Histological and Histomorphometric Insights into Implant Bed Preparation: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Focused Question
2.2. Protocol
2.3. Eligibility Criteria
- Studies focusing on histological analysis or histomorphometric analysis of an implant bed;
- In vitro studies;
- In vivo;
- Studies in English;
- Non-randomized controlled clinical trials (NRSs);
- Randomized controlled clinical trials (RCTs).
- Studies not focusing on histological or histomorphometric insight into implant bed preparation;
- Non-English papers;
- Clinical reports;
- Editorial papers;
- Review articles;
- Systematic review articles;
- No full-text accessible;
- Duplicated publications.
2.4. Information Sources, Search Strategy, and Study Selection
2.5. Data Collection Process and Data Items
2.6. Assessing Risk of Bias in Individual Studies
2.7. Quality Assessment
- Is it clear in the study what is the “cause” and what is the “effect”?
- Were the participants included in any similar comparisons?
- Were the participants included in any comparisons receiving similar treatment/care, other than the exposure or intervention of interest?
- Was there a control group?
- Were there multiple measurements of the outcome both before and after the intervention/exposure?
- Was a follow up completed, and if not, were the differences between groups in terms of their follow up adequately described and analyzed?
- Were the outcomes of the participants included in any comparisons measured in the same way?
- Were the outcomes measured in a reliable way?
- Was an appropriate statistical analysis used?
3. Results
3.1. Study Selection
3.2. General Characteristics of the Studies Included in the Review
3.3. Main Study Outcomes
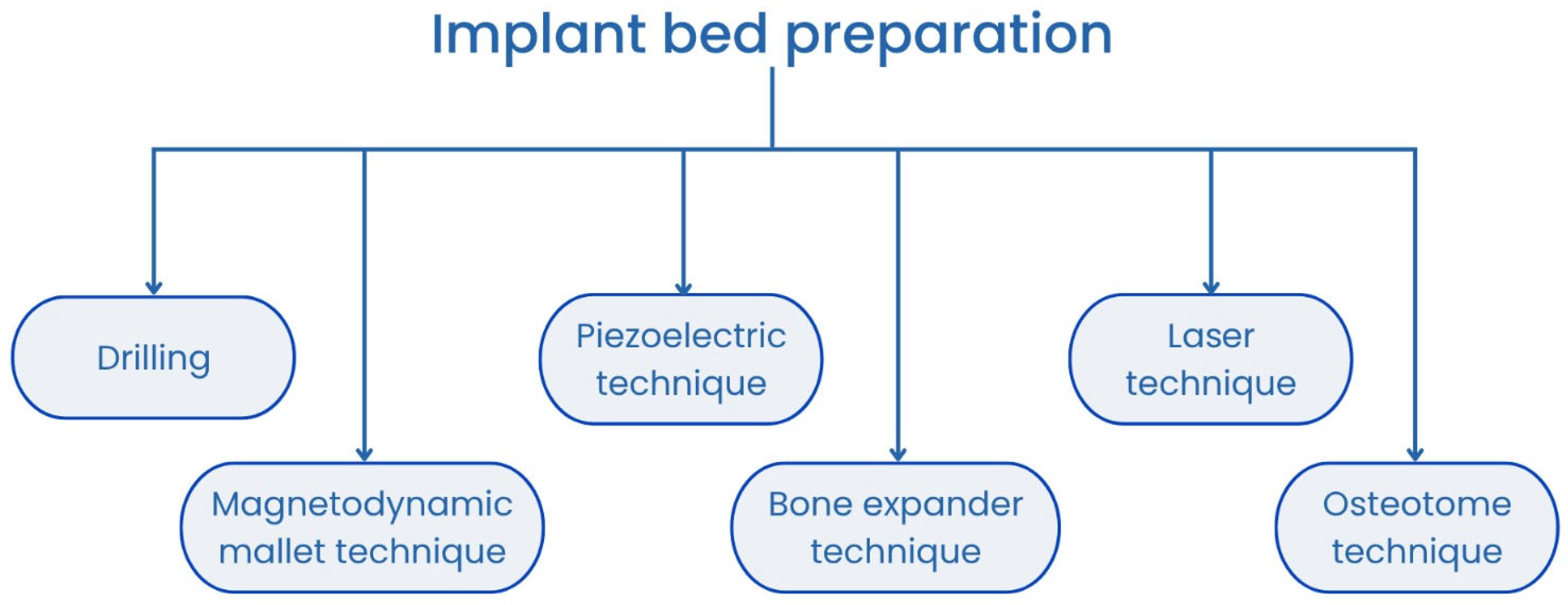
3.3.1. Conventional Burs
3.3.2. Piezosurgery
3.3.3. Osseodensification
3.3.4. Laser
3.3.5. Osteotomy with Bone Condensation
3.3.6. Bone Healing and BIC Outcomes in Histological and Histomorphometric Evaluations
3.4. Quality Assessment of Included Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhong, S.; Chen, M.; Gao, R.; Shu, C. Dental Implant Restoration for Dentition Defects Improves Clinical Efficacy, Masticatory Function and Patient Comfort. Am. J. Transl. Res. 2022, 14, 6399–6406. [Google Scholar] [PubMed]
- Fouda, S.M.; Al-Harbi, F.A.; Khan, S.Q.; Virtanen, J.I.; Raustia, A. Missing Teeth and Prosthetic Treatment in Patients Treated at College of Dentistry, University of Dammam. Int. J. Dent. 2017, 2017, 7593540. [Google Scholar] [CrossRef] [PubMed]
- Angelova Volponi, A.; Zaugg, L.K.; Neves, V.; Liu, Y.; Sharpe, P.T. Tooth Repair and Regeneration. Curr. Oral Health Rep. 2018, 5, 295–303. [Google Scholar] [CrossRef]
- Peng, K.; Zhou, Y.; Dai, Y.; Wang, Q.; Hu, Y.; Dai, Q. The Effect of Denture Restoration and Dental Implant Restoration in the Treatment of Dentition Defect: A Systematic Review and Meta-Analysis. Ann. Palliat. Med. 2021, 10, 3267–3276. [Google Scholar] [CrossRef]
- Preoteasa, E.; Oncescu Moraru, A.M.; Meghea, D.; Murariu Magureanu, C.; Preoteasa, C.T. Food Bolus Properties in Relation to Dentate and Prosthetic Status. Healthcare 2022, 10, 1596. [Google Scholar] [CrossRef]
- Boven, G.C.; Raghoebar, G.M.; Vissink, A.; Meijer, H.J.A. Improving Masticatory Performance, Bite Force, Nutritional State and Patient’s Satisfaction with Implant Overdentures: A Systematic Review of the Literature. J. Oral Rehabil. 2015, 42, 220–233. [Google Scholar] [CrossRef]
- Yoo, S.-Y.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y.; Jeon, H.-R. Clinical Performance of Implant Crown Retained Removable Partial Dentures for Mandibular Edentulism—A Retrospective Study. J. Clin. Med. 2021, 10, 2170. [Google Scholar] [CrossRef]
- Bural, C.; Buzbas, B.; Ozatik, S.; Bayraktar, G.; Emes, Y. Distal Extension Mandibular Removable Partial Denture with Implant Support. Eur. J. Dent. 2016, 10, 566–570. [Google Scholar] [CrossRef]
- Guljé, F.L.; Meijer, H.J.A.; Abrahamsson, I.; Barwacz, C.A.; Chen, S.; Palmer, P.J.; Zadeh, H.; Stanford, C.M. Comparison of 6-mm and 11-mm Dental Implants in the Posterior Region Supporting Fixed Dental Prostheses: 5-year Results of an Open Multicenter Randomized Controlled Trial. Clin. Oral Implants Res. 2021, 32, 15–22. [Google Scholar] [CrossRef]
- Kern, J.; Kern, T.; Wolfart, S.; Heussen, N. A Systematic Review and Meta-analysis of Removable and Fixed Implant-supported Prostheses in Edentulous Jaws: Post-loading Implant Loss. Clin. Oral Implants Res. 2016, 27, 174–195. [Google Scholar] [CrossRef]
- Cristea, I.; Agop-Forna, D.; Martu, M.-A.; Dascălu, C.; Topoliceanu, C.; Török, R.; Török, B.; Bardis, D.; Bardi, P.M.; Forna, N. Oral and Periodontal Risk Factors of Prosthetic Success for 3-Unit Natural Tooth-Supported Bridges versus Implant-Supported Fixed Dental Prostheses. Diagnostics 2023, 13, 852. [Google Scholar] [CrossRef] [PubMed]
- Makary, C.; Menhall, A.; Zammarie, C.; Lombardi, T.; Lee, S.Y.; Stacchi, C.; Park, K.B. Primary Stability Optimization by Using Fixtures with Different Thread Depth According To Bone Density: A Clinical Prospective Study on Early Loaded Implants. Materials 2019, 12, 2398. [Google Scholar] [CrossRef]
- Parithimarkalaignan, S.; Padmanabhan, T.V. Osseointegration: An Update. J. Indian Prosthodont. Soc. 2013, 13, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Matys, J.; Świder, K.; Flieger, R.; Dominiak, M. Assessment of the Primary Stability of Root Analog Zirconia Implants Designed Using Cone Beam Computed Tomography Software by Means of the Periotest® Device: An Ex Vivo Study. A Preliminary Report. Adv. Clin. Exp. Med. 2017, 26, 803–809. [Google Scholar] [CrossRef]
- Stavropoulos, A.; Cochran, D.; Obrecht, M.; Pippenger, B.E.; Dard, M. Effect of Osteotomy Preparation on Osseointegration of Immediately Loaded, Tapered Dental Implants. Adv. Dent. Res. 2016, 28, 34–41. [Google Scholar] [CrossRef]
