Intramedullary Nailing vs. Plate Fixation for Trochanteric Femoral Fractures: A Systematic Review and Meta-Analysis of Randomized Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
- Design: Randomized controlled trials.
- Population: Adult patients with proximal femoral fractures involving the trochanteric region (i.e., fractures affecting the greater and/or lesser trochanter, with or without intertrochanteric extension). Studies focusing exclusively on subtrochanteric, femoral neck, or femoral shaft fractures were excluded.
- Interventions: Intramedullary nailing (e.g., proximal femoral nails, Ender nails, Gamma nails, etc.).
- Comparators: Plate fixation (e.g., sliding/dynamic hip screws, locking plates, compression plates).
- Outcomes: Reporting of at least one relevant clinical, functional, perioperative, or biomechanical outcome.
2.3. Data Extraction and Outcomes
2.4. Statistical Analysis
3. Results
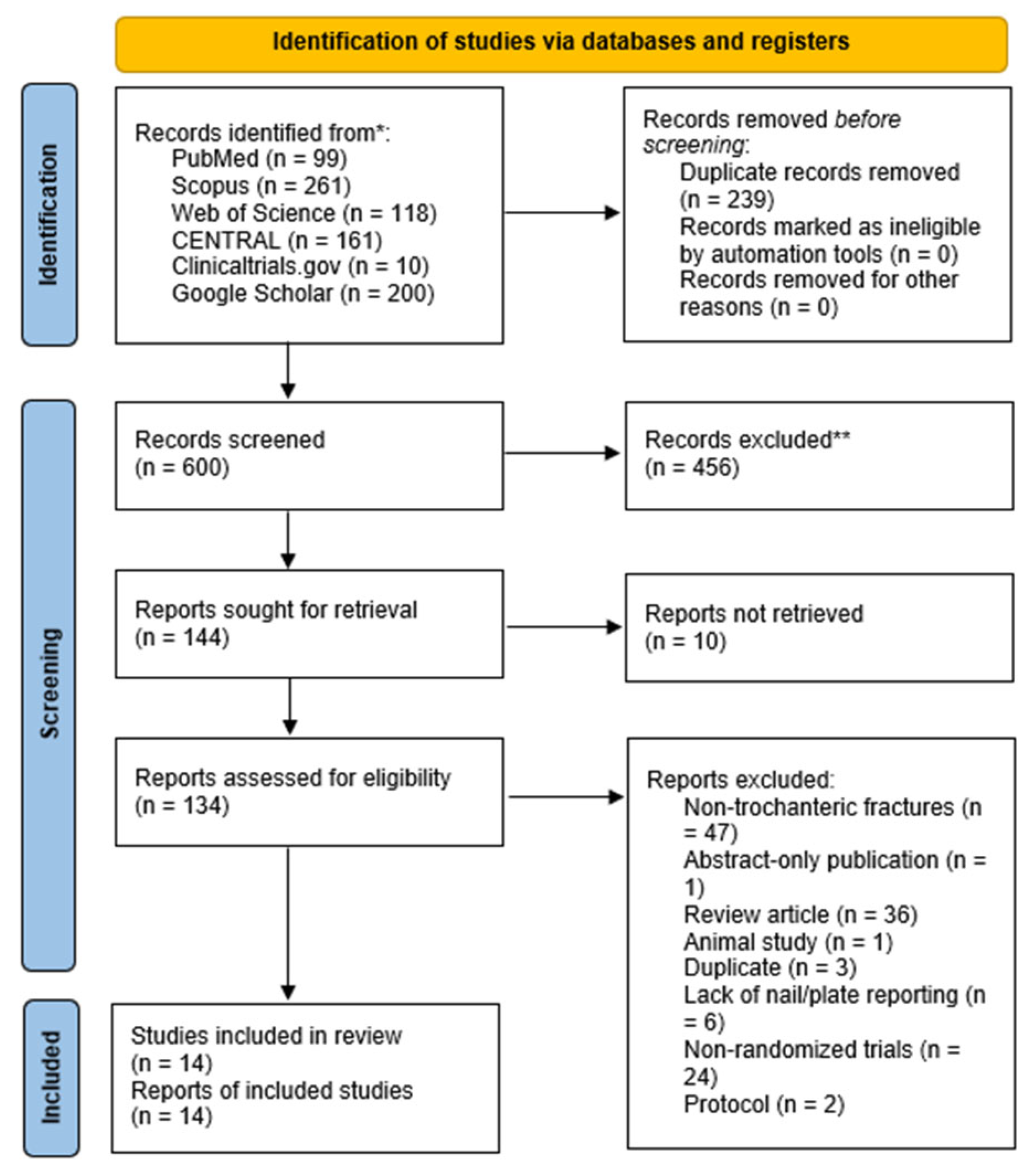
3.1. Literature Review Results
3.2. Baseline Characteristics of Included RCTs
3.3. Risk of Bias Assessment
3.4. Primary Outcomes
3.4.1. Reoperation Rate
3.4.2. Union Time (Months)
3.4.3. Implant Cut-Out
3.4.4. Complications and Mortality
3.5. Perioperative Outcomes
3.5.1. Operative Time
3.5.2. Fluoroscopy Time
3.5.3. Perioperative Blood Loss
3.5.4. Need for Blood Transfusion
3.5.5. Length of Hospital Stay
3.6. Functional and Anatomical Outcomes
3.6.1. Harris Hip Score
3.6.2. Hip Range of Motion (ROM)
3.6.3. Shortening
3.7. Implant-Related Complications
Additional Perioperative Fractures/Fissures
4. Discussion
4.1. Strengths and Limitations
4.2. Clinical Implications and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AVN | Avascular necrosis |
| CI | Confidence interval |
| DVT | Deep vein thrombosis |
| FU | Follow-up |
| IMN | Intramedullary nailing |
| I2 | Measure of heterogeneity |
| LD | Linear dichroism |
| MD | Mean difference |
| MDPI | Multidisciplinary Digital Publishing Institute |
| OR | Odds ratio |
| PF | Plate fixation |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RCT | Randomized controlled trial |
| RoB 2.0 | Revised Cochrane Risk of Bias tool for Randomized Trials |
| ROM | Range of motion |
| SD | Standard deviation |
| TLA | Three-letter acronym |
References
- Wu, J.; Che, Y.; Zhang, Y.; Wang, J.; Chen, M.; Jiang, J.; Jiang, Q.; Zhou, Y. Global, regional, national trends of femur fracture and machine learning prediction: Comprehensive findings and questions from global burden of disease 1990–2019. J. Orthop. Transl. 2024, 46, 46–52. [Google Scholar] [CrossRef]
- Saita, Y.; Ishijima, M.; Mogami, A.; Kubota, M.; Baba, T.; Kaketa, T.; Nagao, M.; Sakamoto, Y.; Sakai, K.; Kato, R. The fracture sites of atypical femoral fractures are associated with the weight-bearing lower limb alignment. Bone 2014, 66, 105–110. [Google Scholar] [CrossRef]
- Ricci, W.M.; Gallagher, B.; Haidukewych, G.J. Intramedullary nailing of femoral shaft fractures: Current concepts. JAAOS-J. Am. Acad. Orthop. Surg. 2009, 17, 296–305. [Google Scholar] [CrossRef]
