Effects of NMES-Guided Scapular Retraction Exercise Program in Amateur Female Handball Players with Scapular Dyskinesis Without Shoulder Pain: A Randomized Controlled Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Desgin
2.2. Participants
- (a)
- Static scapular assessment: The test was assessed in a neutral and standing position as proposed Sayaca et al. [24]. SD was accepted as positive if the difference between the upper horizontal distance and lower horizontal distance was >1.5 cm.
- (b)
- Visual-based palpation classification method for SD according to Huang et al. [25]: SD was classified as a single abnormal scapular pattern [inferior angle (pattern I), medial border (pattern II), superior border of scapula prominence or abnormal scapulohumeral rhythm (pattern III)], a mixture of the above abnormal scapular patterns, or a normal pattern (pattern IV). The assessment of SD was evaluated as the subjects performed bilateral arm raising/lowering movements with a weighted load (1.5 kg) in the scapular plane (5 repetitions). This method has shown moderate-to-substantial inter-rater reliability [25].
- (c)
- Test battery according to the McClure scale [26]: This measurement represents a reliable and feasible method for clinical examination of overhead athletes. Each test movement (flexion and abduction) was rated as follows:
- Normal: Both test motions are rated as normal, or 1 motion is rated as normal, and the other as having a subtle abnormality.
- Subtle abnormality: Both flexion and abduction are rated as having subtle abnormalities.
- Obvious abnormality: Either flexion or abduction is rated as having obvious abnormality.
- Exclusion criteria: players with presence of instability shown by a positive apprehension test, sulcus sign, and/or positive anterior drawer [27] at the time of recruitment or within the last 12 months; (ii) history of recurrent shoulder subluxation [28]; (iii) drug consumption with potential effects on balance and/or postural control in the 24 h prior to the initial assessment; (iv) having participated in an exercise-based preventive program or having had shoulder complex surgery in the last 12 months [26,29].
2.3. Sample Size Calculation
2.4. Randomization
2.5. Procedures
Outcomes Measures
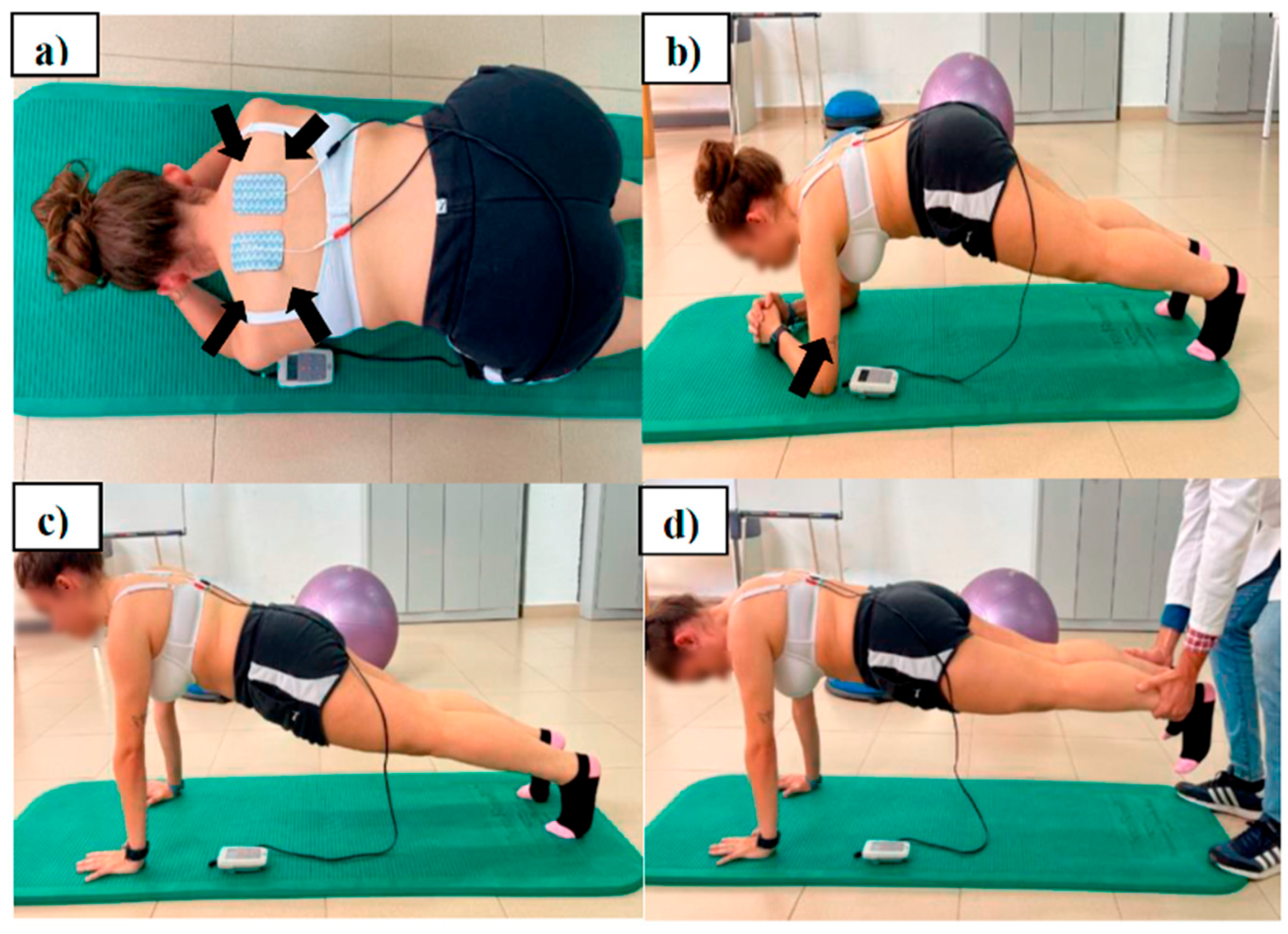
2.6. Intervention
2.7. Statistical Analysis
3. Results
4. Discussion
4.1. Clinical Impact of Interventions, as Assessed by Number Needed to Treat
4.2. Clinical Implications
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Asker, M.; Brooke, H.; Walden, M.; Tranaeus, U.; Johansson, F.; Skillgate, E.; Holm, L.W. Glenohumeral internal rotation deficit and risk of upper extremity injury in overhead athletes: A meta-analysis and systematic review. Br. J. Sports Med. 2018, 52, 1312–1319. [Google Scholar]
