High-Quality Targeted Temperature Management After Cardiac Arrest; Results from the Korean Hypothermia Network Prospective Registry
Abstract
1. Introduction
2. Materials and Methods
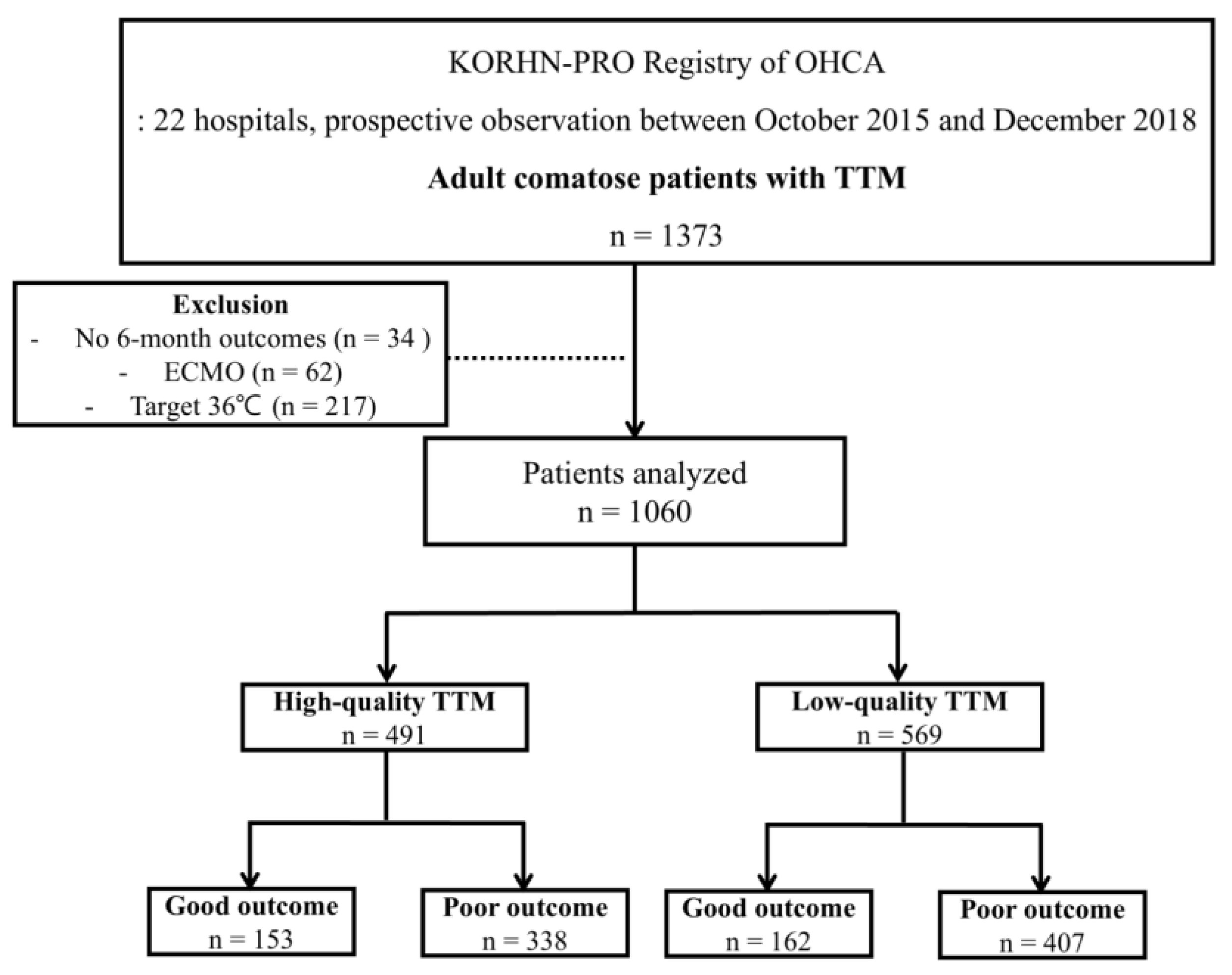
2.1. Study Design and Participants
2.2. Data Collection
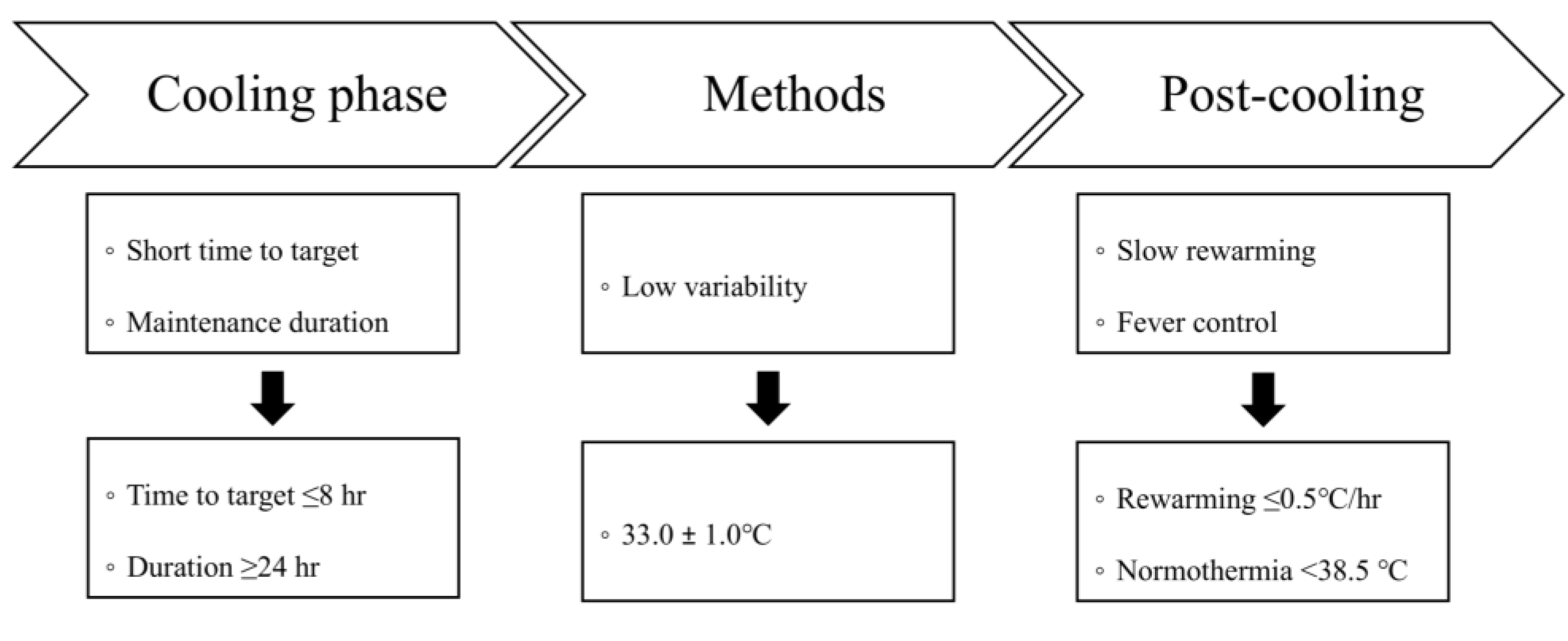
2.3. Definition of High-Quality TTM
2.4. Outcome Measures
2.5. Statistical Analysis
3. Results
3.1. Patients
3.2. Quality of TTM According to Neurological Outcomes
3.3. Quality of TTM and Clinical Outcome
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Laver, S.; Farrow, C.; Turner, D.; Nolan, J. Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Med. 2004, 30, 2126–2128. [Google Scholar] [CrossRef]
- Lemiale, V.; Dumas, F.; Mongardon, N.; Giovanetti, O.; Charpentier, J.; Chiche, J.D.; Carli, P.; Mira, J.P.; Nolan, J.; Cariou, A. Intensive care unit mortality after cardiac arrest: The relative contribution of shock and brain injury in a large cohort. Intensive Care Med. 2013, 39, 1972–1980. [Google Scholar] [CrossRef] [PubMed]
- Panchal, A.R.; Bartos, J.A.; Cabanas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S366–S468. [Google Scholar] [CrossRef] [PubMed]
- Nolan, J.P.; Sandroni, C.; Böttiger, B.W.; Cariou, A.; Cronberg, T.; Friberg, H.; Genbrugge, C.; Haywood, K.; Lilja, G.; Moulaert, V.R.M.; et al. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines 2021: Post-resuscitation Care. Intensive Care Med. 2021, 47, 369–421. [Google Scholar] [CrossRef] [PubMed]
- Holmberg, M.J.; Nicholson, T.; Nolan, J.P.; Schexnayder, S.; Reynolds, J.; Nation, K.; Welsford, M.; Morley, P.; Soar, J.; Berg, K.M.; et al. Oxygenation and ventilation targets after cardiac arrest: A systematic review and meta-analysis. Resuscitation 2020, 152, 107–115. [Google Scholar] [CrossRef]
- Roberts, B.W.; Kilgannon, J.H.; Chansky, M.E.; Mittal, N.; Wooden, J.; Trzeciak, S. Association between postresuscitation partial pressure of arterial carbon dioxide and neurological outcome in patients with post-cardiac arrest syndrome. Circulation 2013, 127, 2107–2113. [Google Scholar] [CrossRef]
- Miao, B.J.M.; Skaar, J.R.; O’Hara, M.; Post, A.; Kelly, T.; Abella, B.S. A Systematic Literature Review to Assess Fever Management and the Quality of Targeted Temperature Management in Critically Ill Patients. Ther. Hypothermia Temp. Manag. 2024, 14, 68–79. [Google Scholar] [CrossRef]
