Does Preoperative CT Improve Outcomes in Femoral Neck Fracture Fixation? A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design: Retrospective Cohort Study
| Garden Classification | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | Total | ||||||
| n | % | n | % | n | % | n | % | n | % | |
| Total | 6 | 10.91% | 25 | 45.45% | 22 | 40% | 2 | 3.64% | 55 | 100% |
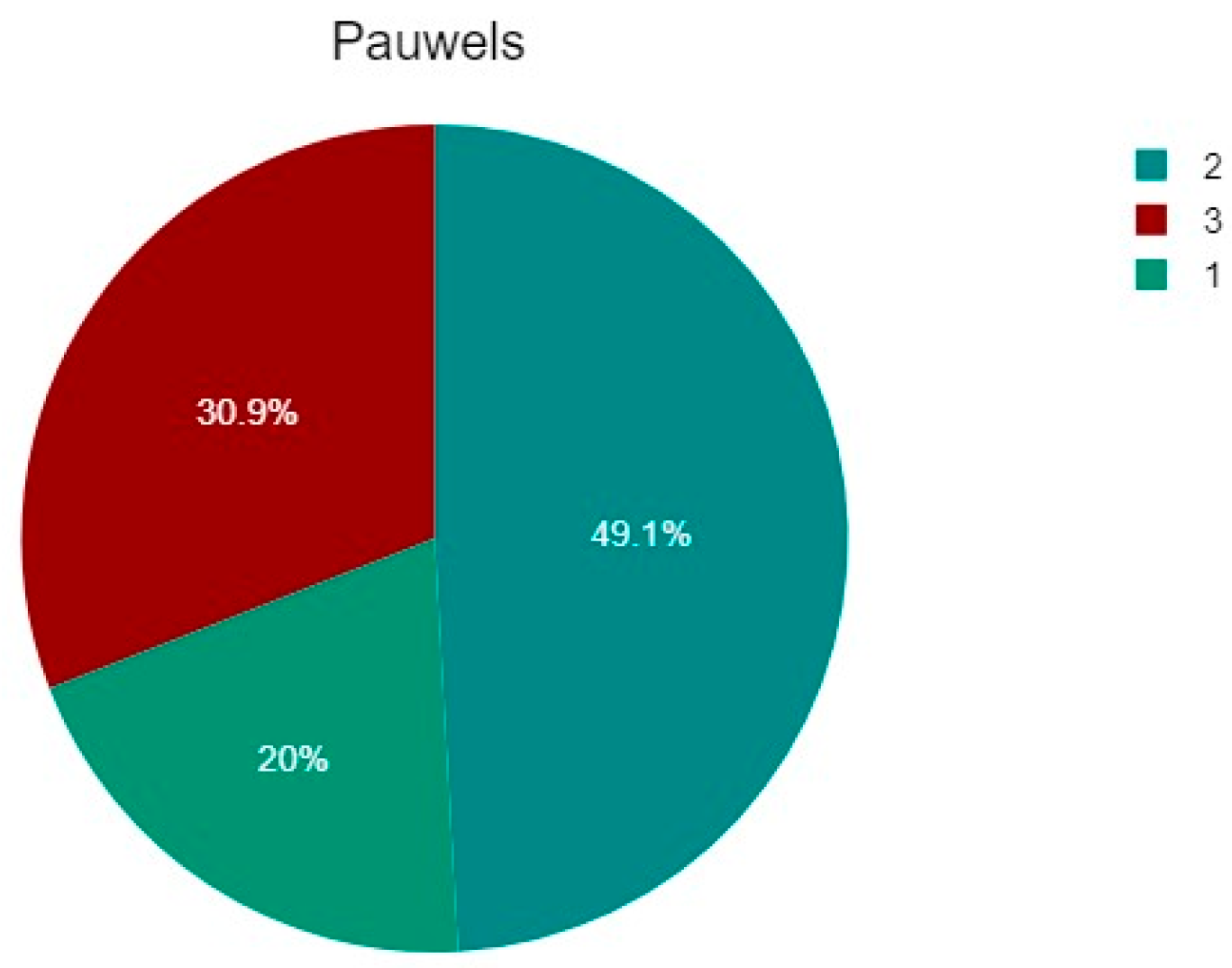
| Pauwels Classification | ||||||||||
| 1 | 2 | 3 | Total | |||||||
| n | % | n | % | n | % | n | % | |||
| Total | 11 | 20% | 27 | 49.09% | 17 | 30.91% | 55 | 100% | ||

2.2. Surgical Technique
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Saul, D.; Riekenberg, J.; Ammon, J.C.; Hoffmann, D.B.; Sehmisch, S. Hip Fractures: Therapy, Timing, and Complication Spectrum. Orthop. Surg. 2019, 11, 994–1002. [Google Scholar] [CrossRef]
- Li, L.; Bennett-Brown, K.; Morgan, C.; Dattani, R. Hip Fractures. Br. J. Hosp. Med. 2020, 81, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sànchez-Riera, L.; Wilson, N. Fragility Fractures & Their Impact on Older People. Best Pract. Res. Clin. Rheumatol. 2017, 31, 169–191. [Google Scholar] [CrossRef] [PubMed]
- Trajanoska, K.; Schoufour, J.D.; De Jonge, E.A.L.; Kieboom, B.C.T.; Mulder, M.; Stricker, B.H.; Voortman, T.; Uitterlinden, A.G.; Oei, E.H.G.; Ikram, M.A.; et al. Fracture Incidence and Secular Trends between 1989 and 2013 in a Population Based Cohort: The Rotterdam Study. Bone 2018, 114, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Jacob, G.; Pai, S.; Huggi, V.; Kotekar, M.F.; Yogesh, K.; Kumar, M.A.; Tirumalesh, G.N.; Shetty, M.S. Lag Screw with DHS (LSD) for Vertical Angle Femoral Neck Fractures in Young Adults. Injury 2020, 51, 2628–2633. [Google Scholar] [CrossRef]
- Roberts, K.C.; Brox, W.T.; Jevsevar, D.S.; Sevarino, K. Management of Hip Fractures in the Elderly. J. Am. Acad. Orthop. Surg. 2015, 23, 131–137. [Google Scholar] [CrossRef]
- Garden, R.S. Low-Angle Fixation in Fractures of the Femoral Neck. J. Bone Jt. Surg. Br. Vol. 1961, 43-B, 647–663. [Google Scholar] [CrossRef]
- Kazley, J.M.; Banerjee, S.; Abousayed, M.M.; Rosenbaum, A.J. Classifications in Brief: Garden Classification of Femoral Neck Fractures. Clin. Orthop. Relat. Res. 2018, 476, 441–445. [Google Scholar] [CrossRef]
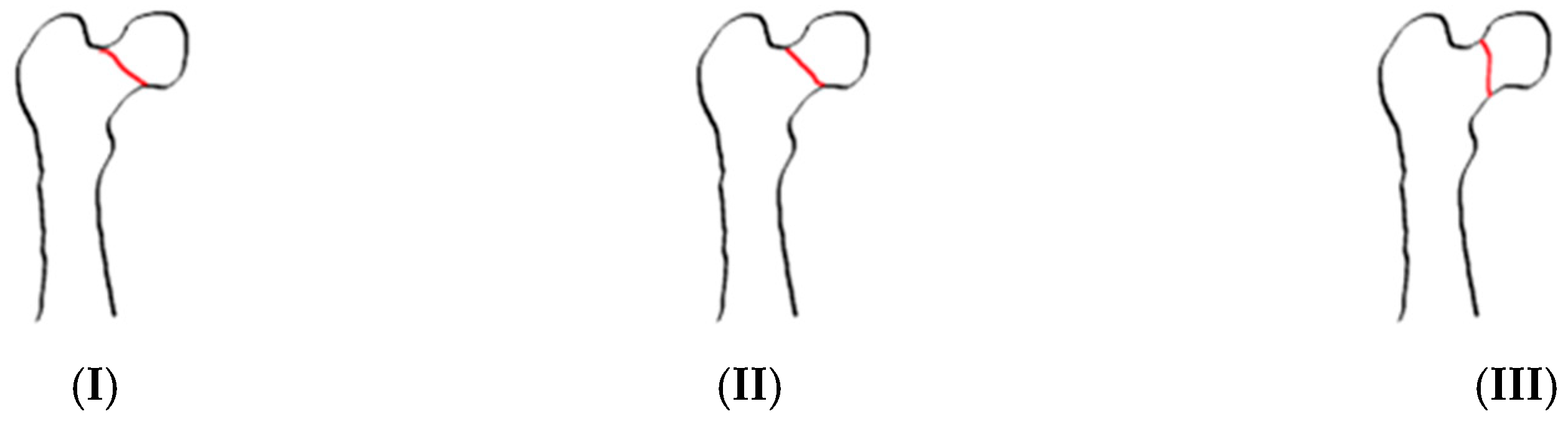
