Antenatal Maternal Hemoglobin Level and Severe Maternal Morbidity
Abstract
1. Introduction
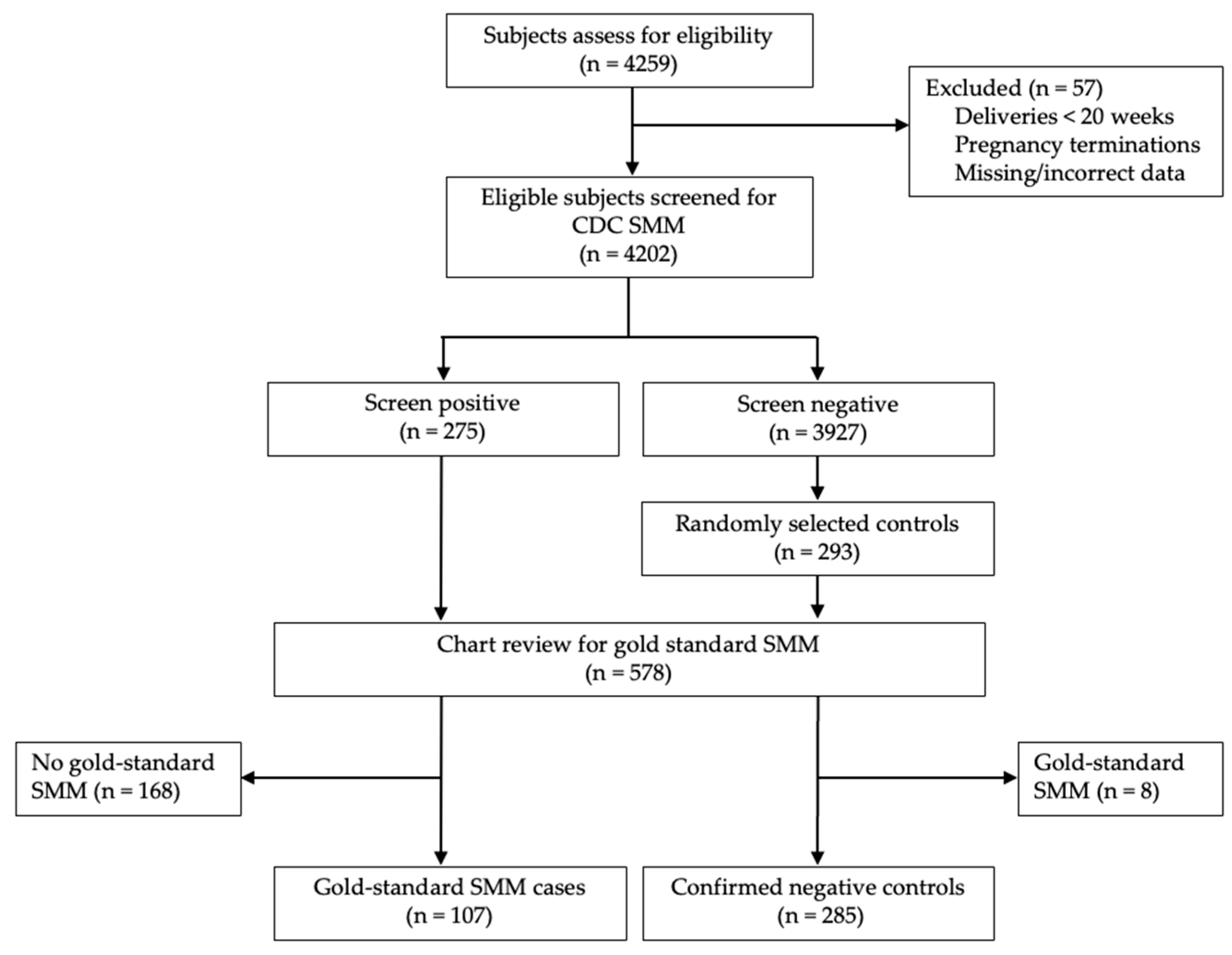
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CDC | Centers for Disease Control and Prevention |
| CI | Confidence interval |
| CMQCC | California Maternal Quality Care Collaborative |
| ICD10 | International Classification of Diseases, Tenth Revision, Clinical Modification |
| OR | Odds ratio |
| RBC | Red blood cell |
| SMM | Severe maternal morbidity |
Appendix A
| CDC SMM Indicators [8] | Gold-Standard SMM Indicators from Main et al. [6] |
|---|---|
| Acute myocardial infarction | Acute myocardial infarction |
| Aneurysm | Aneurysm |
| Acute renal failure | Acute renal failure
|
| Adult respiratory distress syndrome | Adult respiratory distress syndrome
|
| Amniotic fluid embolism | Amniotic fluid embolism |
| Cardiac arrest/ventricular fibrillation | Cardiac arrest/ventricular fibrillation |
| Conversion of cardiac rhythm | Conversion of cardiac rhythm
|
| Disseminated intravascular coagulation | Disseminated intravascular coagulation |
| Eclampsia | Eclampsia and severe pre-eclampsia
|
| Heart failure/arrest during surgery or procedure | Heart failure/arrest during surgery or procedure
|
| Puerperal cerebrovascular disorders | Puerperal cerebrovascular disorders |
| Pulmonary edema/acute heart failure | Pulmonary edema/acute heart failure |
| Severe anesthesia complications | Severe anesthesia complications
|
| Sepsis | Sepsis
|
| Shock | Shock |
| Sickle cell disease with crisis | Sickle cell disease with crisis |
| Air and thrombotic embolism | Air and thrombotic embolism |
| Blood product transfusion | Blood product transfusion
|
| Hysterectomy | Hysterectomy and surgical complications
|
| Temporary tracheostomy | Temporary tracheostomy |
| Ventilation | Ventilation (other than ventilation for a surgical procedure) |
References
- Harrison, R.K.; Lauhon, S.R.; Colvin, Z.A.; McIntosh, J.J. Maternal anemia and severe maternal morbidity in a US cohort. Am. J. Obstet. Gynecol. MFM 2021, 3, 100395. [Google Scholar] [CrossRef]
- Ray, J.G.; Davidson, A.; Berger, H.; Dayan, N.; Park, A.L. Haemoglobin levels in early pregnancy and severe maternal morbidity: Population-based cohort study. BJOG Int. J. Obstet. Gynaecol. 2020, 127, 1154–1164. [Google Scholar] [CrossRef]
