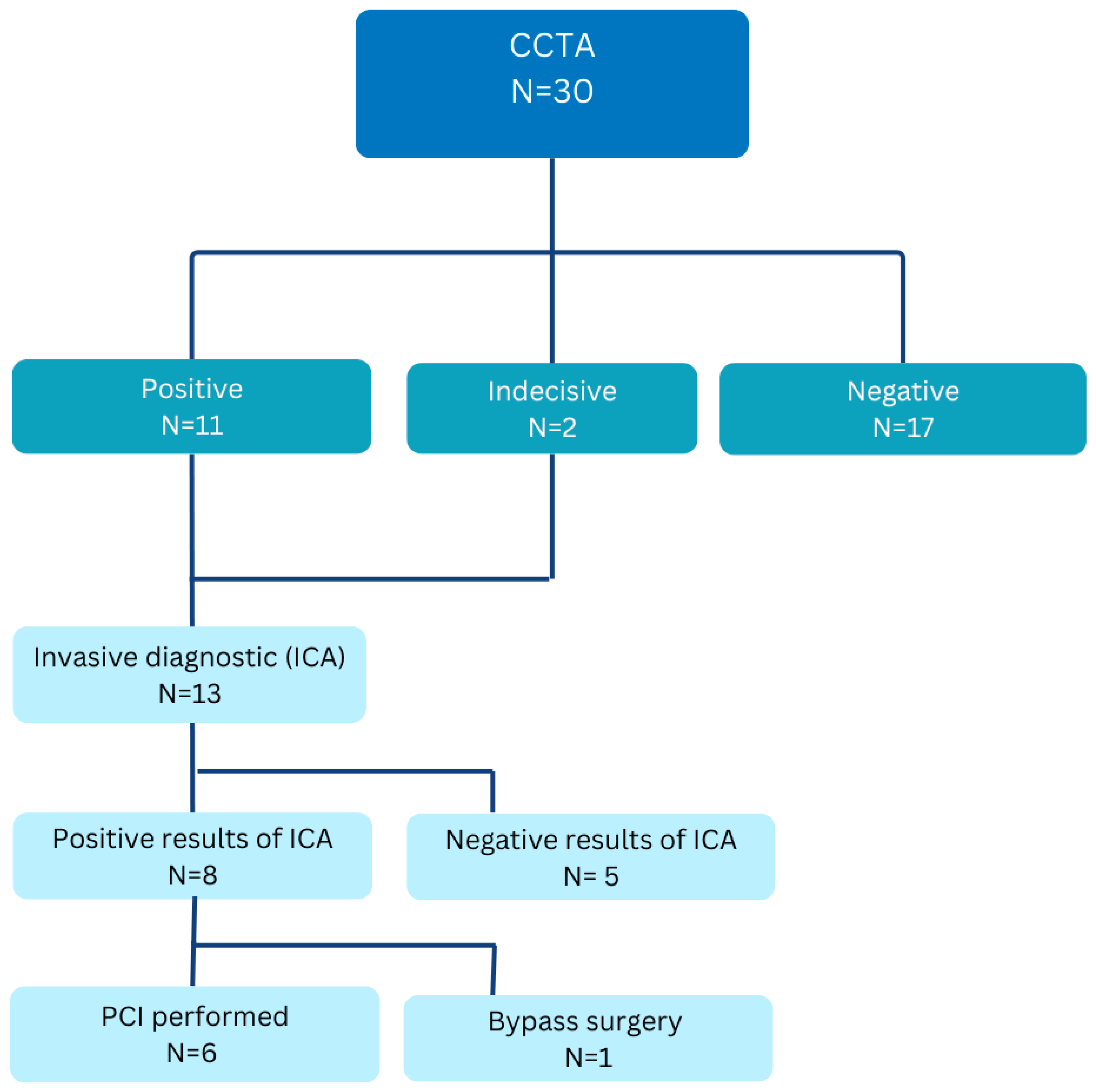
- Performance metrics of CTCA (sensitivity 75%, specificity 77%) were slightly lower than those reported in multicenter trials, possibly due to the small sample size and single-center design.
