Physiotherapy in Prehabilitation for Bariatric Surgery—Analysis of Its Impact on Functional Capacity and Original Predictive Models of Functional Status Outcome
Abstract
1. Introduction
1.1. Treatment Methods for Obesity
1.2. Prehabilitation in Surgery
1.3. Prehabilitation in Bariatric Surgery
1.4. Aim and Hypotheses
- -
- -
- To formulate an original predictive linear model of functional status outcomes among patients awaiting bariatric surgery.
2. Materials and Methods
Specialized Care Program for Patients with Obesity
- -
- The preparation of the patient for bariatric surgery (including health condition counseling, diagnostic tests, and consultations);
- -
- Preoperative care, specifically a 3–6-month period of care provided by a multi-specialist team, including surgeons, specialists in internal medicine or diabetology, anesthesiologists, physiotherapists, psychologists, and dietitians;
- -
- The final qualification of the patient for bariatric surgery;
- -
- Surgery;
- -
- A follow-up visit after surgery, to be implemented within seven to 14 days after discharge.
- -
- BMI > 40;
- -
- Participation in the Specialized Care Program for Patients with Obesity;
- -
- Qualification for bariatric surgery.
- -
- Disqualification from the Specialized Care Program for Patients with Obesity;
- -
- Cancer (history or active);
- -
- Significant physical disability or a musculoskeletal disorder at the time of enrollment;
- -
- Serious medical conditions, such as myocardial infarction, stroke, acute heart failure, or pulmonary embolism within 30 days prior to study enrollment;
- -
- An inability to participate in outpatient physiotherapy.
- -
- A study group, including 30 patients who were given exercise-based physiotherapy during prehabilitation.
- -
- A control group, including 20 patients who were not given exercise-based physiotherapy during prehabilitation.
- 2.
- Assessment of activities of daily living: The Barthel mobility index.
- 3.
- Assessment of fatigue: The Borg Rating of Perceived Exertion (RPE) scale [25].
3. Results
3.1. First Assessment—Prior to Prehabilitation
3.2. Comparison of Results to Norms
3.3. Linear Models for 6MWT Results
4. Discussion
Limitations of This Study
5. Conclusions
- Exercise-based physiotherapy during prehabilitation was associated with improved functional capacity in patients being prepared for bariatric surgery.
- Exercise-based physiotherapy during prehabilitation can contribute to the improvement of distance travelled in the 6MWT, including in relation to norms and data in the literature.
- Exercise-based physiotherapy during prehabilitation can make a significant contribution to improving exercise tolerance in terms of normalizing blood pressure.
- Body weight may be an independent factor significantly determining distance travelled in the 6MWT for women and men undergoing physiotherapy during prehabilitation before bariatric surgery.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wharton, S.; Lau, D.C.W.; Vallis, M.; Sharma, A.M.; Biertho, L.; Campbell-Scherer, D.; Adamo, K.; Alberga, A.; Bell, R.; Boulé, N.; et al. Obesity in adults: A clinical practice guideline. Can. Med. Assoc. J. 2020, 192, E875–E891. [Google Scholar] [CrossRef] [PubMed]
- Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [CrossRef] [PubMed]
