Three-Dimensional Model Improves Body Image Perception After Bariatric Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Body Weight Measurements
2.3. Assessment of Anxiety and Depression
2.4. Assessment of Body Image
- -
- Prior to visualizing the avatar (“Q1”): “Are you aware of your physical change?”
- -
- After visualizing the avatar (“Q2”): “Did the avatar allow you to become aware of your physical change?”
2.5. Computerized 3D Modeling of Body Silhouettes
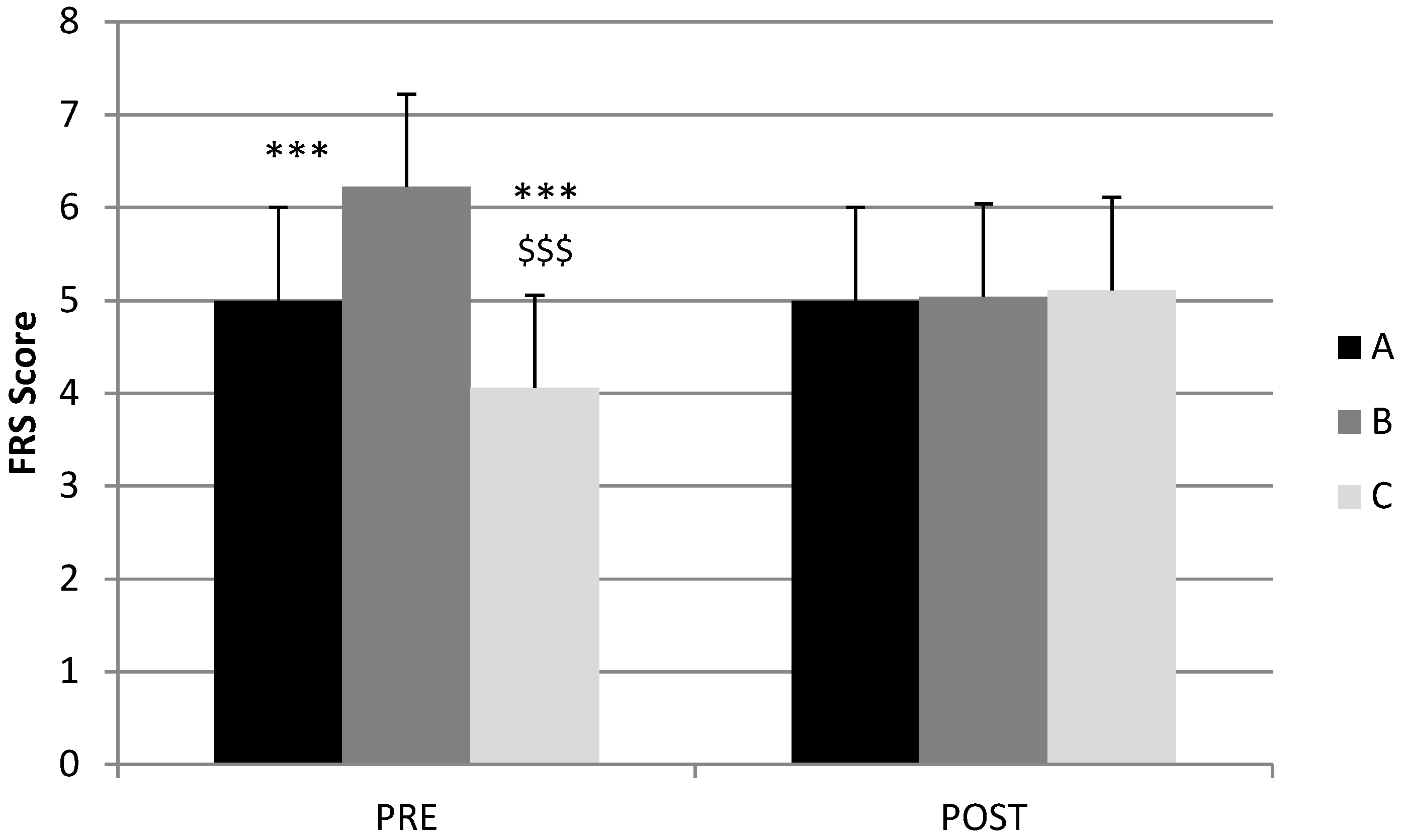
- Group A: FRS-pre = FRS-post, respectively;
- Group B: FRS-pre > FRS-post, respectively;
- Group C: FRS-pre < FRS-post, respectively.
