Lateralized Reverse Shoulder Arthroplasty vs. Medialized Design with Latissimus Dorsi Transfer for Cuff Tear Arthropathy with Loss of External Rotation and ER Lag Sign
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pogorzelski, J.; Fritz, E.M.; Horan, M.P.; Katthagen, J.C.; Hussain, Z.B.; Godin, J.A.; Millett, P.J. Minimum Five-Year Outcomes and Clinical Survivorship for Arthroscopic Transosseous-Equivalent Double-Row Rotator Cuff Repair. J. Am. Acad. Orthop. Surg. 2019, 27, e1093–e1101. [Google Scholar] [CrossRef]
- Raiss, P.; Rettig, O.; Wolf, S.; Loew, M.; Kasten, P. Das Bewegungsausmaß Der Schulter Und Des Ellenbogens Bei Alltagsbewegungen in Der 3D-Bewegungsanalyse. Z. Orthop. Unfall. 2007, 145, 493–498. [Google Scholar] [CrossRef]
- Boileau, P.; Watkinson, D.; Hatzidakis, A.M.; Hovorka, I. Neer Award 2005: The Grammont Reverse Shoulder Prosthesis: Results in Cuff Tear Arthritis, Fracture Sequelae, and Revision Arthroplasty. J. Shoulder Elb. Surg. 2006, 15, 527–540. [Google Scholar] [CrossRef] [PubMed]
- Werner, C.M.L.; Steinmann, P.A.; Gilbart, M.; Gerber, C. Treatment of Painful Pseudoparesis Due to Irreparable Rotator Cuff Dysfunction With the Delta Iii Reverse-Ball-And-Socket Total Shoulder Prosthesis. J. Bone Jt. Surg. 2005, 87, 1476–1486. [Google Scholar]
- Gerber, C.; Vinh, T.S.; Hertel, R.; Hess, C.W. Latissimus Dorsi Transfer for the Treatment of Massive Tears of the Rotator Cuff. A Preliminary Report. Clin. Orthop. Relat. Res. 1988, 232, 51–61. [Google Scholar] [CrossRef]
- Boileau, P.; Chuinard, C.; Roussanne, Y.; Neyton, L.; Trojani, C. Modified Latissimus Dorsi and Teres Major Transfer through a Single Delto-Pectoral Approach for External Rotation Deficit of the Shoulder: As an Isolated Procedure or with a Reverse Arthroplasty. J. Shoulder Elbow Surg. 2007, 16, 671–682. [Google Scholar] [CrossRef]
- Gerber, C.; Pennington, S.D.; Lingenfelter, E.J.; Sukthankar, A. Reverse Delta-III Total Shoulder Replacement Combined with Latissimus Dorsi Transfer: A Preliminary Report. J. Bone Jt. Surg. 2007, 89, 940–947. [Google Scholar] [CrossRef]
- Hamilton, M.A.; Diep, P.; Roche, C.; Flurin, P.H.; Wright, T.W.; Zuckerman, J.D.; Routman, H. Effect of Reverse Shoulder Design Philosophy on Muscle Moment Arms. J. Orthop. Res. 2015, 33, 605–613. [Google Scholar] [CrossRef]