- Stocchero, M.; Toia, M.; Jinno, Y.; Cecchinato, F.; Becktor, J.P.; Naito, Y.; Halldin, A.; Jimbo, R. Influence of Different Drilling Preparation on Cortical Bone: A Biomechanical, Histological, and Micro-CT Study on Sheep. Clin. Oral Implants Res. 2018, 29, 707–715. [Google Scholar] [CrossRef]
- Marheineke, N.; Scherer, U.; Rücker, M.; von See, C.; Rahlf, B.; Gellrich, N.-C.; Stoetzer, M. Evaluation of Accuracy in Implant Site Preparation Performed in Single- or Multi-Step Drilling Procedures. Clin. Oral Investig. 2018, 22, 2057–2067. [Google Scholar] [CrossRef]
- Seymen, G.; Turgut, Z.; Berk, G.; Bodur, A. Implant Bed Preparation with an Erbium, Chromium Doped Yttrium Scandium Gallium Garnet (Er,Cr: YSGG) Laser Using Stereolithographic Surgical Guide. J. Lasers Med. Sci. 2013, 4, 25–32. [Google Scholar]
- Stacchi, C.; Troiano, G.; Montaruli, G.; Mozzati, M.; Lamazza, L.; Antonelli, A.; Giudice, A.; Lombardi, T. Changes in Implant Stability Using Different Site Preparation Techniques: Osseodensification Drills versus Piezoelectric Surgery. A Multi-center Prospective Randomized Controlled Clinical Trial. Clin. Implant Dent. Relat. Res. 2023, 25, 133–140. [Google Scholar] [CrossRef]
- Rastelli, C.; Falisi, G.; Gatto, R.; Galli, M.; Saccone, E.; Severino, M.; Di Paolo, C. Implant Stability in Different Techniques of Surgical Sites Preparation: An in Vitro Study. Oral Implantol. 2014, 7, 33–39. [Google Scholar] [CrossRef]
- Dominiak, M.; Matys, J. Assessment of Pain When Uncovering Implants with Er:YAG Laser or Scalpel for Second Stage Surgery. Adv. Clin. Exp Med 2016, 25, 1179–1184. [Google Scholar] [CrossRef] [PubMed]
- Matys, J.; Flieger, R.; Świder, K.; Gedrange, T.; Hutchings, G.; Dyszkiewicz-Konwińska, M.; Kempisty, B.; Nammour, S.; Dominiak, M.; Grzech-Leśniak, K. A Clinical Trial of Photobiomodulation Effect on Orthodontic Microscrews Stability Using a 635 Nm Red Laser Light. Photobiomodul. Photomed. Laser Surg. 2020, 38, 607–613. [Google Scholar] [CrossRef]
- Matys, J.; Flieger, R.; Gedrange, T.; Janowicz, K.; Kempisty, B.; Grzech-Leśniak, K.; Dominiak, M. Effect of 808 Nm Semiconductor Laser on the Stability of Orthodontic Micro-Implants: A Split-Mouth Study. Materials 2020, 13, 2265. [Google Scholar] [CrossRef]
- Krafft, T.; Graef, F.; Winter, W.; Wichmann, M.; Karl, M. Use of Osteotomes for Implant Bed Preparation—Effect on Material Properties of Bone and Primary Implant Stability. J. Oral Implantol. 2013, 39, 241–247. [Google Scholar] [CrossRef]
- Baldi, D.; Jones, J.M.; Lertora, E.; Burgio, C.; Lugas, A.T.; Schierano, G.; Colombo, J. Influence of Dental Implant Site Preparation Method on Three Aspects of the Site: Magnetodynamic Mallet versus Conventional Drill. Explor. Med. 2024, 5, 467–476. [Google Scholar] [CrossRef]
- Matys, J.; Świder, K.; Flieger, R. Laser Instant Implant Impression Method: A Case Presentation. Dent. Med. Probl. 2017, 54, 101–106. [Google Scholar] [CrossRef]
- Matys, J.; Hadzik, J.; Dominiak, M. Schneiderian Membrane Perforation Rate and Increase in Bone Temperature During Maxillary Sinus Floor Elevation by Means of Er: YAG Laser—An Animal Study in Pigs. Implant. Dent. 2017, 26, 238–244. [Google Scholar] [CrossRef]
- Matys, J.; Grzech-Leśniak, K.; Flieger, R.; Dominiak, M. Assessment of an Impact of a Diode Laser Mode with Wavelength of 980 Nm on a Temperature Rise Measured by Means of K-02 Thermocouple: Preliminary Results. Dent. Med. Probl. 2016, 53, 345–351. [Google Scholar] [CrossRef]
- Matys, J.; Flieger, R.; Dominiak, M. Assessment of Temperature Rise and Time of Alveolar Ridge Splitting by Means of Er:YAG Laser, Piezosurgery, and Surgical Saw: An Ex Vivo Study. BioMed Res. Int. 2016, 2016, 9654975. [Google Scholar] [CrossRef]
- Rugova, S.; Abboud, M. Thermal Evaluation of Bone Drilling with a One-Drill Protocol. Bioengineering 2024, 11, 1022. [Google Scholar] [CrossRef]
- Saxena, V.; Dhawan, P.; Rani, S. Effect of Guided Implant Drilling on Bone Temperature Changes During Implant Osteotomy: A Comprehensive Systematic Review. Cureus 2024, 16, e70216. [Google Scholar] [CrossRef] [PubMed]
- Aghvami, M.; Brunski, J.B.; Serdar Tulu, U.; Chen, C.-H.; Helms, J.A. A Thermal and Biological Analysis of Bone Drilling. J. Biomech. Eng. 2018, 140, 1010101–1010108. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A.; Tumedei, M.; Aramburú Júnior, J.; Treichel, T.L.E.; Kolerman, R.; Lepore, S.; Piattelli, A.; Iezzi, G. Histological and Histomorphometrical Evaluation of a New Implant Macrogeometry. A Sheep Study. Int. J. Environ. Res. Public Health 2020, 17, 3477. [Google Scholar] [CrossRef]
- Kosior, P.; Dobrzyński, M.; Wiśniewska, K.; Kulus, M.; Struzik, N.; Matys, J.; Kuropka, P. Comparative Analysis of the Histological Characteristics of Bone Tissue Following Implant Drill Preparation Under Various Parameters: An In Vitro Study. J. Clin. Med. 2025, 14, 2161. [Google Scholar] [CrossRef]
- Moradi Haghgoo, J.; Khoshhal, M.; Sharifi, S.; Khodadadi, I.; Ghadidmi Pour, H.; Seif Rabie, M.A.; Rabienejad, N. Determination of Osteoblast Cell Viability and Histological Changes of Samples Obtained from Different Implant Drills during Osteotomy. J. Dent. 2023, 24, 220–225. [Google Scholar] [CrossRef]
- Möhlhenrich, S.C.; Modabber, A.; Steiner, T.; Mitchell, D.A.; Hölzle, F. Heat Generation and Drill Wear during Dental Implant Site Preparation: Systematic Review. Br. J. Oral Maxillofac. Surg. 2015, 53, 679–689. [Google Scholar] [CrossRef]
- Baires-Campos, F.-E.; Jimbo, R.; Bonfante, E.-A.; Fonseca-Oliveira, M.-T.; Moura, C.; Zanetta-Barbosa, D.; Coelho, P.-G. Drilling Dimension Effects in Early Stages of Osseointegration and Implant Stability in a Canine Model. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e471–e479. [Google Scholar] [CrossRef]