- Clarsen, B.; Bahr, R.; Andersson, S.H.; Munk, R.; Myklebust, G. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: A prospective cohort study. Br. J. Sports Med. 2014, 48, 1327–1333. [Google Scholar]
- Andersson, S.; Bahr, R.; Clarsen, B.; Myklebust, G. Risk factors for overuse shoulder injuries in a mixed-sex cohort of 329 elite handball players: Previous findings could not be confirmed. Br. J. Sports Med. 2017, 52, 1191–1198. [Google Scholar]
- Edouard, P.; Degache, F.; Oullion, R.; Plessis, J.Y.; Gleizes-Cervera, S.; Clamels, P. Shoulder strength imbalances as injury risk in handball. Int. J. Sports Med. 2013, 34, 654–660. [Google Scholar]
- Giroto, N.; Hespanhol Junior, L.; Gomes, M.; Lopes, A. Incidence and risk factors of injuries in Brazilian elite handball players: A prospective cohort study. Scand. J. Med. Sci. Sports 2015, 27, 195–202. [Google Scholar]
- Mornieux, G.; Hirschmüller, A.; Gollhofer, A.; Südkamp, N.P.; Maier, D. Multimodal assessment of sensorimotor shoulder function in patients with untreated anterior shoulder instability and asymptomatic handball players. J. Sports Med. Phys. Fitness 2018, 58, 472–479. [Google Scholar]
- Møller, M.; Nielsen, R.; Attermann, J.; Wedderkopp, N.; Lind, M.; Sørensen, H.; Myklebust, G. Handball load and shoulder injury rate: A 31-week cohort study of 679 elite youth handball players. Br. J. Sports Med. 2017, 51, 231–237. [Google Scholar]
- Hickey, D.; Solvig, V.; Cavalheri, V.; Harrold, M.; McKenna, L. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 102–110. [Google Scholar]
- Huang, T.-S.; Ou, H.-L.; Huang, C.-Y.; Lin, J.-J. Specific kinematics and associated muscle activation in individuals with scapular dyskinesis. J. Shoulder Elbow Surg. 2015, 24, 1227–1234. [Google Scholar]
- Asker, M.; Holm, L.; Källberg, H.; Waldén, M.; Skillgate, E. Female adolescent elite handball players are more susceptible to shoulder problems than their male counterparts. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1892–1900. [Google Scholar]
- Huang, T.S.; Du, W.Y.; Lin, J.J. Clinical Factors Related to Improved Scapular Control After a Scapular Conscious Control Program in Symptomatic Overhead Athletes: Secondary Analysis of a Randomized Controlled Trial. Orthop. J. Sports Med. 2020, 8, 2325967120964600. [Google Scholar]
- Kibler, W.B.; Ludewig, P.M.; McClure, P.W.; Michener, L.A.; Bak, K.; Sciascia, A.D. Clinical implications of scapular dyskinesis in shoulder injury: The 2013 consensus statement from the “Scapular Summit”. Br. J. Sports Med. 2013, 47, 877–885. [Google Scholar] [CrossRef]
- Cools, A.; Declercq, G.; Cambier, D.; Mahieu, N.; Witvrouw, E. Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand. J. Med. Sci. Sports 2007, 17, 25–33. [Google Scholar]
- Cools, A.M.; Struyf, F.; De Mey, K.; Maenhout, A.; Castelein, B.; Cagnie, B. Rehabilitation of scapular dyskinesis: From the office worker to the elite overhead athlete. Br. J. Sports Med. 2014, 48, 692–697. [Google Scholar] [CrossRef]