- Taccone, F.S.; Picetti, E.; Vincent, J.L. High-Quality Targeted Temperature Management (TTM) after Cardiac Arrest. Crit. Care 2020, 24, 6. [Google Scholar] [CrossRef]
- Kim, S.H.; Park, K.N.; Youn, C.S.; Chae, M.K.; Kim, W.Y.; Lee, B.K.; Lee, D.H.; Jang, T.C.; Lee, J.H.; Choi, Y.H.; et al. Outcome and status of postcardiac arrest care in Korea: Results from the Korean Hypothermia Network prospective registry. Clin. Exp. Emerg. Med. 2020, 7, 250–258. [Google Scholar] [CrossRef]
- Zeiner, A.; Holzer, M.; Sterz, F.; Schörkhuber, W.; Eisenburger, P.; Havel, C.; Kliegel, A.; Laggner, A.N. Hyperthermia after cardiac arrest is associated with an unfavorable neurologic outcome. Arch. Intern. Med. 2001, 161, 2007–2012. [Google Scholar] [CrossRef]
- Yamashita, S.; Hifumi, T.; Kawakita, K.; Inoue, A.; Egawa, S.; Shindo, A.; Kawanishi, M.; Yagi, T.; Kuroda, Y. Clinical Effect of Rebound Hyperthermia After Cooling Postcardiac Arrest: A Meta-Analysis. Ther. Hypothermia Temp. Manag. 2017, 7, 206–209. [Google Scholar] [CrossRef]
- Leary, M.; Grossestreuer, A.V.; Iannacone, S.; Gonzalez, M.; Shofer, F.S.; Povey, C.; Wendell, G.; Archer, S.E.; Gaieski, D.F.; Abella, B.S.; et al. Pyrexia and neurologic outcomes after therapeutic hypothermia for cardiac arrest. Resuscitation 2013, 84, 1056–1061. [Google Scholar] [CrossRef]
- Nielsen, N.; Sunde, K.; Hovdenes, J.; Riker, R.R.; Rubertsson, S.; Stammet, P.; Nilsson, F.; Friberg, H.; Network, H. Adverse events and their relation to mortality in out-of-hospital cardiac arrest patients treated with therapeutic hypothermia. Crit. Care Med. 2011, 39, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Oddo, M.; Schaller, M.D.; Feihl, F.; Ribordy, V.; Liaudet, L. From evidence to clinical practice: Effective implementation of therapeutic hypothermia to improve patient outcome after cardiac arrest. Crit. Care Med. 2006, 34, 1865–1873. [Google Scholar] [CrossRef] [PubMed]
- Haugk, M.; Testori, C.; Sterz, F.; Uranitsch, M.; Holzer, M.; Behringer, W.; Herkner, H.; The Time to Target Temperature Study Group. Relationship between time to target temperature and outcome in patients treated with therapeutic hypothermia after cardiac arrest. Crit Care 2011, 15, R101. [Google Scholar] [CrossRef] [PubMed]