- Rust, C.; Prior, R.M.; Stec, M. Implementation of a clinical practice guideline in a primary care setting for the prevention and management of obesity in adults. Nurs. Forum 2020, 55, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Cornier, M.A. A review of current guidelines for the treatment of obesity. Am. J. Manag. Care 2022, 28 (Suppl. S15), S288–S296. [Google Scholar] [PubMed]
- Yanovski, S.Z.; Yanovski, J.A. Approach to Obesity Treatment in Primary Care: A Review. JAMA Intern. Med. 2024, 184, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Bąk-Sosnowska, M.B.M.; Bogdański, P.; Chomiuk, T.; Dobrowolski, P.; Gałązka-Sobotka, M.; Holecki, M.; Jankowska-Zduńczyk, A.; Jarosińska, A.; Jezierska, M.; Kamiński, P.; et al. Zalecenia kliniczne dotyczące postępowania u chorych na otyłość 2024—Stanowisko Polskiego Towarzystwa Leczenia Otyłości. Med. Prakt. 2024, 1–116. [Google Scholar]
- Sjöström, L. Review of the key results from the Swedish Obese Subjects (SOS) trial—A prospective controlled intervention study of bariatric surgery. J. Intern. Med. 2013, 273, 219–234. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, D.; Shikora, S.A.; Aarts, E.; Aminian, A.; Angrisani, L.; Cohen, R.V.; de Luca, M.; Faria, S.L.; Goodpaster, K.P.; Haddad, A.; et al. 2022 American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) Indications for Metabolic and Bariatric Surgery. Obes. Surg. 2023, 33, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Chmelo, J.; Chmelová, I.; Phillips, A.W. Prehabilitation, improving postoperative outcomes. Rozhl. Chir. 2021, 100, 421–428. [Google Scholar] [PubMed]
- Carli, F.; Zavorsky, G.S. Optimizing functional exercise capacity in the elderly surgical population. Curr. Opin. Clin. Nutr. Metab. Care 2005, 8, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Valkenet, K.; van de Port, I.G.; Dronkers, J.J.; de Vries, W.R.; Lindeman, E.; Backx, F.J. The effects of preoperative exercise therapy on postoperative outcome: A systematic review. Clin. Rehabil. 2011, 25, 99–111. [Google Scholar] [CrossRef] [PubMed]
- O’Doherty, A.F.; West, M.; Jack, S.; Grocott, M.P. Preoperative aerobic exercise training in elective intra-cavity surgery: A systematic review. Br. J. Anaesth. 2013, 110, 679–689. [Google Scholar] [CrossRef] [PubMed]
- Mayo, N.E.; Feldman, L.; Scott, S.; Zavorsky, G.; Kim, D.J.; Charlebois, P.; Stein, B.; Carli, F. Impact of preoperative change in physical function on postoperative recovery: Argument supporting prehabilitation for colorectal surgery. Surgery 2011, 150, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Hornsby, W.E.; Douglas, P.S.; West, M.J.; Kenjale, A.A.; Lane, A.R.; Schwitzer, E.R.; Ray, K.A.; Herndon, J.E.; Coan, A.; Gutierrez, A.; et al. Safety and efficacy of aerobic training in operable breast cancer patients receiving neoadjuvant chemotherapy: A phase II randomized trial. Acta Oncol. 2014, 53, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Santelices, A.; Argüello-Florencio, G.; Westphal, G.; Nardo Junior, N.; Zamunér, A.R. Effects of Supervised Physical Exercise as Prehabilitation on Body Composition, Functional Capacity and Quality of Life in Bariatric Surgery Candidates: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 5091. [Google Scholar] [CrossRef] [PubMed]