- Virani, N.A.; Cabezas, A.; Gutiérrez, S.; Santoni, B.G.; Otto, R.; Frankle, M. Reverse Shoulder Arthroplasty Components and Surgical Techniques That Restore Glenohumeral Motion. J. Shoulder Elb. Surg. 2013, 22, 179–187. [Google Scholar] [CrossRef]
- Boileau, P.; Watkinson, D.J.; Hatzidakis, A.M.; Balg, F. Grammont Reverse Prosthesis: Design, Rationale, and Biomechanics. J. Shoulder Elb. Surg. 2005, 14, S147–S161. [Google Scholar] [CrossRef]
- Lawrence, C.; Williams, G.R.; Namdari, S. Influence of Glenosphere Design on Outcomes and Complications of Reverse Arthroplasty: A Systematic Review. CIOS Clin. Orthop. Surg. 2016, 8, 288–297. [Google Scholar] [CrossRef]
- Hertel, R.; Ballmer, F.T.; Lambert, S.M.; Gerber, C. Lag Signs in the Diagnosis of Rotator Cuff Rupture. J. Shoulder. Elb. Surg. 1996, 5, 307–313. [Google Scholar] [CrossRef]
- Goutallier, D.; Postel, J.M.; Bernageau, J.; Lavau, L.; Voisin, M.C. Fatty Muscle Degeneration in Cuff Ruptures. Pre- and Postoperative Evaluation by CT Scan. Clin. Orthop. Relat. Res. 1994, 304, 78–83. [Google Scholar] [CrossRef]
- Hamada, K.; Yamanaka, K.; Uchiyama, Y.; Mikasa, T.; Mikasa, M. A Radiographic Classification of Massive Rotator Cuff Tear Arthritis. Clin. Orthop. Relat. Res. 2011, 469, 2452–2460. [Google Scholar] [CrossRef] [PubMed]
- Flury, M.; Kwisda, S.; Kolling, C.; Audigé, L. Latissimus Dorsi Muscle Transfer Reduces External Rotation Deficit at the Cost of Internal Rotation in Reverse Shoulder Arthroplasty Patients: A Cohort Study. J. Shoulder Elb. Surg. 2019, 28, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Scholten Ii, D.J.; Trasolini, N.A.; Waterman, B.R. Reverse Total Shoulder Arthroplasty with Concurrent Latissimus Dorsi Tendon Transfer. Curr. Rev. Musculoskelet. Med. 2021, 14, 297–303. [Google Scholar] [CrossRef]
- Kazum, E.; Martinez-Catalan, N.; Caruso, G.; Schofield, B.A.; Nidtahar, I.; Zampeli, F.; Valenti, P. Reverse Shoulder Arthroplasty with Isolated Latissimus Dorsi or Combined with Teres Major Transfer for Lack of External Rotation: A Comparative Study. Int. Orthop. 2022, 46, 2273–2281. [Google Scholar] [CrossRef]