- Tabrizi, R.; Nazhvanai, A.D.; Farahmand, M.M.; Pourali, S.Y.; Hosseinpour, S. Do Increased Drilling Speed and Depth Affect Bone Viability at Implant Site? Dent. Res. J. 2017, 14, 331–335. [Google Scholar] [CrossRef]
- Nkenke, E.; Fenner, M.; Vairaktaris, E.G.; Neukam, F.W.; Radespiel-Tröger, M. Immediate versus Delayed Loading of Dental Implants in the Maxillae of Minipigs. Part II: Histomorphometric Analysis. Int. J. Oral Maxillofac. Implants 2005, 20, 540–546. [Google Scholar]
- Stelzle, F.; Frenkel, C.; Riemann, M.; Knipfer, C.; Stockmann, P.; Nkenke, E. The Effect of Load on Heat Production, Thermal Effects and Expenditure of Time during Implant Site Preparation—An Experimental Ex Vivo Comparison between Piezosurgery and Conventional Drilling. Clin. Oral Implants Re.s 2014, 25, e140–e148. [Google Scholar] [CrossRef]
- Semez, G.; Cescato, A.; Luca, R.E.; Tonetti, L.; Todea, D.C. A Comparative Analysis Regarding the Osseointegration of Immediate Loaded Implants Using Two Different Implant Site Preparations: Erbium:Yttrium-Aluminum-Garnet Laser Versus Surgical Conventional Way-An In Vivo and Histological Animal Study. Photobiomodul. Photomed. Laser Surg. 2021, 39, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Schierano, G.; Baldi, D.; Peirone, B.; von Degerfeld, M.M.; Modica, F.; Notaro, V.; Boretto, C.; Muzio, G.; Autelli, R. Implant Stability Quotient and Osteogenic Process in Dental Implant Sites Prepared Using Piezoelectric Technique: A Study in Minipigs. J. Prosthodont. 2025; ahead of print. [Google Scholar] [CrossRef]
- Schierano, G.; Baldi, D.; Peirone, B.; Mauthe von Degerfeld, M.; Navone, R.; Bragoni, A.; Colombo, J.; Autelli, R.; Muzio, G. Biomolecular, Histological, Clinical, and Radiological Analyses of Dental Implant Bone Sites Prepared Using Magnetic Mallet Technology: A Pilot Study in Animals. Materials 2021, 14, 6945. [Google Scholar] [CrossRef]
- Kosior, P.; Kuropka, P.; Janeczek, M.; Mikulewicz, M.; Zakrzewski, W.; Dobrzyński, M. The Influence of Various Preparation Parameters on the Histological Image of Bone Tissue during Implant Bed Preparation—An In Vitro Study. Appl. Sci. 2021, 11, 1916. [Google Scholar] [CrossRef]
- Eom, T.-G.; Kim, H.-W.; Jeon, G.-R.; Yun, M.-J.; Huh, J.-B.; Jeong, C.-M. Effects of Different Implant Osteotomy Preparation Sizes on Implant Stability and Bone Response in the Minipig Mandible. Int. J. Oral Maxillofac. Implants 2016, 31, 997–1006. [Google Scholar] [CrossRef]
- Sakita, G.; Allegrini Junior, S.; Salles, M.B.; Batista, M.P.C.; Pistarini, L.Y.; Fraga, R.M.; Yoshimoto, M. Comparison between a Piezoelectric Device and Rotary Instruments in Implant Site Preparation: An in Vivo Morphological, Histological Analysis Using Pigs. RGO Rev. Gaúch. Odontol. 2015, 63, 47–54. [Google Scholar] [CrossRef]
- Fujiwara, S.; Botticelli, D.; Kaneko, N.; Urbizo Velez, J.; Tumedei, M.; Bengazi, F. Effect of Low-Speed Drilling without Irrigation on Osseointegration: An Experimental Study in Dogs. Oral Maxillofac. Surg. 2022, 26, 595–601. [Google Scholar] [CrossRef]
- Fujiwara, S.; Kato, S.; Bengazi, F.; Urbizo Velez, J.; Tumedei, M.; Kotsu, M.; Botticelli, D. Healing at Implants Installed in Osteotomies Prepared Either with a Piezoelectric Device or Drills: An Experimental Study in Dogs. Oral Maxillofac. Surg. 2021, 25, 65–73. [Google Scholar] [CrossRef]
- Yi, H.-Y.; Park, Y.-S.; Pippenger, B.E.; Lee, B.; Miron, R.J.; Dard, M. Dimensional Changes Following Immediate and Delayed Implant Placement: A Histomorphometric Study in the Canine. Int. J. Oral Maxillofac. Implants 2017, 32, 541–546. [Google Scholar] [CrossRef]
- Schwarz, F.; Olivier, W.; Herten, M.; Sager, M.; Chaker, A.; Becker, J. Influence of Implant Bed Preparation Using an Er:YAG Laser on the Osseointegration of Titanium Implants: A Histomorphometrical Study in Dogs. J. Oral Rehabil. 2007, 34, 273–281. [Google Scholar] [CrossRef]
- Cesaretti, G.; Lang, N.P.; Salata, L.A.; Schweikert, M.T.; Gutierrez Hernandez, M.E.; Botticelli, D. Sub-Crestal Positioning of Implants Results in Higher Bony Crest Resorption: An Experimental Study in Dogs. Clin. Oral Implants Res. 2015, 26, 1355–1360. [Google Scholar] [CrossRef]
- Pantani, F.; Botticelli, D.; Garcia, I.R.; Salata, L.A.; Borges, G.J.; Lang, N.P. Influence of Lateral Pressure to the Implant Bed on Osseointegration: An Experimental Study in Dogs. Clin. Oral Implants Res. 2010, 21, 1264–1270. [Google Scholar] [CrossRef] [PubMed]
- Al-Marshood, M.M.; Junker, R.; Al-Rasheed, A.; Al Farraj Aldosari, A.; Jansen, J.A.; Anil, S. Study of the Osseointegration of Dental Implants Placed with an Adapted Surgical Technique. Clin. Oral Implants Res. 2011, 22, 753–759. [Google Scholar] [CrossRef]
- Trisi, P.; Berardini, M.; Falco, A.; Podaliri Vulpiani, M.; Perfetti, G. Insufficient Irrigation Induces Peri-Implant Bone Resorption: An in Vivo Histologic Analysis in Sheep. Clin. Oral Implants Res. 2014, 25, 696–701. [Google Scholar] [CrossRef]
- Trisi, P.; Falco, A.; Berardini, M. Single-Drill Implant Induces Bone Corticalization during Submerged Healing: An in Vivo Pilot Study. Int. J. Implant Dent. 2020, 6, 2. [Google Scholar] [CrossRef] [PubMed]
- Trisi, P.; Berardini, M.; Falco, A.; Podaliri Vulpiani, M. New Osseodensification Implant Site Preparation Method to Increase Bone Density in Low-Density Bone: In Vivo Evaluation in Sheep. Implant Dent. 2016, 25, 24–31. [Google Scholar] [CrossRef]
- Stübinger, S.; Biermeier, K.; Bächi, B.; Ferguson, S.J.; Sader, R.; von Rechenberg, B. Comparison of Er:YAG Laser, Piezoelectric, and Drill Osteotomy for Dental Implant Site Preparation: A Biomechanical and Histological Analysis in Sheep. Lasers Surg. Med. 2010, 42, 652–661. [Google Scholar] [CrossRef]
- Rugova, S.; Abboud, M. Comparison of One-Drill Protocol to Sequential Drilling In Vitro and In Vivo. Bioengineering 2025, 12, 51. [Google Scholar] [CrossRef]