- Perman, S.M.; Ellenberg, J.H.; Grossestreuer, A.V.; Gaieski, D.F.; Leary, M.; Abella, B.S.; Carr, B.G. Shorter time to target temperature is associated with poor neurologic outcome in post-arrest patients treated with targeted temperature management. Resuscitation 2015, 88, 114–119. [Google Scholar] [CrossRef]
- Nishimura, T.; Hatakeyama, T.; Yoshida, H.; Yoshimura, S.; Kiguchi, T.; Irisawa, T.; Yamada, T.; Yoshiya, K.; Park, C.; Ishibe, T.; et al. Non-linear Association Between the Time Required to Reaching Temperature Targets and the Neurological Outcome in Patients Undergoing Targeted Temperature Management After Out-of-Hospital Cardiac Arrest: Observational Multicentre Cohort Study. Resusc. Plus 2024, 18, 100607. [Google Scholar] [CrossRef]
- Abella, B.S.; Zhao, D.H.; Alvarado, J.; Hamann, K.; Vanden Hoek, T.L.; Becker, L.B. Intra-arrest cooling improves outcomes in a murine cardiac arrest model. Circulation 2004, 109, 2786–2791. [Google Scholar] [CrossRef]
- Che, D.F.; Li, L.C.; Kopil, C.M.; Liu, Z.Y.; Guo, W.S.; Neumar, R.W. Impact of therapeutic hypothermia onset and duration on survival, neurologic function, and neurodegeneration after cardiac arrest. Crit. Care Med. 2011, 39, 1423–1430. [Google Scholar] [CrossRef]
- Castrén, M.; Nordberg, P.; Svensson, L.; Taccone, F.; Vincent, J.L.; Desruelles, D.; Eichwede, F.; Mols, P.; Schwab, T.; Vergnion, M.; et al. Intra-Arrest Transnasal Evaporative Cooling a Randomized, Prehospital, Multicenter Study (PRINCE: Pre-ROSC IntraNasal Cooling Effectiveness). Circulation 2010, 122, 729–736. [Google Scholar] [CrossRef]
- Nordberg, P.; Taccone, F.S.; Truhlar, A.; Forsberg, S.; Hollenberg, J.; Jonsson, M.; Cuny, J.; Goldstein, P.; Vermeersch, N.; Higuet, A.; et al. Effect of Trans-Nasal Evaporative Intra-arrest Cooling on Functional Neurologic Outcome in Out-of-Hospital Cardiac Arrest: The PRINCESS Randomized Clinical Trial. JAMA-J. Am. Med. Assoc. 2019, 321, 1677–1685. [Google Scholar] [CrossRef]
- De Fazio, C.; Skrifvars, M.B.; Soreide, E.; Grejs, A.M.; Di Bernardini, E.; Jeppesen, A.N.; Storm, C.; Kjaergaard, J.; Laitio, T.; Rasmussen, B.S.; et al. Quality of targeted temperature management and outcome of out-of-hospital cardiac arrest patients: A analysis of the TTH48 study. Resuscitation 2021, 165, 85–92. [Google Scholar] [CrossRef]
- Bradley, S.M.; Liu, W.H.; McNally, B.; Vellano, K.; Henry, T.D.; Mooney, M.R.; Burke, M.N.; Brilakis, E.S.; Grunwald, G.K.; Adhaduk, M.; et al. Temporal Trends in the Use of Therapeutic Hypothermia for Out-of-Hospital Cardiac Arrest. JAMA Netw. Open 2018, 1, e184511. [Google Scholar] [CrossRef]
