The FT3/FT4 Ratio as a Metabolic Marker of Frailty and Prognosis in Older Adults with Heart Failure
Abstract
1. Introduction
2. Materials and Methods
2.1. Clinical and Laboratory Assessments
2.2. Laboratory Measures
2.3. Statistical Analysis
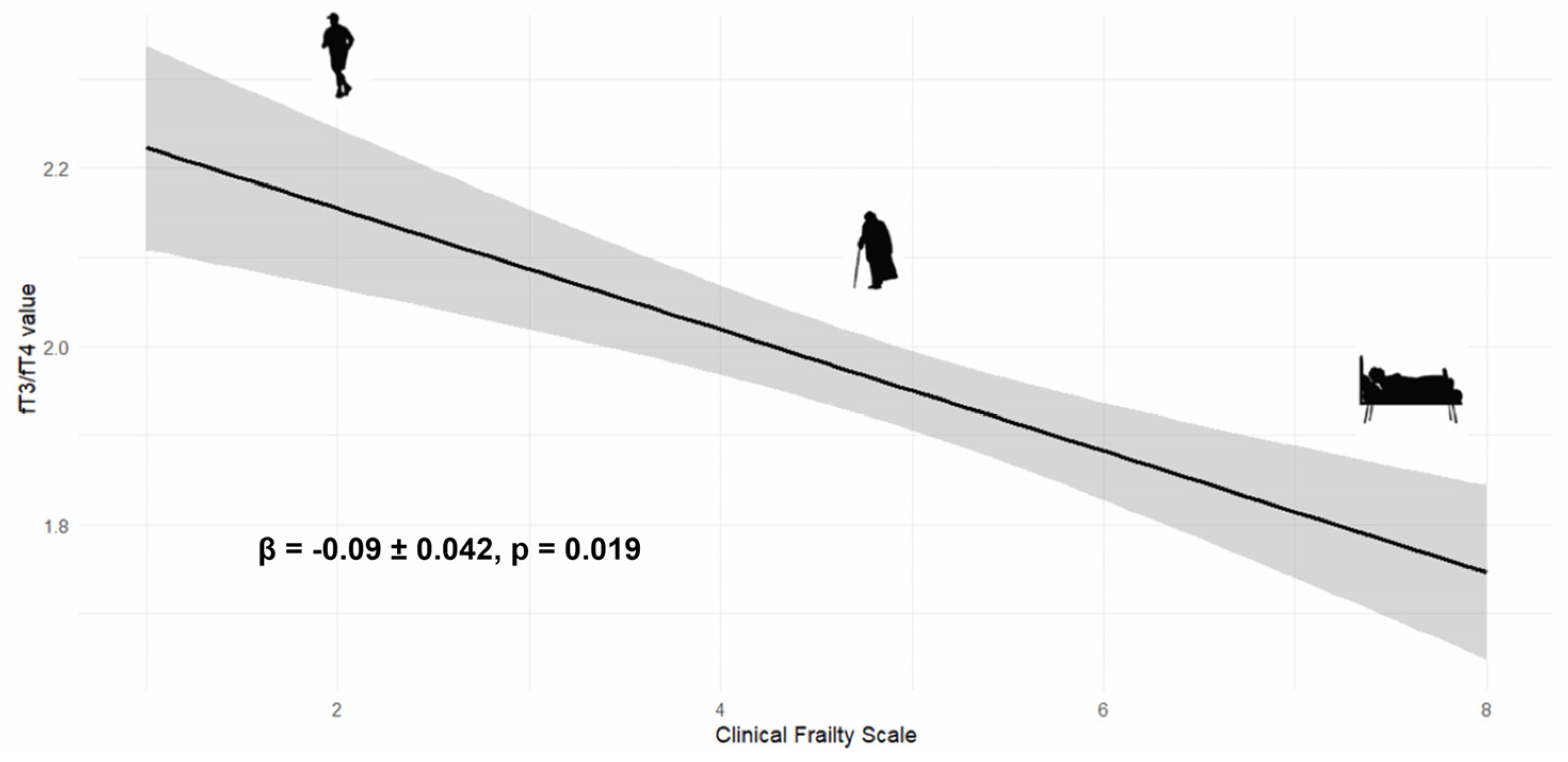
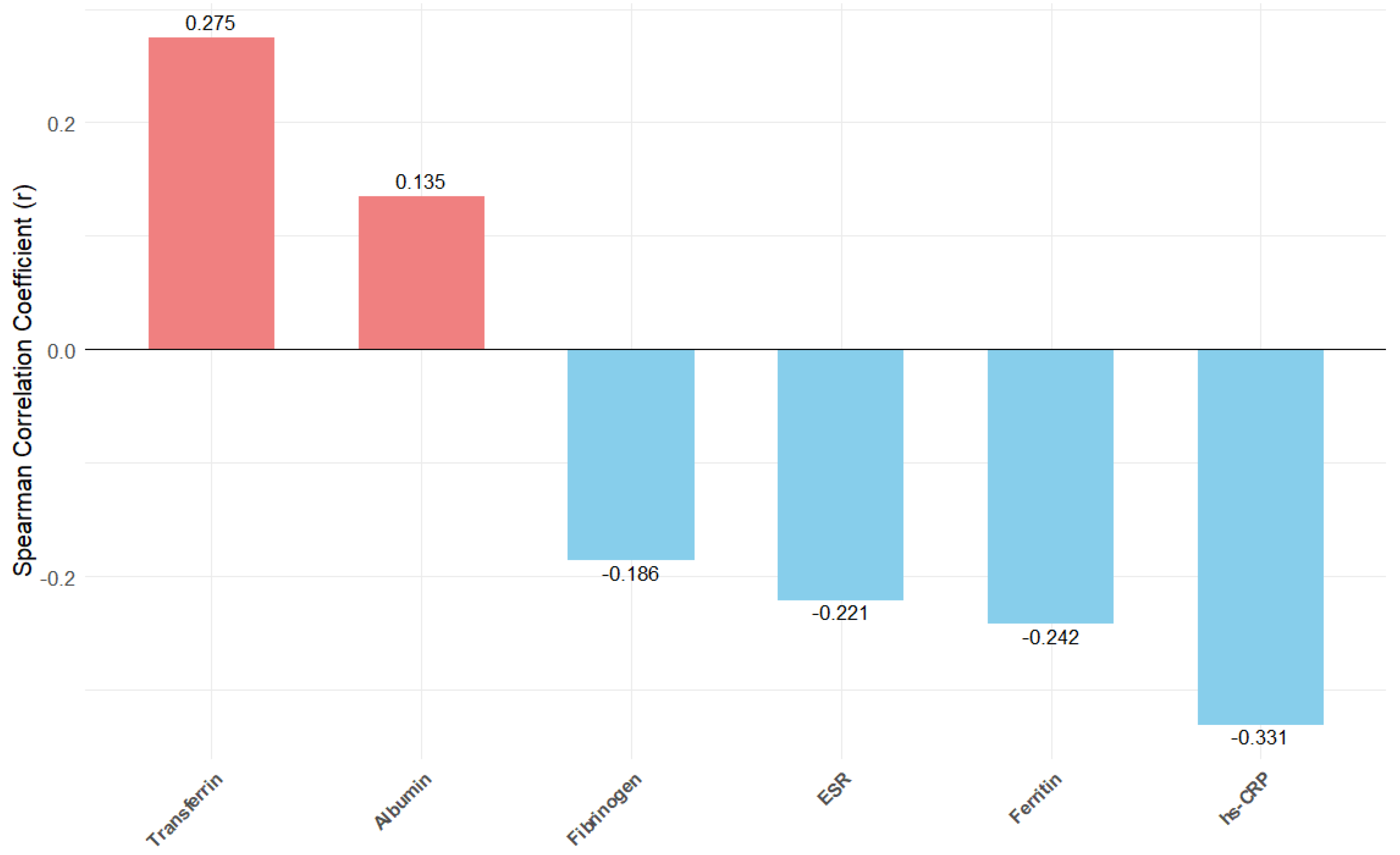
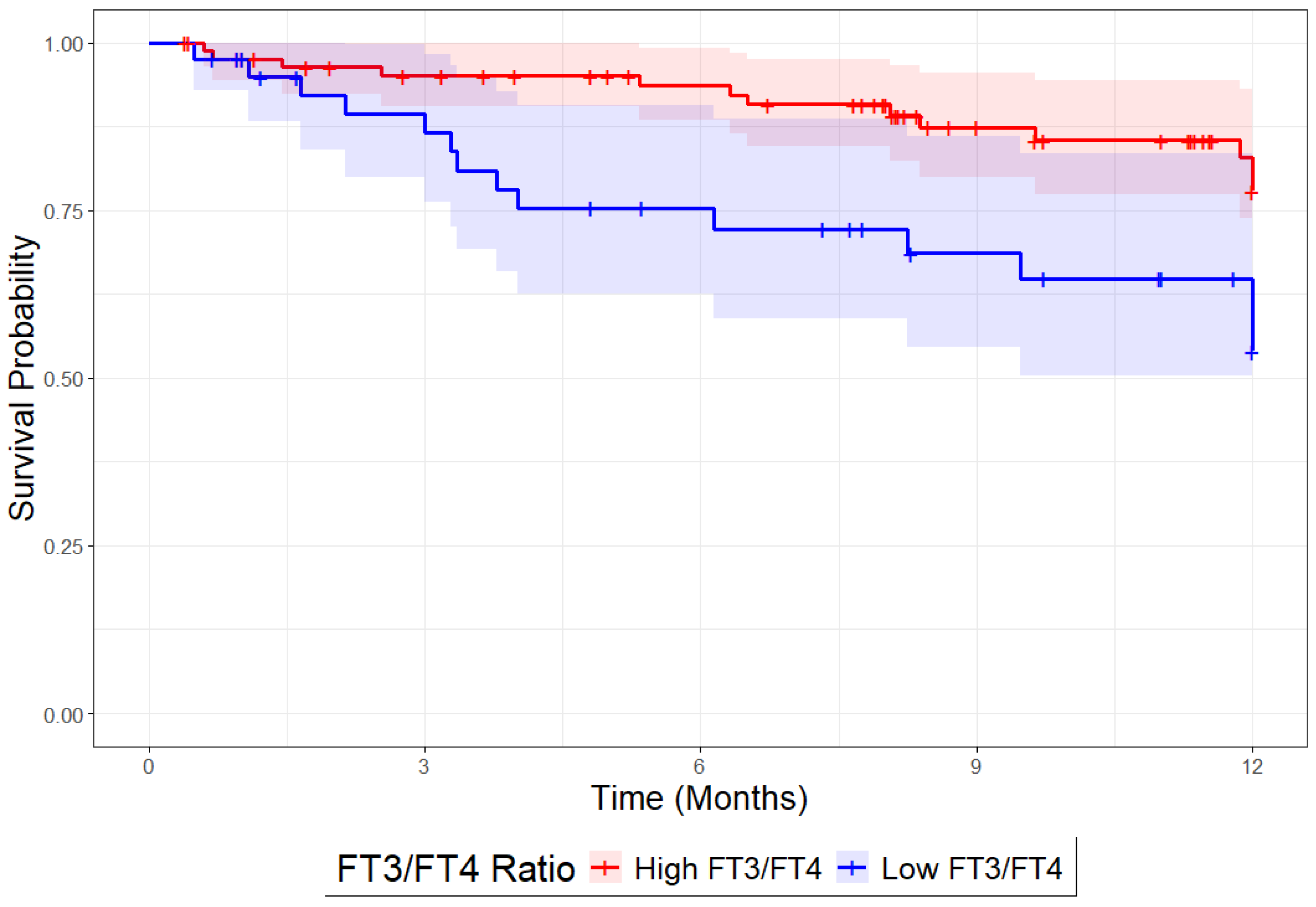
3. Results
3.1. Baseline Characteristics
3.2. Nutritional and Inflammatory Markers
3.3. Cardiovascular Assessments
3.4. Mortality Risk
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADL | Activities of Daily Living |
| AF | Atrial Fibrillation |
| BADL | Basic Activities of Daily Living |
| BMI | Body Mass Index |
| CFS | Clinical Frailty Scale |
| CGA | Comprehensive Geriatric Assessment |
| CKD | Chronic Kidney Disease |
| CIRS-c | Cumulative Illness Rating Scale-Comorbidity Index |
| COPD | Chronic Obstructive Pulmonary Disease |
| EF | Ejection Fraction |
| FT3 | Free Triiodothyronine |
| FT4 | Free Thyroxine |
| HF | Heart Failure |
| HFpEF | Heart Failure with Preserved Ejection Fraction |
| HFrEF | Heart Failure with Reduced Ejection Fraction |
| HGS | Handgrip Strength |
| Hs-CRP | High-Sensitivity-C-Reactive Protein |
| IADL | Instrumental Activities of Daily Living |
| LVEF | Left Ventricular Ejection Fraction |
| MNA-SF | Mini Nutritional Assessment-Short Form |
| NT-proBNP | N-terminal pro-B-type Natriuretic Peptide |
| SPMSQ | Short Portable Mental Status Questionnaire |
| TAPSE | Tricuspid Annular Plane Systolic Excursion |
| TnHS | High-Sensitivity Troponin |
| TSH | Thyroid-Stimulating Hormone |
References
- Dharmarajan, K.; Rich, M.W. Epidemiology, Pathophysiology, and Prognosis of Heart Failure in Older Adults. Heart Fail. Clin. 2017, 13, 417–426. [Google Scholar] [CrossRef] [PubMed]
- Van Riet, E.E.S.; Hoes, A.W.; Wagenaar, K.P.; Limburg, A.; Landman, M.A.J.; Rutten, F.H. Epidemiology of heart failure: The prevalence of heart failure and ventricular dysfunction in older adults over time. A systematic review. Eur. J. Heart Fail. 2016, 18, 242–252. [Google Scholar] [CrossRef] [PubMed]