- Zizzari, V.L.; Berardi, D.; Congedi, F.; Tumedei, M.; Cataldi, A.; Perfetti, G. Morphological Aspect and iNOS and Bax Expression Modification in Bone Tissue Around Dental Implants Positioned Using Piezoelectric Bone Surgery Versus Conventional Drill Technique. J. Craniofacial Surg. 2015, 26, 741–744. [Google Scholar] [CrossRef]
- Zeitouni, J.; Clough, B.; Zeitouni, S.; Saleem, M.; Al Aisami, K.; Gregory, C. The Effects of the Er:YAG Laser on Trabecular Bone Micro-Architecture: Comparison with Conventional Dental Drilling by Micro-Computed Tomographic and Histological Techniques. F1000Res 2017, 6, 1133. [Google Scholar] [CrossRef]
- Scarano, A.; Iezzi, G.; Perrotti, V.; Tetè, S.; Staiti, G.; Mortellaro, C.; Cappucci, C. Ultrasonic versus Drills Implant Site Preparation: A Histologic Analysis in Bovine Ribs. J. Craniofacial Surg. 2014, 25, 814–817. [Google Scholar] [CrossRef]
- Semez, G.; Luca, R.E.; Cescato, A.; Faoro, V.; Mocuţa, D.E.; Todea, D.C.M. Effect of the Laser Beam on Implant Site Preparation: A Preliminary Pilot Study. Rom. J. Morphol. Embryol. 2018, 59, 861–867. [Google Scholar]
- Gaspar, J.; Borrecho, G.; Oliveira, P.; Salvado, F.; Martins dos Santos, J. Osteotomy at Low-Speed Drilling without Irrigation versus High-Speed Drilling with Irrigation: An Experimental Study. Acta Med. Port. 2013, 26, 231–236. [Google Scholar]
- Sirolli, M.; Mafra, C.E.S.; Santos, R.A.B.D.; Saraiva, L.; Holzhausen, M.; César, J.B. Influence of Piezosurgery on Bone Healing around Titanium Implants: A Histological Study in Rats. Braz. Dent. J. 2016, 27, 278–283. [Google Scholar] [CrossRef]
- Chen, C.-H.; Coyac, B.R.; Arioka, M.; Leahy, B.; Tulu, U.S.; Aghvami, M.; Holst, S.; Hoffmann, W.; Quarry, A.; Bahat, O.; et al. A Novel Osteotomy Preparation Technique to Preserve Implant Site Viability and Enhance Osteogenesis. J. Clin. Med. 2019, 8, 170. [Google Scholar] [CrossRef]
- Kesler, G.; Romanos, G.; Koren, R. Use of Er:YAG Laser to Improve Osseointegration of Titanium Alloy Implants—A Comparison of Bone Healing. Int. J. Oral Maxillofac. Implants 2006, 21, 375–379. [Google Scholar] [CrossRef]
- Conserva, E.; Lanuti, A.; Menini, M. Cell Behavior Related to Implant Surfaces with Different Microstructure and Chemical Composition: An in Vitro Analysis. Int. J. Oral Maxillofac. Implants 2010, 25, 1099–1107. [Google Scholar]
- Van Oirschot, B.A.J.A.; Zhang, Y.; Alghamdi, H.S.; Cordeiro, J.M.; Nagay, B.E.; Barao, V.A.R.; De Avila, E.D.; Van Den Beucken, J.J.J.P. Surface Engineering for Dental Implantology: Favoring Tissue Responses Along the Implant. Tissue Eng. Part A 2022, 28, 555–572. [Google Scholar] [CrossRef]
- Deng, T.-G.; Liu, P.; Zhou, H.-Z.; Xue, Y.; Zheng, X.-N.; Ji, Z.-H.; Wang, L.; Hu, K.-J.; Ding, Y.-X. Effect on Implant Drills and Postoperative Reactions for Pre-Extraction Interradicular Implant Bed Preparation during the COVID-19 Pandemic and Beyond. Medicine 2022, 101, e29249. [Google Scholar] [CrossRef]

| Study | Aim of the Study | Material and Methods | Results | Conclusions |
|---|---|---|---|---|
| Nkenke [39] | Analysis of histomorphometric parameters of implants implanted in the maxilla of minipigs. | In 9 mini-pigs, 4 teeth were extracted and 6 implants were placed in the maxilla, which were immediately or after 1, 2, 3, 4 and 5 months loaded with dentures. The implant beds were prepared using osteotomies or spiral drills. After 6 months of loading, the implants were removed, sectioned and the image digitally analyzed. | The palatal BIC was higher for the osteotome technique with healing up to 3 months, while it was higher for the drill with healing up to 4–5 months. The longer the healing time, the greater the resorption, regardless of the preparation technique used. | Healing time and implant site preparation technique influence histomorphometric parameters such as BIC and bone resorption. |
| Stubinger [57] | To assess how different implant site preparation techniques affect the osseointegration of titanium dental implants. | 108 titanium implants were placed in the pelvis of 6 sheep. Implant sites were prepared using a Er:YAG laser, piezoelectric device or conventional drills. After 4, 6 or 8 weeks, the BIC was assessed histologically, and implant stability was evaluated. Fluorochrome labeling with calcein green and xylenol orange was used to visualize bone remodeling. | Initial BIC values (4 weeks) were slightly higher in laser and piezoelectric groups versus drill osteotomy. At 6 weeks, the BIC decreased in the laser and piezoelectric groups but increased in the drill group. By 8 weeks, BIC improved in laser and piezoelectric groups. Removal torque testing showed the laser group had the highest values at 8 weeks. Fluorescence labeling demonstrated active bone remodeling in all groups. | Laser and piezoelectric osteotomy techniques showed comparable or superior results to conventional drilling for dental implant placement. Both alternative methods demonstrated favorable osseointegration by 8 weeks, with laser osteotomy achieving significantly higher mechanical stability. |
| Gaspar [63] | Comparison of histological changes after implant osteotomy preparation using low -speed drilling without irrigation and high-speed drilling with irrigation. | 36 implants were inserted into the tibias of the rabbits using 2 types of preparation speeds (low without irrigation and high with irrigation) using drills of increasing diameter. Samples were taken for histological analysis. | Histological analysis revealed no differences between the two surgical drilling techniques. | Both types of drillings similarly preserve bone cell viability, allowing the surgeon to choose the method based on other factors. |