- Thorell, A.; MacCormick, A.D.; Awad, S.; Reynolds, N.; Roulin, D.; Demartines, N.; Vignaud, M.; Alvarez, A.; Singh, P.M.; Lobo, D.N. Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J. Surg. 2016, 40, 2065–2083. [Google Scholar] [CrossRef] [PubMed]
- Szeliga, J.; Wyleżoł, M.; Major, P.; Budzyński, A.; Binda, A.; Proczko-Stepaniak, M.; Boniecka, I.; Matłok, M.; Sekuła, M.; Kaska, Ł.; et al. Metabolic and Bariatric Surgery Chapter of the Association of Polish Surgeons. Bariatric and metabolic surgery care standards. Wideochirurgia Inne Tech. Maloinwazyjne 2020, 15, 391–394. [Google Scholar] [CrossRef] [PubMed]
- García-Delgado, Y.; López-Madrazo-Hernández, M.J.; Alvarado-Martel, D.; Miranda-Calderín, G.; Ugarte-Lopetegui, A.; González-Medina, R.A.; Hernández-Lázaro, A.; Zamora, G.; Pérez-Martín, N.; Sánchez-Hernández, R.M.; et al. Prehabilitation for Bariatric Surgery: A Randomized, Controlled Trial Protocol and Pilot Study. Nutrients 2021, 13, 2903. [Google Scholar] [CrossRef] [PubMed]
- Przybyłowski, T.; Tomalak, W.; Siergiejko, Z.; Jastrzębski, D.; Maskey-Warzęchowska, M.; Piorunek, T.; Wojda, E.; Boros, P. Polish Respiratory Society Guidelines for the Methodology and Interpretation of the 6 Minute Walk Test (6MWT). Adv. Respir. Med. 2015, 83, 283–297. [Google Scholar] [CrossRef] [PubMed]
- Enright, P.L.; Sherrill, D.L. Reference equations for the six-minute walk in healthy adults. Am. J. Respir. Crit. Care Med. 1998, 158 Pt 1, 1384–1387. [Google Scholar] [CrossRef] [PubMed]
- WHO. Waist Circumference and Waist-Hip Ratio Report of a WHO Expert Consultation; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- Kear, B.M.; Guck, T.P.; McGaha, A.L. Timed Up and Go (TUG) Test: Normative Reference Values for Ages 20 to 59 Years and Relationships With Physical and Mental Health Risk Factors. J. Prim. Care Community Health 2017, 8, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Pelliccia, A.; Sharma, S.; Gati, S.; Bäck, M.; Börjesson, M.; Caselli, S.; Collet, J.-P.; Corrado, D.; Drezner, J.A.; Halle, M.; et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 2021, 42, 17–96. [Google Scholar] [CrossRef] [PubMed]
- Hulsbæk, S.; Larsen, R.F.; Rosthøj, S.; Kristensen, M.T. The Barthel Index and the Cumulated Ambulation Score are superior to the de Morton Mobility Index for the early assessment of outcome in patients with a hip fracture admitted to an acute geriatric ward. Disabil. Rehabil. 2019, 41, 1351–1359. [Google Scholar] [CrossRef] [PubMed]
- Scherr, J.; Wolfarth, B.; Christle, J.W.; Pressler, A.; Wagenpfeil, S.; Halle, M. Associations between Borg’s rating of perceived exertion and physiological measures of exercise intensity. Eur. J. Appl. Physiol. 2013, 113, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Jegier, A.; Szalewska, D.; Mawlichanów, A.; Bednarczyk, T.; Eysymontt, Z.; Gałaszek, M.; Mamcarz, A.; Mierzyńska, A.; Piotrowicz, E.; Piotrowicz, R.; et al. Kompleksowa rehabilitacja kardiologiczna podstawą prewencji wtórnej chorób układu sercowo-naczyniowego. Opinia ekspertów Sekcji Rehabilitacji Kardiologicznej i Fizjologii Wysiłku Polskiego Towarzystwa Kardiologicznego. Pol. Heart J. (Kardiol. Pol.) 2021, 79, 28–45. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.R-project.org/ (accessed on 18 May 2021).