- Cesari, M.; Prince, M.; Thiyagarajan, J.A.; De Carvalho, I.A.; Bernabei, R.; Chan, P.; Gutierrez-Robledo, L.M.; Michel, J.-P.; Morley, J.E.; Ong, P.; et al. Frailty: An Emerging Public Health Priority. J. Am. Med. Dir. Assoc. 2016, 17, 188–192. [Google Scholar] [CrossRef]
- Kim, D.H.; Rockwood, K. Frailty in Older Adults. N. Engl. J. Med. 2024, 391, 538–548. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Pandey, A.; Kitzman, D.; Reeves, G. Frailty Is Intertwined with Heart Failure: Mechanisms, Prevalence, Prognosis, Assessment, and Management. JACC Heart Fail. 2019, 7, 1001–1011. [Google Scholar] [CrossRef]
- Faller, J.W.; Pereira, D.d.N.; de Souza, S.; Nampo, F.K.; Orlandi, F.d.S.; Matumoto, S. Instruments for the detection of frailty syndrome in older adults: A systematic review. PLoS ONE 2019, 14, e0216166. [Google Scholar] [CrossRef]
- Sze, S.; Pellicori, P.; Zhang, J.; Weston, J.; Clark, A.L. Which frailty tool best predicts morbidity and mortality in ambulatory patients with heart failure? A prospective study. Eur. Heart J. Qual. Care Clin. Outcomes 2022, 9, qcac073. [Google Scholar] [CrossRef]
- Rodríguez-Mañas, L.; Rodriguez-Sánchez, I. Research on Frailty: Where We Stand and Where We Need to Go. J. Am. Med. Dir. Assoc. 2021, 22, 520–523. [Google Scholar] [CrossRef]
- El Assar, M.; Rodríguez-Sánchez, I.; Álvarez-Bustos, A.; Rodríguez-Mañas, L. Biomarkers of frailty. Mol. Asp. Med. 2024, 97, 101271. [Google Scholar] [CrossRef]
- Pasqualetti, G.; Calsolaro, V.; Bernardini, S.; Linsalata, G.; Bigazzi, R.; Caraccio, N.; Monzani, F. Degree of Peripheral Thyroxin Deiodination, Frailty, and Long-Term Survival in Hospitalized Older Patients. J. Clin. Endocrinol. Metab. 2018, 103, 1867–1876. [Google Scholar] [CrossRef]
- Arosio, B.; Monti, D.; Mari, D.; Passarino, G.; Ostan, R.; Ferri, E.; De Rango, F.; Franceschi, C.; Cesari, M.; Vitale, G. Thyroid hormones and frailty in persons experiencing extreme longevity. Exp. Gerontol. 2020, 138, 111000. [Google Scholar] [CrossRef] [PubMed]
