Ultrasonographic Evaluation of Labor Patterns: A Prospective Cohort Study in Greece
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design
2.2. Sonographic Technique
2.3. Statistical Analysis
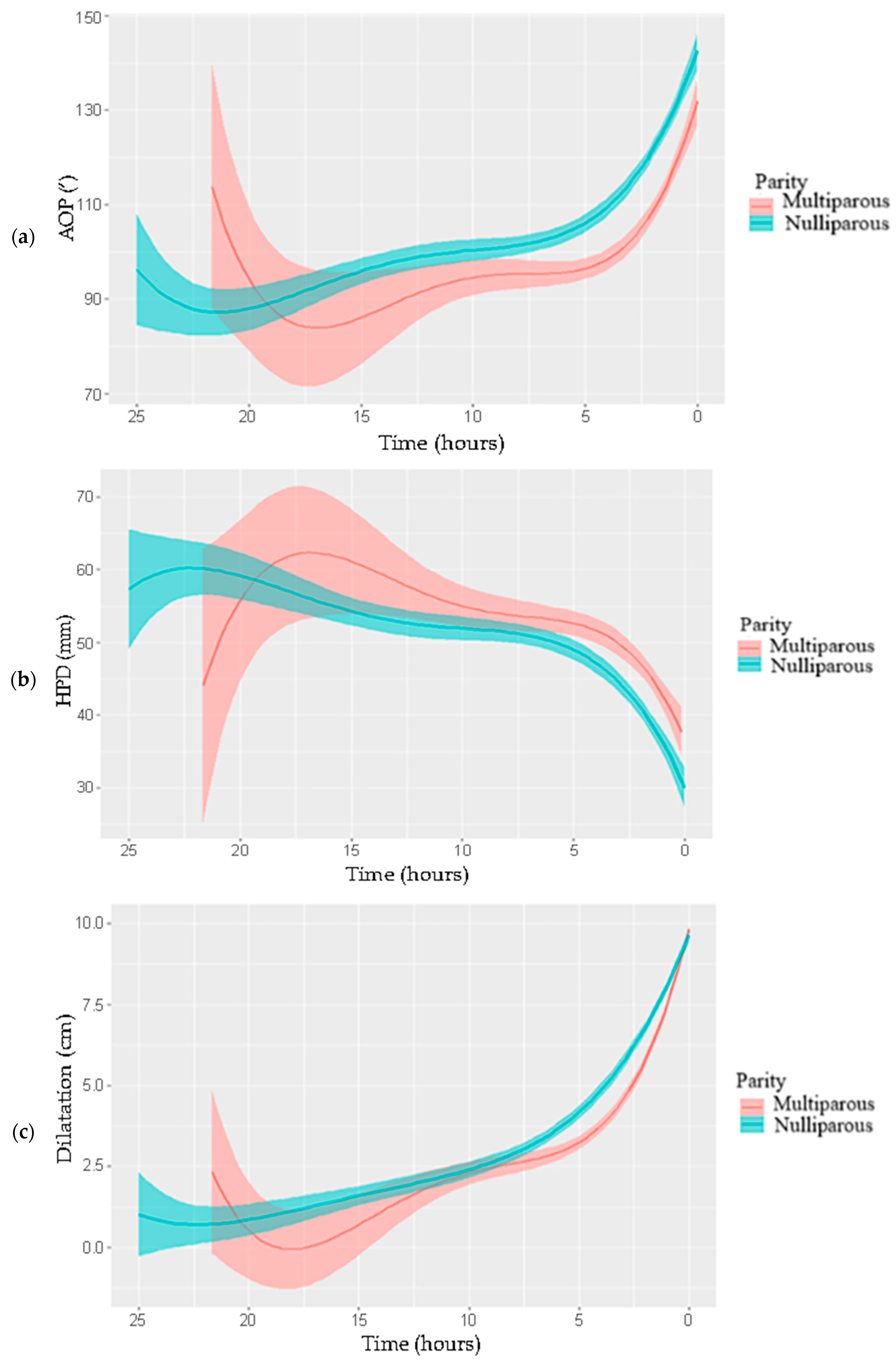
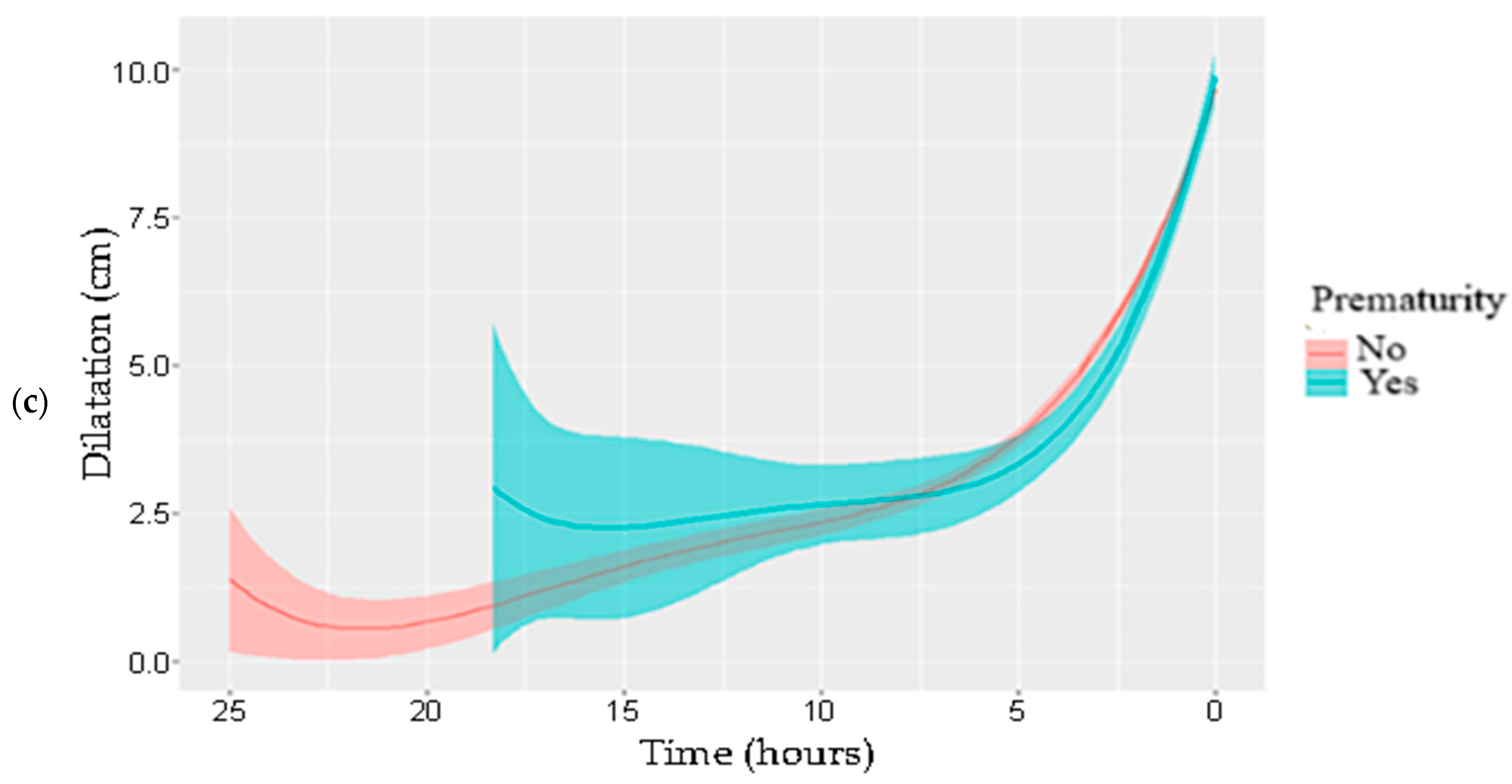
3. Results
3.1. Study Population
3.2. Labor Patterns
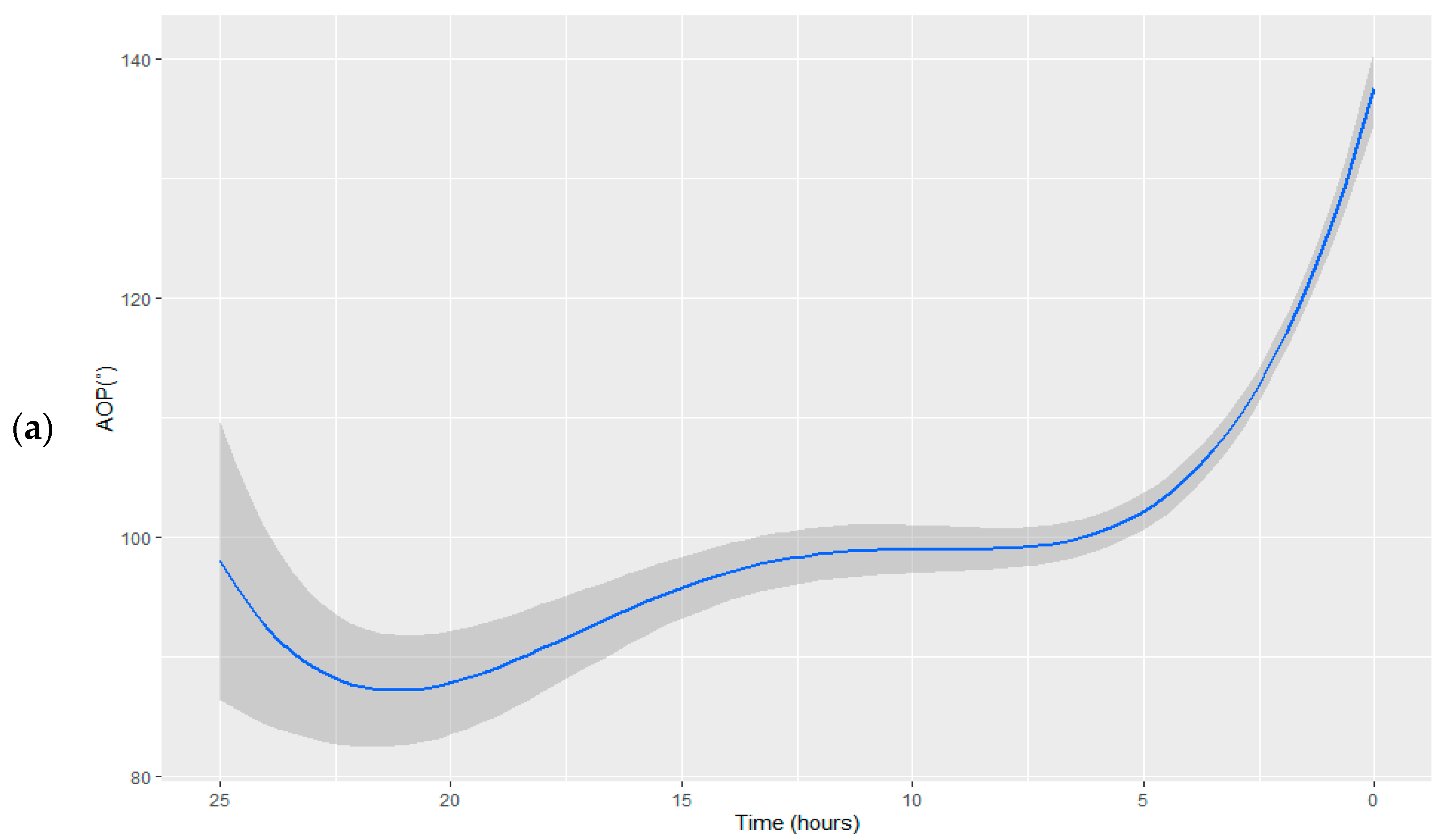
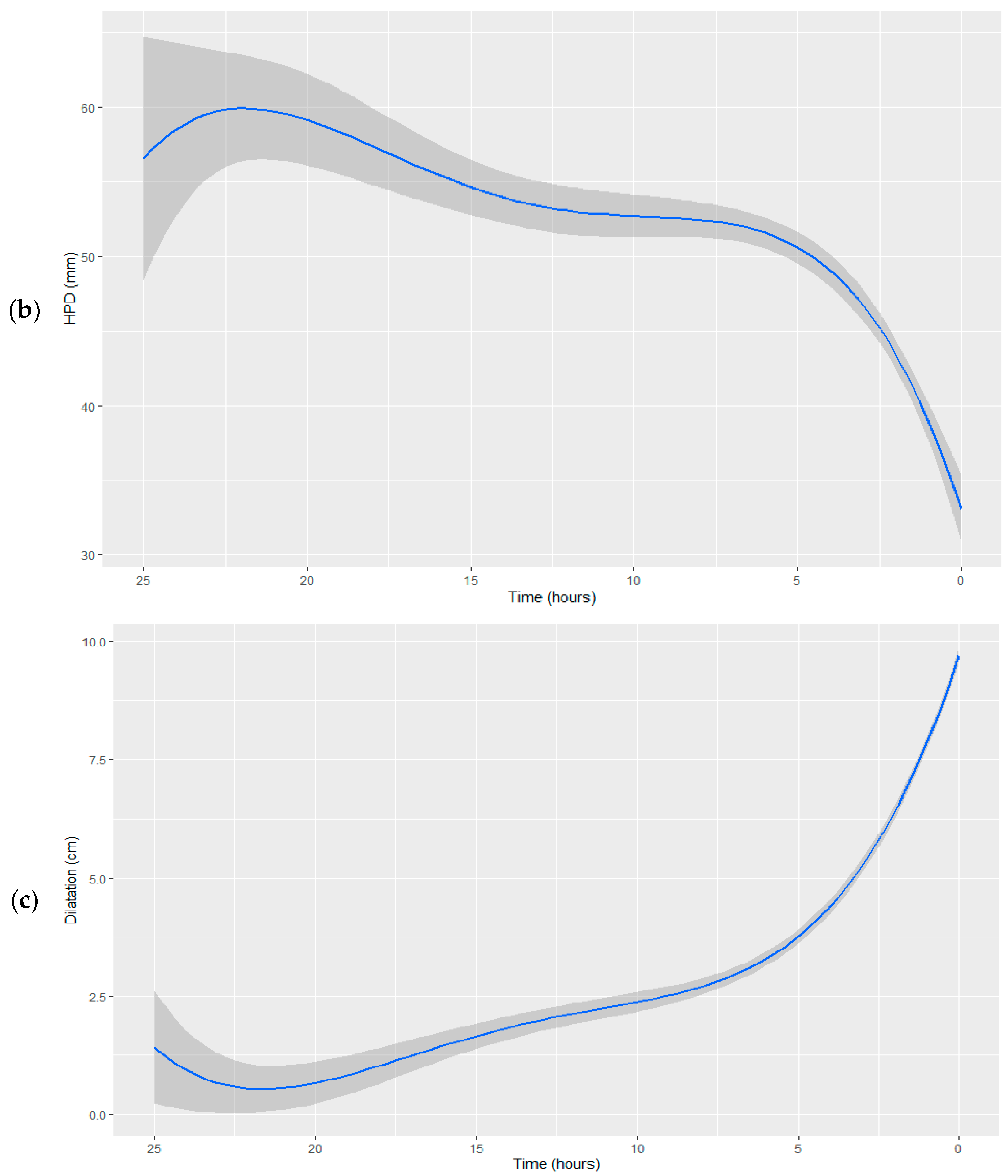
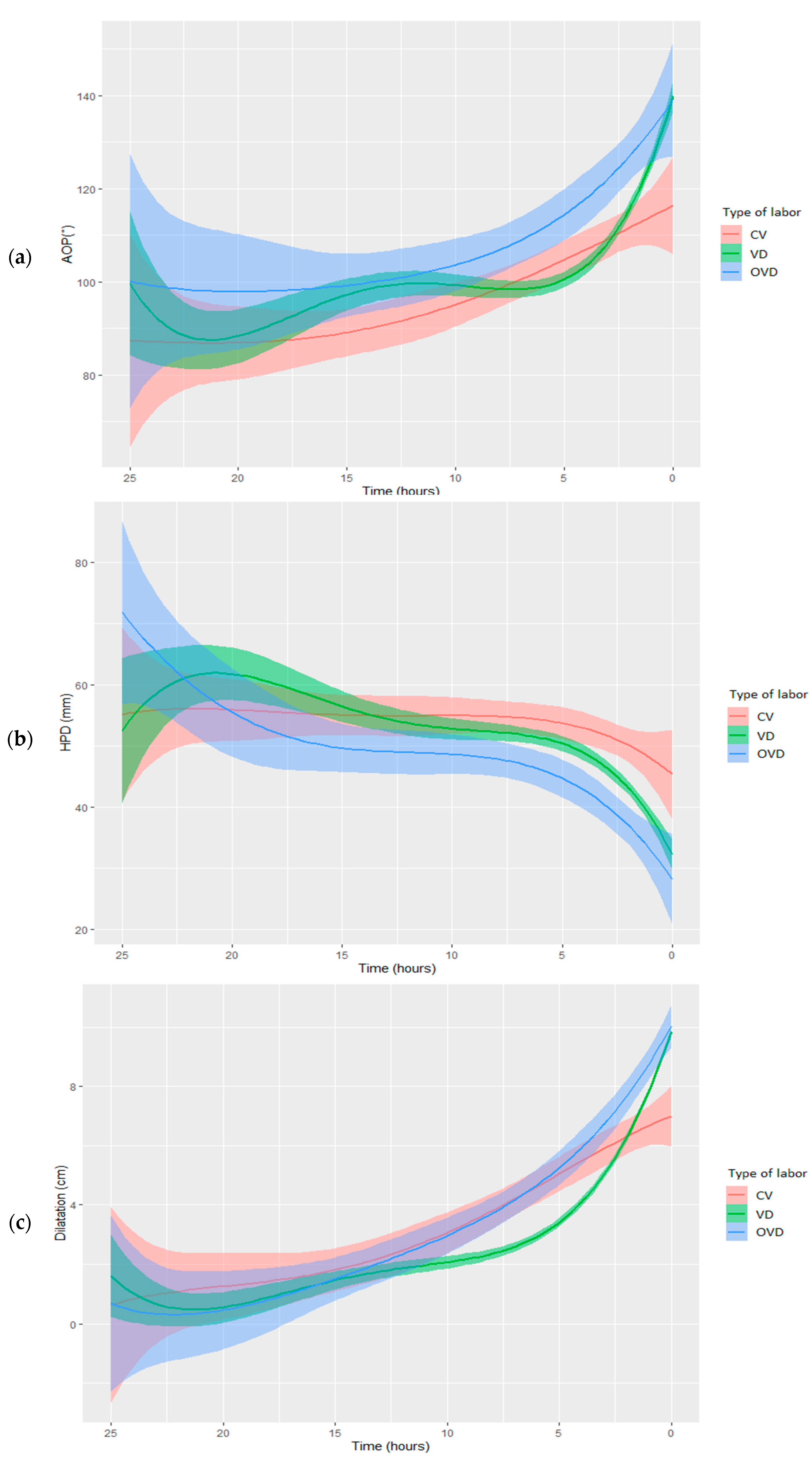
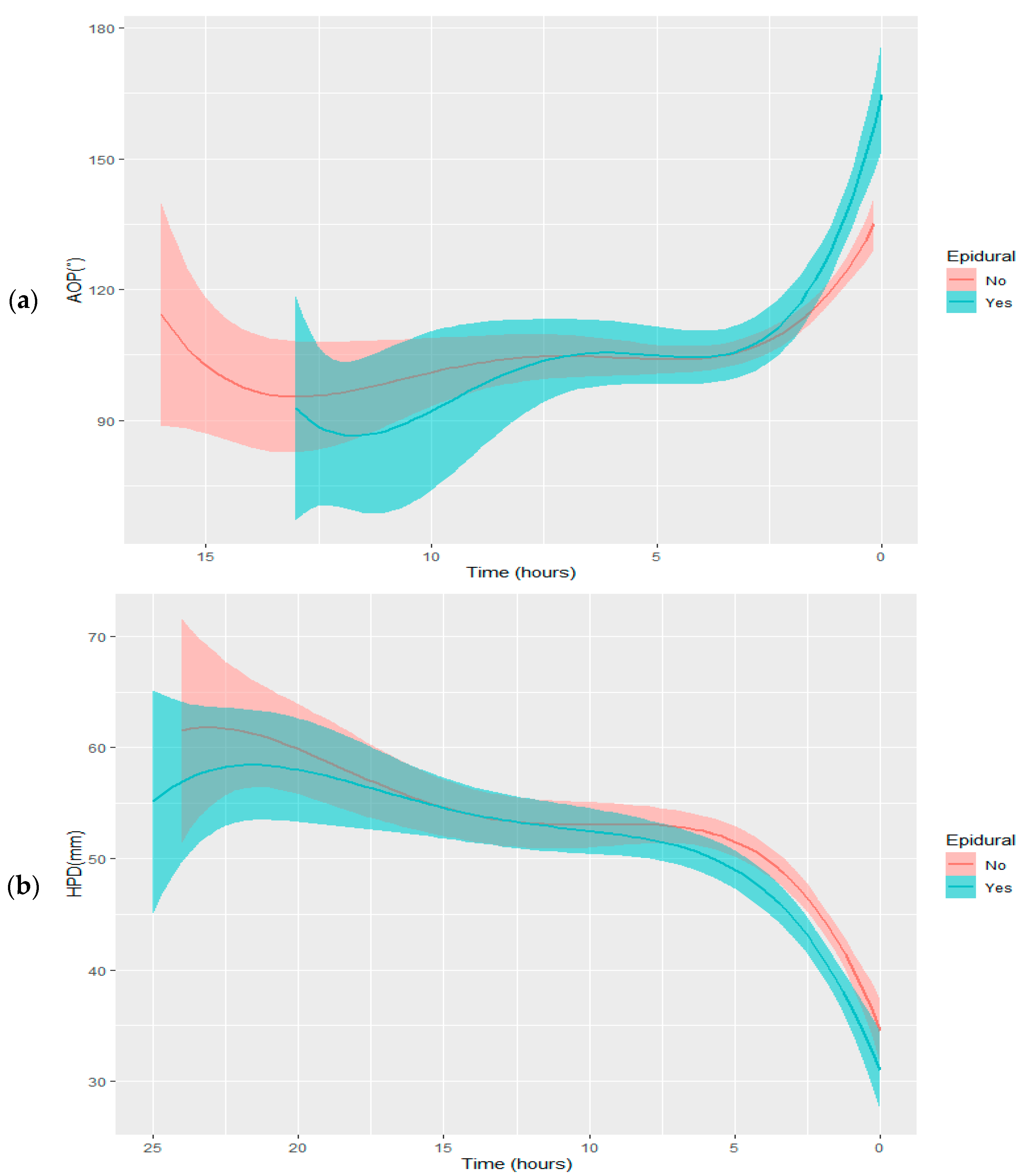
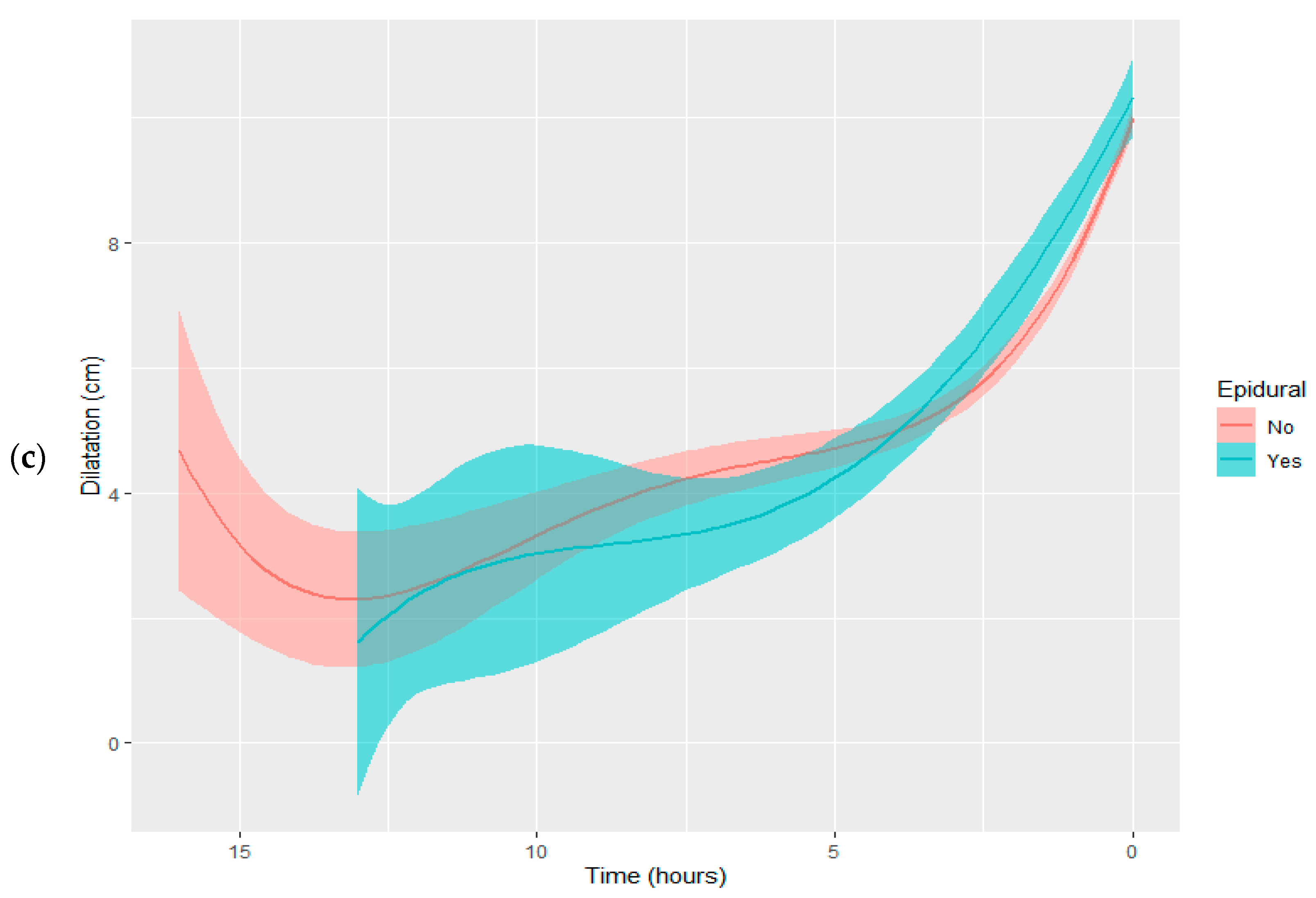
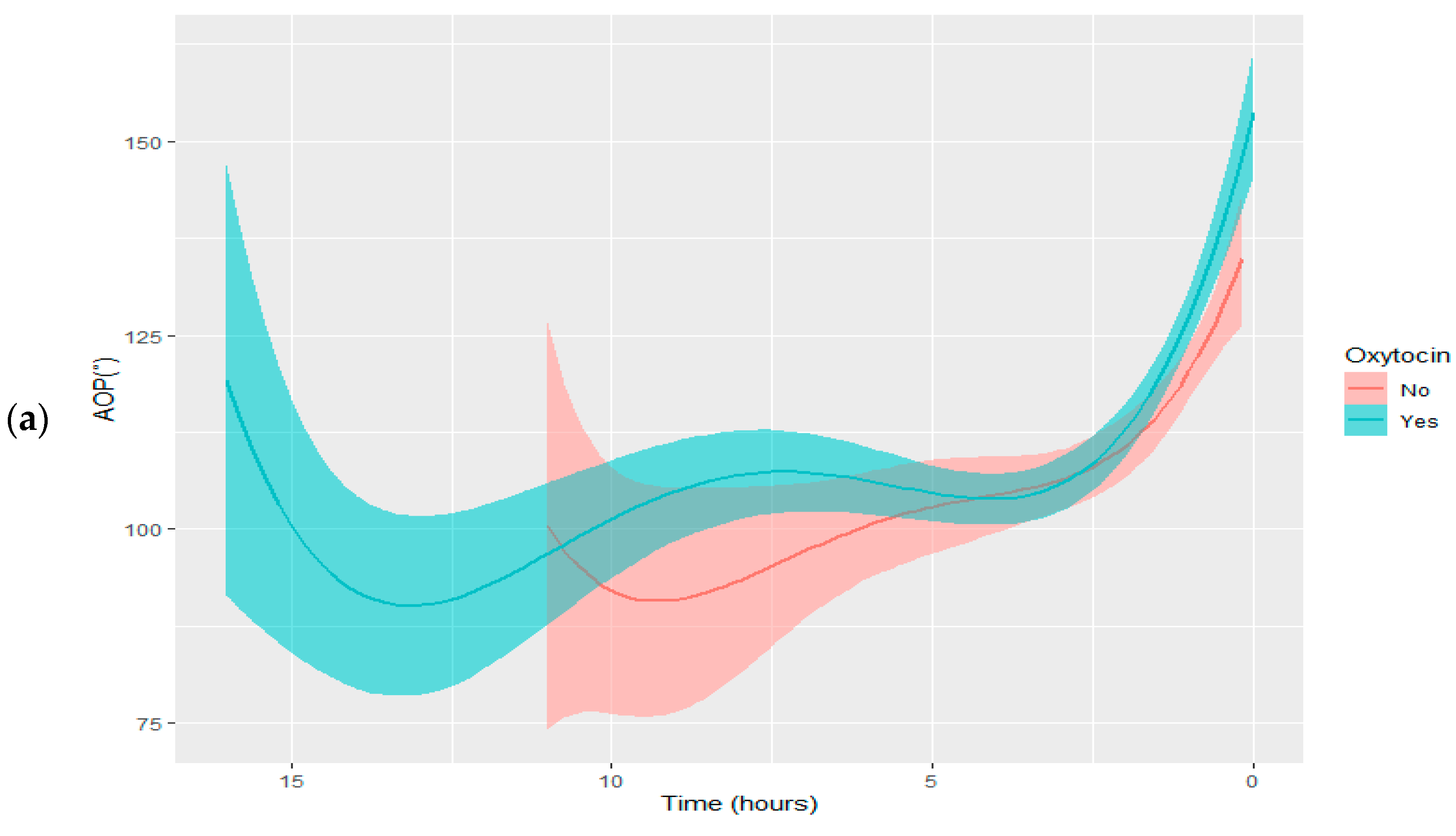
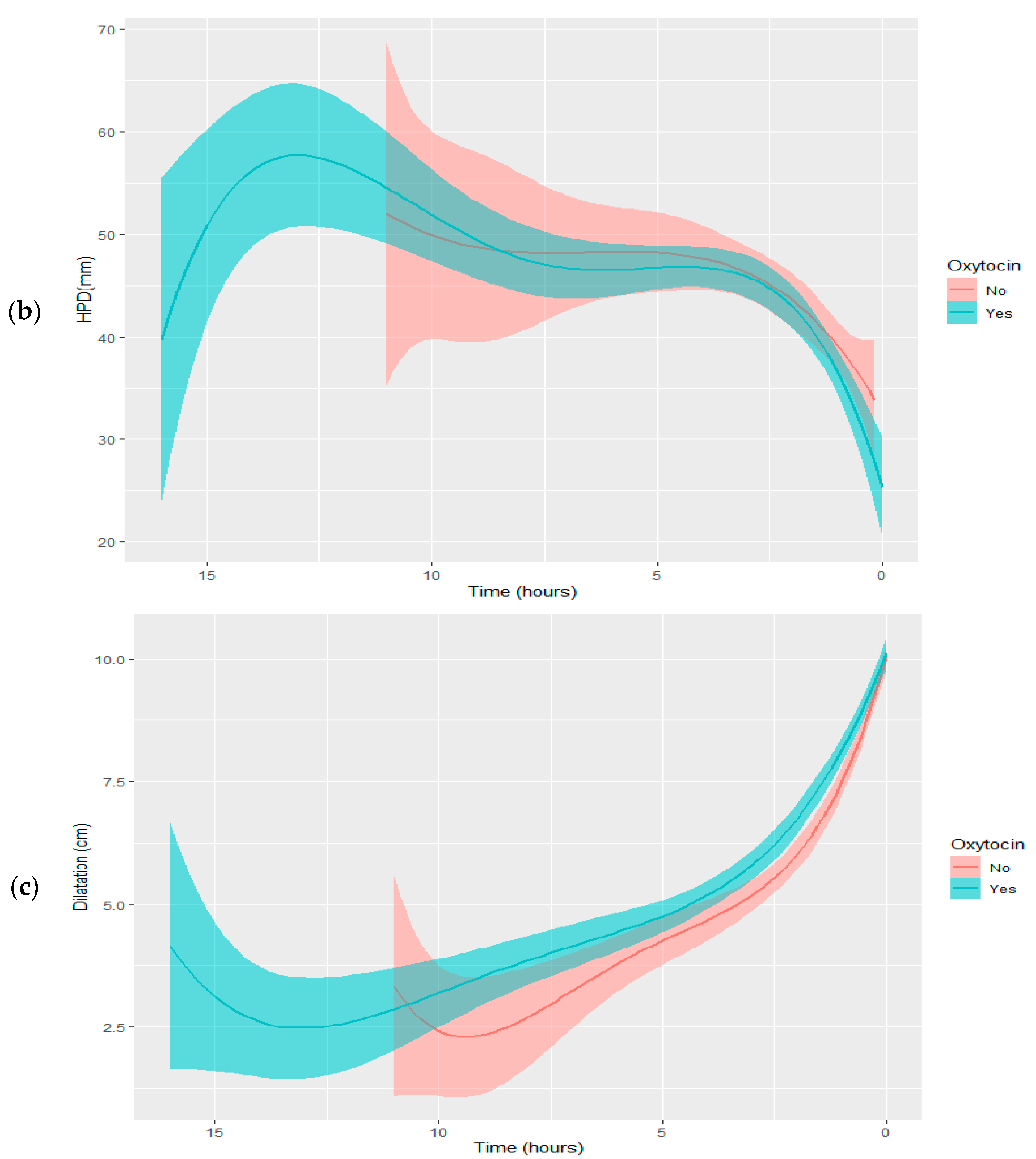
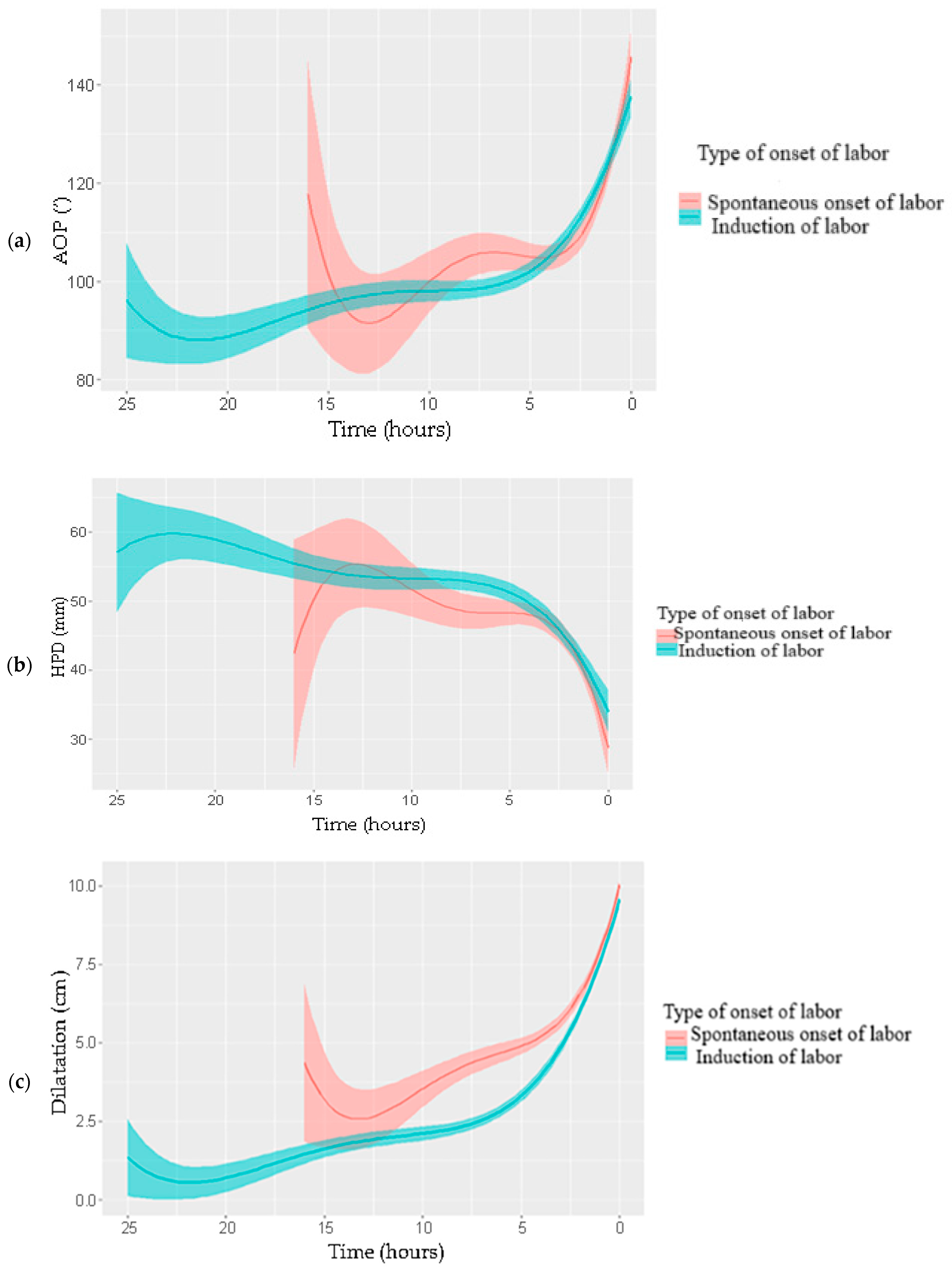
4. Discussion
4.1. Main Findings
4.2. Interpretation of the Findings
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Friedman, E.A. The labor curve. Clin. Perinatol. 1981, 8, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Troendle, J.F.; Yancey, M.K. Reassessing the labor curve in nulliparous women. Am. J. Obstet. Gynecol. 2002, 187, 824–828. [Google Scholar] [CrossRef] [PubMed]
- Souka, A.P.; Haritos, T.; Basayiannis, K.; Noikokyri, N.; Antsaklis, A. Intrapartum ultrasound for the examination of the fetal head position in normal and obstructed labor. J. Matern. Fetal Neonatal Med. 2003, 13, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Tutschek, B.; Torkildsen, E.A.; Eggebo, T.M. Comparison between ultrasound parameters and clinical examination to assess fetal head station in labor. Ultrasound Obstet. Gynecol. 2013, 41, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Duckelmann, A.M.; Bamberg, C.; Michaelis, S.A.; Lange, J.; Nonnenmacher, A.; Dudenhausen, J.W.; Kalache, K.D. Measurement of fetal head descent using the ‘angle of progression’ on transperineal ultrasound imaging is reliable regardless of fetal head station or ultrasound expertise. Ultrasound Obstet. Gynecol. 2010, 35, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Ghi, T.; Eggebo, T.; Lees, C.; Kalache, K.; Rozenberg, P.; Youssef, A.; Salomon, L.J.; Tutschek, B. ISUOG Practice Guidelines: Intrapartum ultrasound. Ultrasound Obstet. Gynecol. 2018, 52, 128–139. [Google Scholar] [CrossRef] [PubMed]