- Smith, N.A.; Martin, G.; Marginson, B. Preoperative assessment and prehabilitation in patients with obesity undergoing non-bariatric surgery: A systematic review. J. Clin. Anesth. 2022, 78, 110676. [Google Scholar] [CrossRef] [PubMed]
- Conaty, E.A.; Bonamici, N.J.; Gitelis, M.E.; Johnson, B.J.; DeAsis, F.; Carbray, J.M.; Lapin, B.; Joehl, R.; Denham, W.; Linn, J.G.; et al. Efficacy of a Required Preoperative Weight Loss Program for Patients Undergoing Bariatric Surgery. J. Gastrointest. Surg. 2016, 20, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Ekici, U.; Ferhatoglu, M.F. Perioperative and Postoperative Effects of Preoperative Low-Calorie Restrictive Diets on Patients Undergoing Laparoscopic Sleeve Gastrectomy. J. Gastrointest. Surg. 2020, 24, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Marcon, E.R.; Baglioni, S.; Bittencourt, L.; Lopes, C.L.; Neumann, C.R.; Trindade, M.R. What Is the Best Treatment before Bariatric Surgery? Exercise, Exercise and Group Therapy, or Conventional Waiting: A Randomized Controlled Trial. Obes. Surg. 2017, 27, 763–773. [Google Scholar] [CrossRef] [PubMed]
- Picó-Sirvent, I.; Aracil-Marco, A.; Pastor, D.; Moya-Ramón, M. Effects of a Combined High-Intensity Interval Training and Resistance Training Program in Patients Awaiting Bariatric Surgery: A Pilot Study. Sports 2019, 7, 72. [Google Scholar] [CrossRef] [PubMed]
- Baillot, A.; Mampuya, W.M.; Dionne, I.J.; Comeau, E.; Méziat-Burdin, A.; Langlois, M.F. Impacts of Supervised Exercise Training in Addition to Interdisciplinary Lifestyle Management in Subjects Awaiting Bariatric Surgery: A Randomized Controlled Study. Obes. Surg. 2016, 26, 2602–2610. [Google Scholar] [CrossRef] [PubMed]
- Baillot, A.; Boissy, P.; Tousignant, M.; Langlois, M.-F. Feasibility and effect of in-home physical exercise training delivered via telehealth before bariatric surgery. J. Telemed. Telecare 2016, 23, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Głuszewska, A.; Gryglewska, B.; Gąsowski, J.; Bilo, G.; Zarzycki, B.; Dzieża-Grudnik, A.; Major, P.; Budzyński, A.; Faini, A.; Parati, G.; et al. Reduction of 24-h blood pressure variability in extreme obese patients 10 days and 6 months after bariatric surgery depending on pre-existing hypertension. Eur. J. Intern. Med. 2019, 60, 39–45. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Study Group (n = 30) | Control Group (n = 20) | p-Value | Effect Size | Statistical Power |