- Okoye, C.; Arosio, B.; Carino, S.; Putrino, L.; Franchi, R.; Rogani, S.; Cesari, M.; Mari, D.; Vitale, G.; Malara, A.; et al. The Free Triiodothyronine/Free Thyroxine Ratio Is Associated with Frailty in Older Adults: A Longitudinal Multisetting Study. Thyroid. Off. J. Am. Thyroid. Assoc. 2023, 33, 169–176. [Google Scholar] [CrossRef]
- Tognini, S.; Marchini, F.; Dardano, A.; Polini, A.; Ferdeghini, M.; Castiglioni, M.; Monzani, F. Non-thyroidal illness syndrome and short-term survival in a hospitalised older population. Age Ageing 2010, 39, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Yoshihisa, A.; Kimishima, Y.; Kiko, T.; Kanno, Y.; Yokokawa, T.; Abe, S.; Misaka, T.; Sato, T.; Oikawa, M.; et al. Low T3 Syndrome Is Associated With High Mortality in Hospitalized Patients with Heart Failure. J. Card. Fail. 2019, 25, 195–203. [Google Scholar] [CrossRef]
- Lang, X.; Li, Y.; Zhang, D.; Zhang, Y.; Wu, N.; Zhang, Y. FT3/FT4 ratio is correlated with all-cause mortality, cardiovascular mortality, and cardiovascular disease risk: NHANES 2007–2012. Front. Endocrinol. 2022, 13, 964822. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Okoye, C.; Mazzarone, T.; Finazzi, A.; Daniela, G.; Bruni, A.A.; Maccioni, L.; Pescatore, G.; Bianco, M.G.; Guerrini, C.; Giusti, A.; et al. Outcomes of early post-discharge cardio-geriatric care in frail patients after acute heart failure: A before-and-after study. BMC Geriatr. 2025, 25, 236. [Google Scholar] [CrossRef]
- Stuck, A.E.; Siu, A.L.; Wieland, G.D.; Adams, J.; Rubenstein, L.Z. Comprehensive geriatric assessment: A meta-analysis of controlled trials. Lancet 1993, 342, 1032–1036. [Google Scholar] [CrossRef]
- Pfeiffer, E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef]