- Tsakiridis, I.; Mamopoulos, A.; Athanasiadis, A.; Dagklis, T. Induction of Labor: An Overview of Guidelines. Obstet. Gynecol. Surv. 2020, 75, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Tsakiridis, I.; Giouleka, S.; Mamopoulos, A.; Athanasiadis, A.; Daniilidis, A.; Dagklis, T. Operative vaginal delivery: A review of four national guidelines. J. Perinat. Med. 2020, 48, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Tutschek, B.; Braun, T.; Chantraine, F.; Henrich, W. A study of progress of labour using intrapartum translabial ultrasound, assessing head station, direction, and angle of descent. BJOG 2011, 118, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Barbera, A.F.; Pombar, X.; Perugino, G.; Lezotte, D.C.; Hobbins, J.C. A new method to assess fetal head descent in labor with transperineal ultrasound. Ultrasound Obstet. Gynecol. 2009, 33, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Eggebo, T.M.; Gjessing, L.K.; Heien, C.; Smedvig, E.; Okland, I.; Romundstad, P.; Salvesen, K.A. Prediction of labor and delivery by transperineal ultrasound in pregnancies with prelabor rupture of membranes at term. Ultrasound Obstet. Gynecol. 2006, 27, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Friedman, E.A.; Sachtleben, M.R. Station of the fetal presenting part: I. Pattern of descent. Am. J. Obstet. Gynecol. 1965, 93, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Hjartardottir, H.; Lund, S.H.; Benediktsdottir, S.; Geirsson, R.T.; Eggebo, T.M. Fetal descent in nulliparous women assessed by ultrasound: A longitudinal study. Am. J. Obstet. Gynecol. 2021, 224, 378.e1–378.e15. [Google Scholar] [CrossRef] [PubMed]
- Graseck, A.; Tuuli, M.; Roehl, K.; Odibo, A.; Macones, G.; Cahill, A. Fetal descent in labor. Obstet. Gynecol. 2014, 123, 521–526. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, E.F.; Simoneau, G.; Ciampi, A.; Warrick, P.; Collins, K.; Smith, S.; Garite, T.J. Descent of the fetal head (station) during the first stage of labor. Am. J. Obstet. Gynecol. 2016, 214, 360.e1–360.e6. [Google Scholar] [CrossRef] [PubMed]