|---|---|---|---|---|---|
| Anthropometric measures | |||||
| Age (years) | 43.0 ± 10 | 40.8 ± 8.2 | 0.3977 t | 0.2367 cd | 0.1266 |
| Gender: female; male | 19 11 | 11 9 | 0.7683 c | 0.0833 ph | 0.0906 |
| Body weight (kg) | 125.5 (105.5; 141.8) | 128 (104; 143.5) | 0.9763 w | 0.0042 wr | 0.061 mb |
| Height (cm) | 171.5 ± 7.8 | 174.2 ± 10.1 | 0.3247 w | 0.3036 cd | 0.1778 |
| BMI (kg/m2) | 42.3 (37.9; 48.3) | 41.7 (37.0; 45.8) | 0.4819 | 0.0995 wr | 0.061 mb |
| Abdominal circumference (cm) | 132 (118.5; 149) | 128.5 (117.0; 138.2) | 0.4335 w | 0.1108 wr | 0.128 mb |
| Chest mobility test (cm) | 3.8 (3; 4) | 3 (3; 4) | 0.9666 w | 0.0059 wr | 0.040 mb |
| TUG (s) | 8.9 ± 1.7 | 7.5 ± 1.8 | 0.0084 t | 0.8060 cd | 0.7811 |
| Resting parameters | |||||
| Heart rate (bpm) | 76.3 ± 9.7 | 77.0 ± 8.8 | 0.8163 t | 0.0662 cd | 0.0558 |
| Systolic pressure (mmHg) | 131.7 ± 14.4 | 133.3 ± 16.2 | 0.7283 t | 0.1035 cd | 0.0643 |
| Diastolic pressure (mmHg) | 89.4 ± 7.9 | 89.5 (83.8; 94.2) | 0.7358 w | 0.0477 wr | 0.054 mb |
| Saturation (%) | 98.0 (97.0; 98.8) | 98.0 (97.0; 99.0) | 0.2122 w | 0.1764 wr | 0.267 mb |
| Borg RPE scale (10 degrees) | 0 (0; 0.5) | 0 (0; 0.5) | 0.5786 w | 0.0785 wr | 0.075 mb |
| Parameters after exertion | |||||
| Heart rate (bpm) | 113.5 (106.2; 121.8) | 119.3 ± 22.4 | 0.3885 w | 0.1220 wr | 0.159 mb |
| Systolic pressure (mmHg) | 145.0 (130.0; 149.0) | 144.5 (132.8; 150.5) | 0.7361 w | 0.0447 wr | 0.065 mb |
| Diastolic pressure (mmHg) | 88.4 ± 8.4 | 89.2 ± 5.9 | 0.6928 t | 0.1070 cd | 0.0653 |
| Saturation (%) | 97.0 (96.0; 98.0) | 98.0 (96.8; 99.0) | 0.1659 w | 0.1960 wr | 0.307 mb |
| Borg RPE scale (10 degrees) | 2 (0.5; 3) | 2 (0.5; 3) | 0.6980 w | 0.0549 wr | 0.079 mb |
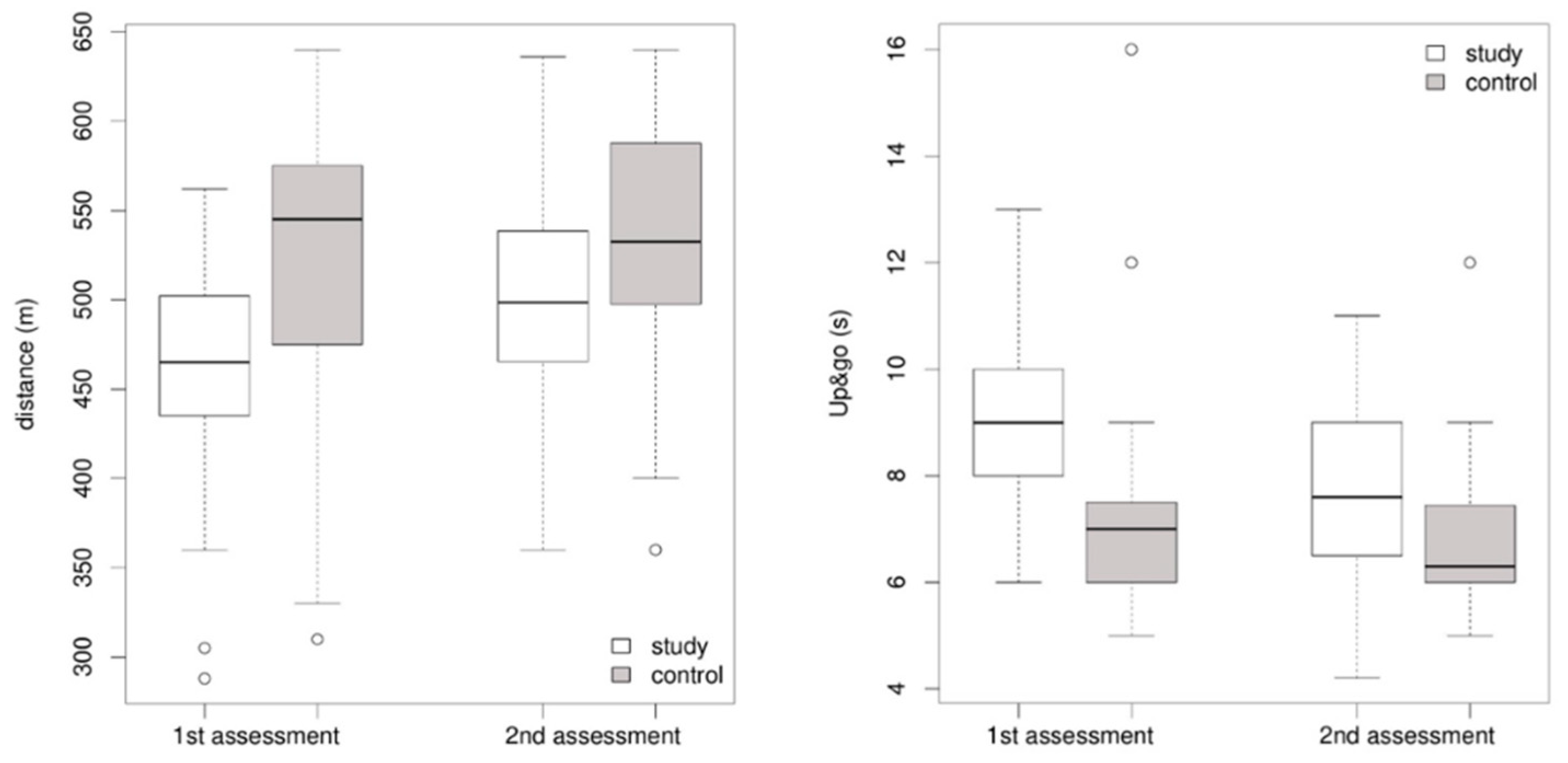
| Distance (m) | 458.3 ± 65.7 | 500.5 ± 70.7 | 0.0399 t | 0.6230 cd | 0.5616 |
| Parameter | Study Group (n = 30) | Control Group (n = 20) | p-Value | Effect Size | Statistical Power |
|---|---|---|---|---|---|
| Anthropometric measures | |||||
| Body weight (kg) | 117.5 (101.2; 140.2) | 122 (99.4; 137.8) | 0.8741 w | 0.0224 wr | 0.052 mb |