| Scarano [61] | Comparison of two methods of bone preparation for implantation: piezoelectric and using a drill | In 10 beef ribs, 50 bone perforations were made using a drill and 50 using a piezoelectric device. The samples were sectioned and evaluated using a light microscope. | Bone preparation with a piezoelectric device resulted in a bone structure with fewer microcracks, a more regular structure of the bone edges and a histological image of the bone structure that was less disturbed compared to the method using a drill. | Bone prepared for implantation using a piezoelectric device has a more desirable structure than when using a drill. |
| Sakita [46] | Comparison of histomorphological aspects of bone tissue after osteotomy of porcine tibias using a piezoelectric system and rotary instruments, taking into account different postoperative periods. | After exposing the tibia in pigs, 4 preparations for dental implants were performed: 2 using classic drills, where the widest one had a diameter of 3 mm, and the others using a piezoelectric system. Then, the wounds were sutured. The animals were killed after 2, 7, 14 and 28 days. | After 2 days, the tissue edges were jagged after piezosurgery and smooth after using rotary instruments. After 7 days, greater osteogenesis was visible after using classical drills. After 14 days, the piezo group showed diffuse bone formation throughout the surgical site, with a vascular stroma composed of adipose tissue, the presence of bone trabeculae with osteocytes, and a peripheral line. In the rotational group, there was intensive neoformation of the 1/3 of the cortical and medullary bone starting with thicker trabecular bone in greater quantity and better organization. | Bone neoformation was more evident when the implant site was prepared using conventional rotary instruments. |
| Kesler [66] | To evaluate whether implant site preparation with an Er:YAG laser improves implant osseointegration. | The implantation site was prepared using an Er:YAG laser (test group) in 18 rats and a drill (control group) in 18 rats. Implant samples with surrounding bone were examined after 3 weeks or 3 months. %BIC was assessed. | %BIC after 3 weeks and 3 months was higher for the test group (Er:YAG laser). | Preparation of the implant site using an Er:YAG laser increases the successful implant osseointegration. |
| Semez [62] | To compare the histological effects of the Er:YAG laser and conventional tools on tissues during implant bed preparation. | The bovine tongue and rib were used for the study. A 5 mm Er:YAG laser scalpel and a conventional bur were used to prepare the holes. Each group consisted of six laser-prepared samples and one (soft tissue) or six (hard tissue) control samples. The tissues were fixed in 10% formalin, processed in ethanol, xylene, and paraffin, and analyzed microscopically after staining. | Implant bed prepared using conventional burs contains more debris and blood cells than laser treated samples. Thermal damage to soft tissue was observed with the laser’s MAX mode but not with the QSP mode. | Laser use for implant bone preparation is more promising in terms of successful osseointegration as it does not form debris in the implant bed. |
| Semez [41] | To evaluate the use of an Er:YAG laser for implant site preparation and reduce the time between primary and secondary stability, focusing on immediate occlusal loading in single implants. | The study included 6 minipigs that underwent implant site preparation using either a conventional bur kit or an Er:YAG laser. Four implants- positions 34, 37 (traditional burs) and 44, 47 (laser preparation) were placed in each pig. Bone samples were collected at 45, 60, 90 and 120 days post-surgery and subjected to the histological analysis. | Implants placed with the Er:YAG laser showed better bone healing and remodeling, especially in deeper areas, but with limited coronal bone-to-implant contact. In contrast, the bur-prepared sites had some implants fail due to necrotic or immature bone and weak coronal BIC. The laser promoted more consistent and less traumatic healing compared to the conventional bur method. | The use of the Er:YAG laser for implant site preparation results in higher-quality bone healing, with more lamellar bone and less necrosis compared to conventional drilling. |
| Schwarz [50] | To assess how using an Er:YAG laser for implant bed preparation affects the osseointegration of titanium dental implants compared to conventional drilling methods. | Implant sites in the lower jaw of 4 beagle dogs were prepared using either an Er:YAG laser or conventional drills. 24 implant channels were created, with 3 different commercial titanium implants randomly inserted into both sites. After healing periods of 2 and 12 weeks, the histological assessment was performed. | The Er:YAG laser preparation showed no thermal damage but created significantly wider peri-implant gaps and lower initial bone-to-implant contact at 2 weeks compared to conventional drilling. By 12 weeks, both methods achieved comparable osseointegration with mature lamellar bone formation, despite the laser method requiring significantly more preparation time. | Er:YAG laser could be a promising instrument for implant bed preparation. |
| Zeitouni [60] | Comparison of implant bed preparation: Er:Yag laser vs. conventional drilling technique. | Micro-computed tomographic histomorphometric analysis and histological examination were performed after bed preparation using different laser parameters and the conventional dental drill technique in the ovine femoral heads. | There was absence of trabecular collapse and reduced thermal and mechanical damage with Er:Yag laser preparation. | Laser cutting promotes tissue healing, unlike conventional drilling, which may delay healing through trabecular collapse and thermal damage. |
