Prevention of Epidural Catheter Migration and Inflammation by Tunneling: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Inclusion and Exclusion Criteria
2.4. Outcomes
2.5. Data Extraction
2.6. Data Synthesis and Analysis
2.7. Risk of Bias
2.8. Assessments of Confidence
3. Results
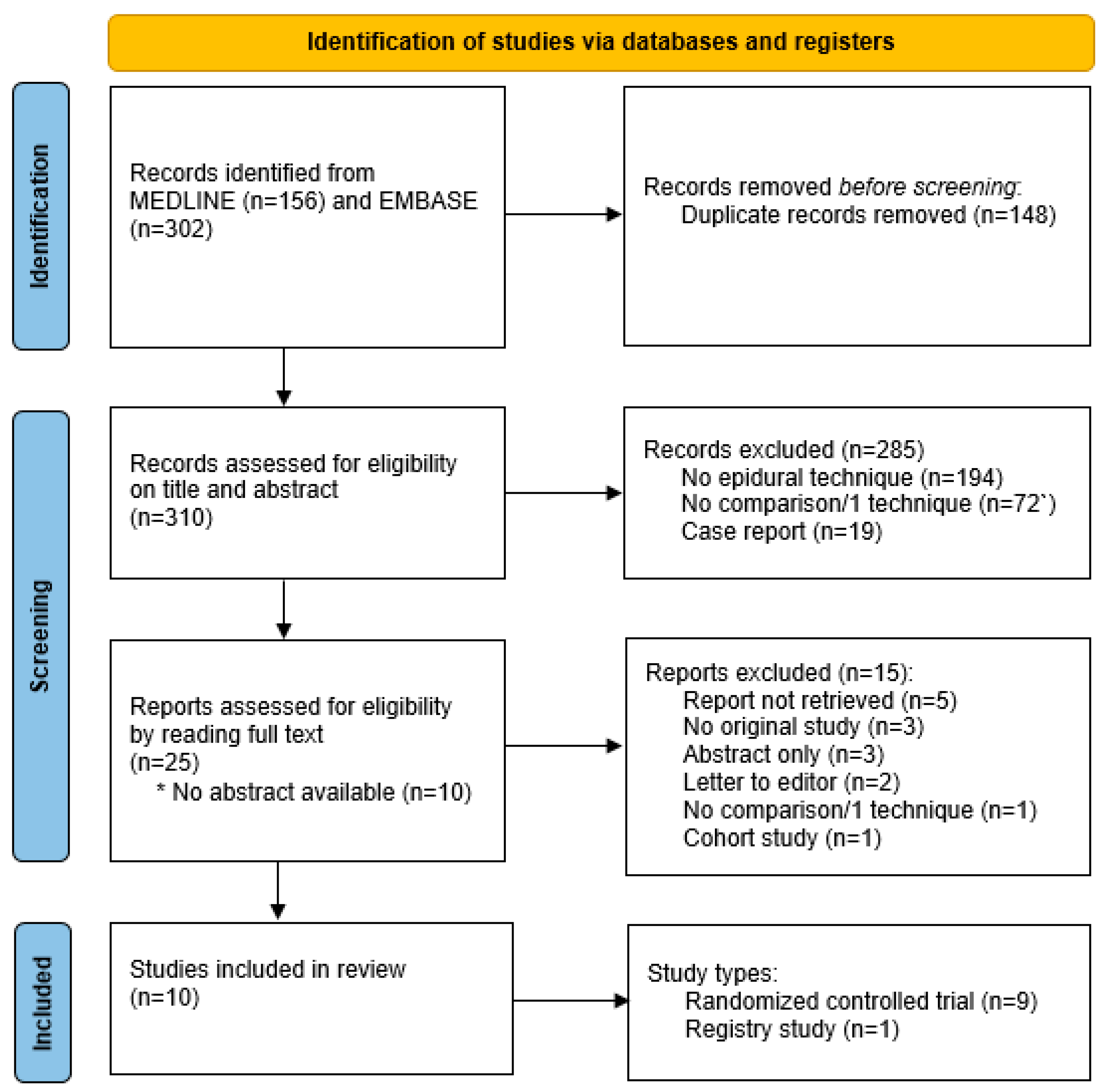
3.1. Search Results and Study Characteristics
3.2. Primary Outcomes
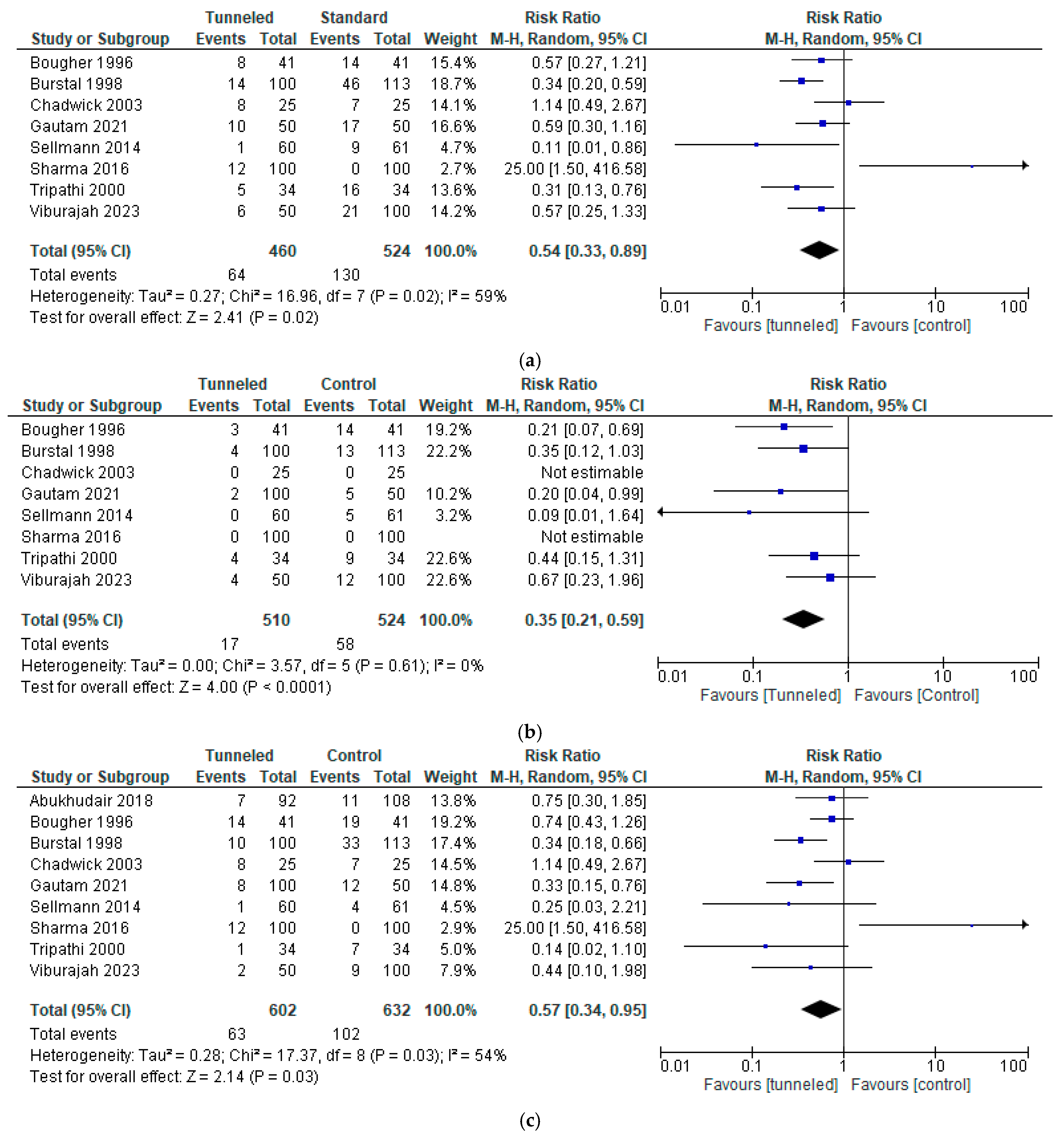
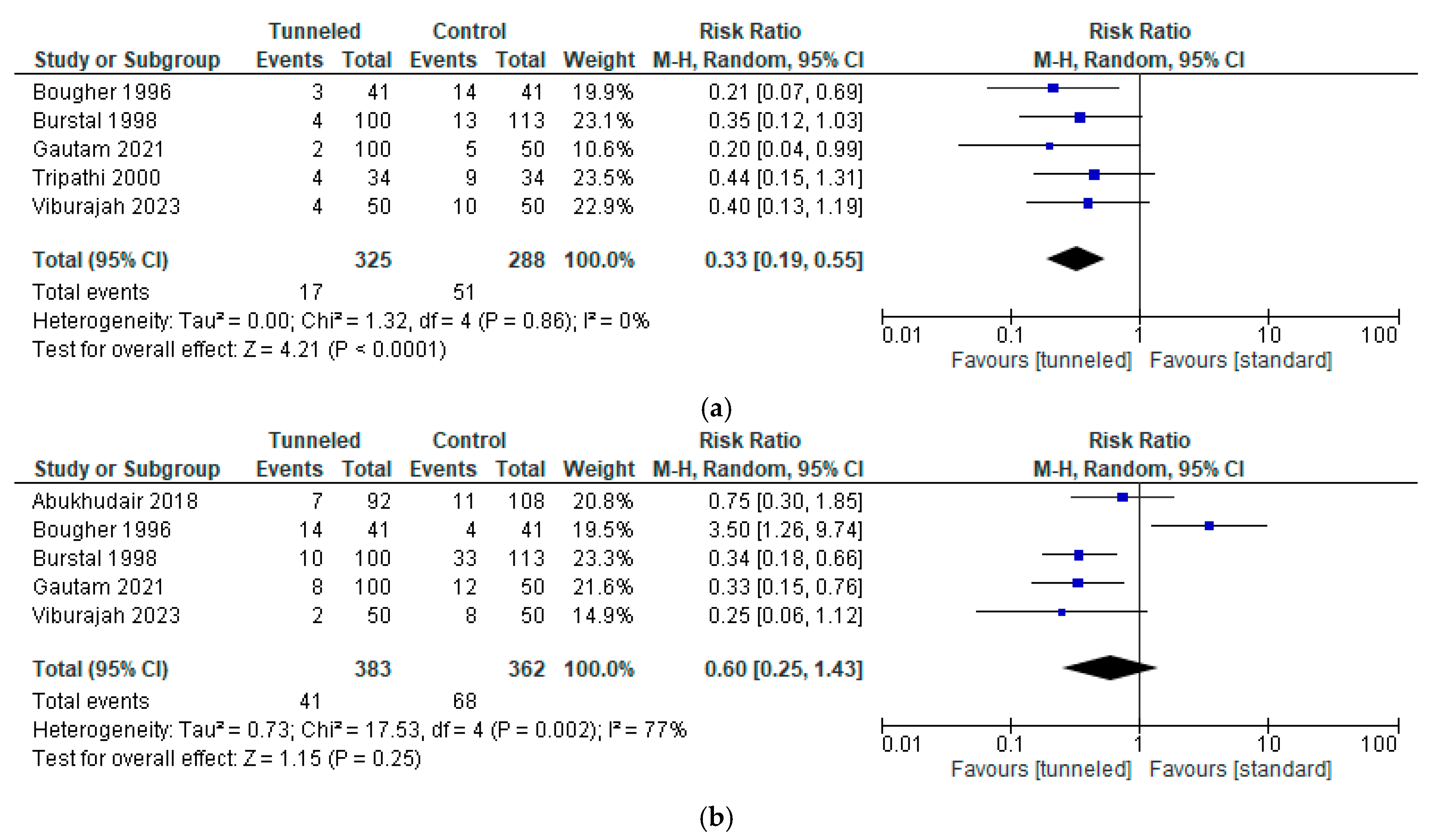
3.2.1. Migration
3.2.2. Infection
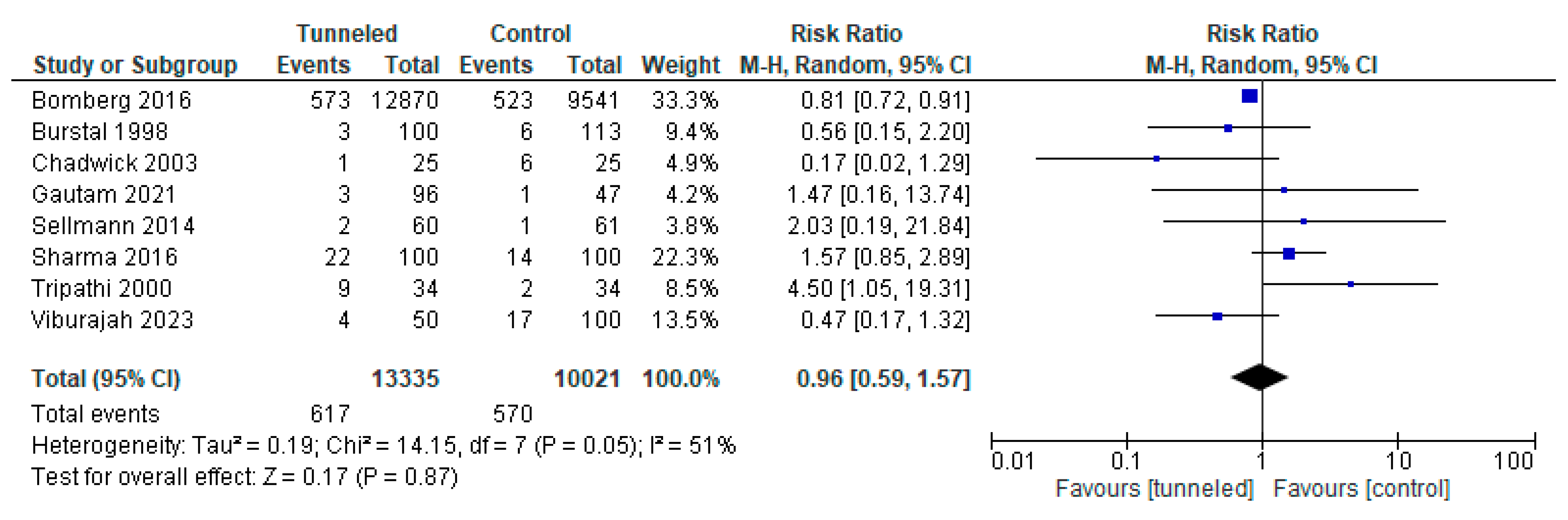
3.3. Secondary Outcome
3.4. Risk of Bias
3.5. Assessment of Confidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| RRs | Risk ratios |
| CIs | Confidence intervals |
| TG | Epidural tunnel fixation technique; tunneled group |
| CG | Any conventional epidural fixation technique; control group |
| ROB-2 | Risk of Bias assessment tool |
| GRADE | Grading of Recommendations Assessment, Development, and Evaluation |
| NNT | Number needed to treat |
References
- Faculty of Pain Medicine RCoA, Royal College of Nursing; Association of Anaesthetists; British Pain Society; European Society of Regional Anaesthesia and Pain Therapy; Association of Paediatric Anaesthetists of Great Britain and Ireland. Best Practice in the Management of Epidural Analgesia in the Hospital Setting; The Faculty of Pain Medicine of the Royal College of Anaesthetists: London, UK, 2022; pp. 1–19. [Google Scholar]
- Rosero, E.B.; Joshi, G.P. Nationwide incidence of serious complications of epidural analgesia in the United States. Acta Anaesthesiol. Scand. 2016, 60, 810–820. [Google Scholar] [CrossRef] [PubMed]