- Bartoníček, J. Pauwels’ Classification of Femoral Neck Fractures: Correct Interpretation of the Original. J. Orthop. Trauma 2001, 15, 358–360. [Google Scholar] [CrossRef]
- Augat, P.; Bliven, E.; Hackl, S. Biomechanics of Femoral Neck Fractures and Implications for Fixation. J. Orthop. Trauma 2019, 33, S27–S32. [Google Scholar] [CrossRef]
- Xu, D.-F.; Bi, F.-G.; Ma, C.-Y.; Wen, Z.-F.; Cai, X.-Z. A Systematic Review of Undisplaced Femoral Neck Fracture Treatments for Patients over 65 Years of Age, with a Focus on Union Rates and Avascular Necrosis. J. Orthop. Surg. Res. 2017, 12, 28. [Google Scholar] [CrossRef]
- Wang, X.; Lan, H.; Li, K. Treatment of Femoral Neck Fractures with Cannulated Screw Invasive Internal Fixation Assisted by Orthopaedic Surgery Robot Positioning System. Orthop. Surg. 2019, 11, 864–872. [Google Scholar] [CrossRef]
- Zelle, B.A.; Salazar, L.M.; Howard, S.L.; Parikh, K.; Pape, H.-C. Surgical Treatment Options for Femoral Neck Fractures in the Elderly. Int. Orthop. 2022, 46, 1111–1122. [Google Scholar] [CrossRef] [PubMed]
- Fischer, H.; Maleitzke, T.; Eder, C.; Ahmad, S.; Stöckle, U.; Braun, K.F. Management of Proximal Femur Fractures in the Elderly: Current Concepts and Treatment Options. Eur. J. Med. Res. 2021, 26, 86. [Google Scholar] [CrossRef]
- Xia, Y.; Zhang, W.; Zhang, Z.; Wang, J.; Yan, L. Treatment of Femoral Neck Fractures: Sliding Hip Screw or Cannulated Screws? A Meta-Analysis. J. Orthop. Surg. Res. 2021, 16, 54. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhao, X.; Yang, X.; Tang, X.; Liu, M. Dynamic Hip Screws versus Cannulated Screws for Femoral Neck Fractures: A Systematic Review and Meta-Analysis. J. Orthop. Surg. Res. 2020, 15, 352. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Chen, K.; Tian, K.; Li, W.; Mauffrey, C.; Hak, D.J. Medial Buttress Plate Augmentation of Cannulated Screw Fixation in Vertically Unstable Femoral Neck Fractures: Surgical Technique and Preliminary Results. Injury 2017, 48, 2189–2193. [Google Scholar] [CrossRef]
- Stoffel, K.; Zderic, I.; Gras, F.; Sommer, C.; Eberli, U.; Mueller, D.; Oswald, M.; Gueorguiev, B. Biomechanical Evaluation of the Femoral Neck System in Unstable Pauwels III Femoral Neck Fractures: A Comparison with the Dynamic Hip Screw and Cannulated Screws. J. Orthop. Trauma 2017, 31, 131–137. [Google Scholar] [CrossRef]
- Ballas, E.R.; Nguyen, V.T.; Wolin, E.A. Femoral Neck Fracture with Avascular Necrosis. J. Nucl. Med. Technol. 2023, 51, 78–79. [Google Scholar] [CrossRef]