| Fujiwara [48] | To evaluate the effect of two methods of implant bed preparation: using a drill or piezoelectric device on osseointegration and bone level. | In 12 dogs, implantation beds were prepared using a piezoelectric device (test group) and drills (control group). Samples were examined after 4 and 8 weeks using an Eclipse Ci microscope. The following were assessed: IS-B and M-B distance, BIC, pre-existing bone and soft tissue. | The amount of bone formation was greater at 8 weeks than at 4 weeks regardless of the used method. Mean distance between B and M after 4 and 8 weeks was smaller in the piezoelectric group. | Both tested methods provide similar and satisfactory histomorphological parameters, which allows for proper osseointegration. |
| Stelzle [40] | To compare piezosurgery and conventional drilling for implant site preparation. | 360 implant beds were prepared on the porcine skull using a drill, trephine drill or piezoelectric device. The drills used external cooling, and the piezoelectric device used internal cooling. The samples were subjected to histomorphometric analysis. The following were examined: both sides of the cortical bone, the lateral walls of the prepared implant site on both sides and its bottom. | Thermal tissue changes increased with higher loads for both piezosurgery and trephine bur, with maximum effects at 900–1000 g for piezosurgery and 700–800 g for the trephine bur. The spiral bur showed the highest thermal effects at 400–500 g. The thermal changes were greatest in the cortical bone and a positive correlation was observed between load and thermal alterations for both techniques. | Piezosurgery causes significantly higher temperatures and more thermal tissue changes when the load exceeds 500 g and is slower compared to spiral bur and trephine bur for implant site preparation. |
| Schierano [42] | To investigate the early cellular and molecular processes involved in dental implant osseointegration when using piezoelectric surgery. | Two implant sites were created in the tibiae of four minipigs. After implantation cortical bone thickness and Implant Stability Quotient (ISQ) were measured. After 14 days CT scans and ISQ measurements were repeated. Bone sections were then processed for histological and biomolecular analyses. | 48% of the tissue around the implants was newly formed bone, with a high presence of osteoblasts. The thickness of this new bone ranged from 300 to 1600 μm. No osteoclasts were detected, and inflammatory cell presence was minimal. | Piezoelectric surgery promotes a favorable biological response at implant sites, marked by increased osteogenic factors and new bone formation. These changes are associated with improved implant stability, as indicated by higher ISQ values. |
| Sirolli [64] | To investigate the influence of conventional drilling and piezosurgery on bone healing around implants. | 15 male rats received titanium implants in their tibias, prepared with conventional drilling or piezosurgery. After 30 days, the histomorphometric evaluation was performed, comparing the BIC, bone area and mineralized tissue in cortical and cancellous regions. | Piezosurgery showed better bone healing in cancellous bone, with higher bone area and mineralized tissue percentage. Conventional drilling performed better in cortical bone, particularly for bone-to-implant contact. | The surgical preparation technique’s effectiveness varies depending on the bone region. |
| Zizzari [59] | Assessment of differences in bone tissue around dental implants after piezoelectric technique vs. conventional drilling technique preparation. | 24 dental implants were implanted using 2 different preparation techniques into the iliac crest of sheeps. Samples were collected for analysis after 15 and 30 days. | No statistically significant higher expression of iNos and Bax when using the conventional drill technique | Piezoelectric bed preparation technique may reduce peri-implant inflammation and improve bone tissue healing |
| Trisi [56] | To assess a new method for preparing implant sites that could improve the bone density, ridge width, and the stability of implants after placement. | Implants were inserted into the iliac bones of two sheep, with one side prepared with standard drilling and the other using the osseodensification method. After a healing period of two months, the animals were euthanized and biomechanical and histological evaluation was performed. | The drilling group showed a thin layer of new bone with some broken trabeculae and fragments. The bone densification group showed thicker bone at the implant site, especially at the top, with more active bone formation and higher bone density. The drilling group had approximately 30% greater bone volume (%BV), while there was no significant difference in BIC. | The osseodensification technique increased bone volume around implants in low-density bone compared to traditional drilling, which may help improve implant stability and reduce micromovement. |
| Schierano [43] | To evaluate whether the magneto-dynamic mallet technique is more effective than conventional drilling. | 12 titanium implants were placed in 3 male mini pigs tibias with half using each technique. Implant stability was measured immediately and after 14 days. Samples underwent histological and biomolecular assessment. | Mallet-prepared sites showed significantly better bone formation than drill sites, with higher bone percentage and osteoblast counts. The key findings include elevated BMP-4 expression, distinctive trabecular bone densification visible on CT around implants and elevated inflammatory markers, but balanced increased anti-inflammatory IL-10. Both techniques showed increased implant stability after 14 days. | The magneto-dynamic mallet technique effectively prepares sites for dental implants, creates more bone and osteoblasts than conventional drilling, which increases primary stability and promotes osteogenesis. This technique is less effective for dense bone but valuable for sites with thin cortex and poor bone quality. |