- Gautam, S.; Agarwal, A.; Das, P.K.; Khuba, S.; Kumar, S. Prevention of epidural catheter migration: A comparative evaluation of two tunneling techniques. Korean J. Anesthesiol. 2020, 74, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, C.L.; Riley, E.T.; Cohen, S.E. Changes in the position of epidural catheters associated with patient movement. Anesthesiology 1997, 86, 778–784; discussion 29A. [Google Scholar] [CrossRef] [PubMed]
- Jose, R.; Greenlin, L.; Isac, D.; Yadav, B.; Joselyn, A.S. Epidural catheter migration in non-obstetric adult surgical patients: A prospective, observational, cohort study. Indian. J. Anaesth. 2023, 67, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Phillips, D.C.; Macdonald, R. Epidural catheter migration during labour. Anaesthesia 1987, 42, 661–663. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Chambers, W.A. Tunnelling epidural catheters: A worthwhile exercise? Anaesthesia 2000, 55, 625–626. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Parasa, S.K.; Tejvath, K.; Ramachandran, G. Epidural catheter fixation. A comparison of subcutaneous tunneling versus device fixation technique. J. Anaesthesiol. Clin. Pharmacol. 2016, 32, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Bomberg, H.; Kubulus, C.; Herberger, S.; Wagenpfeil, S.; Kessler, P.; Steinfeldt, T.; Standl, T.; Gottschalk, A.; Stork, J.; Meissner, W.; et al. Tunnelling of thoracic epidural catheters is associated with fewer catheter-related infections: A retrospective registry analysis. Br. J. Anaesth. 2016, 116, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Cameron, C.M.; Scott, D.A.; McDonald, W.M.; Davies, M.J. A review of neuraxial epidural morbidity: Experience of more than 8,000 cases at a single teaching hospital. Anesthesiology 2007, 106, 997–1002. [Google Scholar] [CrossRef] [PubMed]