- Lodde, M.; Raschke, M.; Stolberg-Stolberg, J.; Everding, J.; Rosslenbroich, S.; Katthagen, J. Union rates and functional outcome of double plating of the femur: Systematic review of the literature. Arch. Orthop. Trauma Surg. 2022, 142, 1009–1030. [Google Scholar] [CrossRef]
- Mavrogenis, A.F.; Panagopoulos, G.N.; Megaloikonomos, P.D.; Igoumenou, V.G.; Galanopoulos, I.; Vottis, C.T.; Karabinas, P.; Koulouvaris, P.; Kontogeorgakos, V.A.; Vlamis, J. Complications after hip nailing for fractures. Orthopedics 2016, 39, e108–e116. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Bierrum, W.; Wormald, J.; Ramachandran, M.; Firth, G.; Eastwood, D. Plate fixation versus flexible intramedullary nails for management of closed femoral shaft fractures in the pediatric population: A systematic review and meta-analysis of the adverse outcomes. J. Child. Orthop. 2023, 17, 442–452. [Google Scholar] [CrossRef] [PubMed]
- Saad, A.; Iyengar, K.; Vaishya, R.; Botchu, R. The incidence and management of isolated greater trochanteric fractures—A systematic review of 166 cases. J. Clin. Orthop. Trauma 2021, 21, 101537. [Google Scholar] [CrossRef] [PubMed]
- Joglekar, S.B.; Lindvall, E.M.; Martirosian, A. Contemporary management of subtrochanteric fractures. Orthop. Clin. 2015, 46, 21–35. [Google Scholar] [CrossRef]
- Kaplan, K.; Miyamoto, R.; Levine, B.R.; Egol, K.A.; Zuckerman, J.D. Surgical management of hip fractures: An evidence-based review of the literature. II: Intertrochanteric fractures. JAAOS-J. Am. Acad. Orthop. Surg. 2008, 16, 665–673. [Google Scholar] [CrossRef]
- Chinoy, M.; Parker, M. Fixed nail plates versus sliding hip systems for the treatment of trochanteric femoral fractures: A meta analysis of 14 studies. Injury 1999, 30, 157–163. [Google Scholar] [CrossRef]
- Hao, Z.; Wang, X.; Zhang, X. Comparing surgical interventions for intertrochanteric hip fracture by blood loss and operation time: A network meta-analysis. J. Orthop. Surg. Res. 2018, 13, 157. [Google Scholar] [CrossRef]
- Hu, L.; Xiong, Y.; Mi, B.; Panayi, A.C.; Zhou, W.; Liu, Y.; Liu, J.; Xue, H.; Yan, C.; Abududilibaier, A. Comparison of intramedullary nailing and plate fixation in distal tibial fractures with metaphyseal damage: A meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2019, 14, 30. [Google Scholar] [CrossRef]
- Donovan, R.L.; Harries, L.; Whitehouse, M.R. Flexible nails have a significantly increased risk of complications compared with plating techniques when treating diaphyseal femoral fractures in children aged 5–12: A systematic review. Injury 2020, 51, 2763–2770. [Google Scholar] [CrossRef] [PubMed]
- Neradi, D.; Sodavarapu, P.; Jindal, K.; Kumar, D.; Kumar, V.; Goni, V. Locked plating versus retrograde intramedullary nailing for distal femur fractures: A systematic review and meta-analysis. Arch. Bone Jt. Surg. 2022, 10, 141. [Google Scholar] [PubMed]