- Tse, W.T.; Chaemsaithong, P.; Chan, W.W.Y.; Kwan, A.H.W.; Huang, J.; Appiah, K.; Chong, K.C.; Poon, L.C. Labor progress determined by ultrasound is different in women requiring cesarean delivery from those who experience a vaginal delivery following induction of labor. Am. J. Obstet. Gynecol. 2019, 221, 335.e1–335.e18. [Google Scholar] [CrossRef] [PubMed]
- Alexander, J.M.; Lucas, M.J.; Ramin, S.M.; McIntire, D.D.; Leveno, K.J. The course of labor with and without epidural analgesia. Am. J. Obstet. Gynecol. 1998, 178, 516–520. [Google Scholar] [CrossRef] [PubMed]
- Anim-Somuah, M.; Smyth, R.M.; Cyna, A.M.; Cuthbert, A. Epidural versus non-epidural or no analgesia for pain management in labour. Cochrane Database Syst. Rev. 2018, 5, CD000331. [Google Scholar] [CrossRef] [PubMed]
- Bofill, J.A.; Vincent, R.D.; Ross, E.L.; Martin, R.W.; Norman, P.F.; Werhan, C.F.; Morrison, J.C. Nulliparous active labor, epidural analgesia, and cesarean delivery for dystocia. Am. J. Obstet. Gynecol. 1997, 177, 1465–1470. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.; Carr, D.; Loyd, G.; Cook, V.; Spinnato, J. The influence of epidural analgesia on cesarean delivery rates: A randomized, prospective clinical trial. Am. J. Obstet. Gynecol. 1998, 179, 1527–1533. [Google Scholar] [CrossRef] [PubMed]
- Comparative Obstetric Mobile Epidural Trial Study Group UK. Effect of low-dose mobile versus traditional epidural techniques on mode of delivery: A randomised controlled trial. Lancet 2001, 358, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.S. Continuous lumbar epidural analgesia for labour and delivery. Br. Med. J. 1979, 1, 72–74. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Arya, V.K.; Gopalan, S.; Jain, V. Analgesic efficacy of intramuscular opioids versus epidural analgesia in labor. Int. J. Gynaecol. Obstet. 