| BMI (kg/m2) | 39.7 (36.2; 45.1) | 39.7 (34.9; 42.9) | 0.6416 w | 0.0658 wr | 0.081 mb |
| Abdominal circumference (cm) | 121.5 (109.2;145.0) | 121.0 (109.8; 136.0) | 0.9367 w | ||
| Chest mobility test (cm) | 4.0 (3.0; 4.8) | 3.2 ± 1.2 | 0.0874 w | 0.2417 wr | 0.408 mb |
| TUG test (s) | 7.0 (6.0; 7.4) | 6.3 (6.0; 7.4) | 0.7870 w | 0.0382 wr | 0.062 mb |
| Resting parameters | |||||
| Heart rate (bpm) | 72.4 ± 10.9 | 75.8 ± 10.5 | 0.2744 t | 0.3172 cd | 0.1898 |
| Systolic pressure (mmHg) | 120.8 ± 15.3 | 128.3 ± 17.7 | 0.1272 t | 0.4637 cd | 0.3500 |
| Diastolic pressure (mmHg) | 78.1 ± 9.1 | 82.7 ± 10.6 | 0.1231 t | 0.4703 cd | 0.3584 |
| Saturation (%) | 98 (97; 99) | 98 (97; 99) | 0.5027 w | 0.0948 wr | 0.125 mb |
| Borg RPE scale (10 degrees) | 0 (0; 0) | 0 (0; 0) | 0.9661 w | 0.0060 wr | 0.041 mb |
| Parameters after exertion | |||||
| Heart rate (bpm) | 115.6 ± 23.4 | 119.6 ± 19.2 | 0.5174 t | 0.1808 cd | 0.0942 |
| Systolic pressure (mmHg) | 128.8 ± 20.4 | 142.1 ± 18.2 | 0.0204 t | 0.6782 cd | 0.6339 |
| Diastolic pressure (mmHg) | 79.2 ± 10.5 | 86.4 ± 12.3 | 0.0377 t | 0.6431 cd | 0.5883 |
| Saturation (%) | 98.0 (96.2; 99.0) | 98.5 (97.0; 99.0) | 0.6186 w | 0.0704 wr | 0.063 mb |
| Borg RPE scale (10 degrees) | 2 (0.6; 3.8) | 2 (0.5; 3.0) | 0.6022 w | 0.0737 wr | 0.083 mb |
| Distance (m) | 545.0 (476.2; 573.8) | 532.8 ± 79.2 | 0.7435 w | 0.0463 wr | 0.078 mb |
| Parameter | p-Value (Comparison of Study 1 and Study 2 for Study Group (n = 30)) | Effect Size | Statistical Power | p-Value (Comparison of Study 1 and Study 2 for Control Group (n = 20)) | Effect Size | Statistical Power |
|---|---|---|---|---|---|---|
| Body weight (kg) | <0.0001 np | 0.8334 | 1 mb | 0.0003 np | 0.8291 | 1 mb |
| Abdominal circumference (cm) | <0.0001 np | 0.8065 | 1 mb | 0.0143 np | 0.5475 | 0.706 mb |
| Chest mobility test (cm) | 0.3338 np | 0.1765 | 0.145 mb | 0.0922 np | 0.3863 | 0.421 mb |
| TUG test (s) | 0.0001 np | 0.7045 | 0.999 mb | 0.1705 np | 0.3064 | 0.268 mb |
| 6MWT distance (m) | 0.0005 np | 0.6384 | 0.958 mb | 0.0628 tp | 0.4295 | 0.446 mb |
| Distance Determined from Models | Study Group (1st Assessment) | p-Value (For the Values Obtained in the Model with the Actual Distance) | Control Group (1st Assessment) | p-Value (For the Values Obtained in the Model with the Actual Distance) |