- Strait, R.T.; Pankey, C. Submuscular plating versus elastic intramedullary nailing in children with femoral shaft fracture; A systematic review and meta-analysis. J. Clin. Orthop. Trauma 2023, 42, 102203. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, S.; Rajnish, R.K.; Kumar, P.; Srivastava, A.; Rathor, K.; Haq, R.U. Comparison of outcomes of retrograde intramedullary nailing versus locking plate fixation in distal femur fractures: A systematic review and meta-analysis of 936 patients in 16 studies. J. Orthop. 2023, 36, 36–48. [Google Scholar] [CrossRef]
- Parker, M.; Raval, P.; Gjertsen, J.-E. Nail or plate fixation for A3 trochanteric hip fractures: A systematic review of randomised controlled trials. Injury 2018, 49, 1319–1323. [Google Scholar] [CrossRef]
- Parker, M.J. Sliding hip screw versus intramedullary nail for trochanteric hip fractures; a randomised trial of 1000 patients with presentation of results related to fracture stability. Injury 2017, 48, 2762–2767. [Google Scholar] [CrossRef]
- Parker, M.J.; Cawley, S. Sliding hip screw versus the Targon PFT nail for trochanteric hip fractures: A randomised trial of 400 patients. Bone Jt. J. 2017, 99, 1210–1215. [Google Scholar] [CrossRef]
- Chen, Z.; Han, D.; Wang, Q.; Li, L. Four interventions for pediatric femoral shaft fractures: Network meta-analysis of randomized trials. Int. J. Surg. 2020, 80, 53–60. [Google Scholar] [CrossRef]
- Muka, T.; Glisic, M.; Milic, J.; Verhoog, S.; Bohlius, J.; Bramer, W.; Chowdhury, R.; Franco, O.H. A 24-step guide on how to design, conduct, and successfully publish a systematic review and meta-analysis in medical research. Eur. J. Epidemiol. 2020, 35, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Abu Serhan, H.; Abdelaal, A.; Abuawwad, M.T.; Taha, M.J.; Irshaidat, S.; Abu Serhan, L.; Abu-Ismail, L.; Abu Salim, Q.F.; Abdelazeem, B.; Elnahry, A.G. Ocular vascular events following COVID-19 vaccines: A systematic review. Vaccines 2022, 10, 2143. [Google Scholar] [CrossRef] [PubMed]
- Aune, A.K.E.; Ødegaard, A.; Grøgaard, B.; Alho, A.B. Gamma nail vs. compression screw for trochanteric femoral fractures: 15 reoperations in a prospective, randomized study of 378 patients. Acta Orthop. Scand. 1994, 65, 127–130. [Google Scholar] [CrossRef]
- Bretherton, C.P.P.; Martyn, J. Femoral medialization, fixation failures, and functional outcome in trochanteric hip fractures treated with either a sliding hip screw or an intramedullary nail from within a randomized trial. J. Orthop. Trauma 2016, 30, 642–646. [Google Scholar] [CrossRef]
- Dujardin, F.H.; Benez, C.; Polle, G.; Alain, J.; Biga, N.; Thomine, J.M. Prospective randomized comparison between a dynamic hip screw and a mini-invasive static nail in fractures of the trochanteric area: Preliminary results. J. Orthop. Trauma 2001, 15, 401–406. [Google Scholar] [CrossRef]
- Kam, N.K.; Jain, A.; Nepal, P.; Singh, M.P.; Das, N. A prospective randomized control trial comparing proximal femoral nail and sliding hip screw in the management of trochanteric fracture of the femur. Health Renaiss. 2011, 9, 7–11. [Google Scholar] [CrossRef][Green Version]