- Moghadam, A.N.; Rahnama, L.; Dehkordi, S.N.; Abdollahi, S. Exercise therapy may affect scapular position and motion in individuals with scapular dyskinesis: A systematic review of clinical trials. J. Shoulder Elbow Surg. 2020, 29, e29–e36. [Google Scholar] [CrossRef]
- Kamonseki, D.H.; Haik, M.N.; Ribeiro, L.P.; Almeida, R.F.; Camargo, P.R. Scapular movement training is not superior to standardized exercises in the treatment of individuals with chronic shoulder pain and scapular dyskinesis: Randomized controlled trial. Disabil. Rehabil. 2023, 45, 2925–2935. [Google Scholar]
- Colson, S.S.; Benchortane, M.; Tanant, V.; Faghan, J.-P.; Fournier-Mehouas, M.; Benaïm, C.; Desnuelle, C.; Sacconi, S. Neuromuscular Electrical Stimulation on Training: A Safe and Effective Treatment for Facioscapulohumeral Muscular Dystrophy Patients. Arch. Phys. Med. Rehabil. 2010, 91, 697–702. [Google Scholar] [CrossRef]
- Veldman, M.P.; Gondin, J.; Place, N.; Maffiuletti, N.A. Effects of Neuromuscular Electrical Stimulation Training on Endurance Performance. Front. Physiol. 2016, 7, 544. [Google Scholar] [CrossRef]
- Baldwin, E.R.L.; Baldwin, T.D.; Lancaster, J.S.; McNeely, M.L.; Collins, D.F. Neuromuscular electrical stimulation and exercise for reducing trapezius muscle dysfunction in survivors of head and neck cancer: A case-series report. Physiother. Can. 2012, 64, 317–324. [Google Scholar] [CrossRef]
- Gomes da Silva, C.; Lima e Silva, F.; Vianna, K.; Oliveira, G.; Vaz, M.; Baroni, B. Eccentric training combined to neuromuscular electrical stimulation is not superior to eccentric training alone for quadriceps strengthening in healthy subjects: A randomized controlled trial. Braz. J. Phys. Ther. 2018, 22, 502–511. [Google Scholar]
- Yanase, K.; Hasegawa, S.; Nakamura, M.; Yamauchi, T.; Nishishita, S.; Araki, K.; Umehara, J.; Fujita, K.; Sato, I.; Ibuki, S.; et al. Electrical stimulation to the infraspinatus on hypertrophy and strength of the shoulder. Int. J. Sports Med. 2018, 39, 828–834. [Google Scholar]
- Burn, M.B.; McCulloch, P.C.; Lintner, D.M.; Liberman, S.R.; Harris, J.D. Prevalence of scapular dyskinesis in overhead and non-overhead athletes: A systematic review. Orthop. J. Sports Med. 2016, 4, 2325967115627608. [Google Scholar] [CrossRef]
- Vigolvino, L.P.; Barros, B.R.S.; Medeiros, C.E.B.; Pinheiro, S.M.; Sousa, C.O. Analysis of the presence and influence of Glenohumeral Internal Rotation Deficit on posterior stiffness and isometric shoulder rotators strength ratio in recreational and amateur handball players. Phys. Ther. Sport 2020, 42, 1–8. [Google Scholar] [CrossRef]
- Sayaca, C.; Unal, M.; Calik, M.; Eyuboglu, F.E.; Kaya, D.; Ozenci, M. Scapular Dyskinesis, Shoulder Joint Position Sense, and Functional Level After Arthroscopic Bankart Repair. Orthop. J. Sports Med. 2021, 9, 2325967120985207. [Google Scholar] [CrossRef]