- Dawson, S. Epidural catheter infections. J. Hosp. Infect. 2001, 47, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Burstal, R.; Wegener, F.; Hayes, C.; Lantry, G. Subcutaneous tunnelling of epidural catheters for postoperative analgesia to prevent accidental dislodgement: A randomized controlled trial. Anaesth. Intensive Care 1998, 26, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Sellmann, T.; Bierfischer, V.; Schmitz, A.; Weiss, M.; Rabenalt, S.; MacKenzie, C.; Kienbaum, P. Tunneling and suture of thoracic epidural catheters decrease the incidence of catheter dislodgement. Sci. World J. 2014, 2014, 610635. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.S.J.; Page, M.J.; Elbers, R.G.; Sterne, J.A.C. Chapter 8: Assessing risk of bias in a randomized trial. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J.P.T.T.J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2024. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Abukhudair, H.Y.; Farhoud, E.N.; Abufarah, K.M.; Obaid, A.T.; Yousef, O.A.; Aloqoul, A.M. Tunneling Does Not Prevent Dislodgment of Epidural Catheters: A Randomized Trial. Anesth. Essays Res. 2018, 12, 930–936. [Google Scholar] [CrossRef] [PubMed]
- Bougher, R.J.; Corbett, A.R.; Ramage, D.T. The effect of tunnelling on epidural catheter migration. Anaesthesia 1996, 51, 191–194. [Google Scholar] [CrossRef] [PubMed]
- Chadwick, V.L.; Jones, M.; Poulton, B.; Fleming, B.G. Epidural catheter migration: A comparison of tunnelling against a new technique of catheter fixation. Anaesth. Intensive Care 2003, 31, 518–522. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, M.; Pandey, M. Epidural catheter fixation: Subcutaneous tunnelling with a loop to prevent displacement. Anaesthesia 2000, 55, 1113–1116. [Google Scholar] [CrossRef] [PubMed]