- Shi, L.L.; Cahill, K.E.; Ek, E.T.; Tompson, J.D.; Higgins, L.D.; Warner, J.J.P. Latissimus Dorsi and Teres Major Transfer With Reverse Shoulder Arthroplasty Restores Active Motion and Reduces Pain for Posterosuperior Cuff Dysfunction. Clin. Orthop. Relat. Res. 2015, 473, 3212–3217. [Google Scholar] [CrossRef]
- Ortmaier, R.; Hitzl, W.; Matis, N.; Mattiassich, G.; Hochreiter, J.; Resch, H. Reverse Shoulder Arthroplasty Combined with Latissimus Dorsi Transfer: A Systemic Review. Orthop. Traumatol. Surg. Res. 2017, 103, 853–859. [Google Scholar] [CrossRef]
- Patel, A.V.; Matijakovich, D.J.; Brochin, R.L.; Zastrow, R.K.; Parsons, B.O.; Flatow, E.L.; Hausman, M.R.; Cagle, P.J. Mid-Term Outcomes after Reverse Total Shoulder Arthroplasty with Latissimus Dorsi Transfer. Shoulder Elb. 2022, 14, 286–294. [Google Scholar] [CrossRef]
- Bonnevialle, N.; Elia, F.; Thomas, J.; Martinel, V.; Mansat, P. Osteolysis at the Insertion of L’Episcopo Tendon Transfer: Incidence and Clinical Impact. Orthop. Traumatol. Surg. Res. 2021, 107, 102917. [Google Scholar] [CrossRef]
- Klein, J.S.; Johnston, P.S.; Sears, B.W.; Patel, M.S.; Hatzidakis, A.M.; Lazarus, M.D. Osseous Changes Following Reverse Total Shoulder Arthroplasty Combined with Latissimus Dorsi Transfer: A Case Series. JSES Int. 2020, 4, 964–968. [Google Scholar] [CrossRef]
- Checketts, J.X.; Steele, R.; Patel, A.; Stephens, J.; Buhrke, K.; Reddy, A.; Stallings, L.; Triplet, J.J.; Chalkin, B. Clinical and Functional Outcomes of Reverse Total Shoulder Arthroplasty Supplemented with Latissimus Dorsi Transfer: A Systematic Review and Meta-Analysis. JSES Rev. Rep. Tech. 2023, 3, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Namdari, S.; Yagnik, G.; Ebaugh, D.D.; Nagda, S.; Ramsey, M.L.; Williams, G.R.; Mehta, S. Defining Functional Shoulder Range of Motion for Activities of Daily Living. J. Shoulder Elb. Surg. 2012, 21, 1177–1183. [Google Scholar] [CrossRef] [PubMed]
- Doğan, M.; Koçak, M.; Onursal Kılınç, Ö.; Ayvat, F.; Sütçü, G.; Ayvat, E.; Kılınç, M.; Ünver, Ö.; Aksu Yıldırım, S. Functional Range of Motion in the Upper Extremity and Trunk Joints: Nine Functional Everyday Tasks with Inertial Sensors. Gait Posture 2019, 70, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Collin, P.; Treseder, T.; Denard, P.J.; Neyton, L.; Walch, G.; Lädermann, A. What Is the Best Clinical Test for Assessment of the Teres Minor in Massive Rotator Cuff Tears? Clin. Orthop. Relat. Res. 2015, 473, 2959–2966. [Google Scholar] [CrossRef]