- Konarski, W.; Poboży, T.; Kotela, A.; Śliwczyński, A.; Kotela, I.; Hordowicz, M.; Krakowiak, J. The Risk of Avascular Necrosis Following the Stabilization of Femoral Neck Fractures: A Systematic Review and Meta-Analysis. IJERPH 2022, 19, 10050. [Google Scholar] [CrossRef]
- Kawamura, T.; Minehara, H.; Tazawa, R.; Matsuura, T.; Sakai, R.; Takaso, M. Biomechanical Evaluation of Extramedullary Versus Intramedullary Reduction in Unstable Femoral Trochanteric Fractures. Geriatr Orthop. Surg. Rehabil. 2021, 12, 2151459321998611. [Google Scholar] [CrossRef]
- Cho, Y.; Shin, J.; Kim, S. Comparative Study for Osteosynthesis of Femoral Neck Fractures: Cannulated Screws versus Femoral Neck System. Hip Pelvis 2023, 35, 47. [Google Scholar] [CrossRef] [PubMed]
- Gupta, G.K.; Rai, A.; Mandal, S.; Rani, S.; Shekhar, S.; Halder, S.; Prasad, P.; Kumar, A.; Haque, Z.U. Comparison of Femoral Neck System Versus Cannulated Cancellous Screws for the Fixation of Femoral Neck Fracture in Young Adults: A Systematic Review and Meta-Analysis. Cureus 2022, 14, e32011. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Kumar, V.; Baburaj, V.; Dhillon, M.S. The Use of the Femoral Neck System (FNS) Leads to Better Outcomes in the Surgical Management of Femoral Neck Fractures in Adults Compared to Fixation with Cannulated Screws: A Systematic Review and Meta-Analysis. Eur. J. Orthop. Surg. Traumatol. 2022, 33, 2101–2109. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Chen, J.; Xing, F.; Liu, H.; Xiang, Z. Comparison of Femoral Neck System versus Cannulated Screws for Treatment of Femoral Neck Fractures: A Systematic Review and Meta-Analysis. BMC Musculoskelet. Disord. 2023, 24, 285. [Google Scholar] [CrossRef]
- Chen, Y.; Ren, D.; Yao, S.; Geng, L.; Su, Y.; Kang, B.; Wang, P. Accurate Placement of Cannulated Screws in Femoral Neck Fractures: Screw and Guide Wire Combined Technique. Orthop. Surg. 2021, 13, 2472–2476. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.-W.; Hsu, W.-H.; Peng, K.-T.; Lee, C.-Y. Effect of Integrity of the Posterior Cortex in Displaced Femoral Neck Fractures on Outcome after Surgical Fixation in Young Adults. Injury 2011, 42, 217–222. [Google Scholar] [CrossRef]
- Kalsbeek, J.H.; Van Donkelaar, M.F.; Krijnen, P.; Roerdink, W.H.; De Groot, R.; Schipper, I.B. What Makes Fixation of Femoral Neck Fractures Fail? A Systematic Review and Meta-Analysis of Risk Factors. Injury 2023, 54, 652–660. [Google Scholar] [CrossRef]