- Greif, R.; Bray, J.E.; Djärv, T.; Drennan, I.R.; Liley, H.G.; Ng, K.C.; Cheng, A.; Douma, M.J.; Scholefield, B.R.; Smyth, M.; et al. 2024 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation 2024, 150, E580–E687. [Google Scholar] [CrossRef] [PubMed]
- Nayeri, A.; Bhatia, N.; Holmes, B.; Borges, N.; Armstrong, W.; Xu, M.; Farber-Eger, E.; Wells, Q.S.; McPherson, J.A. Temperature variability during targeted temperature management is not associated with neurological outcomes following cardiac arrest. Am. J. Emerg. Med. 2017, 35, 889–892. [Google Scholar] [CrossRef] [PubMed]
- Cordoza, M.; Thompson, H.; Bridges, E.; Burr, R.; Carlbom, D. Association Between Target Temperature Variability and Neurologic Outcomes for Patients Receiving Targeted Temperature Management at 36 °C After Cardiac Arrest: A Retrospective Cohort Study. Ther. Hypothermia Temp. Manag. 2021, 11, 103–109. [Google Scholar] [CrossRef]
- Hifumi, T.; Inoue, A.; Kokubu, N.; Hase, M.; Yonemoto, N.; Kuroda, Y.; Kawakita, K.; Sawano, H.; Tahara, Y.; Nishioka, K.; et al. Association between rewarming duration and neurological outcome in out-of-hospital cardiac arrest patients receiving therapeutic hypothermia. Resuscitation 2020, 146, 170–177. [Google Scholar] [CrossRef]
- Hassager, C.; Schmidt, H.; Moller, J.E.; Grand, J.; Molstrom, S.; Beske, R.P.; Boesgaard, S.; Borregaard, B.; Bekker-Jensen, D.; Dahl, J.S.; et al. Duration of Device-Based Fever Prevention after Cardiac Arrest. N. Engl. J. Med. 2023, 388, 888–897. [Google Scholar] [CrossRef]
- Kirkegaard, H.; Soreide, E.; de Haas, I.; Pettilä, V.; Taccone, F.S.; Arus, U.; Storm, C.; Hassager, C.; Nielsen, J.F.; Sorensen, C.A.; et al. Targeted Temperature Management for 48 vs 24 Hours and Neurologic Outcome After Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA-J. Am. Med. Assoc. 2017, 318, 341–350. [Google Scholar] [CrossRef]
- Uminska, J.M.; Buszko, K.; Ratajczak, J.; Lach, P.; Pstragowski, K.; Dabrowska, A.; Adamski, P.; Skonieczny, G.; Manitius, J.; Kubica, J. Comparison of temperature measurements in esophagus and urinary bladder in comatose patients after cardiac arrest undergoing mild therapeutic hypothermia. Cardiol. J. 2020, 27, 735–741. [Google Scholar] [CrossRef] [PubMed]