- Cuff, D.; Pupello, D.; Virani, N.; Levy, J.; Frankle, M. Reverse Shoulder Arthroplasty for the Treatment of Rotator Cuff Deficiency. J. Bone Jt. Surg. 2008, 90, 1244–1251. [Google Scholar] [CrossRef]
- Frankle, M.; Siegal, S.; Pupello, D.; Saleem, A.; Mighell, M.; Vasey, M. The Reverse Shoulder Prosthesis for Glenohumeral Arthritis Associated With Severe Rotator Cuff Deficiency: A Minimum Two-Year Follow-up Study of Sixty Patients. J. Bone Jt. Surg. 2005, 87, 1697–1705. [Google Scholar] [CrossRef]
- Greiner, S.; Schmidt, C.; König, C.; Perka, C.; Herrmann, S. Lateralized Reverse Shoulder Arthroplasty Maintains Rotational Function of the Remaining Rotator Cuff Shoulder. Clin. Orthop. Relat. Res. 2013, 471, 940–946. [Google Scholar] [CrossRef]
- Cho, S.H.; Lee, H.J.; Aldhafian, O.R.; Kim, Y.S. Comparison of Lateralized Versus Medialized Reverse Total Shoulder Arthroplasty: A Systematic Review and Meta-Analysis. Orthop. J. Sports Med. 2022, 10, 23259671211063922. [Google Scholar] [CrossRef]
- Berglund, D.D.; Rosas, S.; Triplet, J.J.; Kurowicki, J.; Horn, B.; Levy, J.C. Restoration of External Rotation Following Reverse Shoulder Arthroplasty without Latissimus Dorsi Transfer. JBJS Open Access 2018, 3, e0054. [Google Scholar] [CrossRef]
- Kwapisz, A.; Rogers, J.P.; Thigpen, C.A.; Shanley, E.; Newton, E.; Adams, K.J.; Alexander, R.; Hawkins, R.J.; Kissenberth, M.J.; Tokish, J.M.; et al. Infraspinatus or Teres Minor Fatty Infiltration Does Not Influence Patient Outcomes after Reverse Shoulder Arthroplasty with a Lateralized Glenoid. JSES Int. 2021, 5, 109–113. [Google Scholar] [CrossRef]
- Young, B.L.; Connor, P.M.; Schiffern, S.C.; Roberts, K.M.; Hamid, N. Reverse Shoulder Arthroplasty with and without Latissimus and Teres Major Transfer for Patients with Combined Loss of Elevation and External Rotation: A Prospective, Randomized Investigation. J. Shoulder Elb. Surg. 2020, 29, 874–881. [Google Scholar] [CrossRef]