| Cesaretti [51] | Evaluation of soft and hard tissue integration around the implant using juxta or sub-crestally implantation. Comparison of site preparation using drills or sonic devices. | Implantation of two implants was performed at different bone depths in each of the six dogs. The test site was prepared 1.3 mm deeper than the control site. After 8 weeks, samples were taken for histological analysis. | The test sites showed greater bone loss and a more apical placement of the peri-implant mucosa. | The sub-crestal implant showed the greatest horizontal crestal bone loss. No significant differences between the bed preparation methods. |
| Trisi [54] | Evaluation of the effect of irrigation on implant osseointegration. | A total of 20 implants were implanted in the mandibles of 5 sheep. Depending on the cooling used during the procedure, they were divided into groups: A—no irrigation; B—internal irrigation; C—external irrigation; D—external and internal irrigation. After 2 months, histomorphometric and histological analysis was performed. | The studied parameters were more favorable in the groups in which irrigation was used, especially when internal or combined irrigation (external + internal) was used. | The presence of irrigation and its type have a significant impact on implant osseointegration. |
| Trisi [55] | Evaluation and comparison of two implant bed preparation protocols: single drill or drill sequence. | A total of 20 implants were implanted in 2 sheep. Half using 1 pilot drill and 10 implants using a drill sequence. After 2 months, the following parameters were assessed: %BIC, %BV, VAM, RT and ISQ. | In the test group, the studied histomorphometrical parameters were significantly higher. Osteocorticization and VAM was greater in the test group. | Implant placement using a drill sequence allows for better histomorphometric parameters and, as a result, better osteointegration of the implants. |
| Fujiwara [47] | Comparison of the effect on implant osseointegration of bed preparation with irrigation and high speed or without irrigation and low speed. | In 12 dogs, 3 months after tooth extraction, implantation sites were prepared: 1. irrigation + high speed 2. no irrigation + low speed. The implants were removed after 4 or 8 weeks. The following were assessed: BIC%, existing bone and soft tissue in contact with the implant. | The amount of new bone after 8 weeks was greater than after 4 weeks, regardless of the bed preparation method. Both methods tested gave similar %BIC parameters after 4 and 8 weeks. | Both methods tested have a similar effect on osseointegration. |
| Yi [49] | To compare hard tissue changes around titanium implants placed immediately after extraction versus after an 8-week healing period. | In 5 beagle dogs, mandibular premolars were extracted for experimental use. The left side assessed bone healing after extraction or site preparation, while the right side compared immediate and 8-week delayed implant placement. Bone regeneration, implant integration, and bone height were analyzed histologically. | Implant bed preparation resulted in greater bone height loss and lower bone area/total area (BATA) than regular extractions. Immediate implants showed more buccal and lingual bone loss compared to delayed implants. However, immediate placement achieved significantly higher bone-to-implant contact (BIC) | Implant bed preparation and immediate placement increased bone height loss, despite better implant integration. |
| Tabrizi [38] | To determine whether bone viability is affected by speed and depth of drilling. | 100 patients requiring mandibular first molar implants were divided into four equal groups with different drilling parameters: 1000 rpm/10 mm, 1500 rpm/10 mm, 1000 rpm/13 mm, and 1500 rpm/13 mm. Collected bone samples underwent histological processing at 200× magnification. | Bone viability was low across all groups, but significantly the lowest was the group with the following parameters: 1500 rpm/13 mm indicating that the combined increase in both speed and depth substantially reduced bone viability. | Increasing either drilling speed or drilling depth alone does not significantly affect bone viability while increasing both parameters significantly reduces viability of bone cells at the implant site. |
| Rugova and Abboud [58] | To assess the thermal effects and osseointegration outcomes of different dental implant drilling protocols. | 54 dental implants were inserted in 5 male sheep. The groups used different drilling techniques: a standard sequential protocol, a modified protocol with a new-generation drill bit, and a one-drill protocol. Two implant types were used. Histological analysis was conducted 3 weeks post-surgery. | The new-generation one-drill protocol generated significantly less heat, the one-drill protocol remained below 50 °C at all drilling depths, while the sequential drilling protocol consistently exceeded 50 °C, indicating potential thermal damage to bone tissue. Simplified drilling protocols showed slightly higher BIC compared to the traditional approach. The duration of the modified protocol was 2–4 min while the traditional protocol was 12 min. | Simplified drilling protocols using new-generation drill bits can reduce procedure time while maintaining comparable bone-to-implant contact. |