- Markota, A.; Palfy, M.; Stozer, A.; Sinkovic, A. Difference Between Bladder and Esophageal Temperatures in Mild Induced Hypothermia. J. Emerg. Med. 2015, 49, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Lefrant, J.Y.; Muller, L.; de La Coussaye, J.E.; Benbabaali, M.; Lebris, C.; Zeitoun, N.; Mari, C.; Saissi, G.; Ripart, J.; Eledjam, J.J. Temperature measurement in intensive care patients: Comparison of urinary bladder, oesophageal, rectal, axillary, and inguinal methods versus pulmonary artery core method. Intensive Care Med. 2003, 29, 414–418. [Google Scholar] [CrossRef] [PubMed]
| Total (N = 1060) | High-Quality TTM (N = 491) | Low-Quality TTM (N = 569) | p-Value | |
|---|---|---|---|---|
| Male (n) | 751 (10.8%) | 334 (68.0%) | 417 (73.3%) | 0.060 |
| Age (year, IQRs) | 58.0 (47.0–69.0) | 59.0 (48.0–69.0) | 57.0 (46.0–68.0) | 0.937 |
| BMI (kg/m2, IQRs) | 23.4 (21.0–25.7) | 23.1 (20.8–25.8) | 23.7 (21.5–25.9) | 0.267 |
| Comorbidity (n) | ||||
| History of CAD | 125 (11.8%) | 54 (11.0%) | 71 (12.5%) | 0.456 |
| History of CVA | 58 (5.5%) | 30 (6.1%) | 28 (4.9%) | 0.396 |
| History of HTN | 389 (36.7%) | 187 (38.1%) | 202 (35.5%) | 0.384 |
| History of DM | 269 (25.4%) | 137 (27.9%) | 132 (23.2%) | 0.079 |
| Cardiac arrest at public place (n) | 500 (47.2%) | 244 (49.7%) | 256 (45.0%) | 0.126 |
| Witnessed arrest (n) | 755 (71.2%) | 348 (70.9%) | 407 (71.5%) | 0.815 |
| Bystander CPR (n) | 645 (60.8%) | 311 (68.3%) | 334 (58.7%) | 0.123 |
| Shockable initial rhythm (n) | 355 (33.5%) | 156 (31.8%) | 199 (35.0%) | 0.271 |
| Total anoxic time (min, IQRs) | 25.0 (15.0–38.0) | 25.0 (15.0–38.0) | 25.0 (15.0–38.0) | 0.522 |
| Cardiac etiology (n) | 654 (61.7%) | 294 (59.9%) | 360 (63.3%) | 0.257 |
| Core temperature measurement (n) | 1040 (98.1%) | 487 (99.2%) | 553 (97.2%) | 0.017 |
| Temperature feedback method (n) | 1058 (99.8%) | 490 (99.8%) | 568 (99.8%) | 0.917 |
| Induction time to target temperature ≤ 8 h (n) | 719 (67.8%) | 344 (70.1%) | 375 (65.9%) | 0.149 |
| Induction time to target temperature (h, IQRs) | 2.0 (1.0–4.0) | 2.0 (1.0–3.0) | 3.0 (1.0–5.0) | 0.004 |
| Maintaining time ≥ 24 h (n) | 789 (79.9%) | 491 (100%) | 298 (60.0%) | <0.001 |
| Maintaining time (h, IQRs) | 28.0 (26.0–30.0) | 28.0 (27.0–29.0) | 27.0 (21.0–30.0) | <0.001 |
| Variability during TTM ± 1.0 °C (n) | 718 (72.5%) | 491 (100%) | 227 (45.4%) | <0.001 |
| Variability during TTM (°C, IQRs) | 1.4 (1.1–1.8) | 1.2 (1.0–1.4) | 1.5 (0.8–2.1) | <0.001 |