- Findings support broader implementation of CTCA as a first-line diagnostic tool in stable CAD, especially following its recent reimbursement approval in Germany (2024).
Abstract
1. Introduction
2. Methods
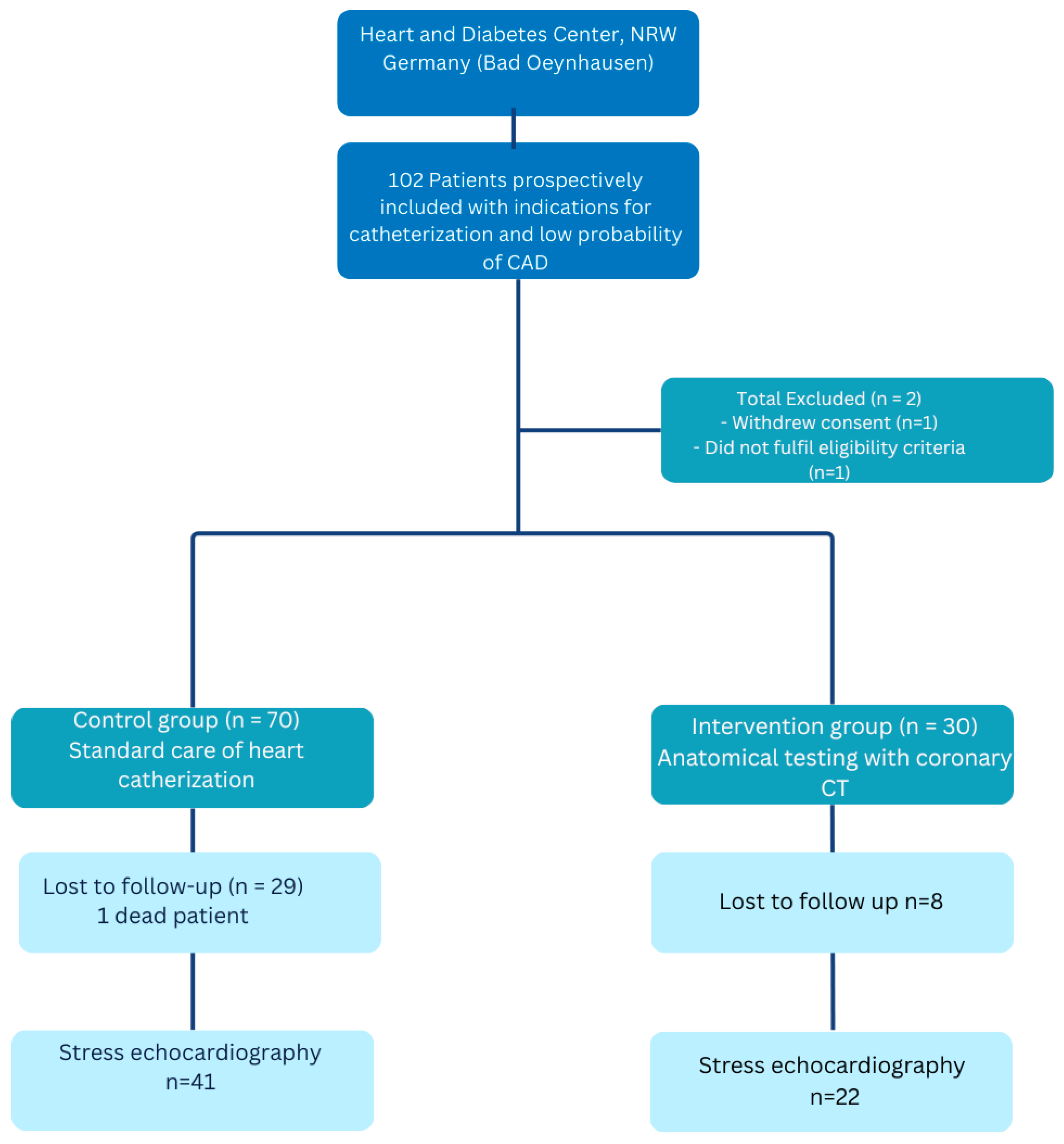
2.1. Patient Recruitment
2.2. Study Design
2.3. Endpoints
3. Statistical Analyses
4. Results
4.1. Study Population
4.2. Baseline Characteristics
4.3. Diagnostic Results
4.3.1. CTCA Arm
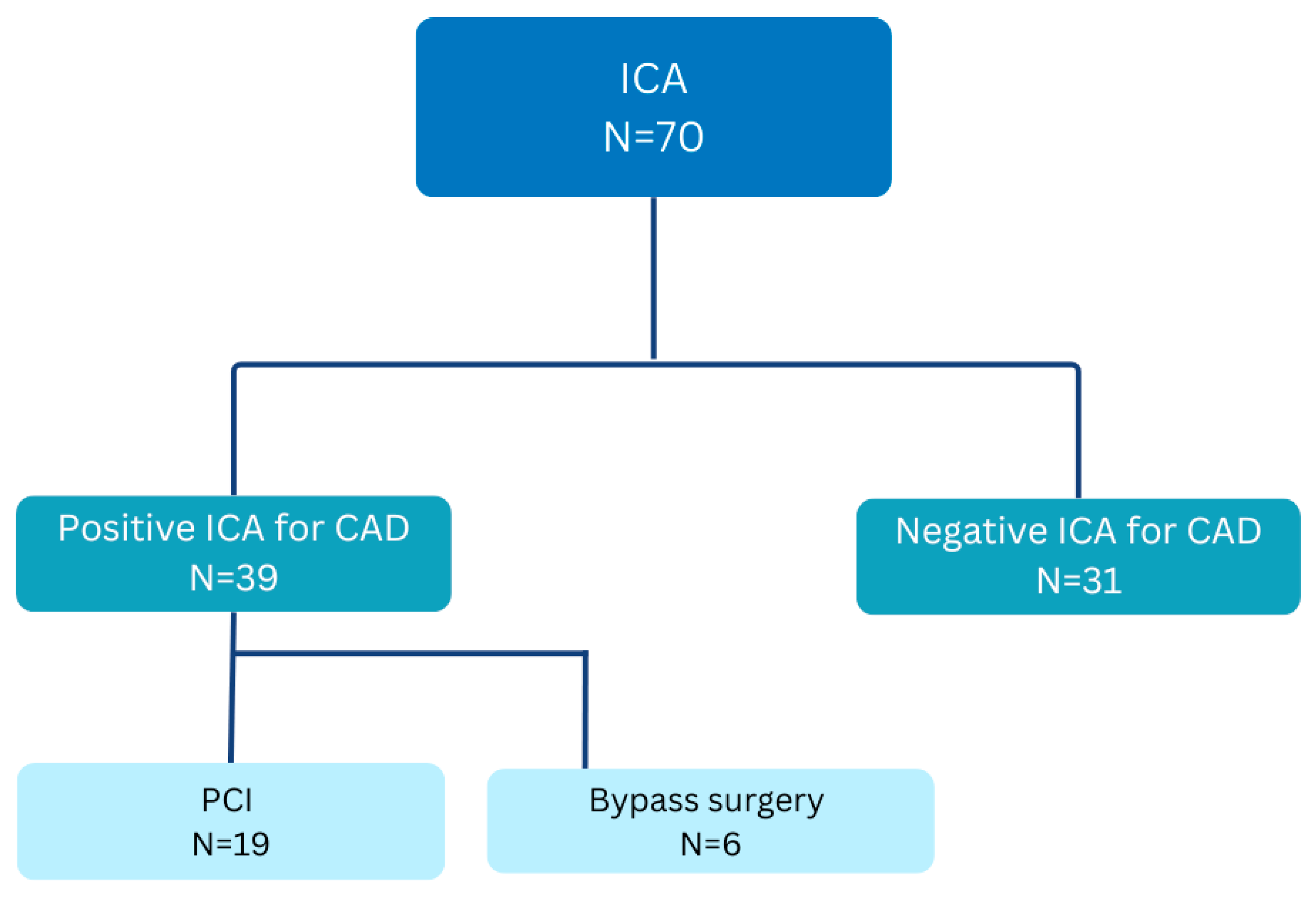
4.3.2. ICA Arm
4.4. Follow-Up and Endpoint Measures
5. Discussion and Study Limitations
Implications for Practice
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CAD | coronary artery diseases |
| CABG | coronary artery bypass grafting |
| CTCA | computed tomography coronary angiography |
| ICA | invasive coronary disease |
| Stress ECG | stress electrocardiography |
| Stress ECHO | stress echocardiography |
| WMSI | wall motion score index |
| PCI | percutaneous coronary intervention |
| CTO | chronic total occlusion |
| NPV | negative predictive value |
| PPV | positive predictive value |
| MPS | myocardial perfusion scintigraphy |
References
- Herz-Kreislauferkrankungen, RKI. Available online: https://www.rki.de/DE/Themen/Nichtuebertragbare-Krankheiten/Nichtuebertragbare-Krankheiten-A-Z/K/KHK-Herzinfarkt/koronare-herzkrankheit-myokardinfarkt-node.html (accessed on 15 June 2023).
- Douglas, P.S.; Hoffmann, U.; Patel, M.R.; Mark, D.B.; Al-Khalidi, H.R.; Cavanaugh, B.; Cole, J.; Dolor, R.J.; Fordyce, C.B.; Huang, M.; et al. PROMISE Trial, Outcomes of anatomical versus Functional Testing for Coronary Artery Disease. N. Engl. J. Med. 2015, 372, 1291–1300. [Google Scholar] [CrossRef] [PubMed]
- SCOT-Heart Investigators. SCOT-Heart Trial, Coronary CT Angiography and 5-Year Risk of Myocardial Infarction. N. Engl. J. Med. 2018, 379, 924–933. [Google Scholar] [CrossRef] [PubMed]