- Merolla, G.; Cuoghi, F.; Athwal, G.S.; Parel, I.; Filippi, M.V.; Cutti, A.G.; Fabbri, E.; Padolino, A.; Paladini, P.; Catani, F.; et al. A Kinematic and Electromyographic Comparison of a Grammont-Style Reverse Arthroplasty Combined with a l’Episcopo Transfer Compared to a Lateralized Humeral Component Reverse for Restoration of Active External Rotation. Int. Orthop. 2021, 45, 2061–2069. [Google Scholar] [CrossRef]
- Freislederer, F.; Moroder, P.; Audigé, L.; Spagna, G.; Ameziane, Y.; Schneller, T.; Scheibel, M. Lateralized Reverse Shoulder Arthroplasty Vs. Medialized Design With Latissimus Dorsi Transfer For Cuff Tear Arthropathy With Loss Of External Rotation. J. Shoulder Elb. Surg. 2023, 32, e271. [Google Scholar] [CrossRef]

| Baseline Parameters | Group L (n) | Mean (SD) | Median (Range) | Group T (n) | Mean (SD) | Median (Range) | SMD |
|---|---|---|---|---|---|---|---|
| Age at surgery | 21 | 78 (7) | 79 (62 to 87) | 13 | 69 (6) | 69 (57 to 77) | 1.425 |
| Age (3 classes) (n, %) | 1.65 | ||||||
| < 70 | 3 (14) | 9 (69) | |||||
| 70–80 | 9 (43) | 4 (31) | |||||
| >80 | 9 (43) | ||||||
| Sex (n, %) | 0.107 | ||||||
| Female | 14 (67) | 8 (62) | |||||
| Male | 7 (33) | 5 (38) | |||||
| Diagnosis (n, %) | 0.459 | ||||||
| CTA | 21 (100) | 13 (100) | |||||
| Classification of arthrosis acc. to Samilson | 0.76 | ||||||
| I | 4 (36) | 8 (62) | |||||
| II | 5 (45) | 5 (38) | |||||
| III | 2 (18) | ||||||
| Classification of arthropathy acc. to Hamada | 0.768 | ||||||
| Stage 1 | 5 (45) | 3 (23) | |||||
| Stage 2 | 2 (18) | 1 (8) | |||||
| Stage 3 | 1 (9) | 2 (15) | |||||
| Stage 4A | 1 (8) | ||||||
| Stage 4B | 3 (27) | 6 (46) | |||||
| Fatty infiltration of teres minor Goutallier 3/4 in % | 42 | 46 | |||||
| Flexion (active) (°) | 21 | 73 (43) | 70 (0 to 170) | 13 | 87 (52) | 80 (10 to 170) | 0.294 |
| Abduction (active) (°) | 21 | 68 (35) | 70 (0 to 130) | 13 | 86 (45) | 70 (20 to 170) | 0.433 |
| External rotation (active) (°) | 21 | 0 (0) | 0 (0 to 0) | 12 | −13 (12) | −15 (−30 to 0) | 1.58 |
| Internal rotation (active) (n, %) | 0.8 | ||||||
| Lat. thigh | 1 (5) | ||||||
| Gluteal region | 3 (14) | 1 (8) | |||||
| Lumbosacral region | 2 (10) | 1 (8) | |||||
| L3 | 10 (48) | 6 (46) | |||||
| Th12 | 3 (14) | 5 (38) | |||||
| Th7 | 2 (10) | ||||||
| Flexion (passive) (°) | 21 | 101 (42) | 90 (15 to 170) | 13 | 115 (45) | 125 (40 to 180) | 0.306 |
| Abduction (passive) (°) | 21 | 92 (33) | 80 (50 to 170) | 13 | 113 (42) | 115 (50 to 180) | 0.553 |