2003, 83, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Lewkowitz, A.K.; Tuuli, M.G.; Stout, M.J.; Woolfolk, C.; Roehl, K.; Macones, G.A.; Cahill, A.G. Epidurals and the Modern Labor Curve: How Epidural Timing Impacts Fetal Station during Active Labor. Am. J. Perinatol. 2018, 35, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Nageotte, M.P.; Larson, D.; Rumney, P.J.; Sidhu, M.; Hollenbach, K. Epidural analgesia compared with combined spinal-epidural analgesia during labor in nulliparous women. N. Engl. J. Med. 1997, 337, 1715–1719. [Google Scholar] [CrossRef] [PubMed]
- Ohel, G.; Gonen, R.; Vaida, S.; Barak, S.; Gaitini, L. Early versus late initiation of epidural analgesia in labor: Does it increase the risk of cesarean section? A randomized trial. Am. J. Obstet. Gynecol. 2006, 194, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Potter, N.; Macdonald, R.D. Obstetric consequences of epidural analgesia in nulliparous patients. Lancet 1971, 1, 1031–1034. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.K.; Alexander, J.M.; Messick, G.; Bloom, S.L.; McIntire, D.D.; Wiley, J.; Leveno, K.J. Cesarean delivery: A randomized trial of epidural analgesia versus intravenous meperidine analgesia during labor in nulliparous women. Anesthesiology 2002, 96, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Studd, J.W.; Crawford, J.S.; Duignan, N.M.; Rowbotham, C.J.; Hughes, A.O. The effect of lumbar epidural analgesia on the rate of cervical dilatation and the outcome of labour of spontaneous onset. Br. J. Obstet. Gynaecol. 1980, 87, 1015–1021. [Google Scholar] [CrossRef] [PubMed]
- Thorp, J.A.; Hu, D.H.; Albin, R.M.; McNitt, J.; Meyer, B.A.; Cohen, G.R.; Yeast, J.D. The effect of intrapartum epidural analgesia on nulliparous labor: A randomized, controlled, prospective trial. Am. J. Obstet. Gynecol. 1993, 169, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Mitta, K.; Tsakiridis, I.; Dagklis, T.; Kalogiannidis, I.; Mamopoulos, A.; Michos, G.; Virgiliou, A.; Athanasiadis, A. Ultrasonographic Evaluation of the Second Stage of Labor according to the Mode of Delivery: A Prospective Study in Greece. J. Clin. Med. 2024, 13, 1068. [Google Scholar] [CrossRef] [PubMed]