- DISCHARGE Trial Group. DISCHARGE Trial, CT or Invasive Coronary Angiography in Stable chest Pain. N. Engl. J. Med. 2022, 386, 1591–1602. [Google Scholar] [CrossRef] [PubMed]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef] [PubMed]
- Kardio-CT als Kassenleistung: Herzstiftung begrüßt G-BA-Beschluss, Herzstiftung. January 2024. Available online: https://herzstiftung.de/service-und-aktuelles/presse/pressemitteilungen/kardio-ct-kassenleistung (accessed on 25 August 2025).
- Sicari, R.; Pasanisi, E.; Venneri, L.; Landi, P.; Cortigiani, L.; Picano, E.; Echo Persantine International Cooperative (EPIC); Echo Dobutamine International Cooperative (EDIC) Study Groups. Stress echo results predict mortality: A large-scale multicenter prospective international study. J. Am. Coll. Cardiol. 2003, 41, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Bhatia, M. Coronary artery disease reporting and data system: A comprehensive review. J. Cardiovasc. Imaging 2021, 30, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Carroll, D.; Campos, A.; Murphy, A. Wall Motion Score index. Radiopaedia.org 2019. [Google Scholar] [CrossRef]
- Groothuis, J.G.; Beek, A.M.; Meijerink, M.R.; Brinckman, S.L.; Heymans, M.W.; van Kuijk, C.; van Rossum, A.C. Positive predictive value of computed tomography coronary angiography in clinical practice. Int. J. Cardiol. 2012, 156, 315–319. [Google Scholar] [CrossRef] [PubMed]
| Socio-Demographic Variable | Description | CT (n = 30) Mean ± SD or n (%) | ICA (n = 70) Mean ± SD or n (%) | p-Value |
| Age (years) | Self-reported | 63 ± 11.6 | 65 ± 9.4 | 0.26 |
| Male sex | 20 (66.7%) | 47 (67.1%) | 0.96 | |
| Height (cm) | Self-reported | 174 ± 6.0 | 174 ± 9.4 | 0.98 |
| Weight (kg) | Self-reported | 87 ± 18.4 | 88.3 ± 18.6 | 0.43 |