- Stenroos, A.; Brinck, T.; Handolin, L. Recommendation of Use of Checklists in Tibial Intramedullary Nail Removal: Retrospective Study of Mechanical Complications Related to Nail Removal. Injury 2018, 49, 1341–1347. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, A.-A.; Liu, J.-M.; Tong, W.-L.; Xiao, S.-N.; Liu, Z.-L. Effect of Screw Tunnels on Proximal Femur Strength after Screw Removal: A Finite Element Analysis. Orthop. Traumatol. Surg. Res. 2022, 108, 103408. [Google Scholar] [CrossRef]
- Medda, S.; Snoap, T.; Carroll, E.A. Treatment of Young Femoral Neck Fractures. J. Orthop. Trauma 2019, 33, S1–S6. [Google Scholar] [CrossRef]
- Papakostidis, C.; Panagiotopoulos, A.; Piccioli, A.; Giannoudis, P.V. Timing of Internal Fixation of Femoral Neck Fractures. A Systematic Review and Meta-Analysis of the Final Outcome. Injury 2015, 46, 459–466. [Google Scholar] [CrossRef]
- Gumustas, S.; Tosun, H.B.; Isyar, M.; Serbest, S.; Oznam, K.; Bulut, G. Femur Neck Fracture in Young Adults, Is It Really an Urgent Surgery Indication: Retrospective Clinical Study. Pan. Afr. Med. J. 2018, 30, 13643. [Google Scholar] [CrossRef]
- Langlois, J.; Vieira, T.D.; Ait Si Selmi, T.; Bonnin, M.P. A Simple CT Scan Protocol for Planning of Total Hip Arthroplasty in Patients with Femoral Neck Fractures. Orthop. Traumatol. Surg. Res. 2024, 110, 103943. [Google Scholar] [CrossRef]
- Bout, C.A.; Cannegieter, D.M.; Juttmann, J.W. Percutaneous Cannulated Screw Fixation of Femoral Neck Fractures: The Three Point Principle. Injury 1997, 28, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Druart, T.; Fréger, N.; Pries, P.; Losson, A.; Bouget, P.; Vendeuvre, T.; Severyns, M. Analysis of Risk Factors for Modification of Femoral Offset after Internal Fixation of Garden I and II Femoral Neck Fractures. Orthop. Traumatol. Surg. Res. 2024, 110, 103967. [Google Scholar] [CrossRef] [PubMed]
- Lei, K.; Li, D.; Ren, R.; Bai, J.; Qi, Y.; Zhang, X. Ideal Configuration Distribution of Femoral Neck Cannulated Screw in High Altitude Population: A Finite Element Study. BioMed Res. Int. 2022, 2022, 2085378. [Google Scholar] [CrossRef] [PubMed]
- Kwak, D.-K.; Lee, Y.; Lee, S.-J.; Lee, S.; Yoo, J.-H. What Is the Appropriate Axial Position in Cannulated Screw Fixation for Femoral Neck Fractures? A Finite Element Analysis. BMC Musculoskelet. Disord. 2025, 26, 430. [Google Scholar] [CrossRef]