- Nyarko, S.H.; Greenberg, L.T.; Saade, G.R.; Phibbs, C.S.; Buzas, J.S.; Lorch, S.A.; Rogowski, J.; Passarella, M.; Boghossian, N.S. Association between iron deficiency anemia and severe maternal morbidity: A retrospective cohort study. Ann. Epidemiol. 2024, 100, 10–15. [Google Scholar] [CrossRef]
- Beckert, R.H.; Baer, R.J.; Anderson, J.G.; Jelliffe-Pawlowski, L.L.; Rogers, E.E. Maternal anemia and pregnancy outcomes: A population-based study. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2019, 39, 911–919. [Google Scholar] [CrossRef]
- Guignard, J.; Deneux-Tharaux, C.; Seco, A.; Beucher, G.; Kayem, G.; Bonnet, M.P.; EPIMOMS Group. Gestational anaemia and severe acute maternal morbidity: A population-based study. Anaesthesia 2021, 76, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Main, E.K.; Abreo, A.; McNulty, J.; Gilbert, W.; McNally, C.; Poeltler, D.; Lanner-Cusin, K.; Fenton, D.; Gipps, T.; Melsop, K.; et al. Measuring severe maternal morbidity: Validation of potential measures. Am. J. Obstet. Gynecol. 2016, 214, 643.e1–643.e10. [Google Scholar] [CrossRef] [PubMed]
- Fabricant, S.P.; Opara, K.N.; Paul, J.V.; Blissett, G.; Rau, A.R.; White, J.D.; Girma, A.; Sriprasert, I.; Korst, L.M.; Mitchell, E.N. The Positive Predictive Value of Hospital Discharge Data for Identifying Severe Maternal Morbidity With and Without Blood Transfusion. Jt. Comm. J. Qual. Patient Saf. 2023, 49, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. How Does CDC Identify Severe Maternal Morbidity? 26 December 2019. Available online: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/smm/severe-morbidity-ICD.htm (accessed on 7 September 2021).
- Snowden, J.M.; Lyndon, A.; Kan, P.; El Ayadi, A.; Main, E.; Carmichael, S.L. Severe Maternal Morbidity: A Comparison of Definitions and Data Sources. Am. J. Epidemiol. 2021, 190, 1890–1897. [Google Scholar] [CrossRef]
- World Health Organization. Prevalence of Anaemia in Pregnant Women (aged 15–49) (%). 2021. Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/4552 (accessed on 7 September 2021).
- California Maternal Quality Care Collaborative. Maternal Data Center. 2021. Available online: https://www.cmqcc.org/maternal-data-center (accessed on 5 December 2021).