| Body mass index (kg/m2) | Calculated | 28.8 ± 5.7 | 29.1 ± 5.8 | 0.83 |
| Mean blood pressure (mmHg) | Ambulatory care | 98.8 ± 12.1 | 103 ± 13.4 | 0.14 |
| Heart rate (bpm) | Ambulatory care | 68.3 ± 10.8 | 68.8 ± 11.8 | 0.84 |
| Cardiac risk factors | ||||
| Risk Factor | Description | CT (n = 30) | ICA (n = 70) | p-Value |
| Hypertension | Pre-diagnosed | 23 (76.7%) | 59 (84.3%) | 0.36 |
| Diabetes mellitus | Pre-diagnosed | 8 (26.7%) | 22 (31.4%) | 0.63 |
| Hypercholesterolemia | Pre-diagnosed | 17 (56.7%) | 42 (60.0%) | 0.75 |
| Current smoker | Self-reported | 7 (23.3%) | 23 (32.9%) | 0.34 |
| Ex-smoker | Self-reported | 5 (16.7%) | 16 (22.9%) | 0.48 |
| Adiposity | BMI-based | 15 (50.0%) | 30 (42.9%) | 0.51 |
| Family history of CAD | Self-reported | 8 (26.7%) | 24 (34.3%) | 0.40 |
| Symptoms | ||||
| Symptom | Description | CT (n = 30) | ICA (n = 70) | p-Value |
| Angina | CCS 0–IV, self-reported | 18 (60.0%) | 38 (54.3%) | 0.90 |
| Dyspnea | Self-reported, primary/only symptom | 4 (13.3%) | 19 (27.1%) | 0.13 |
| Pre-diagnostic tests | ||||
| Test | Description | CT (n = 30) | ICA (n = 70) | p-Value |
| Pathological ECG, extremity leads | Ambulatory care | 4 (13.3%) | 11 (15.7%) | 0.76 |
| Pathological ECG, chest leads | Ambulatory care | 3 (10.0%) | 5 (7.1%) | 0.62 |
| Pathological echocardiography (wall motion) | Referring cardiologist | 2 (6.7%) | 9 (12.9%) | 0.36 |
| Stress ECG performed | Referring cardiologist | 9 (30.0%) | 32 (45.7%) | 0.14 |
| Pathological stress ECG, extremity leads | Subgroup (performed only) | 7 (77.8%) | 18 (56.3%) | 0.80 |
| Pathological stress ECG, chest leads | Subgroup (performed only) | 4 (44.4%) | 13 (40.6%) | 0.52 |
| Stress echocardiography performed | Referring cardiologist | 3 (10.0%) | 8 (11.4%) | 0.83 |