- Bjorklund, J.; Wiberg-Itzel, E.; Wallstrom, T. Is there an increased risk of cesarean section in obese women after induction of labor? A retrospective cohort study. PLoS ONE 2022, 17, e0263685. [Google Scholar] [CrossRef] [PubMed]
- Al-Kubaisy, W.; Al-Rubaey, M.; Al-Naggar, R.A.; Karim, B.; Mohd Noor, N.A. Maternal obesity and its relation with the cesarean section: A hospital based cross sectional study in Iraq. BMC Pregnancy Childbirth 2014, 14, 235. [Google Scholar] [CrossRef] [PubMed]
- Lundborg, L.; Aberg, K.; Sandstrom, A.; Liu, X.; Tilden, E.; Stephansson, O.; Ahlberg, M. Association between first and second stage of labour duration and mode of delivery: A population-based cohort study. Paediatr. Perinat. Epidemiol. 2022, 36, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Walsh, J.M.; Hehir, M.P.; Robson, M.S.; Mahony, R.M. Mode of delivery and outcomes by birth weight among spontaneous and induced singleton cephalic nulliparous labors. Int. J. Gynaecol. Obstet. 2015, 129, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Seyb, S.T.; Berka, R.J.; Socol, M.L.; Dooley, S.L. Risk of cesarean delivery with elective induction of labor at term in nulliparous women. Obstet. Gynecol. 1999, 94, 600–607. [Google Scholar] [CrossRef] [PubMed]
- Cammu, H.; Martens, G.; Ruyssinck, G.; Amy, J.J. Outcome after elective labor induction in nulliparous women: A matched cohort study. Am. J. Obstet. Gynecol. 2002, 186, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Vrouenraets, F.P.; Roumen, F.J.; Dehing, C.J.; van den Akker, E.S.; Aarts, M.J.; Scheve, E.J. Bishop score and risk of cesarean delivery after induction of labor in nulliparous women. Obstet. Gynecol. 2005, 105, 690–697. [Google Scholar] [CrossRef] [PubMed]
- Ehrenthal, D.B.; Jiang, X.; Strobino, D.M. Labor induction and the risk of a cesarean delivery among nulliparous women at term. Obstet. Gynecol. 2010, 116, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Maslow, A.S.; Sweeny, A.L. Elective induction of labor as a risk factor for cesarean delivery among low-risk women at term. Obstet. Gynecol. 2000, 95, 917–922. [Google Scholar] [CrossRef] [PubMed]