- Viburajah, V.; Selvaraj, V.; Sree Kumar, E.J.; Kalyan, S. Comparison of Epidural Catheter Migration in Three Different Techniques of Catheter Fixation: A Prospective Randomised Study. Anestezi Dergisi 2023, 31, 203–209. [Google Scholar] [CrossRef]
- Hermanides, J.; Hollmann, M.W.; Stevens, M.F.; Lirk, P. Failed epidural: Causes and management. Br. J. Anaesth. 2012, 109, 144–154. [Google Scholar] [CrossRef] [PubMed]

| Author, Date | Type | Population | Level Epidural | T/Co | Tunneling Technique | Fixation Technique Control | Tunneled Mean Duration Epidural (SD) | Control Mean Duration Epidural (SD) |
|---|---|---|---|---|---|---|---|---|
| Abukhudair 2018 [17] | RCT | >18 years, major surgery, ASA 1 or 2 | Both; 94%/6% 1 | 92/108 | No loop, Tuohy needle, 5 cm lateral | Adhesive tape | 2.7 d (range 1–4 d) | 2.5 d (range 1–5 d) |
| Bomberg 2016 [9] | Registry | All thoracic epidural analgesia included in the German Network for Regional Anesthesia registry (25 hospitals) | Thoracic | 12,870/9541 | N.A. | N.A. | 6.0 d (2.4 d) | 5.7d (2.2 d) |
| Bougher 1996 [18] | RCT | Post-operative epidural analgesia | Both; 45%/55% 1 | 41/41 | No loop, Tuohy needle, 5 cm lateral | Loop, adhesive spray, transparent adhesive dressing | 2.20 d (0.87 d) | 2.22d (1.11 d) |
| Burstal 1998 [13] | RCT | Post-operative epidural analgesia > 2 days | Both; 83%/17% 1 | 100/113 | No loop, 16G venflon, 6–8 cm lateral | N.A. | 3.5 d (1.3 d) | 3.1d (1.5 d) |
| Chadwick 2003 [19] | RCT | Mentally competent, major abdominal surgery | Thoracic; Th7–Th12 | 25/25 | No loop, 14G needle, 5 cm | Adhesive foam + suture, tegaderm | 4.7 d (1.4 d) | 5.3 d (1.7 d) |
| Gautam 2020 [3] 2 | RCT | 20–65 years, major upper abdominal surgery, ASA I/II | Thoracic; Th7–Th10 | 1002/50 | TG 1; with loop (1.0 cm), 16G venflon, 4 cm cranial; TG 2 no loop, 16G venflon, 4 cm cranial | Transparent adhesive dressing | TG1 5.1 d (1.4 d); TG2 5.9 d (1.2 d) | 5.7 d [1.3 d] |
