Midterm Outcomes of Medial Patellofemoral Ligament Reconstruction in Adolescent Athletes: Comparison Between Acute and Recurrent Patella Dislocation
Abstract
1. Introduction
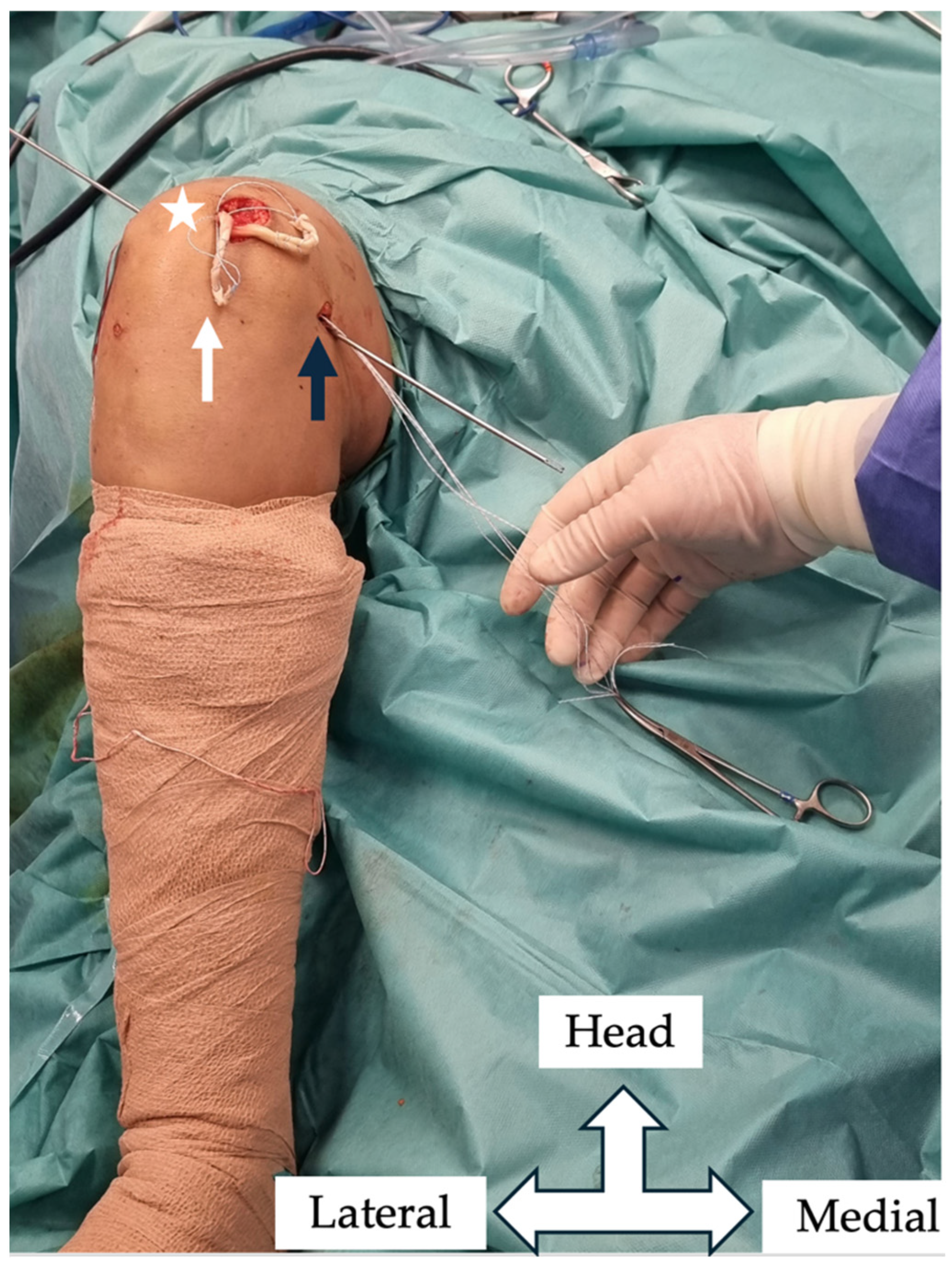
2. Materials and Methods
3. Results
3.1. Demographic Data
3.2. Clinical Outcomes
3.3. VAS Score and Knee Range of Motion
3.4. Functional and Activity Scores
3.5. Patient Satisfaction
3.6. Complications
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MPFL | Medial Patellofemoral Ligament |
| Pedi-IKDC | Pediatric International Knee Documentation Committee’s scale |
| VAS | visual analog scale |
| TAS | Tegner activity scale |
| TT–TG | Tibial Tubercle–Trochlear Groove |
| PROMs | Patient-Reported Outcome Measures |
References
- Hawkins, R.J.; Bell, R.H.; Anisette, G. Acute Patellar Dislocations. The Natural History. Am. J. Sports Med. 1986, 14, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Fithian, D.C.; Paxton, E.W.; Stone, M.L.; Silva, P.; Davis, D.K.; Elias, D.A.; White, L.M. Epidemiology and Natural History of Acute Patellar Dislocation. Am. J. Sports Med. 2004, 32, 1114–1121. [Google Scholar] [CrossRef] [PubMed]
- Jaquith, B.P.; Parikh, S.N. Predictors of Recurrent Patellar Instability in Children and Adolescents After First-Time Dislocation. J. Pediatr. Orthop. 2017, 37, 484–490. [Google Scholar] [CrossRef]
- Huntington, L.S.; Webster, K.E.; Devitt, B.M.; Scanlon, J.P.; Feller, J.A. Factors Associated with an Increased Risk of Recurrence After a First-Time Patellar Dislocation: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2020, 48, 2552–2562. [Google Scholar] [CrossRef]
- Kepler, C.K.; Bogner, E.A.; Hammoud, S.; Malcolmson, G.; Potter, H.G.; Green, D.W. Zone of Injury of the Medial Patellofemoral Ligament after Acute Patellar Dislocation in Children and Adolescents. Am. J. Sports Med. 2011, 39, 1444–1449. [Google Scholar] [CrossRef]
- Nelitz, M.; Dreyhaupt, J.; Reichel, H.; Woelfle, J.; Lippacher, S. Anatomic Reconstruction of the Medial Patellofemoral Ligament in Children and Adolescents with Open Growth Plates: Surgical Technique and Clinical Outcome. Am. J. Sports Med. 2013, 41, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Deie, M.; Ochi, M.; Sumen, Y.; Yasumoto, M.; Kobayashi, K.; Kimura, H. Reconstruction of the Medial Patellofemoral Ligament for the Treatment of Habitual or Recurrent Dislocation of the Patella in Children. J. Bone Joint Surg. Br. 2003, 85, 887–890. [Google Scholar]
- Ntagiopoulos, P.; Pozzi, P.; Kalinterakis, G.; Fligkos, D.; Dimou, T.; Compagnoni, R.; Ferrua, P.; Randelli, P.S. Anatomic Physeal-sparing MPFL Reconstruction in Skeletally Immature Patients Shows Favourable Outcomes at a Minimum of 24-month Follow-up. J. Exp. Orthop. 2024, 11, e70063. [Google Scholar] [CrossRef]