- Sharma, G.; Gn, K.K.; Yadav, S.; Lakhotia, D.; Singh, R.; Gamanagatti, S.; Sharma, V. Pertrochanteric Fractures (AO/OTA 31-A1 and A2) Not Amenable to Closed Reduction: Causes of Irreducibility. Injury 2014, 45, 1950–1957. [Google Scholar] [CrossRef]
- Chen, H.-F.; Mi, J.; Zhang, H.-H.; Zhao, C.-Q. Pelvic Incidence Measurement Using a Computed Tomography Data-Based Three-Dimensional Pelvic Model. J. Orthop. Surg. Res. 2019, 14, 13. [Google Scholar] [CrossRef]
- Arık, A.; Yasin Hatipoğlu, M.; Özcanyüz, B.; Bulut, M.; Seyfettinoğlu, F. A Radiographic Study of Dorsovolar Wrist Axes and a Database of Angular Measurements on Axial Computed Tomography Images. Jt. Dis. Relat. Surg. 2023, 34, 176–182. [Google Scholar] [CrossRef]
- Alabousi, M.; Gauthier, I.D.; Li, N.; Dos Santos, G.M.; Golev, D.; Patlas, M.N.; Alabousi, A. Multi-Detector CT for Suspected Hip Fragility Fractures: A Diagnostic Test Accuracy Systematic Review and Meta-Analysis. Emerg. Radiol. 2019, 26, 549–556. [Google Scholar] [CrossRef]
- Kellock, T.T.; Khurana, B.; Mandell, J.C. Diagnostic Performance of CT for Occult Proximal Femoral Fractures: A Systematic Review and Meta-Analysis. Am. J. Roentgenol. 2019, 213, 1324–1330. [Google Scholar] [CrossRef]
- Liu, F.; Su, P.; Zhang, L.; Zhang, Y.; Zhu, J.; Zhang, R. Preoperative Computed Tomography Morphological Characteristics of Displaced Femoral Neck Fractures. Jt. Dis. Relat. Surg. 2023, 34, 253–264. [Google Scholar] [CrossRef] [PubMed]
- Kanthasamy, S.; To, K.; Webb, J.I.; Elbashir, M.; Parker, M.J. Timing of Surgery for Internal Fixation of Intracapsular Hip Fractures and Complications at 1 Year; a 32 Year Clinical Study of 2366 Patients at a Single Center. Injury 2022, 53, 584–589. [Google Scholar] [CrossRef]
- Farooq, M.A.; Orkazai, S.H.; Okusanya, O.; Devitt, A.T. Intracapsular Fractures of the Femoral Neck in Younger Patients. Ir. J. Med. Sci. 2005, 174, 42–45. [Google Scholar] [CrossRef]
- Brox, W.T.; Roberts, K.C.; Taksali, S.; Wright, D.G.; Wixted, J.J.; Tubb, C.C.; Patt, J.C.; Templeton, K.J.; Dickman, E.; Adler, R.A.; et al. The American Academy of Orthopaedic Surgeons Evidence-Based Guideline on Management of Hip Fractures in the Elderly. J. Bone Jt. Surg.-Am. Vol. 2015, 97, 1196–1199. [Google Scholar] [CrossRef]