2.6. Statistical Analyses
3. Results
3.1. Population Characteristics—Demographic Data
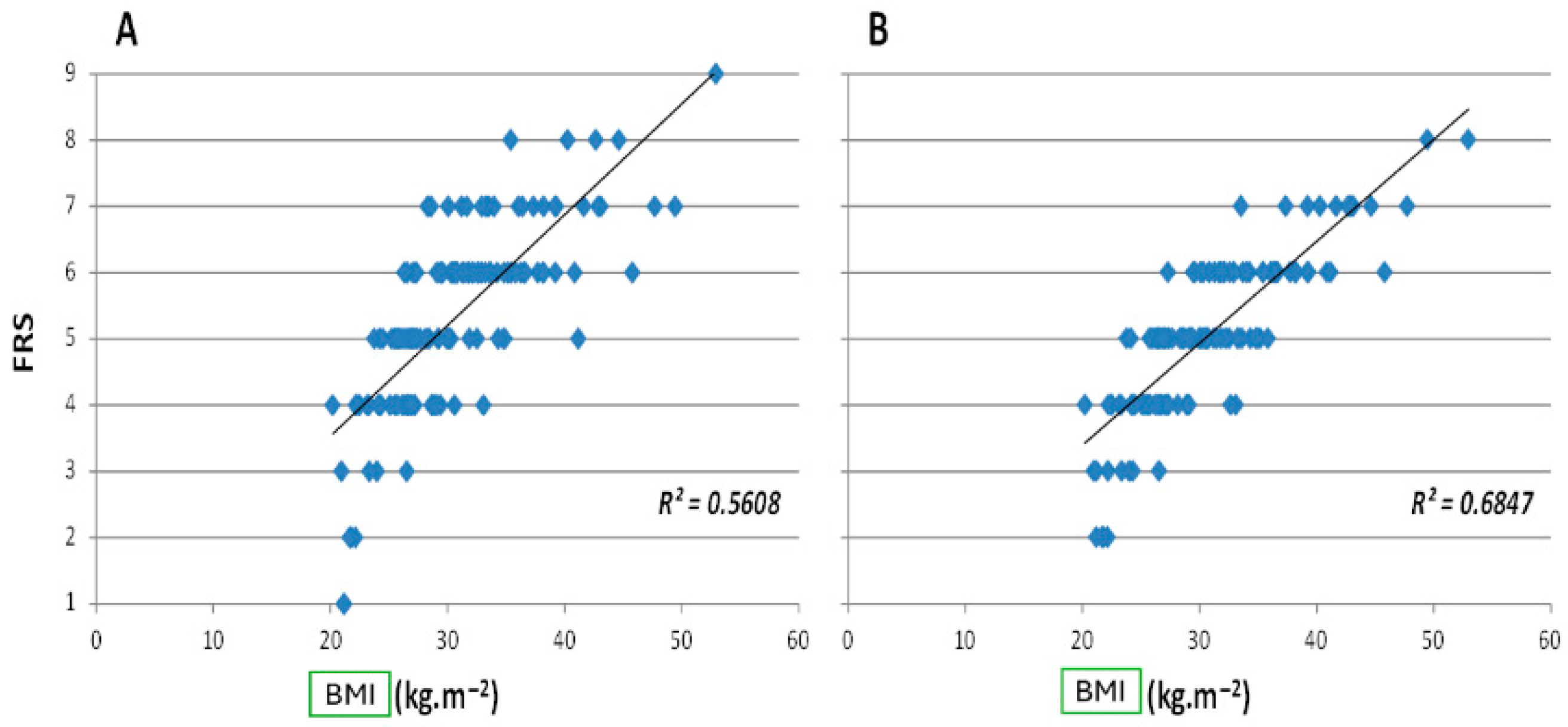
3.2. Body Image Perception Outcomes
3.3. Three-Dimensional Analysis Findings
Self-Evaluation Questions on the Perception of Physical Change and Usefulness of the 3D Tool
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ceriani, V.; Sarro, G.; Micheletto, G.; Giovanelli, A.; Zakaria, A.S.; Fanchini, M.; Osio, C.; Nosari, I.; Morabito, A.; Pontiroli, A.E.; et al. Long-term mortality in obese subjects undergoing malabsorptive surgery (biliopancreatic diversion and biliointestinal bypass) versus medical treatment. Int. J. Obes. 2019, 43, 1147–1153. [Google Scholar] [CrossRef] [PubMed]
- Puzziferri, N.; Roshek, T.B., 3rd; Mayo, H.G.; Gallagher, R.; Belle, S.H.; Livingston, E.H. Long-term follow-up after bariatric surgery: A systematic review. JAMA 2014, 312, 934–942. [Google Scholar] [CrossRef] [PubMed]
- Angrisani, L.; Santonicola, A.; Iovino, P.; Vitiello, A.; Zundel, N.; Buchwald, H.; Scopinaro, N. Bariatric Surgery and Endoluminal Procedures: IFSO Worldwide Survey 2014. Obes. Surg. 2017, 27, 2279–2289, Erratum in Obes. Surg. 2017, 27, 2290–2292. [Google Scholar] [CrossRef]
- Arterburn, D.; Wellman, R.; Emiliano, A.; Smith, S.R.; Odegaard, A.O.; Murali, S.; Williams, N.; Coleman, K.J.; Courcoulas, A.; Coley, R.Y.; et al. Comparative Effectiveness and Safety of Bariatric Procedures for Weight Loss: A PCORnet Cohort Study. Ann. Intern. Med. 2018, 169, 741–750. [Google Scholar] [CrossRef] [PubMed]
- Sarwer, D.B.; Steffen, K.J. Quality of Life, Body Image and Sexual Functioning in Bariatric Surgery Patients. Eur. Eat. Disord. Rev. 2015, 23, 504–508. [Google Scholar] [CrossRef]
- Gardner, R.M. Methodological issues in assessment of the perceptual component of body image disturbance. Br. J. Psychol. 1996, 87 Pt 2, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Perdue, T.O.; Schreier, A.; Swanson, M.; Neil, J.; Carels, R. Majority of female bariatric patients retain an obese identity 18–30 months after surgery. Eat. Weight Disord. 2020, 25, 357–364. [Google Scholar] [CrossRef]