- Fridman, M.; Korst, L.M.; Reynen, D.J.; Nicholas, L.A.; Greene, N.; Saeb, S.; Troyan, J.L.; Gregory, K.D. Severe Maternal Morbidity in California Hospitals: Performance Based on a Validated Multivariable Prediction Model. Jt. Comm. J. Qual. Patient Saf. 2021, 47, 686–695. [Google Scholar] [CrossRef]
- World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. 2011. Available online: https://www.who.int/publications/i/item/WHO-NMH-NHD-MNM-11.1 (accessed on 7 September 2021).
- Galloway, R. Anemia Prevention and Control: What Works. USAID, World Bank, PAHO/WHO, Micronutrient Initiative, FAO, and UNICEF. 2003. Available online: https://documents1.worldbank.org/curated/en/234691468160187223/pdf/561740WP0v20Bo1PUBLIC10anemia1Part2.pdf (accessed on 7 September 2021).
- Korst, L.M.; Gregory, K.D.; Nicholas, L.A.; Saeb, S.; Reynen, D.J.; Troyan, J.L.; Greene, N.; Fridman, M. A scoping review of severe maternal morbidity: Describing risk factors and methodological approaches to inform population-based surveillance. Matern. Health Neonatol. Perinatol. 2021, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Howell, E.A. Reducing disparities in severe maternal morbidity and mortality. Clin. Obstet. Gynecol. 2018, 61, 387–399. [Google Scholar] [CrossRef] [PubMed]
- Anemia in Pregnancy: Practice Bulletin, Number 233. Obstet. Gynecol. 2021, 138, e55–e64. [CrossRef] [PubMed]
- Cresswell, J.A.; Alexander, M.; Chong, M.Y.C.; Link, H.M.; Pejchinovska, M.; Gazeley, U.; Ahmed, S.M.A.; Chou, D.; Moller, A.B.; Simpson, D.; et al. Global and regional causes of maternal deaths 2009-20: A WHO systematic analysis. Lancet. Glob. Health 2025, 13, e626–e634. [Google Scholar] [CrossRef]
- Silver, H.M.; Seebeck, M.; Carlson, R. Comparison of total blood volume in normal, preeclamptic, and nonproteinuric gestational hypertensive pregnancy by simultaneous measurement of red blood cell and plasma volumes. Am. J. Obstet. Gynecol. 1998, 179, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.; Teng, F.; Branch, E.; Chu, S.; Joseph, K.S. Maternal and Perinatal Morbidity and Mortality Associated With Anemia in Pregnancy. Obstet. Gynecol. 2019, 134, 1234–1244. [Google Scholar] [CrossRef]
- Surbek, D.; Vial, Y.; Girard, T.; Breymann, C.; Bencaiova, G.A.; Baud, D.; Hornung, R.; Taleghani, B.M.; Hösli, I. Patient blood management (PBM) in pregnancy and childbirth: Literature review and expert opinion. Arch. Gynecol. Obstet. 2020, 301, 627–641. [Google Scholar] [CrossRef]
- Zhang, J.; Li, Q.; Song, Y.; Fang, L.; Huang, L.; Sun, Y. Nutritional factors for anemia in pregnancy: A systematic review with meta-analysis. Front. Public Health 2022, 10, 1041136. [Google Scholar] [CrossRef]
- Jung, J.; Rahman, M.M.; Rahman, M.S.; Swe, K.T.; Islam, M.R.; Rahman, M.O.; Akter, S. Effects of hemoglobin levels during pregnancy on adverse maternal and infant outcomes: A systematic review and meta-analysis. Ann. N. Y. Acad. Sci. 2019, 1450, 69–82. [Google Scholar] [CrossRef]
- Ge, S.; Ali, S.; Haldane, V.; Bekdache, C.; Tang, G.H.; Sholzberg, M. An approach to Hemequity: Identifying the barriers and facilitators of iron deficiency reduction strategies in low- to middle-income countries. Br. J. Haematol. 2025, 206, 428–442. [Google Scholar] [CrossRef]
- Society for Maternal-Fetal Medicine (SMFM); Lappen, J.R.; Pettker, C.M.; Louis, J.M. Society for Maternal-Fetal Medicine Consult Series #54: Assessing the risk of maternal morbidity and mortality. Am. J. Obstet. Gynecol. 2021, 224, B2–B15. [Google Scholar] [CrossRef]
- California Maternal Quality Care Collaborative. Obstetric Hemorrhage Toolkit. 24 March 2015. Available online: https://www.cmqcc.org/node/2036 (accessed on 24 September 2021).