- Haberman, S.; Atallah, F.; Nizard, J.; Buhule, O.; Albert, P.; Gonen, R.; Ville, Y.; Paltieli, Y. A Novel Partogram for Stages 1 and 2 of Labor Based on Fetal Head Station Measured by Ultrasound: A Prospective Multicenter Cohort Study. Am. J. Perinatol. 2021, 38, e14–e20. [Google Scholar] [CrossRef] [PubMed]
- Bamberg, C.; Scheuermann, S.; Fotopoulou, C.; Slowinski, T.; Duckelmann, A.M.; Teichgraber, U.; Streitparth, F.; Henrich, W.; Dudenhausen, J.W.; Kalache, K.D. Angle of progression measurements of fetal head at term: A systematic comparison between open magnetic resonance imaging and transperineal ultrasound. Am. J. Obstet. Gynecol. 2012, 206, 161.e1–161.e5. [Google Scholar] [CrossRef] [PubMed]


| Type of Labor | p | |||||
|---|---|---|---|---|---|---|
| n = 500 | Total Sample | CS (n = 52; 10.4%) | OVD (n = 35; 7.0%) | VD (n = 413; 82.6%) | ||
| Maternal characteristics | ||||||
| Age (years), mean (SD) | 28.8 (6.5) | 30 (5.4) | 27.4 (6) | 28.7 (6.7) | 0.167 ‡ | |
| ΒΜΙ, mean (SD) | 30 (5.18) | 32.03 (5.6) | 29.94 (5.22) | 29.75 (5.08) | 0.011 ‡ | |
| Pregnancy- and labor- related characteristics | ||||||
| Gestational age (weeks), mean (SD) | 38.8 (1.5) | 38.9 (1.5) | 39.1 (1.3) | 38.8 (1.5) | 0.384 ‡ | |
| Preterm labor, n (%) | 44 (8.8) | 5 (9.6) | 3 (8.6) | 36 (8.7) | 0.951 ++ | |
| Nulliparous, n (%) | 286 (57.2) | 45 (86.5) | 33 (94.3) | 208 (50.4) | <0.001 + | |
| Epidural, n (%) | 181 (36.2) | 22 (42.3) | 17 (48.6) | 142 (34.4) | 0.153 + | |
| Oxytocin, n (%) | 329 (65.8) | 40 (76.9) | 27 (77.1) | 262 (63.4) | 0.050 + | |
| Labor onset, n (%) | ||||||
| Spontaneous | 201 (40.2) | 12 (23.1) | 10 (28.6) | 179 (43.3) | ||
| Induction | 299 (59.8) | 40 (76.9) | 25 (71.4) | 234 (56.7) | 0.007 + | |
| Total labor duration, median (IQR) | 8.3 (5–12) | 15 (10–21) | 12 (7–17) | 8 (5–12) | <0.001 ‡‡ | |