| Pathological stress echocardiography | Subgroup (performed only) | 3 (100.0%) | 6 (75.0%) | 0.81 |
| Stress myocardial scintigraphy performed | Referring cardiologist | 11 (36.7%) | 31 (44.3%) | 0.47 |
| Pathological stress myocardial scintigraphy | Subgroup (performed only) | 8 (72.7%) | 30 (96.8%) | 0.12 |
| Variable | Description | CT (n = 30) | ICA (n = 70) | p-Value |
|---|---|---|---|---|
| Coronary stenoses (all) | Any degree | 13 (43.3%) | 41 (58.6%) | 0.16 |
| Moderate stenosis | 75–90% | 3 (10.0%) | 16 (22.9%) | 0.13 |
| Severe stenosis | >90% | 3 (10.0%) | 18 (25.7%) | 0.07 |
| Chronic total occlusion (CTO) | 2 (6.7%) | 7 (10.0%) | 0.59 | |
| RCA stenosis | ICA diagnosed | 6 (46.2%) | 22 (52.9%) | 0.24 |
| RCX stenosis | ICA diagnosed | 5 (38.5%) | 24 (57.8%) | 0.07 |
| LAD stenosis | ICA diagnosed | 11 (84.6%) | 29 (69.9%) | 0.65 |
| Left main stenosis | ICA diagnosed | 1 (3.3%) | 1 (1.4%) | 0.53 |
| Hemodynamically significant stenosis | ICA diagnosed | 8 (26.7%) | 28 (40.0%) | 0.20 |
| PCI performed | Intervention | 5 (16.7%) | 18 (25.7%) | 0.32 |
| CABG performed | Surgery | 1 (3.3%) | 7 (10.0%) | 0.43 |
| RCA PCI | Intervention | 3 (10.0%) | 9 (12.9%) | 0.68 |
| RCX PCI | Intervention | 0 | 9 (12.9%) | 0.04 |
| LAD PCI | Intervention | 4 (13.3%) | 11 (15.7%) | 0.76 |
| Left main PCI | Intervention | 1 (3.3%) | 1 (1.4%) | 0.53 |
| Effective radiation dose (mSv) | Mean ± SD | 2.33 ± 1.26 | 1.70 ± 1.68 | 0.04 |
| Contrast volume (ml) | Mean ± SD (range) | 55.5 ± 6.1 (50–70) | 76.7 ± 35.4 (29–164) | <0.01 |
| Outcome | Description | CT (n = 30) | ICA (n = 70) | p-Value |
|---|---|---|---|---|
| Follow-up duration (months) | Mean ± SD | 8.6 ± 2.7 | 12.2 ± 4.8 | 0.002 |
| Cardiovascular deaths | Clinical | 0 | 1 (non-angina) | – |
| Rehospitalization for angina | Clinical | 1 (3.3%) | 1 (1.4%) | 0.90 |