- Migliorini, F.; Maffulli, N.; Bell, A.; Betsch, M. Outcomes, Return to Sport, and Failures of MPFL Reconstruction Using Autografts in Children and Adolescents with Recurrent Patellofemoral Instability: A Systematic Review. Children 2022, 9, 1892. [Google Scholar] [CrossRef]
- Kalinterakis, G.; Vlastos, I.; Gianzina, E.; Dimitriadis, S.; Mastrantonakis, K.; Chronopoulos, E.; Yiannakopoulos, C.K. MPFL Reconstruction in Skeletally Immature Patients: Comparison Between Anatomic and Non-Anatomic Femoral Fixation-Systematic Review. Children 2024, 11, 1275. [Google Scholar] [CrossRef]
- McFarlane, K.H.; Coene, R.P.; Feldman, L.; Miller, P.E.; Heyworth, B.E.; Kramer, D.E.; Kocher, M.S.; Yen, Y.-M.; Milewski, M.D. Increased Incidence of Acute Patellar Dislocations and Patellar Instability Surgical Procedures across the United States in Paediatric and Adolescent Patients. J. Child. Orthop. 2021, 15, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Le May, S.; Ballard, A.; Khadra, C.; Gouin, S.; Plint, A.C.; Villeneuve, E.; Mâsse, B.; Tsze, D.S.; Neto, G.; Drendel, A.L.; et al. Comparison of the Psychometric Properties of 3 Pain Scales Used in the Pediatric Emergency Department: Visual Analogue Scale, Faces Pain Scale-Revised, and Colour Analogue Scale. Pain 2018, 159, 1508–1517. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, C.; Constantinou, A.; Cheimonidou, A.-Z.; Stasinopoulos, D. Greek Cultural Adaption and Validation of the Kujala Anterior Knee Pain Scale in Patients with Patellofemoral Pain Syndrome. Disabil. Rehabil. 2017, 39, 704–708. [Google Scholar] [CrossRef]
- van der Velden, C.A.; van der Steen, M.C.; Leenders, J.; van Douveren, F.Q.M.P.; Janssen, R.P.A.; Reijman, M. Pedi-IKDC or KOOS-Child: Which Questionnaire Should Be Used in Children with Knee Disorders? BMC Musculoskelet. Disord. 2019, 20, 240. [Google Scholar] [CrossRef]
- Nasreddine, A.Y.; Connell, P.L.; Kalish, L.A.; Nelson, S.; Iversen, M.D.; Anderson, A.F.; Kocher, M.S. The Pediatric International Knee Documentation Committee (Pedi-IKDC) Subjective Knee Evaluation Form: Normative Data. Am. J. Sports Med. 2017, 45, 527–534. [Google Scholar] [CrossRef]
- Fawdry, A.; O’Dowd, D. Assesing the use of the Tegner Activity Scale in Children: Is it a Useful Tool? Orthop. Proc. 2023, 105-B, 18. [Google Scholar] [CrossRef]
- Hasler, C.C.; Studer, D. Patella Instability in Children and Adolescents. EFORT Open Rev. 2016, 1, 160–166. [Google Scholar] [CrossRef]
- Sinikumpu, J.; Nicolaou, N. Current Concepts in the Treatment of First-Time Patella Dislocation in Children and Adolescents. J. Child. Orthop. 2023, 17, 28–33. [Google Scholar] [CrossRef]
- Sahin, E.; Tandogan, R.; Liebensteiner, M.; Demey, G.; Kayaalp, A. Management of Patellar Instability in Skeletally Immature Patients. EFORT Open Rev. 2024, 9, 60–68. [Google Scholar] [CrossRef]