- Huang, T.S.; Huang, H.Y.; Wang, T.G.; Tsai, Y.-S.; Lin, J.-J. Comprehensive classification test of scapular dyskinesis: A reliability study. Man. Ther. 2015, 20, 427–432. [Google Scholar]
- McClure, P.; Tate, A.R.; Kareha, S.; Irwin, D.; Zlupko, E. A clinical method for identifying scapular dyskinesis, Part 1: Reliability. J. Athl. Train. 2009, 44, 160–164. [Google Scholar]
- Myers, J.B.; Laudner, K.G.; Pasquale, M.R.; Bradley, J.P.; Lephart, S.M. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am. J. Sports Med. 2006, 34, 385–391. [Google Scholar]
- Cieminski, C.J.; Klaers, H.; Kelly, S.M.; Stelzmiller, M.R.; Nawrocki, T.J.; Indrelie, A.J. Total arc of motion in the sidelying position: Evidence for new method to assess glenohumeral internal rotation deficit in overhead athletes. Int. J. Sports Phys. Ther. 2015, 10, 319–331. [Google Scholar]
- Guney, H.; Harput, G.; Colakoglu, F.; Baltaci, G. The Effect of Glenohumeral Internal-Rotation Deficit on Functional Rotator-Strength Ratio in Adolescent Overhead Athletes. J. Sport Rehabil. 2016, 25, 52–57. [Google Scholar] [CrossRef]
- Larsen, C.; Søgaard, K.; Eshoj, H.; Ingwersen, K.; Juul-Kristensen, B. Clinical assessment methods for scapular positioning and function: An inter-rater reliability study. Physiother. Theory Pract. 2020, 36, 1399–1420. [Google Scholar]
- Wirtz, N.; Zinner, C.; Doermann, U.; Kleinoeder, H.; Mester, J. Effects of loaded squat exercise with and without application of superimposed EMS on physical performance. J. Sports Sci. Med. 2016, 15, 26–33. [Google Scholar]
- Kibler, W.B.; Sciascia, A. Evaluation and Management of Scapular Dyskinesis in Overhead Athletes. Curr. Rev. Musculoskelet. Med. 2019, 12, 515–526. [Google Scholar] [CrossRef]
- Schory, A.; Bidinger, E.; Joshua, W.; Murray, L. A systematic review of the exercises that produce optimal muscle ratios of the scapular stabilizers in normal shoulders. Int. J. Sports Phys. Ther. 2016, 11, 321–336. [Google Scholar]
- Asker, M.; Hägglund, M.; Waldén, M.; Källberg, H.; Skillgate, E. The Effect of Shoulder and Knee Exercise Programmes on the Risk of Shoulder and Knee Injuries in Adolescent Elite Handball Players: A Three-Armed Cluster Randomised Controlled Trial. Sports Med. Open 2022, 8, 91. [Google Scholar] [CrossRef]
- Lee, J.; Kim, L.N.; Song, H.; Kim, S.; Woo, S. The effect of glenohumeral internal rotation deficit on the isokinetic strength, pain, and quality of life in male high school baseball players. Ann. Rehabil. Med. 2015, 39, 183–190. [Google Scholar]
- Slade, S.C.; Dionne, C.E.; Underwood, M.; Buchbinder, R. Consensus on Exercise Reporting Template (CERT): Modified Delphi Study. Phys. Ther. 2016, 96, 1514–1524. Available online: https://academic.oup.com/ptj/article/96/10/1514/2870241 (accessed on 16 June 2021).