| Sellman 2014 [14] | RCT | >18 years, major abdominal or thoracic surgery | Thoracic; Th3–Th12 | 60/61 | No loop, 16G venflon, >2 cm lateral, suture | Steri-strips, tegaderm | 109 h (46 h) | 97 h (37 h) |
| Sharma 2016 [8] | RCT | All, lower extremity orthopedic surgery | Lumbar; L3–L5 | 100/100 | With loop (1.5 cm), Tuohy needle, 3–5 cm caudal/cranial | Lock-It device | 72 h | 72 h |
| Tripathi 2000 [20] | RCT | Post-operative thoracic epidural analgesia | Thoracic; Th7–Th11 | 34/34 | With loop (1.5 cm), Tuohy needle, 3–5 cm caudal | Loop, adhesive dressing | 2.4 d (3.0 d) | 4.6 d (2.1 d) |
| Viburajah 2023 [21] 3 | RCT | Adult, non-obstetric surgery patients under regional anesthesia with a lumbar epidural | Lumbar; L2–L4 | 50/1003 | No loop, Tuohy needle, 2–3 cm caudal | Co1: transparent adhesive dressing tape; Co2: Lock-It device | 48 h | 48 h |
| Study | Definition Migration | Definition Infection | Definition Analgesia |
|---|---|---|---|
| Abukhudair 2018 [17] | Found loose, entirely outside patient, leaking | Not studied | Patient’s complaints of uncontrolled pain; Faces Pain scale (rest/dynamic) |
| Bomberg 2016 [9] | Not studied | Classification German Society of Anesthesiologists 1 | Not predefined: In results, pain intensity, rest/activity, infusion rate, patient satisfaction |
| Bougher 1996 [18] | Any in- or outward migration | Not studied | Not studied |
| Burstal 1998 [13] | Inward > 1 cm; Outward > 2.5 cm | Erythema and induration > 5 mm around the skin exit site; visible pus | Not studied |