- Saccomanno, M.F.; Sircana, G.; Fodale, M.; Donati, F.; Milano, G. Surgical versus Conservative Treatment of Primary Patellar Dislocation. A Systematic Review and Meta-Analysis. Int. Orthop. 2016, 40, 2277–2287. [Google Scholar] [CrossRef]
- Smith, T.O.; Donell, S.; Song, F.; Hing, C.B. Surgical versus Non-Surgical Interventions for Treating Patellar Dislocation. Cochrane Database Syst. Rev. 2015, 26, CD008106. [Google Scholar] [CrossRef]
- Zhang, K.; Jiang, H.; Li, J.; Fu, W. Comparison Between Surgical and Nonsurgical Treatment for Primary Patellar Dislocations in Adolescents: A Systematic Review and Meta-Analysis of Comparative Studies. Orthop. J. Sports Med. 2020, 8, 2325967120946446. [Google Scholar] [CrossRef] [PubMed]
- Fuller, J.A.; Hammil, H.L.; Pronschinske, K.J.; Durall, C.J. Operative Versus Nonoperative Treatment After Acute Patellar Dislocation: Which Is More Effective at Reducing Recurrence in Adolescents? J. Sport Rehabil. 2018, 27, 601–604. [Google Scholar] [CrossRef] [PubMed]
- Nwachukwu, B.U.; So, C.; Schairer, W.W.; Green, D.W.; Dodwell, E.R. Surgical versus Conservative Management of Acute Patellar Dislocation in Children and Adolescents: A Systematic Review. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2016, 24, 760–767. [Google Scholar] [CrossRef]
- Rund, J.M.; Hinckel, B.B.; Sherman, S.L. Acute Patellofemoral Dislocation: Controversial Decision-Making. Curr. Rev. Musculoskelet. Med. 2021, 14, 82–87. [Google Scholar] [CrossRef]
- Kalinterakis, G.; Vlastos, I.; Gianzina, E.; Sachinis, N.P.; Yiannakopoulos, C.K. Medial Patellofemoral Ligament Reconstruction Using Patella Bone Tunnel Techniques with or without Implants. A Systematic Review of Outcomes and Complications. Eur. J. Orthop. Surg. Traumatol. Orthop. Traumatol. 2023, 33, 3225–3234. [Google Scholar] [CrossRef]
- Schlumberger, M.; Schuster, P.; Hofmann, S.; Mayer, P.; Immendörfer, M.; Mayr, R.; Richter, J. Midterm Results After Isolated Medial Patellofemoral Ligament Reconstruction as First-Line Surgical Treatment in Skeletally Immature Patients Irrespective of Patellar Height and Trochlear Dysplasia. Am. J. Sports Med. 2021, 49, 3859–3866. [Google Scholar] [CrossRef]
- Bremond, N.; Prima, R.; Rabattu, P.-Y.; Accadbled, F.; Chotel, F.; Konkel, M.; Eid, A.; Philippe, C.; Godinho, A.; Turati, M.; et al. Isolated MPFL Reconstruction with Soft Tissue Femoral Fixation Technique in 54 Skeletally Immature Patients: Clinical Outcomes at 2 Years Follow-up. A French Multicenter Retrospective Study. Orthop. Traumatol. Surg. Res. OTSR 2023, 109, 103530. [Google Scholar] [CrossRef]
- Arendt, E.A.; Donell, S.T.; Sillanpää, P.J.; Feller, J.A. The Management of Lateral Patellar Dislocation: State of the Art. J. ISAKOS 2017, 2, 205–212. [Google Scholar] [CrossRef]