- Main, E.K.; Chang, S.C.; Dhurjati, R.; Cape, V.; Profit, J.; Gould, J.B. Reduction in racial disparities in severe maternal morbidity from hemorrhage in a large-scale quality improvement collaborative. Am. J. Obstet. Gynecol. 2020, 223, 123.e1–123.e14. [Google Scholar] [CrossRef] [PubMed]
- Cantor, A.G.; Holmes, R.; Bougatsos, C.; Atchison, C.; DeLoughery, T.; Chou, R. Screening and Supplementation for Iron Deficiency and Iron Deficiency Anemia During Pregnancy: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2024, 332, 914–928. [Google Scholar] [CrossRef] [PubMed]
- Lain, S.J.; Hadfield, R.M.; Raynes-Greenow, C.H.; Ford, J.B.; Mealing, N.M.; Algert, C.S.; Roberts, C.L. Quality of data in perinatal population health databases: A systematic review. Med. Care 2012, 50, e7–e20. [Google Scholar] [CrossRef] [PubMed]
| Baseline Characteristics | Cases (N = 107) | Controls (N = 285) | p α |
|---|---|---|---|
| Age, y | |||
| <20 | 8 (7.5%) | 27 (9.5%) | 0.81 |
| 20–34 | 75 (70.1%) | 198 (69.5%) | |
| ≥35 | 24 (22.4%) | 60 (21.1%) | |
| Race | |||
| Asian/Pacific Islander | 4 (3.7%) | 15 (5.3%) | 0.84 |
| Black (non-Hispanic) | 14 (13.1%) | 30 (10.5%) | |
| White (non-Hispanic) | 42 (39.3%) | 115 (40.4%) | |
| Hispanic | 44 (41.1%) | 118 (41.4%) | |
| Other | 1 (0.9%) | 1 (0.4%) | |
| Unknown | 2 (1.9%) | 6 (2.1%) | |
| Gestational age at delivery | |||
| ≥37 weeks | 39 (36.4%) | 231 (81.2%) | <0.01 |
| 32 to <37 weeks | 41 (38.3%) | 43 (15.1%) | |
| <32 weeks | 27 (25.2%) | 11 (3.9%) | |
| Pre-pregnancy body mass index (kg/m2) | 29.4 ± 9.1 (n = 101) | 28.1 ± 6.7 (n = 275) | 0.49 |
| Public health insurance | 98 (91.6%) | 284 (97.3%) | <0.01 |
| Nulliparous | 44 (41.9%) (n = 105) | 114 (40.3%) (n = 283) | 0.82 |
| Cesarean delivery | 86 (80.4%) | 98 (34.4%) | <0.0001 |
| Fetal growth restriction | 18 (16.8%) | 19 (6.7%) | <0.01 |
| Prior cesarean delivery | 41 (38.3%) | 72 (25.3%) | 0.01 |
| Multifetal gestation | 7 (6.5%) | 2 (0.7%) | <0.01 |
| Fetal malpresentation | 25 (23.4%) | 22 (7.7%) | <0.01 |
| Placenta previa or accreta spectrum | 12 (11.2%) | 4 (1.4%) | <0.01 |
| Cardiac disease | 28 (26.2%) | 6 (2.1%) | <0.01 |
| Pulmonary disease | 20 (18.7%) | 23 (8.1%) | <0.01 |
| Renal disease | 20 (18.7%) | 5 (1.8%) | <0.01 |
| Thyroid disease | 14 (13.1%) | 13 (4.6%) | <0.01 |
| Bowel disease | 12 (11.2%) | 16 (5.6%) | 0.08 |
| Gestational diabetes | 12 (11.2%) | 22 (7.7%) | 0.31 |
| Pre-gestational diabetes | 12 (11.2%) | 15 (5.3%) | 0.05 |
| Gestational hypertension or pre-eclampsia | 63 (58.9%) | 47 (16.5%) | <0.01 |
| Group B streptococcus colonization | 13 (12.1%) | 54 (18.9%) | 0.13 |
| Human immunodeficiency virus infection | 13 (12.1%) | 20 (7.0%) | 0.11 |
| Hemoglobin level on delivery admission | 11.2 ± 1.7 (95% CI: 10.9–11.5) | 11.9 ± 1.3 (95% CI: 11.7–12.0) | <0.01 |
| Anemia on delivery admission ϕ | 47 (43.9%) | 69 (24.2%) | <0.01 |
| None | 60 (56.1%) | 216 (75.8%) | <0.01 |
| Mild | 37 (34.6%) | 62 (21.8%) | |
| Moderate | 9 (8.4%) | 7 (2.5%) | |
| Severe | 1 (0.9%) | 0 (0%) |