| Stress echocardiography follow-up | Clinical | 22 (73.3%) | 41 (58.6%) | 0.16 |
| Angina under stress | Clinical | 1 (4.0%) | 0 | 0.19 |
| Dyspnea under stress | NYHA classification | 14 (60.0%) | 21 (51.2%) | 0.72 |
| ΔWMSI = 0 | Calculated | 22 (73.3%) | 41 (58.6%) | 0.27 |
| Variable | CT (Mean) | ICA (Mean) | p-Value |
|---|---|---|---|
| Contrast dye (mL) | 55 | 66 | 0.09 |
| Effective radiation dose (mSv) | 2.3 | 1.5 | 0.03 |
| Admission time (hours) | 4.8 ± 0.2 | 20.2 ± 11.1 | <0.0001 |
| Diagnostic time (minutes) | 23.5 | 25.5 | 0.60 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Disha, M.; Philip, L.; Dumitrescu, D.; Rudolph, V.; Brinkmann, R.; Ayoub, M. CT Angiography in Patients Referred for Invasive Coronary Angiography: A Single Large-Volume Tertiary Center Experience. J. Clin. Med. 2025, 14, 6211. https://doi.org/10.3390/jcm14176211
Disha M, Philip L, Dumitrescu D, Rudolph V, Brinkmann R, Ayoub M. CT Angiography in Patients Referred for Invasive Coronary Angiography: A Single Large-Volume Tertiary Center Experience. Journal of Clinical Medicine. 2025; 14(17):6211. https://doi.org/10.3390/jcm14176211
Chicago/Turabian StyleDisha, Migena, Legate Philip, Daniel Dumitrescu, Volker Rudolph, Regine Brinkmann, and Mohamed Ayoub. 2025. "CT Angiography in Patients Referred for Invasive Coronary Angiography: A Single Large-Volume Tertiary Center Experience" Journal of Clinical Medicine 14, no. 17: 6211. https://doi.org/10.3390/jcm14176211
APA StyleDisha, M., Philip, L., Dumitrescu, D., Rudolph, V., Brinkmann, R., & Ayoub, M. (2025). CT Angiography in Patients Referred for Invasive Coronary Angiography: A Single Large-Volume Tertiary Center Experience. Journal of Clinical Medicine, 14(17), 6211. https://doi.org/10.3390/jcm14176211