- Cárdenas-López, G.; Torres-Villalobos, G.; Martinez, P.; Carreño, V.; Duran, X.; Dakanalis, A.; Gaggioli, A.; Riva, G. Virtual reality for improving body image disorders and weight loss after gastric band surgery: A case series. Stud. Health Technol. Inform. 2014, 196, 43–47. [Google Scholar]
- Szabó, P.; Peto, Z.; Túry, F. Az evészavarok prevalenciája a középiskolás korosztályban 10 év távlatában [The prevalence of eating disorders in a Hungarian secondary school population over a period of 10 years]. Orvosi Hetil. 2010, 151, 603–612. [Google Scholar] [CrossRef]
- Danan, M.; Carandina, S.; Nedelcu, A.; Zulian, V.; Noel, P.; Nedelcu, M. Additional tools to improve the follow up after bariatric surgery. Surg. Obes. Relat. Dis. 2017, 13, 1787–1789. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Ratcliff, M.B.; Eshleman, K.E.; Reiter-Purtill, J.; Zeller, M.H. Prospective changes in body image dissatisfaction among adolescent bariatric patients: The importance of body size estimation. Surg. Obes. Relat. Dis. 2012, 8, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Untas, A.; Koleck, M.; Rascle, N.; Borteyrou, X. Psychometric properties of the French adaptation of the multidimensional body self relations questionnaire-appearance scales. Psychol. Rep. 2009, 105, 461–471. [Google Scholar] [CrossRef]
- Mitchell, J.E.; King, W.C.; Chen, J.Y.; Devlin, M.J.; Flum, D.; Garcia, L.; Inabet, W.; Pender, J.R.; Kalarchian, M.A.; Khandelwal, S.; et al. Course of depressive symptoms and treatment in the longitudinal assessment of bariatric surgery (LABS-2) study. Obesity 2014, 22, 1799–1806. [Google Scholar] [CrossRef] [PubMed]
- Tindle, H.A.; Omalu, B.; Courcoulas, A.; Marcus, M.; Hammers, J.; Kuller, L.H. Risk of suicide after long-term follow-up from bariatric surgery. Am. J. Med. 2010, 123, 1036–1042. [Google Scholar] [CrossRef]
- Kalarchian, M.A.; King, W.C.; Devlin, M.J.; Hinerman, A.; Marcus, M.D.; Yanovski, S.Z.; Mitchell, J.E. Mental disorders and weight change in a prospective study of bariatric surgery patients: 7 years of follow-up. Surg. Obes Relat. Dis. 2019, 15, 739–748. [Google Scholar] [CrossRef]
- Neven, K.; Dymek, M.; leGrange, D.; Maasdam, H.; Boogerd, A.C.; Alverdy, J. The effects of Roux-en-Y gastric bypass surgery on body image. Obes. Surg. 2002, 12, 265–269. [Google Scholar] [CrossRef]