- Kassem, E.; Younan, R.; Abaskhron, M.; Abo-Elsoud, M. Functional and radiological outcomes of dynamic hip screw with trochanteric stabilizing plate versus short proximal femoral nail in management of unstable trochanteric fractures: A randomized-controlled trial. Jt. Dis. Relat. Surg. 2022, 33, 531–537. [Google Scholar] [CrossRef]
- Parker, M.J.; Bowers, T.R.; Pryor, G.A. Sliding hip screw versus the Targon PF nail in the treatment of trochanteric fractures of the hip: A randomised trial of 600 fractures. J. Bone Jt. Surg. Br. Vol. 2012, 94, 391–397. [Google Scholar] [CrossRef]
- Schemitsch, E.H.; Nowak, L.L.; Schulz, A.P.; Brink, O.; Poolman, R.W.; Mehta, S.; Stengel, D.; Zhang, C.Q.; Martinez, S.; Kinner, B.; et al. Intramedullary nailing vs sliding hip screw in trochanteric fracture management: The INSITE randomized clinical trial. JAMA Netw. Open 2023, 6, e2317164. [Google Scholar] [CrossRef]
- Singh, A.K.; Nidhi, N.; Arun, G.R.; Srivastava, V. Treatment of Unstable Trochanteric Femur Fractures: Proximal Femur Nail Versus Proximal Femur Locking Compression Plate. Am. J. Orthop. 2017, 46, E116–E123. [Google Scholar]
- Stark, A.; Broström, L.Å.; Barrios, C.; Walheim, G.; Olsson, E. A prospective randomized study of the use of sliding hip screws and Ender nails for trochanteric fractures of the femur. Int. Orthop. 1992, 16, 359–362. [Google Scholar] [CrossRef]
- Utrilla, A.L.; Reig, J.S.; Muñoz, F.M.; Tufanisco, C.B. Trochanteric gamma nail and compression hip screw for trochanteric fractures: A randomized, prospective, comparative study in 210 elderly patients with a new design of the gamma nail. J. Orthop. Trauma 2005, 19, 229–233. [Google Scholar] [CrossRef]
- Zehir, S.; Zehir, R.; Zehir, S.; Azboy, İ.; Haykir, N. Proximal femoral nail antirotation against dynamic hip screw for unstable trochanteric fractures; a prospective randomized comparison. Eur. J. Trauma Emerg. Surg. 2015, 41, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Zou, J.; Xu, Y.; Yang, H. A comparison of proximal femoral nail antirotation and dynamic hip screw devices in trochanteric fractures. J. Int. Med. Res. 2009, 37, 1057–1064. [Google Scholar] [CrossRef] [PubMed]
- Schipper, I.; Marti, R.; Van der Werken, C. Unstable trochanteric femoral fractures: Extramedullary or intramedullary fixation: Review of literature. Injury 2004, 35, 142–151. [Google Scholar] [CrossRef] [PubMed]
- Alm, C.E.; Gjertsen, J.-E.; Basso, T.; Matre, K.; Rörhl, S.; Madsen, J.E.; Frihagen, F. Trochanteric stabilizing plate in the treatment of trochanteric fractures: A scoping review. Acta Orthop. 2021, 92, 733–738. [Google Scholar] [CrossRef]
- Norris, R.; Bhattacharjee, D.; Parker, M.J. Occurrence of secondary fracture around intramedullary nails used for trochanteric hip fractures: A systematic review of 13,568 patients. Injury 2012, 43, 706–711. [Google Scholar] [CrossRef]