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of Illness in the Aged: The Index of ADL: A Standardized Measure of Biological and Psychosocial Function. JAMA 1963, 185, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Parmelee, P.A.; Thuras, P.D.; Katz, I.R.; Lawton, M.P. Validation of the Cumulative Illness Rating Scale in a geriatric residential population. J. Am. Geriatr. Soc. 1995, 43, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Guigoz, Y.; Lauque, S.; Vellas, B.J. Identifying the elderly at risk for malnutrition. The Mini Nutritional Assessment. Clin. Geriatr. Med. 2002, 18, 737–757. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. CMAJ Can. Med. Assoc. J. J. L’association Medicale Can. 2005, 173, 489–495. [Google Scholar] [CrossRef]
- Theou, O.; Pérez-Zepeda, M.U.; van der Valk, A.M.; Searle, S.D.; Howlett, S.E.; Rockwood, K. A classification tree to assist with routine scoring of the Clinical Frailty Scale. Age Ageing 2021, 50, 1406–1411. [Google Scholar] [CrossRef]
- Kanesvaran, R.; Koo, K.N.; Chen, W.; Poon, D. An analysis of the prognostic value of handgrip strength and its incorporation into the comprehensive geriatric assessment (CGA) in elderly Asian patients with cancer. J. Clin. Oncol. 2011, 29, 9093. [Google Scholar] [CrossRef]
- Nagre, A. Focus-assessed transthoracic echocardiography: Implications in perioperative and intensive care. Ann. Card. Anaesth. 2019, 22, 302–308. [Google Scholar] [CrossRef]
- Lindner, M.; Thomas, R.; Claggett, B.; Lewis, E.F.; Groarke, J.; Merz, A.A.; Silverman, M.B.; Swamy, V.; Rivero, J.; Hohenstein, C.; et al. Quantification of pleural effusions on thoracic ultrasound in acute heart failure Original scientific paper. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 513–521. [Google Scholar] [CrossRef]
- Zhao, X.; Sun, J.; Xin, S.; Zhang, X. Predictive Effects of FT3/FT4 on Diabetic Kidney Disease: An Exploratory Study on Hospitalized Euthyroid Patients with T2DM in China. Biomedicines 2023, 11, 2211. [Google Scholar] [CrossRef]