| Birth weight (gr), mean (SD) | 3131.69 (471.23) | 3267.88 (502.02) | 3266.86 (380.56) | 3103.09 (470.2) | 0.012 ‡ | |
| Type of Labor | p Kruskal–Wallis Test | p 1 Pairwise Comparisons | |||||
|---|---|---|---|---|---|---|---|
| CS | OVD | VD | |||||
| Median (IQR) | Median (IQR) | Median (IQR) | CS vs. OVD | CS vs. VD | OVD vs. VD | ||
| At first examination | |||||||
| AοP (°) | 92 (84–102.5) | 105 (89–113) | 101 (92–112) | <0.001 | 0.007 | <0.001 | 0.504 |
| HPD (mm) | 55 (51–61) | 50 (44–53) | 49 (42–55) | <0.001 | <0.001 | <0.001 | 0.917 |
| Dilatation (cm) | 1 (1–4) | 2 (1–4) | 3 (1–5) | <0.001 | 0.958 | 0.003 | 0.010 |
| At last examination | |||||||
| AοP (°) | 104.5 (93–126) | 118 (110–141) | 114 (101–129) | 0.002 | <0.001 | 0.009 | 0.029 |
| HPD (mm) | 49 (40–56) | 43.5 (29.5–49) | 43 (35.5–51) | 0.005 | 0.009 | 0.003 | 0.357 |
| Dilatation (cm) | 6 (3–10) | 10 (10–10) | 10 (10–10) | <0.001 | <0.001 | <0.001 | 0.763 |
| Dilatation | AοΡ (°) | HPD (mm) | |||
|---|---|---|---|---|---|
| Estimation | 95% CI | Estimation | 95% CI | ||
| Total sample | 4 cm | 102.6 | 101.1–104.0 | 50.1 | 49.0–51.1 |
| 5 cm | 105.6 | 104.0–107.2 | 48.6 | 47.3–49.8 | |
| 6 cm | 109.4 | 107.7–111.2 | 46.8 | 45.4–48.1 | |
| 7 cm | 113.9 | 112.0–115.8 | 44.8 | 43.3–46.2 | |
| 8 cm | 119.1 | 117.1–121.1 | 42.5 | 40.9–44.0 | |
| 9 cm | 125.1 | 122.9–127.3 | 40.0 | 38.3–41.7 | |
| 10 cm | 131.7 | 129.2–134.3 | 37.2 | 35.3–39.2 | |
| OVD/VD | 4 cm | 103.4 | 102.0–104.9 | 49.5 | 48.4–50.6 |
| 5 cm | 106.6 | 104.9–108.3 | 48.1 | 46.8–49.4 | |
| 6 cm | 110.5 | 108.6–112.5 | 46.4 | 44.9–47.8 | |
| 7 cm | 115.1 | 113.1–117.2 | 44.3 | 42.8–45.9 | |
| 8 cm | 120.5 | 118.3–122.7 | 42.0 | 40.3–43.7 | |
| 9 cm | 126.6 | 124.2–129.0 | 39.4 | 37.5–41.2 | |
| 10 cm | 133.4 | 130.6–136.2 | 36.4 | 34.3–38.5 | |
| CS | 4 cm | 95.4 | 91.3–99.4 | 54.1 | 51.8–56.4 |
| 5 cm | 97.1 | 92.7–101.5 | 52.6 | 50.2–55.0 | |
| 6 cm | 99.6 | 94.9–104.3 | 51.1 | 48.4–53.8 | |
| 7 cm | 103.0 | 98.1–107.9 | 49.6 | 46.6–52.6 | |
| 8 cm | 107.1 | 102.0–112.3 | 48.1 | 44.6–51.5 | |