| Rewarming rate ≤ 0.5 °C/h (n) | 873 (82.4%) | 491 (100%) | 382 (67.1%) | <0.001 |
| Rewarming rate (°C/h, IQRs) | 0.25 (0.21–0.30) | 0.25 (0.21–0.27) | 0.26 (0.20–0.33) | <0.001 |
| Post-rewarming fever control < 38.5 °C (n) | 822 (77.5%) | 491 (100%) | 331 (58.2%) | <0.001 |
| Survival at 6 months (n) | 426 (40.2%) | 219 (44.6%) | 207 (36.4%) | 0.006 |
| Good outcome at 6 months (n) | 315 (29.7%) | 153 (31.2%) | 162 (28.5%) | 0.339 |
| Good Outcome (N = 315) | Poor Outcome (N = 745) | p-Value | |
|---|---|---|---|
| Core temperature measurement (n) | 309 (98.1%) | 731 (98.1%) | 0.978 |
| Temperature feedback method (n) | 315 (100%) | 743 (99.7%) | 0.357 |
| Induction time to target temperature ≤ 8 h (n) | 162 (51.4%) | 557 (74.8%) | <0.001 |
| Induction time to target temperature (h, IQRs) | 3.0 (2.0–5.3) | 2.0 (1.0–3.0) | <0.001 |
| Maintaining time ≥ 24 h (n) | 250 (82.8%) | 539 (78.6%) | 0.128 |
| Maintaining time (h, IQRs) | 28.0 (26.0–29.3) | 28.0 (26.0–30.0) | 0.324 |
| Variability during TTM ± 1.0 °C (n) | 218 (72.2%) | 500 (72.6%) | 0.901 |
| Variability during TTM (°C, IQRs) | 1.4 (1.1–1.7) | 1.3 (1.1–1.8) | 0.064 |
| Rewarming rate ≤ 0.5 °C/h (n) | 281 (89.2%) | 592 (79.5%) | <0.001 |
| Rewarming rate (°C/h, IQRs) | 0.26 (0.22–0.33) | 0.25 (0.20–0.29) | <0.001 |
| Post-rewarming fever control (<38.5 °C, n) | 256 (82.1%) | 566 (89.6%) | 0.001 |
| Survival | Good Outcome | |||||
|---|---|---|---|---|---|---|
| OR | 95% C.I. | p-Value | OR | 95% C.I. | p-Value | |
| Male Sex | 1.394 | 1.058–1.836 | 0.018 | 1.575 | 1.161–2.136 | 0.004 |
| Age | 1.026 | 1.017–1.034 | <0.001 | 1.035 | 1.026–1.044 | <0.001 |
| BMI | 0.995 | 0.965–1.025 | 0.730 | 0.997 | 0.966–1.030 | 0.871 |
| History of CAD | 1.194 | 0.820–1.741 | 0.355 | 1.385 | 0.936–2.050 | 0.103 |
| History of CVA | 0.977 | 0.569–1.678 | 0.932 | 0.896 | 0.496–1.618 | 0.715 |
| History of HTN | 0.625 | 0.482–0.811 | <0.001 | 0.597 | 0.449–0.793 | <0.001 |
| History of DM | 0.508 | 0.377–0.685 | <0.001 | 0.453 | 0.322–0.637 | <0.001 |
| Cardiac arrest at public place | 1.633 | 1.275–2.092 | <0.001 | 1.586 | 1.217–2.068 | <0.001 |
| Witnessed arrest | 3.068 | 2.264–4.158 | <0.001 | 3.321 | 2.335–4.724 | <0.001 |
| Bystander CPR | 1.299 | 1.008–1.675 | 0.043 | 1.37 | 1.041–1.804 | 0.025 |
| Shockable initial rhythm | 7.793 | 5.845–10.390 | <0.001 | 15.299 | 11.108–21.073 | <0.001 |