- Nardin, G.D.; Colombo, B.d.S.; Ronsoni, M.F.; Silva, P.E.S.E.; Fayad, L.; Wildner, L.M.; Bazzo, M.L.; Dantas-Correa, E.B.; Narciso-Schiavon, J.L.; Schiavon, L.d.L. Thyroid hormone profile is related to prognosis in acute decompensation of cirrhosis. Arch. Endocrinol. Metab. 2024, 68, e230249. [Google Scholar] [CrossRef]
- Li, Y.; Pan, T.; Wang, L.; Wang, Y.; Gong, Y.; Wang, G.; Zhang, Q. Increased FT3/FT4 ratio in a certain range is associated with decreased glycemic variability in patients with type 2 diabetes. Sci. Rep. 2024, 14, 26556. [Google Scholar] [CrossRef]
- Nelli, F.; Ruggeri, E.M.; Schirripa, M.; Virtuoso, A.; Giannarelli, D.; Raso, A.; Remotti, D.; Fabbri, A. Longitudinal Assessment of FT3 to FT4 Conversion Ratio in Predicting the Efficacy of First-Line Pembrolizumab-Based Therapy in Advanced Non-Small Cell Lung Cancer: A Propensity-Score Matching Analysis of Data from the National Drug Monitoring Agency. Curr. Oncol. 2024, 31, 7647–7662. [Google Scholar] [CrossRef]
- van Heerebeek, L.; Paulus, W.J. Understanding heart failure with preserved ejection fraction: Where are we today? Neth. Heart J. Mon. J. Neth. Soc. Cardiol. Neth. Heart Found. 2016, 24, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Mantzouratou, P.; Malaxianaki, E.; Cerullo, D.; Lavecchia, A.M.; Pantos, C.; Xinaris, C.; Mourouzis, I. Thyroid Hormone and Heart Failure: Charting Known Pathways for Cardiac Repair/Regeneration. Biomedicines 2023, 11, 975. [Google Scholar] [CrossRef]
- Kannan, L.; Shaw, P.A.; Morley, M.P.; Brandimarto, J.; Fang, J.C.; Sweitzer, N.K.; Cappola, T.P.; Cappola, A.R. Thyroid Dysfunction in Heart Failure and Cardiovascular Outcomes. Circ. Heart Fail. 2018, 11, e005266. [Google Scholar] [CrossRef] [PubMed]
- Upadhya, B.; Pisani, B.; Kitzman, D.W. Evolution of a Geriatric Syndrome: Pathophysiology and Treatment of Heart Failure with Preserved Ejection Fraction. J. Am. Geriatr. Soc. 2017, 65, 2431–2440. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, C.; Garagnani, P.; Parini, P.; Giuliani, C.; Santoro, A. Inflammaging: A new immune-metabolic viewpoint for age-related diseases. Nat. Rev. Endocrinol. 2018, 14, 576–590. [Google Scholar] [CrossRef]