| 9 cm | 112.1 | 106.5–117.6 | 46.6 | 42.6–50.5 | |
| 10 cm | 117.9 | 111.6–124.2 | 45.1 | 40.6–49.6 | |
| Predicted Time to Delivery (Hours) | 95% CI (Hours) | |
|---|---|---|
| AoP (°) | ||
| 78 | 9.01 | 8.50–9.51 |
| 80 | 8.76 | 8.27–9.25 |
| 84 | 8.27 | 7.81–8.72 |
| 85 | 8.14 | 7.70–8.59 |
| 95 | 6.90 | 6.52–7.28 |
| 99 | 6.41 | 6.05–6.77 |
| 110 | 5.05 | 4.71–5.39 |
| 113 | 4.68 | 4.34–5.02 |
| 116 | 4.31 | 3.96–4.66 |
| 120 | 3.81 | 3.45–4.18 |
| 125 | 3.19 | 2.80–3.59 |
| 138 | 1.59 | 1.09–2.08 |
| 140 | 1.33 | 0.83–1.85 |
| 148 | 0.35 | 0.00–0.93 |
| HPD (mm) | ||
| 60 | 7.55 | 7.09–8.00 |
| 54 | 6.46 | 6.08–6.84 |
| 50 | 5.73 | 5.38–6.09 |
| 48 | 5.37 | 5.02–5.72 |
| 40 | 3.92 | 3.53–4.30 |
| 38 | 3.55 | 3.15–3.96 |
| 37 | 3.37 | 2.96–3.79 |
| 36 | 3.19 | 2.77–3.62 |
| 35 | 3.01 | 2.57–3.45 |
| 30 | 2.10 | 1.58–2.62 |
| 20 | 0.29 | 0.00–0.99 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitta, K.; Tsakiridis, I.; Virgiliou, A.; Mamopoulos, A.; Capros, H.; Athanasiadis, A.; Dagklis, T. Ultrasonographic Evaluation of Labor Patterns: A Prospective Cohort Study in Greece. J. Clin. Med. 2025, 14, 5283. https://doi.org/10.3390/jcm14155283
Mitta K, Tsakiridis I, Virgiliou A, Mamopoulos A, Capros H, Athanasiadis A, Dagklis T. Ultrasonographic Evaluation of Labor Patterns: A Prospective Cohort Study in Greece. Journal of Clinical Medicine. 2025; 14(15):5283. https://doi.org/10.3390/jcm14155283
Chicago/Turabian StyleMitta, Kyriaki, Ioannis Tsakiridis, Andriana Virgiliou, Apostolos Mamopoulos, Hristiana Capros, Apostolos Athanasiadis, and Themistoklis Dagklis. 2025. "Ultrasonographic Evaluation of Labor Patterns: A Prospective Cohort Study in Greece" Journal of Clinical Medicine 14, no. 15: 5283. https://doi.org/10.3390/jcm14155283
APA StyleMitta, K., Tsakiridis, I., Virgiliou, A., Mamopoulos, A., Capros, H., Athanasiadis, A., & Dagklis, T. (2025). Ultrasonographic Evaluation of Labor Patterns: A Prospective Cohort Study in Greece. Journal of Clinical Medicine, 14(15), 5283. https://doi.org/10.3390/jcm14155283