|---|---|---|---|---|
| LLN | 378.5 ± 76.8 | 0.000012 td1 | 413.4 ± 66.3 | 0.000017 td1 |
| 6MWT | 522.7 ± 78.5 | 0.000263 td1 | 558.7 ± 67.9 | 0.001159 td1 |
| Study Group (2nd Assessment) | Control Group (2nd Assessment) | |||
| LLN | 397.9 ± 72 | 0.000010 wd2 | 429.2 ± 67.3 | 0.000041 td2 |
| 6MWT | 542 ± 73.9 | 0.800470 wd2 | 574.5 ± 69 | 0.030534 td2 |
| Coefficient | Estimate | p-Value |
|---|---|---|
| Male | ||
| (Intercept) | −182.2877 | 0.7185 |
| Weight | −1.1334 | 0.0258 |
| Height | 4.5586 | 0.1337 |
| Multiple R2: 0.2721; adjusted R2: 0.1865 | ||
| Female | ||
| (Intercept) | 723.8017 | 0.00000000601 |
| Age | −1.9185 | 0.0606 |
| Weight | −1.3952 | 0.0399 |
| Multiple R2: 0.1158; adjusted2: 0.08417 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gierat-Haponiuk, K.; Wąż, P.; Haponiuk-Skwarlińska, J.; Wilczyński, M.; Haponiuk, I. Physiotherapy in Prehabilitation for Bariatric Surgery—Analysis of Its Impact on Functional Capacity and Original Predictive Models of Functional Status Outcome. J. Clin. Med. 2025, 14, 5265. https://doi.org/10.3390/jcm14155265
Gierat-Haponiuk K, Wąż P, Haponiuk-Skwarlińska J, Wilczyński M, Haponiuk I. Physiotherapy in Prehabilitation for Bariatric Surgery—Analysis of Its Impact on Functional Capacity and Original Predictive Models of Functional Status Outcome. Journal of Clinical Medicine. 2025; 14(15):5265. https://doi.org/10.3390/jcm14155265
Chicago/Turabian StyleGierat-Haponiuk, Katarzyna, Piotr Wąż, Julia Haponiuk-Skwarlińska, Maciej Wilczyński, and Ireneusz Haponiuk. 2025. "Physiotherapy in Prehabilitation for Bariatric Surgery—Analysis of Its Impact on Functional Capacity and Original Predictive Models of Functional Status Outcome" Journal of Clinical Medicine 14, no. 15: 5265. https://doi.org/10.3390/jcm14155265
APA StyleGierat-Haponiuk, K., Wąż, P., Haponiuk-Skwarlińska, J., Wilczyński, M., & Haponiuk, I. (2025). Physiotherapy in Prehabilitation for Bariatric Surgery—Analysis of Its Impact on Functional Capacity and Original Predictive Models of Functional Status Outcome. Journal of Clinical Medicine, 14(15), 5265. https://doi.org/10.3390/jcm14155265