| Chadwick 2003 [19] | Inward > 1 cm; Outward > 2 cm | Any signs of inflammation at the site | Patient opinion on technique and quality of analgesia; analgesic failure requires alternative analgesia or replacement epidural |
| Gautam 2020 [3] | Inward ≥ 1 cm; Outward ≥ 2 cm | Erythema and induration > 5 mm around the skin exit site; visible pus | Analgetic adequacy; inadequate analgesia requires alternative analgesia or replacement epidural |
| Sellman 2014 [14] | Inward > 2 cm; Outward > 2 cm | Classification German Society of Anesthesiologists 1 | NRS at rest/activity, after removal, patient satisfaction |
| Sharma 2016 [8] | Inward > 1 cm; Outward > 1 cm | Erythema; induration | VAS pain scores + patient’s comfort during epidural fixation by Likert’s score |
| Tripathi 2000 [20] | Any in- or outward migration | Local inflammation | Not studied |
| Viburajah 2023 [21] | Any in- or outward migration | Erythema, pain, and induration > 5 mm around the skin exit site; visible pus | Analgetic adequacy, pain at the site of injection, patient satisfaction scores (1–5) |
| Study | Analgesia Overall |
|---|---|
| Abukhudair 2018 [17] | 63/111 uncontrolled pain; No difference in uncontrolled pain between groups (p = 0.282). |
| Bomberg 2016 [9] | Only ± 50% of data available; Less pain in rest and during activity at 24 h (p < 0.001) in the tunneled group; Higher patient satisfaction overall (p < 0.001) in the tunneled group |
| Burstal 1998 [13] | 159 catheters functional at time removal; 83% tunneled; 67% control; p = 0.008. Functional without significant movement; 77% tunneled vs. 50% control; p < 0.0001. Functional > 2 days; 68% tunneled; 54% standard p = 0.037. |
| Chadwick 2003 [19] | 2/6 patients in the tunneled group with > 4 cm migration not satisfied with analgesia; 1 patient in the tunneled group unsatisfied with analgesia at day 2 without movement; 1 patient in the control group (sutured) unsatisfied with analgesia < 12 h after placement. |