- De Franco, S.; Ipponi, E.; Ruinato, A.D.; Parchi, P.D.; Andreani, L.; Scaglione, M.; Capanna, R. Femoral Neck Fractures Treated with Cannulated Screws: Can Surgeons Predict Functional Outcomes and Minimize the Risk of Necrosis? Acta Biomed. Atenei Parm. 2023, 94, e2023013. [Google Scholar] [CrossRef]
- Chang, C.-J.; Jou, I.-M.; Wu, T.-T.; Su, F.-C.; Tai, T.-W. Cigarette Smoke Inhalation Impairs Angiogenesis in Early Bone Healing Processes and Delays Fracture Union. Bone Jt. Res. 2020, 9, 99–107. [Google Scholar] [CrossRef] [PubMed]
- John Jebasingam Issace, S.; Singh Jagdeb Singh, R.; Sisubalasingam, N.; Ali Tokgöz, M.; Jaiman, A.; Rampal, S. Does Obesity Affect Diaphyseal Femoral Fracture Healing Treated with Intramedullary Locking Nail? Jt. Dis. Relat. Surg. 2023, 34, 9–15. [Google Scholar] [CrossRef]
- Jin, Z.; Chen, L.; Wang, D.; Ye, Y.; Fu, J.; Yang, Z.; He, B. A Prediction Model for Osteonecrosis of Femoral Head after Internal Fixation with Multiple Cannulated Compression Screws for Adult Femoral Neck Fractures. Jt. Dis. Relat. Surg. 2024, 35, 20–26. [Google Scholar] [CrossRef]
- Crump, E.K.; Quacinella, M.; Deafenbaugh, B.K. Does Screw Location Affect the Risk of Subtrochanteric Femur Fracture After Femoral Neck Fixation? A Biomechanical Study. Clin. Orthop. Relat. Res. 2020, 478, 770–776. [Google Scholar] [CrossRef]
- Mafirakureva, N.; Paruk, F.; Cassim, B.; Lukhele, M.; Gregson, C.L.; Noble, S.M. The Healthcare System Costs of Hip Fracture Care in South Africa. Osteoporos. Int. 2023, 34, 803–813. [Google Scholar] [CrossRef]
- Veronese, N.; Maggi, S. Epidemiology and Social Costs of Hip Fracture. Injury 2018, 49, 1458–1460. [Google Scholar] [CrossRef]
- Williamson, S.; Landeiro, F.; McConnell, T.; Fulford-Smith, L.; Javaid, M.K.; Judge, A.; Leal, J. Costs of Fragility Hip Fractures Globally: A Systematic Review and Meta-Regression Analysis. Osteoporos. Int. 2017, 28, 2791–2800. [Google Scholar] [CrossRef]
- Buchberger, B.; Scholl, K.; Krabbe, L.; Spiller, L.; Lux, B. Radiation Exposure by Medical X-Ray Applications. GMS Ger. Med. Sci. 2022, 20, Doc06. [Google Scholar] [CrossRef] [PubMed]
- Zamora, T.; Klaber, I.; Ananias, J.; Bengoa, F.; Botello, E.; Amenabar, P.; Schweitzer, D. The Influence of the CT Scan in the Evaluation and Treatment of Nondisplaced Femoral Neck Fractures in the Elderly. J. Orthop. Surg. 2019, 27, 2309499019836160. [Google Scholar] [CrossRef] [PubMed]