- Franceschi, C.; Ostan, R.; Mariotti, S.; Monti, D.; Vitale, G. The Aging Thyroid: A Reappraisal Within the Geroscience Integrated Perspective. Endocr. Rev. 2019, 40, 1250–1270. [Google Scholar] [CrossRef]
- Hata, S.; Okada, H.; Minamida, M.; Hironaka, J.; Hasegawa, Y.; Kondo, Y.; Nakajima, H.; Kitagawa, N.; Okamura, T.; Hashimoto, Y.; et al. Associations between thyroid hormones and appendicular skeletal muscle index, and hand grip strength in people with diabetes: The KAMOGAWA-A study. Diabetes Res. Clin. Pract. 2024, 209, 111573. [Google Scholar] [CrossRef]
- Wang, Z.; Wu, P.; Yang, J.; Jiang, Y.; Wang, J.; Lin, C. Serum FT3/FT4, but not TSH is associated with handgrip strength in euthyroid U.S. population: Evidence from NHANES. Front. Endocrinol. 2024, 15, 1323026. [Google Scholar] [CrossRef] [PubMed]
- Zupo, R.; Castellana, F.; Sardone, R.; Lampignano, L.; Paradiso, S.; Giagulli, V.A.; Triggiani, V.; Di Lorenzo, L.; Giannelli, G.; De Pergola, G. Higher Muscle Mass Implies Increased Free-Thyroxine to Free-Triiodothyronine Ratio in Subjects with Overweight and Obesity. Front. Endocrinol. 2020, 11, 565065. [Google Scholar] [CrossRef] [PubMed]
- Dentice, M.; Marsili, A.; Ambrosio, R.; Guardiola, O.; Sibilio, A.; Paik, J.-H.; Minchiotti, G.; DePinho, R.A.; Fenzi, G.; Larsen, P.R.; et al. The FoxO3/type 2 deiodinase pathway is required for normal mouse myogenesis and muscle regeneration. J. Clin. Investig. 2010, 120, 4021–4030. [Google Scholar] [CrossRef] [PubMed]
- Fliers, E.; Bianco, A.C.; Langouche, L.; Boelen, A. Thyroid function in critically ill patients. Lancet Diabetes Endocrinol. 2015, 3, 816–825. [Google Scholar] [CrossRef]
- Van den Berghe, G. Non-thyroidal illness in the ICU: A syndrome with different faces. Thyroid 2014, 24, 1456–1465. [Google Scholar] [CrossRef]
| All Patients N = 193 | FT3/FT4 ≥ 1.7 N = 133 | FT3/FT4 < 1.7 N = 60 | p-Value | |
|---|---|---|---|---|