- Hrabosky, J.I.; Masheb, R.M.; White, M.A.; Rothschild, B.S.; Burke-Martindale, C.H.; Grilo, C.M. A prospective study of body dissatisfaction and concerns in extremely obese gastric bypass patients: 6- and 12-month postoperative outcomes. Obes. Surg. 2006, 16, 1615–1621. [Google Scholar] [CrossRef]
- Ivezaj, V.; Kessler, E.E.; Lydecker, J.A.; Barnes, R.D.; White, M.A.; Grilo, C.M. Loss-of-control eating following sleeve gastrectomy surgery. Surg. Obes. Relat. Dis. 2017, 13, 392–398. [Google Scholar] [CrossRef]
- Smith, A.C.; Stewart, B. Body perceptions and health behaviors in an online bodybuilding community. Qual. Health Res. 2012, 22, 971–985. [Google Scholar] [CrossRef]
- Alleva, J.M.; Diedrichs, P.C.; Halliwell, E.; Martijn, C.; Stuijfzand, B.G.; Treneman-Evans, G.; Rumsey, N. A randomised-controlled trial investigating potential underlying mechanisms of a functionality-based approach to improving women’s body image. Body Image 2018, 25, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Halliwell, E. Future directions for positive body image research. Body Image 2015, 14, 177–189. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gauthier, C.; Poussier, M.; Lloret-Linares, C.; Danan, M.; Nedelcu, A. Three-Dimensional Model Improves Body Image Perception After Bariatric Surgery. J. Clin. Med. 2025, 14, 4787. https://doi.org/10.3390/jcm14134787
Gauthier C, Poussier M, Lloret-Linares C, Danan M, Nedelcu A. Three-Dimensional Model Improves Body Image Perception After Bariatric Surgery. Journal of Clinical Medicine. 2025; 14(13):4787. https://doi.org/10.3390/jcm14134787
Chicago/Turabian StyleGauthier, Cyril, Matthieu Poussier, Célia Lloret-Linares, Marc Danan, and Anamaria Nedelcu. 2025. "Three-Dimensional Model Improves Body Image Perception After Bariatric Surgery" Journal of Clinical Medicine 14, no. 13: 4787. https://doi.org/10.3390/jcm14134787
APA StyleGauthier, C., Poussier, M., Lloret-Linares, C., Danan, M., & Nedelcu, A. (2025). Three-Dimensional Model Improves Body Image Perception After Bariatric Surgery. Journal of Clinical Medicine, 14(13), 4787. https://doi.org/10.3390/jcm14134787