| External rotation (passive) (°) | 21 | 20 (14) | 20 (0 to 55) | 13 | 26 (14) | 20 (10 to 60) | 0.422 |
| Abduction force (kg) | 21 | 0.5 (1.2) | 0.0 (0.0 to 4.0) | 13 | 0.8 (1.3) | 0.0 (0.0 to 4.0) | 0.289 |
| Constant–Murley Score (0 = min 100 = max) | 19 | 30 (16) | 26 (3 to 64) | 13 | 37 (14) | 34 (21 to 72) | 0.45 |
| SPADI (0 = worst, 100 = best) | 21 | 35 (23) | 31 (6 to 82) | 12 | 42 (22) | 41 (13 to 86) | 0.292 |
| Medialization of center of rotation (mm) | 12 | 20.4 (4.4) | 20.4 (14.6 to 27.9) | 12 | 23.7 (2.8) | 24.1 (19.4 to 29.1) | 1.97 |
| Humeral offset (mm) | 20 | 22.0 (3.9) | 21.5 (16.0 to 30.6) | 12 | 17.4 (3.1) | 17.6 (12.7 to 21.7) | 0.733 |
| Glenoidal offset (mm) | 20 | 5.4 (3.2) | 5.1 (1.0 to 16.9) | 11 | 0.3 (1.0) | 0.3 (−1.9 to 2.1) | 0.988 |
| Glenosphere offset (mm) | 19 | 18.4 (1.7) | 18.0 (14.0 to 21.0) | 12 | 15.3 (1.5) | 14.0 (14.0 to 17.0) | 0.105 |
| Parameters | Group L (n) | Mean (SD) | Median (Range) | Group T (n) | Mean (SD) | Median (Range) | p-Value |
|---|---|---|---|---|---|---|---|
| Flexion (active) | 10 | 133 (22) | 125 (110 to 170) | 13 | 134 (22) | 140 (80 to 170) | 0.57 |
| Abduction (active) | 10 | 117 (26) | 115 (90 to 160) | 13 | 129 (26) | 130 (70 to 160) | 0.23 |
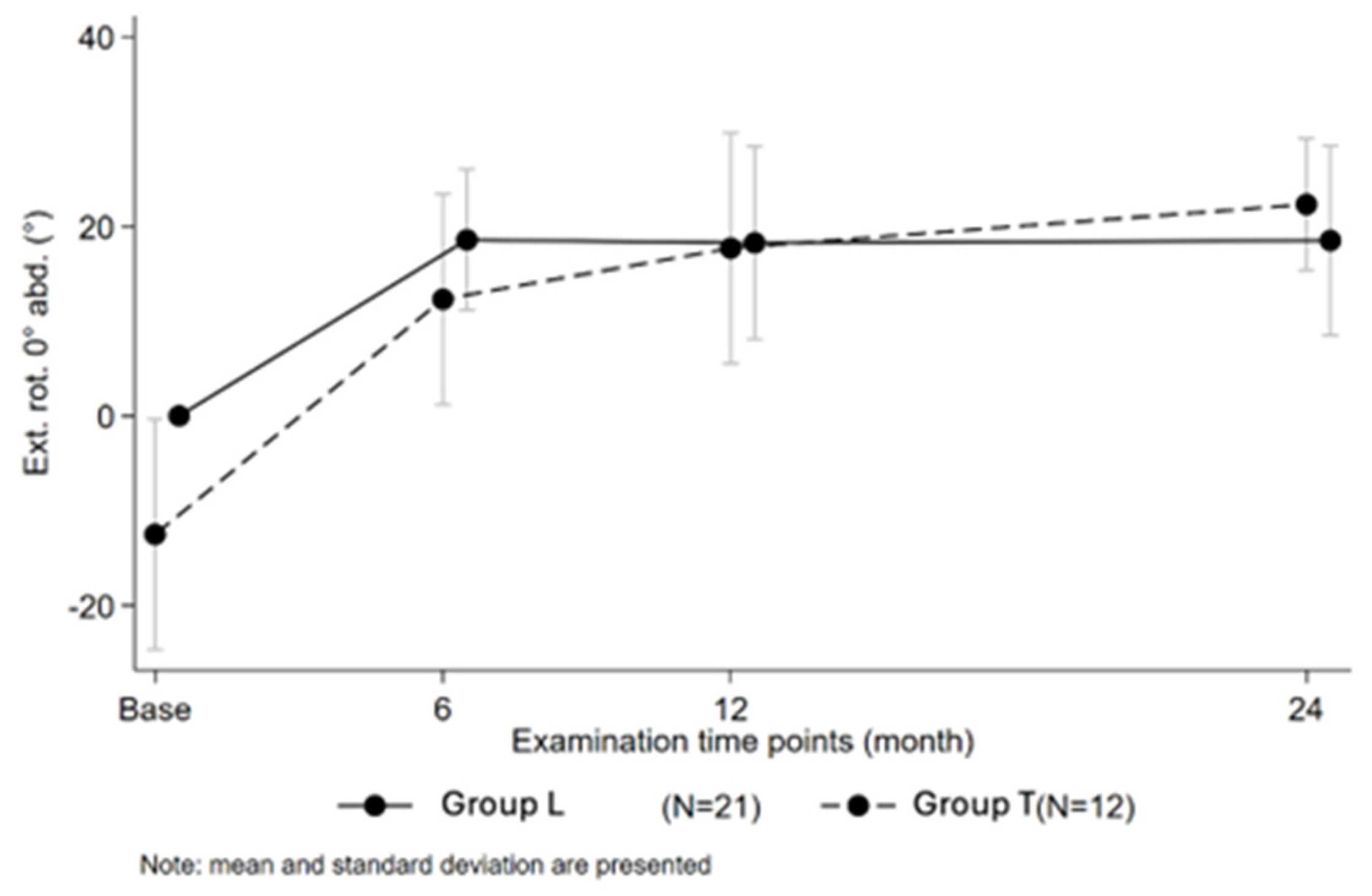
| External rotation (active) | 10 | 19 (10) | 20 (0 to 30) | 13 | 22 (7) | 20 (10 to 30) | 0.35 |
| External rotation (active) change from baseline | 10 | 18.5(9.5) | 20(0 to 30) | 13 | 34.6 (13.1) | 35 (10 to 55) | <0.05 |
| Internal rotation (active) | 0.16 | ||||||
| Lat. thigh | 0 (0) | 0 (0) | |||||
| Gluteal region | 2 (20) | 7 (54) | |||||
| Lumbosacral region | 2 (20) | 3 (23) | |||||
| L3 | 2 (20) | 3 (23) | |||||
| Th12 | 2 (20) | ||||||
| Th7 | 2 (20) | ||||||
| Constant–Murley Score (0 = min 100 = max) | 8 | 63 (9) | 65 (45 to 73) | 11 | 63 (16) | 63 (29 to 83) | 0.93 |
| Abduction force (kg) | 10 | 3.9 (1.7) | 3.8 (1.0 to 7.0) | 12 | 5.5 (2.9) | 5.0 (0.0 to 10.0) | 0.11 |
| SPADI (0 = worst, 100 = best) | 16 | 74 (22) | 80 (23 to 99) | 10 | 73 (20) | 78 (25 to 91) | 0.9 |
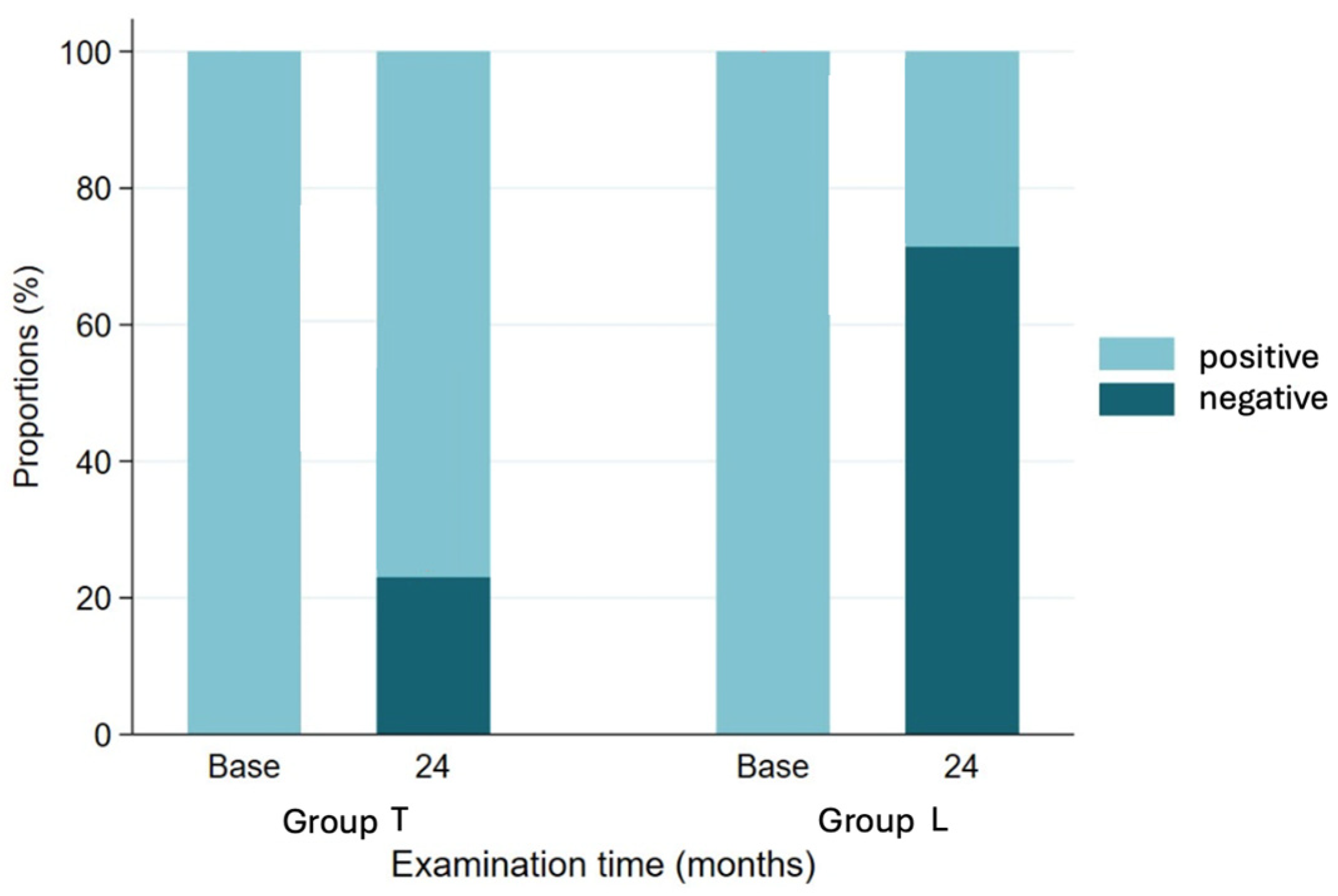
| ER lag sign (n, %) | <0.05 | ||||||
| Negative | 7 (70) | 3 (23) | |||||
| Positive | 3 (30) | 10 (77) | |||||