- Xie, H.; Xie, L.; Wang, J.; Chen, C.; Zhang, C.; Zheng, W. Intramedullary versus extramedullary fixation for the treatment of subtrochanteric fracture: A systematic review and meta-analysis. Int. J. Surg. 2019, 63, 43–57. [Google Scholar] [CrossRef]
- Elgammal, A.I.; Zein, A.B.; Kholeif, A.; Mohamed, M.M.A.; Yafawi, B.E.; Amr, S. Outcomes of Retrograde Intramedullary Nail Versus Locked Compression Plate in Fixation of Extraarticular Distal Femur Fracture: A Prospective Non Blinded Randomized Controlled Study. NeuroQuantology 2022, 20, 2589–2598. [Google Scholar] [CrossRef]
- Kuzyk, P.R.; Bhandari, M.; McKee, M.D.; Russell, T.A.; Schemitsch, E.H. Intramedullary versus extramedullary fixation for subtrochanteric femur fractures. J. Orthop. Trauma 2009, 23, 465–470. [Google Scholar] [CrossRef]
- Van Knegsel, K.P.; Ganse, B.; Haefeli, P.C.; Migliorini, F.; Scaglioni, M.F.; van de Wall, B.J.; Kim, B.-S.; Link, B.-C.; Beeres, F.J.; Nebelung, S. Trochanteric femur fractures: Application of skeletal traction during surgery does not alter soft-tissue microcirculation. Medicina 2021, 57, 884. [Google Scholar] [CrossRef]




| Author (YOP) | Design | Country | Stability | Sample | AO/OTA | Nailing | Plating | Gender (M/F) | Age; Mean (SD) | FU (mo) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stable/Unstable | Nail | Plate | Nail (M) | Nail (F) | Plate (M) | Plate (F) | Nail | Plate | |||||||||
| Aune (1994) [23] | RCT | Norway | Stable/Unstable | 175 | 203 | - | Gamma nail | Compression screw | 66 | 109 | 89 | 114 | 82 | 49–96 | 78 | 45–93 | 3 |
| Bretherton (2016) [24] | RCT | UK | Unstable | 266 | 272 | A1, A2, A3 | Intramedullary nail | Sliding hip screw | 48 | 218 | 54 | 218 | 81.3 | 42–104 | 80.1 | 31–103 | 1.5 |
| Dujardin (2001) [25] | RCT | France | Stable/Unstable | 30 | 30 | - | Mini-invasive static nail | Dynamic hip screw | 6 | 24 | 6 | 24 | 83 | 9.4 | 84 | 6.2 | 6 |
| Karn (2011) [26] | RCT | Nepal | Stable/Unstable | 30 | 30 | - | Proximal femoral nail | Sliding hip screw | 18 | 12 | 12 | 18 | 66.56 | 53–100 | 67.8 | 50–87 | 6 |
| Kassem (2022) [27] | RCT | Egypt | Unstable | 34 | 34 | A2 | Proximal femoral nail | Dynamic hip screw | - | - | - | - | 70.8 | 7.7 | 68.7 | 8.7 | 12 |
| Parker (2012) [28] | RCT | UK | Stable/Unstable | 300 | 300 | B2.1, A1, A2, A3 | Targon Proximal femoral nail | Sliding hip screw | 52 | 248 | 69 | 231 | 82.4 | 26–104 | 81.4 | 27–104 | 12 |
| Parker (2017a) [18] | RCT | UK | Stable/Unstable | 500 | 500 | A1, A2, A3 | Intramedullary nail | Sliding hip screw | 112 | 388 | 116 | 384 | 82.2 | 26–104 | 82.1 | 25–105 | 2 |
| Parker (2017b) [19] | RCT | UK | Stable/Unstable | 200 | 200 | A1, A2, A3 | Targon Proximal femoral nail | Sliding hip screw | 60 | 140 | 47 | 153 | 82 | 36–101 | 83.2 | 25–105 | 12 |
| Schemitsch (2023) [29] | RCT | 12 countries | Stable/Unstable | 418 | 415 | A1, A2 | Intramedullary nail | Sliding hip screw | 153 | 265 | 138 | 277 | 78.2 | 26–102 | 78.8 | 18–100 | 12 |