| Sex (F) | 119 (56.1) | 73 (54.8) | 35 (58.8) | 0.636 |
| Age (mean, SD) | 86.5 (6.1) | 86.2 (6.8) | 87.1 (4.9) | 0.585 |
| BADL (median, IQR) | 5 (5) | 5 (4) | 4 (5) | 0.022 |
| IADL (median, IQR) | 2 (5) | 2 (5) | 1 (5) | 0.047 |
| CFS (median, IQR) | 5 (3) | 4 (3) | 6 (2) | 0.020 |
| SPMSQ (median, IQR) | 3 (4) | 3 (3) | 4 (3) | 0.031 |
| MNA (median, IQR) | 11 (3) | 12 (3) | 10 (4) | 0.008 |
| Handgrip test, Kg, (mean, SD) | 19.7 (4.5) | 20.3 (4.8) | 16.8 (3.7) | 0.002 |
| Females (mean, SD) | 12.3 (7) | 15.8 (4.9) | 14.1 (2.3) | 0.06 |
| Males (mean, SD) | 20.1 (10.3) | 25.8 (7.8) | 17.3 (3.9) | <0.001 |
| CIRS-c (mean, SD) | 3 (2) | 3 (2) | 3 (2) | 0.81 |
| Hypertension (%) | 134 (66.3) | 83 (63.1) | 43 (72.2) | 0.188 |
| T2DM (%) | 56 (27.7) | 34 (26.1) | 18 (30.5) | 0.503 |
| COPD (%) | 54 (26.7) | 66 (27.6) | 15 (25.0) | 0.679 |
| CAD (%) | 33 (16.4) | 21 (16.3) | 10 (16.7) | 0.943 |
| Stroke (%) | 22 (11.0) | 15 (11.5) | 4 (10.0) | 0.74 |
| CKD (%) | 73 (36.5) | 53 (41.1) | 17 (28.2) | 0.069 |
| AF (%) | 114 (56.7) | 81 (62.8) | 21 (35.8) | 0.020 |
| TSH, mIU/L | 1.97 (2.20) | 2.02 (2.25) | 1.87 (2.01) | 0.699 |
| Hs-CRP, mg/L (mean, SD) | 7.8 (8.78) | 5.8 (7.4) | 10.6 (9.7) | <0.001 |
| Fibrinogen, mg/dL (mean, SD) | 461 (172) | 439 (158) | 495 (187) | 0.003 |
| Ferritin, ng/mL (mean, SD) | 441.7 (798) | 323.9 (465) | 604 (1085) | <0.001 |
| Transferrin, mg/dL (mean, SD) | 192 (62.4) | 204.2 (57.2) | 175.1 (65.5) | <0.001 |
| Albumin, g/dL, (mean, SD) | 3.32 (0.49) | 3.42 (0.46) | 3.19 (0.51) | <0.001 |
| ESR, mm/h, (mean, SD) | 61.8 (36.2) | 55.9 (35.6) | 69.7 (35.8) | <0.001 |
| Creatinine, mg/dL, (mean, SD) | 1.44 (0.68) | 1.40 (0.55) | 1.46 (0.73) | 0.28 |
| NT-proBNP, pg/mL, (mean, SD) | 1991 (3380) | 1860 (3669) | 2221 (1951) | 0.966 |
| Uric Acid (mg/dL), (mean, SD) | 6.99 (2.85) | 6.8 (2.6) | 7.2 (3.1) | 0.205 |
| All Patients N = 193 | FT3/FT4 > 1.7 N = 133 | FT3/FT4 < 1.7 N = 60 | p-Value | |
|---|---|---|---|---|