- Liu, J.N.; Brady, J.M.; Kalbian, I.L.; Strickland, S.M.; Ryan, C.B.; Nguyen, J.T.; Shubin Stein, B.E. Clinical Outcomes After Isolated Medial Patellofemoral Ligament Reconstruction for Patellar Instability Among Patients With Trochlear Dysplasia. Am. J. Sports Med. 2018, 46, 883–889. [Google Scholar] [CrossRef]
- Gurusamy, P.; Pedowitz, J.M.; Carroll, A.N.; Johnson, K.; Chambers, H.G.; Edmonds, E.W.; Pennock, A.T. Medial Patellofemoral Ligament Reconstruction for Adolescents With Acute First-Time Patellar Dislocation With an Associated Loose Body. Am. J. Sports Med. 2021, 49, 2159–2164. [Google Scholar] [CrossRef] [PubMed]
- Haraldsdottir, K.; Watson, A.M. Psychosocial Impacts of Sports-Related Injuries in Adolescent Athletes. Curr. Sports Med. Rep. 2021, 20, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Magnussen, R.A.; Verlage, M.; Stock, E.; Zurek, L.; Flanigan, D.C.; Tompkins, M.; Agel, J.; Arendt, E.A. Primary Patellar Dislocations without Surgical Stabilization or Recurrence: How Well Are These Patients Really Doing? Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2017, 25, 2352–2356. [Google Scholar] [CrossRef]
- D’Ambrosi, R.; Corona, K.; Capitani, P.; Coccioli, G.; Ursino, N.; Peretti, G.M. Complications and Recurrence of Patellar Instability after Medial Patellofemoral Ligament Reconstruction in Children and Adolescents: A Systematic Review. Children 2021, 8, 434. [Google Scholar] [CrossRef]
- Migliorini, F.; Rath, B.; Tingart, M.; Meisen, N.; Eschweiler, J. Surgical Management for Recurrent Patellar Dislocations in Skeletally Immature Patients. Eur. J. Orthop. Surg. Traumatol. Orthop. Traumatol. 2019, 29, 1815–1822. [Google Scholar] [CrossRef]




| Group A Acute Patella Dislocation | Group B Recurrent Dislocation | p Value | ||
|---|---|---|---|---|
| Gender (Male/Female) | n = 21, 12 males, 9 females | n = 18, 10 males, 8 females | 0.72 | |
| Age, years, mean (SD) | 14.7 ± 1.6 | 14.8 ± 1.3 | 0.36 | |
| Side (Right/Left) | 13/8 | 10/8 | 0.94 | |
| BMI, kg/m2, mean (SD) | 23.33 ± 4.12 (21.4–26.4) | 24.76 ± 3.08 (20.6–25.9) | 0.23 | |
| Follow-up, months, mean (SD) | 39.32 ± 12.1 | 36.24 ± 16.5 | 0.51 | |
| Sport of injury, Number | Football | 11 | 12 | |
| Basketball | 8 | 5 | ||
| Other | 2 | 1 | ||
| Trochlear Dysplasia, Dejour Grade | A | 16 | 10 | |
| B | 3 | 5 | ||
| C | 1 | 3 | ||
| D | 1 | 0 |
| Score | Δ Group A (Acute) Mean ± SD | Δ Group B (Recurrent) Mean ± SD | p-Value (ΔA vs ΔB) * |
|---|---|---|---|
| Lysholm | 18.39 ± 20.25 | 28.42 ± 8.62 | 0.037 |
| Kujala | 26.00 ± 22.17 | 37.44 ± 21.51 | 0.046 |
| Pedi-IKDC | 25.67 ± 13.14 | 35.46 ± 13.13 | 0.006 |
| VAS | −2.63 ± 1.66 | −3.23 ± 2.49 | 0.238 |