| Singh (2017) [30] | RCT | India | Unstable | 23 | 22 | A2, A3 | Proximal femoral nail | Locking compression plate | 9 | 14 | 7 | 15 | 58.3 | 9.3 | 60.5 | 8.1 | 24 |
| Stark (1992) [31] | RCT | Sweden | Stable/Unstable | 36 | 56 | - | Ender nails | Sliding hip screw | 12 | 24 | 17 | 39 | 74 | - | 75 | - | 6 |
| Utrilla (2005) [32] | RCT | Spain | Stable/Unstable | 104 | 106 | - | Gamma nail | Compression hip screw | 38 | 66 | 78 | 28 | 80.6 | 7.5 | 79.8 | 7.3 | 12 |
| Zehir (2015) [33] | RCT | Turkey | Unstable | 96 | 102 | A2 | Proximal femoral nail anti-rotation | Dynamic hip screw | 37 | 59 | 39 | 63 | 77.22 | 6.82 | 76.86 | 6.74 | 6 |
| Zou (2009) [34] | RCT | China | Stable/Unstable | 58 | 63 | A1, A2, A3 | Proximal femoral nail anti-rotation | Dynamic hip screw | - | - | - | - | - | - | - | - | 12 |
| Complication | Studies | OR | 95% CI | I2 (%) | p-Value for I2 |
|---|---|---|---|---|---|
| AVN | 3 | 0.49 | 0.08–2.94 | 0% | 0.37 |
| DVT | 4 | 1.18 | 0.64–2.19 | 0% | 1.00 |
| Deep infection | 8 | 0.24 | 0.08–0.73 | 0% | 1.00 |
| Heart failure | 2 | 0.54 | 0.15–1.98 | 24.04% | 0.25 |
| Hematoma | 3 | 0.44 | 0.11–1.74 | 0% | 0.95 |
| Infection (not classified) | 2 | 0.58 | 0.13–2.60 | 0% | 0.65 |
| Non-union | 4 | 1.44 | 0.39–5.35 | 0% | 0.9 |
| Pulmonary embolism | 2 | 1.36 | 0.30–6.14 | 0% | 0.84 |
| Pneumonia | 2 | 1.32 | 0.69–2.52 | 0% | 0.74 |
| Pressure ulcers | 2 | 1.03 | 0.55–1.92 | 0% | 0.83 |
| Superficial infection | 7 | 0.92 | 0.53–1.62 | 0% | 0.95 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mert, Ü.; Ghandour, M.; Khasawneh, M.Y.; Milicevic, F.; Al Zuabi, A.; Horst, K.; Hildebrand, F.; Bouillon, B.; Mahmoud, M.A.; Kabir, K. Intramedullary Nailing vs. Plate Fixation for Trochanteric Femoral Fractures: A Systematic Review and Meta-Analysis of Randomized Trials. J. Clin. Med. 2025, 14, 5492. https://doi.org/10.3390/jcm14155492
Mert Ü, Ghandour M, Khasawneh MY, Milicevic F, Al Zuabi A, Horst K, Hildebrand F, Bouillon B, Mahmoud MA, Kabir K. Intramedullary Nailing vs. Plate Fixation for Trochanteric Femoral Fractures: A Systematic Review and Meta-Analysis of Randomized Trials. Journal of Clinical Medicine. 2025; 14(15):5492. https://doi.org/10.3390/jcm14155492
Chicago/Turabian StyleMert, Ümit, Maher Ghandour, Moh’d Yazan Khasawneh, Filip Milicevic, Ahmad Al Zuabi, Klemens Horst, Frank Hildebrand, Bertil Bouillon, Mohamad Agha Mahmoud, and Koroush Kabir. 2025. "Intramedullary Nailing vs. Plate Fixation for Trochanteric Femoral Fractures: A Systematic Review and Meta-Analysis of Randomized Trials" Journal of Clinical Medicine 14, no. 15: 5492. https://doi.org/10.3390/jcm14155492
APA StyleMert, Ü., Ghandour, M., Khasawneh, M. Y., Milicevic, F., Al Zuabi, A., Horst, K., Hildebrand, F., Bouillon, B., Mahmoud, M. A., & Kabir, K. (2025). Intramedullary Nailing vs. Plate Fixation for Trochanteric Femoral Fractures: A Systematic Review and Meta-Analysis of Randomized Trials. Journal of Clinical Medicine, 14(15), 5492. https://doi.org/10.3390/jcm14155492