| Severe Maternal Morbidity Component | Anemia (N = 47) | No Anemia (N = 60) | p α |
|---|---|---|---|
| Acute myocardial infarction | 0 | 0 | - |
| Aneurysm | 1 (2.1%) | 2 (3.3%) | 1.00 |
| Renal failure | 4 (8.5%) | 4 (6.7%) | 0.73 |
| ARDS | 6 (12.8%) | 4 (6.7%) | 0.33 |
| Amniotic fluid embolism | 0 | 0 | - |
| Cardiac arrest | 0 | 0 | - |
| Conversion cardiac rhythm | 1 (2.1%) | 0 | 0.44 |
| DIC | 2 (4.3%) | 1 (1.7%) | 0.58 |
| Pre-eclampsia | 18 (38.3%) | 35 (58.3%) | 0.05 |
| Cardiovascular complications | 1 (2.1%) | 3 (5.0%) | 0.63 |
| Pulmonary edema/acute heart failure | 4 (8.5%) | 6 (10.0%) | 1.00 |
| Anesthesia complications | 1 (2.1%) | 0 (0%) | 0.44 |
| Sepsis | 3 (6.4%) | 5 (8.3%) | 1.00 |
| Shock | 3 (6.4%) | 4 (6.7%) | 1.00 |
| Sickle cell crisis | 1 (2.1%) | 0 (0%) | 0.44 |
| Venous thromboembolism | 0 (0%) | 1 (1.7%) | 1.00 |
| Hysterectomy | 3 (6.4%) | 2 (3.3%) | 0.65 |
| Mechanical ventilation | 3 (6.4%) | 1 (1.7%) | 0.32 |
| Blood transfusion (gold standard) | 18 (38.3%) | 11 (18.3%) | 0.03 |
| Variable | Unadjusted OR (95% CI) | Adjusted OR (95% CI) | p α |
|---|---|---|---|
| Admission hemoglobin | 0.71 (0.61–0.84) | 0.76 (0.01–0.95) | 0.02 |
| Black race | 1.28 (0.65–2.52) | 1.78 (0.74–4.28) | 0.20 |
| Preterm delivery (<37 weeks) | |||
| Preterm delivery (32 0/7–36 6/7 weeks) | 5.81 (3.36–10.04) | 4.47 (2.17–9.19) | <0.0001 |
| Very preterm delivery (<32 weeks) | 17.18 (7.49–39.43) | 13.4 (5.16–34.8) | <0.0001 |
| Placenta previa or accreta spectrum | 8.87 (2.80–28.16) | 8.84 (2.36–33.0) | <0.01 |
| Cardiac disease | 16.5 (6.6–41.2) | 38.0 (12.0–119.8) | <0.0001 |
| Renal disease | 12.9 (4.7–35.3) | 16.5 (4.61–58.8) | <0.0001 |
| Gestational hypertension/pre-eclampsia | 7.3 (4.4–11.9) | 6.13 (3.20–11.7) | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fabricant, S.P.; Opara, K.N.; Rau, A.R.; Paul, J.V.; Girma, A.; White, J.D.; Blissett, G.; Sriprasert, I.; Korst, L.M.; Chadwick, N.M. Antenatal Maternal Hemoglobin Level and Severe Maternal Morbidity. J. Clin. Med. 2025, 14, 5823. https://doi.org/10.3390/jcm14165823
Fabricant SP, Opara KN, Rau AR, Paul JV, Girma A, White JD, Blissett G, Sriprasert I, Korst LM, Chadwick NM. Antenatal Maternal Hemoglobin Level and Severe Maternal Morbidity. Journal of Clinical Medicine. 2025; 14(16):5823. https://doi.org/10.3390/jcm14165823
Chicago/Turabian StyleFabricant, Sonya P., Karen N. Opara, Alesandra R. Rau, Julianna V. Paul, Alodia Girma, Jessica D. White, Gabriella Blissett, Intira Sriprasert, Lisa M. Korst, and Nicole M. Chadwick. 2025. "Antenatal Maternal Hemoglobin Level and Severe Maternal Morbidity" Journal of Clinical Medicine 14, no. 16: 5823. https://doi.org/10.3390/jcm14165823
APA StyleFabricant, S. P., Opara, K. N., Rau, A. R., Paul, J. V., Girma, A., White, J. D., Blissett, G., Sriprasert, I., Korst, L. M., & Chadwick, N. M. (2025). Antenatal Maternal Hemoglobin Level and Severe Maternal Morbidity. Journal of Clinical Medicine, 14(16), 5823. https://doi.org/10.3390/jcm14165823