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Barbour, V.; Barbour, V.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide statements. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef]
- Sciascia, A.; Kibler, W.B. Current Views of Scapular Dyskinesis and its Possible Clinical Relevance. Int. J. Sports Phys. Ther. 2022, 17, 117–130. [Google Scholar] [CrossRef]
- Huang, T.S.; Du, W.Y.; Wang, T.G.; Tsai, Y.S.; Yang, J.L.; Huang, C.Y.; Lin, J.J. Conscious control of scapular orientation with video feedback has improvement in muscle balance ratio in patients with scapular dyskinesis: A randomized controlled trial. J. Shoulder Elbow Surg. 2018, 27, 1407–1414. [Google Scholar]
- DiFiori, J.P.; Benjamin, H.J.; Brenner, J.S.; Gregory, A.; Jayanthi, N.; Landry, G.L.; Luke, A. Overuse injuries and burnout in youth sports: A position statement from the American Medical Society for Sports Medicine. Br. J. Sports Med. 2014, 48, 287–288. [Google Scholar]
- Lynch, S.; Thigpen, C.; Mihalik, J.; Prentice, W.; Padua, D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br. J. Sports Med. 2010, 44, 376–381. [Google Scholar]
- Gondin, J.; Cozzone, P.J.; Bendahan, D. Is high-frequency neuromuscular electrical stimulation a suitable tool for muscle performance improvement in both healthy humans and athletes? Eur. J. Appl. Physiol. 2011, 111, 2473–2487. [Google Scholar]
- Bragazzi, N.L.; Rouissi, M.; Hermassi, S.; Chamari, K. Resistance Training and Handball Players’ Isokinetic, Isometric and Maximal Strength, Muscle Power and Throwing Ball Velocity: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 2663. [Google Scholar]
- Zory, R.F.; Jubeau, M.M.; Maffiuletti, N.A. Contractile impairment after quadriceps strength training via electrical stimulation. J. Strength Cond. Res. 2010, 24, 458–464. [Google Scholar]
- Mascarin, N.C.; Barbosa de Lira, C.A.; Vancini, R.L.; Pochini, A.C.; Da Silva, A.C.; Andrade, M.S.C. Strength training using elastic bands: Improvement of muscle power and throwing performance in young female handball players. J. Sport Rehabil. 2017, 26, 245–252. [Google Scholar]


| Total Sample (n = 32) | Group 1 (n = 16) | Group 2 (n = 16) | p Value * | |
|---|---|---|---|---|
| Mean age (years) | 23 (3.23) | 24 (3.75) | 23 (2.69) | 0.593 |
| Height (cm) | 167 (4.31) | 166 (4.66) | 167 (4.01) | 0.470 |
| Weight (kg) | 60.8 (8.01) | 61.0 (9.01) | 60.7 (7.18) | 0.914 |
| Body mass index | 21.6 (2.25) | 21.8 (2.51) | 21.4 (2.03) | 0.623 |
| Hours of sport/week | 7 (1.01) | 7 (1.05) | 7 (0.95) | 0.194 |
| Throwing shoulder (right/left) | 28/4 | 14/2 | 14/2 | 1 |
| Scapular dyskinesis test | ||||
| Pattern I (%) (subtle/obvious abnormality) | 14 (43.7) Subtle: 3 Obvious: 11 | 8 (50) | 6 (37.5) | |
| Pattern II (%) (subtle/obvious abnormality) | 11 (34.4) Subtle: 2 Obvious: 9 | 5 (31.2) | 6 (37.5) | |
| Pattern III (%) (subtle/obvious abnormality) | 2 (6.2) Obvious: 2 | 1 (6.2) | 1 (6.2) | |
| Pattern IV (%) (subtle/obvious abnormality) | 5 (15.6) Subtle: 1 Obvious: 4 | 2 (12.5) | 3 (18.7) | |
| Upper horizontal distance (mm) | 86.7 (13.41) | 87.2 (12.37) | 86.2 (14.77) | 0.847 |