| Apley’s test internal rotation up to L3 or more (n, %) | <0.05 | ||||||
| No | 3 (33) | 10 (77) | |||||
| Yes | 6 (67) | 3 (23) |
| Parameter | Negative ER Lag (n) | Mean (SD) | Median (Range) | Positive ER Lag (n) | Mean (SD) | Median (Range) | Effect (95% CI) | p-Value |
|---|---|---|---|---|---|---|---|---|
| Humeral Offset | 18 | 21.3 (4.0) | 19.5 (16.9 to 28.4) | 16 | 17.7 (3.2) | 18.5 (12.7 to 21.7) | −3.6 (−6.6 to −0.6) | <0.05 |
| Glenoidal Offset | 18 | 5.6 (5.0) | 5.3 (0.0 to 16.9) | 16 | 1.1 (2.1) | 0.6 (−1.9 to 5.3) | −4.5 (−7.6 to −1.4) | <0.05 |
| Glenosphere Offset | 18 | 17.2 (1.6) | 18.0 (14.0 to 19.5) | 16 | 15.5 (2.0) | 14.0 (14.0 to 19.5) | −1.7 (−3.3 to −0.1) | 0.055 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Warnhoff, M.; Moroder, P.; Audigé, L.; Spagna, G.; Ameziane, Y.; Schneller, T.; Scheibel, M.; Freislederer, F. Lateralized Reverse Shoulder Arthroplasty vs. Medialized Design with Latissimus Dorsi Transfer for Cuff Tear Arthropathy with Loss of External Rotation and ER Lag Sign. J. Clin. Med. 2025, 14, 5679. https://doi.org/10.3390/jcm14165679
Warnhoff M, Moroder P, Audigé L, Spagna G, Ameziane Y, Schneller T, Scheibel M, Freislederer F. Lateralized Reverse Shoulder Arthroplasty vs. Medialized Design with Latissimus Dorsi Transfer for Cuff Tear Arthropathy with Loss of External Rotation and ER Lag Sign. Journal of Clinical Medicine. 2025; 14(16):5679. https://doi.org/10.3390/jcm14165679
Chicago/Turabian StyleWarnhoff, Mara, Philipp Moroder, Laurent Audigé, Giovanni Spagna, Yacine Ameziane, Tim Schneller, Markus Scheibel, and Florian Freislederer. 2025. "Lateralized Reverse Shoulder Arthroplasty vs. Medialized Design with Latissimus Dorsi Transfer for Cuff Tear Arthropathy with Loss of External Rotation and ER Lag Sign" Journal of Clinical Medicine 14, no. 16: 5679. https://doi.org/10.3390/jcm14165679
APA StyleWarnhoff, M., Moroder, P., Audigé, L., Spagna, G., Ameziane, Y., Schneller, T., Scheibel, M., & Freislederer, F. (2025). Lateralized Reverse Shoulder Arthroplasty vs. Medialized Design with Latissimus Dorsi Transfer for Cuff Tear Arthropathy with Loss of External Rotation and ER Lag Sign. Journal of Clinical Medicine, 14(16), 5679. https://doi.org/10.3390/jcm14165679