- Liodakis, E.; Pöhler, G.H.; Sonnow, L.; Mommsen, P.; Clausen, J.-D.; Graulich, T.; Maslaris, A.; Omar, M.; Stübig, T.; Sehmisch, S.; et al. Validation of Direct CT Measurement of Malrotation in Femoral Neck Fractures: A Bone Model Study. PLoS ONE 2023, 18, e0278850. [Google Scholar] [CrossRef] [PubMed]
- Moriarty, M.A.; Stefanov, D.G.; Cohn, R.M.; Brown, M.S.; Walz, D.M.; Walsh, P.J. Utility of Pelvis CT to Assess Occult Intertrochanteric Extension of Greater Trochanteric Fractures. J. Orthop. Trauma 2025, 39, 308–313. [Google Scholar] [CrossRef]
- Zhang, H.; Lv, J.; Xu, X.; Mei, J.; Liu, Y. Kinetic Analysis and Stability Evaluation of Femoral Neck Fracture with Internal Fixation Based on Gait Rehabilitation Training. Med. Eng. Phys. 2024, 131, 104222. [Google Scholar] [CrossRef]
- Gao, Y.; Zhong, F.; Zhan, X.; Bao, Y.; Zhu, X. Postoperative Rehabilitation Exercise Experiences of Geriatric Patients with Femoral Neck Fractures Based on the Perspective of Medical Staff: A Qualitative Study. BMC Geriatr. 2024, 24, 667. [Google Scholar] [CrossRef]


| Garden | Pauwels | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | Total | |||||
| n | % | n | % | n | % | n | % | |
| 1 | 3 | 5.45% | 2 | 3.64% | 1 | 1.82% | 6 | 10.91% |
| 2 | 6 | 10.91% | 10 | 18.18% | 9 | 16.36% | 25 | 45.45% |
| 3 | 2 | 3.64% | 15 | 27.27% | 5 | 9.09% | 22 | 40% |
| 4 | 0 | 0% | 0 | 0% | 2 | 3.64% | 2 | 3.64% |
| Total | 11 | 20% | 27 | 49.09% | 17 | 30.91% | 55 | 100% |
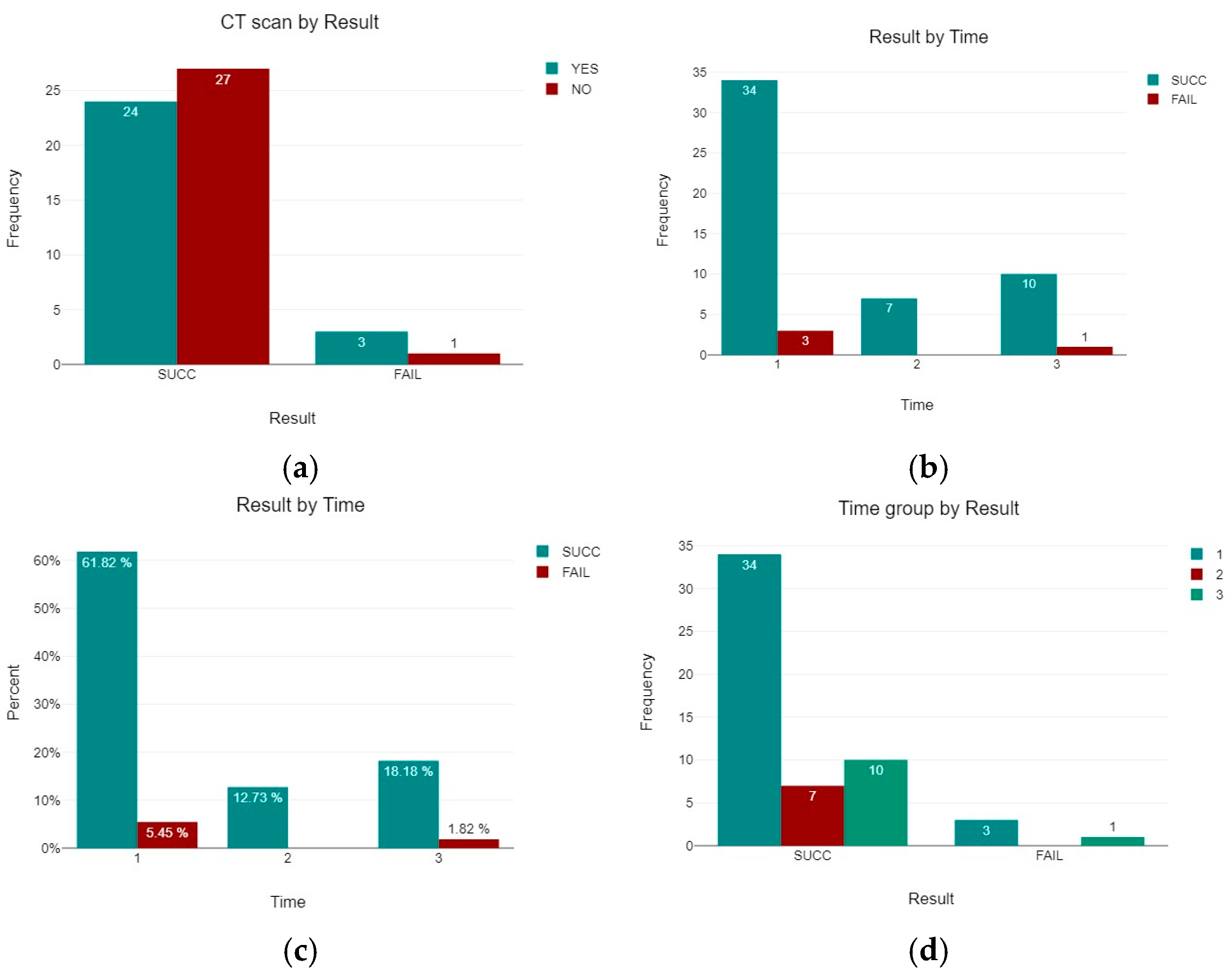
| CT Scan Group | Total (n) | Success (n) | Failure (n) | Failure Rate (%) | 95% CI |
|---|---|---|---|---|---|
| CT Performed | 27 | 24 | 3 | 11.1% | 3.9–28.1% |
| No CT | 28 | 27 | 1 | 3.6% | 0.6–17.7% |
| Total | 55 | 51 | 4 | 7.3% | 2.9–17.3% |
| Classification/Type | Group Delay 1 (<24 h) | Group Delay 2 (<48 h) | Group Delay 3 (>48 h) |
|---|---|---|---|
| Garden 1 | 2 | 0 | 3 |
| Garden 2 | 15 | 3 | 6 |
| Garden 3 | 17 | 3 | 1 |
| Garden 4 | 2 | 0 | 0 |
| Pauwels 1 | 6 | 1 | 3 |
| Pauwels 2 | 17 | 4 | 5 |
| Pauwels 3 | 13 | 1 | 2 |
| Result | Time Group | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 (≤24 h) | 2 (≤48 h) | 3 (>48 h) | Total | |||||||||||
| n | % | % Within Time Group | % Within Result | n | % | % Within Time Group | % Within Result | n | % | % Within Time Group | % Within Result | n | % | |
| SUCC | 34 | 61.82% | 91.89% | 66.67% | 7 | 12.73% | 100% | 13.73% | 10 | 18.18% | 90.91% | 19.61% | 51 | 92.73% |