| Total anoxic time | 1.045 | 1.036–1.055 | <0.001 | 1.056 | 1.044–1.067 | <0.001 |
| Cardiac etiology | 3.946 | 2.975–5.233 | <0.001 | 7.647 | 5.252–11.133 | <0.001 |
| Induction time to target temperature | 0.820 | 0.778–0.865 | <0.001 | 0.814 | 0.773–0.858 | <0.001 |
| Maintaining time | 1.610 | 1.160–2.235 | 0.004 | 1.311 | 0.924–1.861 | 0.129 |
| Variability during TTM | 1.146 | 0.862–1.523 | 0.349 | 0.981 | 0.725–1.327 | 0.901 |
| Rewarming rate | 3.258 | 2.220–4.782 | <0.001 | 2.136 | 1.435–3.180 | <0.001 |
| Post-rewarming fever control | 0.518 | 0.352–0.762 | <0.001 | 0.533 | 0.363–0.784 | 0.001 |
| High-quality TTM | 1.408 | 1.100–1.802 | 0.007 | 1.137 | 0.873–1.481 | 0.339 |
| Survival | Good Outcome | |||||
|---|---|---|---|---|---|---|
| OR | 95% C.I. | p-Value | OR | 95% C.I. | p-Value | |
| High-quality TTM | 1.802 | 1.171–2.773 | 0.007 | 1.748 | 1.102–2.770 | 0.018 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bang, H.J.; Youn, C.S.; Lee, B.K.; Oh, S.H.; Kim, H.J.; Gong, A.K.; Lee, J.-S.; Kim, S.H.; Park, K.N.; Cho, I.S.; et al. High-Quality Targeted Temperature Management After Cardiac Arrest; Results from the Korean Hypothermia Network Prospective Registry. J. Clin. Med. 2025, 14, 5898. https://doi.org/10.3390/jcm14165898
Bang HJ, Youn CS, Lee BK, Oh SH, Kim HJ, Gong AK, Lee J-S, Kim SH, Park KN, Cho IS, et al. High-Quality Targeted Temperature Management After Cardiac Arrest; Results from the Korean Hypothermia Network Prospective Registry. Journal of Clinical Medicine. 2025; 14(16):5898. https://doi.org/10.3390/jcm14165898
Chicago/Turabian StyleBang, Hyo Jin, Chun Song Youn, Byung Kook Lee, Sang Hoon Oh, Hyo Joon Kim, Ae Kyung Gong, Ji-Sook Lee, Soo Hyun Kim, Kyu Nam Park, In Soo Cho, and et al. 2025. "High-Quality Targeted Temperature Management After Cardiac Arrest; Results from the Korean Hypothermia Network Prospective Registry" Journal of Clinical Medicine 14, no. 16: 5898. https://doi.org/10.3390/jcm14165898
APA StyleBang, H. J., Youn, C. S., Lee, B. K., Oh, S. H., Kim, H. J., Gong, A. K., Lee, J.-S., Kim, S. H., Park, K. N., Cho, I. S., & on behalf of the Korean Hypothermia Network Investigators. (2025). High-Quality Targeted Temperature Management After Cardiac Arrest; Results from the Korean Hypothermia Network Prospective Registry. Journal of Clinical Medicine, 14(16), 5898. https://doi.org/10.3390/jcm14165898