| Lower horizontal distance (mm) | 89.1 (10.77) | 89.7 (11.89) | 88.4 (9.87) | 0.749 |
| IR RoM (°) | 40.2 (5.49) | 41.2 (3.68) | 39.2 (6.83) | 0.296 |
| ER strength (N) | 45.29 (7.47) | 44.15 (7.75) | 46.11 (7.26) | 0.777 |
| ER strength (BW%) | 7.75 (1.28) | 7.67 (1.46) | 7.75 (1.16) | 0.739 |
| Baseline | Post-Intervention | Within-Group Mean Changes | d | Between-Groups Mean Changes | |
|---|---|---|---|---|---|
| Upper horizontal distance (mm) | |||||
| Group 1 (SRE) | 87.2 (12.37) | 82.4 (14.04) | 4.8 [0.8/8.6] * | 0.18 | 19.3 [9.7/28.7] †† |
| Group 2 (SRE + NMES) | 86.2 (14.77) | 63.1 (12.22) | 23.1 [17.2/28.9] ** | 0.65 | |
| Lower horizontal distance (mm) | |||||
| Group 1 (SRE) | 89.7 (11.89) | 79.9 (8.92) | 9.8 [5.6/13.8] ** | 0.42 | 10.5 [4.3/16.8] † |
| Group 2 (SRE + NMES) | 88.4 (9.88) | 69.4 (8.34) | 19.0 [15.3/22.7] ** | 0.72 | |
| IR RoM (°) | |||||
| Group 1 (SRE) | 47.2 (3.68) | 47.4 (2.31) | −0.2 [−2.0/1.7] | 3.4 [0.6/7.5] | |
| Group 2 (SRE + NMES) | 45.2 (6.83) | 44.0 (7.58) | 1.2 [−1.7/4.1] | ||
| ER strength (N) | |||||
| Group 1 (SRE) | 44.15 (7.75) | 49.05 (8.34) | −4.91 [−7.85/−1.96] * | 0.29 | 10.79 [4.91/15.70] † |
| Group 2 (SRE + NMES) | 46.11 (7.26) | 59.84 (6.67) | −13.73 [−17.66/−10.79] ** | 0.71 | |
| ER strength (BW%) | |||||
| Group 1 (SRE) | 7.67 (1.46) | 8.47 (1.52) | −0.80 [−1.2/−0.3] * | 0.26 | 1.45 [0.5/2.4] † |
| Group 2 (SRE + NMES) | 7.75 (1.16) | 9.92 (1.15) | −2.17 [−2.72/−1.62] ** | 0.69 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Espejo-Antúnez, L.; Gutiérrez-Coronado, J.; Fernández-Morales, C.; Albornoz-Cabello, M.; Prato, L.F.; Cardero-Durán, M.d.l.Á. Effects of NMES-Guided Scapular Retraction Exercise Program in Amateur Female Handball Players with Scapular Dyskinesis Without Shoulder Pain: A Randomized Controlled Clinical Trial. J. Clin. Med. 2025, 14, 5567. https://doi.org/10.3390/jcm14155567
Espejo-Antúnez L, Gutiérrez-Coronado J, Fernández-Morales C, Albornoz-Cabello M, Prato LF, Cardero-Durán MdlÁ. Effects of NMES-Guided Scapular Retraction Exercise Program in Amateur Female Handball Players with Scapular Dyskinesis Without Shoulder Pain: A Randomized Controlled Clinical Trial. Journal of Clinical Medicine. 2025; 14(15):5567. https://doi.org/10.3390/jcm14155567
Chicago/Turabian StyleEspejo-Antúnez, Luis, Javier Gutiérrez-Coronado, Carlos Fernández-Morales, Manuel Albornoz-Cabello, Luis Fernando Prato, and María de los Ángeles Cardero-Durán. 2025. "Effects of NMES-Guided Scapular Retraction Exercise Program in Amateur Female Handball Players with Scapular Dyskinesis Without Shoulder Pain: A Randomized Controlled Clinical Trial" Journal of Clinical Medicine 14, no. 15: 5567. https://doi.org/10.3390/jcm14155567
APA StyleEspejo-Antúnez, L., Gutiérrez-Coronado, J., Fernández-Morales, C., Albornoz-Cabello, M., Prato, L. F., & Cardero-Durán, M. d. l. Á. (2025). Effects of NMES-Guided Scapular Retraction Exercise Program in Amateur Female Handball Players with Scapular Dyskinesis Without Shoulder Pain: A Randomized Controlled Clinical Trial. Journal of Clinical Medicine, 14(15), 5567. https://doi.org/10.3390/jcm14155567