| FAIL | 3 | 5.45% | 8.11% | 75% | 0 | 0% | 0% | 0% | 1 | 1.82% | 9.09% | 25% | 4 | 7.27% |
| Total | 37 | 67.27% | 100% | 7 | 12.73% | 100% | 11 | 20% | 100% | 55 | 100% | |||
| Garden | Result | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SUCC | FAIL | Total | ||||||||
| n | % | % Within Result | % Within Garden | n | % | % Within Result | % Within Garden | n | % | |
| 1 | 6 | 10.91% | 11.76% | 100% | 0 | 0% | 0% | 0% | 6 | 10.91% |
| 2 | 23 | 41.82% | 45.1% | 92% | 2 | 3.64% | 50% | 8% | 25 | 45.45% |
| 3 | 20 | 36.36% | 39.22% | 90.91% | 2 | 3.64% | 50% | 9.09% | 22 | 40% |
| 4 | 2 | 3.64% | 3.92% | 100% | 0 | 0% | 0% | 0% | 2 | 3.64% |
| Total | 51 | 92.73% | 100% | 4 | 7.27% | 100% | 55 | 100% | ||
| Pauwels | Result | |||||||||
| SUCC | FAIL | Total | ||||||||
| n | % | % within Result | % within Pauwels | n | % | % within Result | % within Pauwels | n | % | |
| 1 | 11 | 20% | 21.57% | 100% | 0 | 0% | 0% | 0% | 11 | 20% |
| 2 | 25 | 45.45% | 49.02% | 92.59% | 2 | 3.64% | 50% | 7.41% | 27 | 49.09% |
| 3 | 15 | 27.27% | 29.41% | 88.24% | 2 | 3.64% | 50% | 11.76% | 17 | 30.91% |
| Total | 51 | 92.73% | 100% | 4 | 7.27% | 100% | 55 | 100% | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucenti, L.; Sodano, A.; Panvini, F.M.C.; Vescio, A.; Papotto, G.; Testa, G.; Pavone, V. Does Preoperative CT Improve Outcomes in Femoral Neck Fracture Fixation? A Retrospective Study. J. Clin. Med. 2025, 14, 5917. https://doi.org/10.3390/jcm14165917
Lucenti L, Sodano A, Panvini FMC, Vescio A, Papotto G, Testa G, Pavone V. Does Preoperative CT Improve Outcomes in Femoral Neck Fracture Fixation? A Retrospective Study. Journal of Clinical Medicine. 2025; 14(16):5917. https://doi.org/10.3390/jcm14165917
Chicago/Turabian StyleLucenti, Ludovico, Andrea Sodano, Flora Maria Chiara Panvini, Andrea Vescio, Giacomo Papotto, Gianluca Testa, and Vito Pavone. 2025. "Does Preoperative CT Improve Outcomes in Femoral Neck Fracture Fixation? A Retrospective Study" Journal of Clinical Medicine 14, no. 16: 5917. https://doi.org/10.3390/jcm14165917
APA StyleLucenti, L., Sodano, A., Panvini, F. M. C., Vescio, A., Papotto, G., Testa, G., & Pavone, V. (2025). Does Preoperative CT Improve Outcomes in Femoral Neck Fracture Fixation? A Retrospective Study. Journal of Clinical Medicine, 14(16), 5917. https://doi.org/10.3390/jcm14165917