| Gautam 2020 [3] | 8/96 (8%) patients of the tunneled and 8/47 (17%) patients of the control group experienced failure of analgesia. Of these 16 patients, catheter migration was observed in 8. |
| Sellman 2014 [14] | No difference in NRS during and after study (p = 0.26) |
| Sharma 2016 [8] | 77% patients in the tunneled group disliked tunneling as a method |
| Viburajah 2023 [21] | No clinically significant difference in VAS scores between the groups; Significant difference in satisfaction in favor of the tunneled and control with Lock-It group, compared to the control with adhesive dressing conventional and other groups (p < 0.001). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Kassel, M.N.; Hermanides, J.; Lirk, P.; Hollmann, M.W. Prevention of Epidural Catheter Migration and Inflammation by Tunneling: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 5788. https://doi.org/10.3390/jcm14165788
van Kassel MN, Hermanides J, Lirk P, Hollmann MW. Prevention of Epidural Catheter Migration and Inflammation by Tunneling: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(16):5788. https://doi.org/10.3390/jcm14165788
Chicago/Turabian Stylevan Kassel, Merel N., Jeroen Hermanides, Philipp Lirk, and Markus W. Hollmann. 2025. "Prevention of Epidural Catheter Migration and Inflammation by Tunneling: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 16: 5788. https://doi.org/10.3390/jcm14165788
APA Stylevan Kassel, M. N., Hermanides, J., Lirk, P., & Hollmann, M. W. (2025). Prevention of Epidural Catheter Migration and Inflammation by Tunneling: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(16), 5788. https://doi.org/10.3390/jcm14165788