| NT-proBNP, pg/mL (median, IQR) | 1991 (3380) | 1860 (3669) | 2221 (1950) | 0.966 |
| Serum Iron, µg/dL (median, IQR) | 43 (26.5) | 44 (23) | 43 (31) | 0.154 |
| EF (%) | 52.5 (18) | 55 (14.7) | 51.5 (11.0) | 0.106 |
| HFrEF, n (%) | 57 (37.0) | 40 (41.2) | 17 (29.8) | 0.159 |
| HFmrEF, n (%) | 26 (16.8) | 18 (18.6) | 8 (14.0) | |
| HFpEF, n (%) | 71 (46.1) | 39 (40.2) | 32 (56.1) | |
| LIS, mm (mean, SD) | 12 (3.3) | 11.9 (3.2) | 12.4 (3.8) | 0.493 |
| PAPS, mm (median, IQR) | 42.5 (13.1) | 40 (11) | 45 (14.2) | 0.787 |
| TAPSE, mm (median, IQR) | 19.7 (3.5) | 19.6 (3.7) | 19.8 (3.1) | 0.684 |
| HR per minute (median, IQR) | 70 (10) | 70 (10) | 75 (12) | 0.814 |
| SBP, mmHg (median, IQR) | 124.1 (20) | 123 (22.0) | 126 (15.6) | 0.513 |
| DBP, mmHg (median, IQR) | 68.9 (10.9) | 67.8 (11.3) | 71.3 (9.9) | 0.077 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okoye, C.; Mazzarone, T.; Niccolai, F.; Finazzi, A.; Esposito, E.; Bellelli, G.; Virdis, A. The FT3/FT4 Ratio as a Metabolic Marker of Frailty and Prognosis in Older Adults with Heart Failure. J. Clin. Med. 2025, 14, 4840. https://doi.org/10.3390/jcm14144840
Okoye C, Mazzarone T, Niccolai F, Finazzi A, Esposito E, Bellelli G, Virdis A. The FT3/FT4 Ratio as a Metabolic Marker of Frailty and Prognosis in Older Adults with Heart Failure. Journal of Clinical Medicine. 2025; 14(14):4840. https://doi.org/10.3390/jcm14144840
Chicago/Turabian StyleOkoye, Chukwuma, Tessa Mazzarone, Filippo Niccolai, Alberto Finazzi, Emma Esposito, Giuseppe Bellelli, and Agostino Virdis. 2025. "The FT3/FT4 Ratio as a Metabolic Marker of Frailty and Prognosis in Older Adults with Heart Failure" Journal of Clinical Medicine 14, no. 14: 4840. https://doi.org/10.3390/jcm14144840
APA StyleOkoye, C., Mazzarone, T., Niccolai, F., Finazzi, A., Esposito, E., Bellelli, G., & Virdis, A. (2025). The FT3/FT4 Ratio as a Metabolic Marker of Frailty and Prognosis in Older Adults with Heart Failure. Journal of Clinical Medicine, 14(14), 4840. https://doi.org/10.3390/jcm14144840