| Tegner | −0.44 ± 2.76 | −0.66 ± 4.29 | 0.783 |
| Group A, Acute Patella Dislocation | Group B, Recurrent Patella Dislocation | |||
|---|---|---|---|---|
| Score | p Value | |||
| Lysholm score, mean ± SD | Preoperatively | 74.18 ± 19.23 | 62.1 ± 11.65 | 0.01 |
| Latest follow-up | 92.57 ± 6.21 | 90.53 ± 8.21 | 0.062 | |
| Kujala score, mean ± SD Range | Preoperatively | 68.21 ± 21.01 (48–79) | 55.32 ± 17.09 (38–72) | 0.01 |
| Latest follow-up | 94.21 ± 9.23 (76–100) | 92.76 ± 12.39 (70–100) | 0.08 | |
| Pedi-IKDC score, mean ± SD Range | Preoperatively | 67.98 ± 12.29 (55–87) | 56.2 ± 13.6 (42–74) | 0.01 |
| Latest follow-up | 93.65 ± 4.1 (81–98) | 91.67 ± 6.21 (75–98) | 0.067 | |
| Tegner activity score, mean ± SD Range | Preoperatively | 7.72 ± 1.65 (6–9) | 7.45 ± 2.09 (6–9) | 0.076 |
| Latest follow-up | 7.28 ± 2.15 | 6.79 ± 3.70 | 0.065 | |
| VAS score, mean ± SD | Preoperatively | 3.1 ± 1.13 | 4.21 ± 3.01 | 0.01 |
| Latest follow-up | 0.47 ± 1.01 | 0.97 ± 1.32 | 0.083 | |
| Patient satisfaction | Satisfied | 16 | 11 | |
| Very satisfied | 4 | 3 | ||
| Moderate | 1 | 1 | ||
| Not satisfied | 0 | 3 |
| Complications | Total (n1+2/N1+2) | Group A (n1/N1) | Group B (n2/N2) | p Value a |
|---|---|---|---|---|
| Postoperative subluxation episodes | 5/39 (12.82%) | 2/21 (9.5%) | 3/18 (16.6%) | 0.21 |
| Reoperations | 3/39 (7.6%) | 1/21 (4.7%) | 2/18 (11.1%) | 0.58 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kalinterakis, G.; Yiannakopoulos, C.K.; Koukos, C.; Mastrantonakis, K.; Chronopoulos, E. Midterm Outcomes of Medial Patellofemoral Ligament Reconstruction in Adolescent Athletes: Comparison Between Acute and Recurrent Patella Dislocation. J. Clin. Med. 2025, 14, 4881. https://doi.org/10.3390/jcm14144881
Kalinterakis G, Yiannakopoulos CK, Koukos C, Mastrantonakis K, Chronopoulos E. Midterm Outcomes of Medial Patellofemoral Ligament Reconstruction in Adolescent Athletes: Comparison Between Acute and Recurrent Patella Dislocation. Journal of Clinical Medicine. 2025; 14(14):4881. https://doi.org/10.3390/jcm14144881
Chicago/Turabian StyleKalinterakis, Georgios, Christos K. Yiannakopoulos, Christos Koukos, Konstantinos Mastrantonakis, and Efstathios Chronopoulos. 2025. "Midterm Outcomes of Medial Patellofemoral Ligament Reconstruction in Adolescent Athletes: Comparison Between Acute and Recurrent Patella Dislocation" Journal of Clinical Medicine 14, no. 14: 4881. https://doi.org/10.3390/jcm14144881
APA StyleKalinterakis, G., Yiannakopoulos, C. K., Koukos, C., Mastrantonakis, K., & Chronopoulos, E. (2025). Midterm Outcomes of Medial Patellofemoral Ligament Reconstruction in Adolescent Athletes: Comparison Between Acute and Recurrent Patella Dislocation. Journal of Clinical Medicine, 14(14), 4881. https://doi.org/10.3390/jcm14144881