| Chen [65] | Assessment of implant healing and osteogenesis using a new preparation technique. | New drill design with low speed were used to prepare beds for implants. | This method reduced tissue overheating due to lower speed of preparation, | This method efficiently cuts bone at low rotational speeds, eliminating the need for irrigation while preserving osteocyte viability and accelerating bone reconstruction. |
| Kosior [44] | Microscopic analysis of the level of bone tissue deformation after drilling under variable conditions in three dental implant system—Straumann, Osstem and S-wide. | 27 samples—3 dental implant systems, 3 speeds: 800, 1200, 1500 rpm and 3 types of cooling—without irrigation; with using physiological saline at room temperature; with physiological saline at low temperature were used for this study. | All drilling systems showed satisfactory results when the rotational speed was kept below 800 rpm, regardless of the cooling temperature. | The Straumann system provides the optimal bone surface structure for successful osseointegration. |
| Pantani [52] | To investigate the influence of lateral pressure exerted on the implant bed as well as osseointegration and changes at the bone level. | In 6 Labradors, bilateral premolars were removed and first molars were hemisectioned. After 3 months, 2 implants of 3.75 mm diameter and 8.5 mm length were implanted on one side using a 3 mm diameter drill as the last. On the other side, the last drill was 2.8 mm in diameter. The dogs were euthanized after 4 months and a histopathological examination was performed. | All implants were integrated with mineralized bone, well embedded in a mature bone plate in the cortical compartment, the apical part of the implant was surrounded by bone marrow. The alveolar process was resorbed in both the premolar and molar regions. | In the case of conventional implant placement, lateral pressure on the walls of the implant bed has no influence on the osseointegration process. |
| Eom [45] | To investigate the influence of the implant and drill diameter on the implant stability and bone response. | In 10 pigs, the premolars and first molars of the mandible were removed. After 8 months, implants of 3.5 mm in diameter and 8.5 mm in length were implanted using different diameter end drills. Group I: 3 mm, group II: 3.3 mm, group III: 3.5 mm. One animal was killed immediately, the others after 1, 3 or 5 weeks. | In groups I and II, microcracks and collagen deformation were visible in the bone surrounding the implant. In group I, bone resorption reached 1.2 mm, and in group III, up to 0.5 mm. | Bone resorption and fibrous tissue formation occur when an implant is placed in overloaded bone and microcracks develop. |
| Al-Marshood [53] | To investigate the osseointegration of dental implants implanted in the mandible of dogs using the conventional or undersized technique. | Lower premolars were removed from 12 Beagle dogs. After 3 months, 4.1 mm diameter × 8.5 mm long implants were placed using a 3.8 mm diameter drill in group I and a 3.3 mm diameter drill in group II. The dogs were euthanized 3 months later. | In group II, the implant-to-bone contact occurred at or above the first screw thread of the implant. In half of the implants in group I, the first screw thread was not covered with bone tissue but with fibrous tissue. The bone-to-implant contact percentage (BIC%) was higher in group II. | Preparing the implant bed to be too small may improve the bone response to the implant. |
| Authors | Animal Model/Tissue Type/Samples Number | Site of Implant Placement/Bed Preparation | Implant Bed Preparation Methods/Surgical Technique | Healing Time | Results of Histological Analysis | Bone-to-Implant Contact (BIC%) |
|---|---|---|---|---|---|---|
| Nkenke [39] | 9 minipigs, 6 implant site preparations each | Maxilla | Spiral drill Osteotome | 0, 1, 2, 3, 4 or 5 months | No data. | Osteotome: 0 months: buccal-82 ± 7, palatal-79 ± 7 1–3 months: buccal-87 ± 10, palatal-82 ± 24 4–5 months: buccal-72 ± 22, palatal-75 ± 16 Spiral drills: 0 months: buccal 79 ± 6, palatal-59 ± 30 1–3 months: buccal-58 ± 31, palatal-53 ± 26 4–5 months: buccal-77 ± 22, palatal-76 ± 18 |
| Trisi [54] | 5 sheep bone, 20 implant site preparations | Mandible | Drill sequence 3.2 to 3.9 mm | 2 months | A (no irradiation)—complete bone resorption, no implant integration, necrosis, sequestrum, clearly visible inflammatory infiltrate. B (internal irradiation)—integration of all implants, noticeable bone remodeling, small defects present. C (external irradiation)—noticeable new bone formation and its remodeling, good integration of implants with bone. D (internal and external irradiation)—large areas of bone resorption present, noticeable inflammatory cells, areas integrated with preserved bone present. | Group A 15.068 ± 10.07 Group B 44.02 ± 8.29 Group C 41.198 ± 13.48 Group D 31.024 ± 8.21 |
| Trisi [55] | 2 sheep, 20 implant site preparations | Iliac crest | -Drill (1.8 mm) -control group -Drill (3.2 mm) -test group | 2 months | Control group: Thread areas not covered by bone are present. Tested group: Newly formed continuous bone layer around the implant is present; osteocorticization phenomenon is noticeable. | Test group: 70.91 ± 7.95 Control group: 49.33 ± 10.73 |
| Kesler [66] | 36 rats, 2 implant site preparation each | Tibia | -Er:YAG laser (Opus 20; Lumenis, Nowy Jork, NY) -Drill (1.3 mm) | 3 weeks and 3 months | After 3 weeks: The test group (laser) showed more new bone formation in contact with the implant than the control group (drill). After 3 months: Both groups showed the presence of new trabecular bone. | 3 weeks: laser: 59.48 control: 12.85 3 months: laser 73.54 control 32.65 |
| Fujiwara [47] | 12 dogs, 2 implant site preparation each | Mandible | -Drill (3 mm) | 4 and 8 weeks | In both groups, there was noticeable new bone growth after 4 and 8 weeks. | After 4 weeks: Low speed: 46.6 ± 7.3 High speed: 43.1 ± 6.8 After 8 weeks Low speed: 60.0 ± 11.1 High speed: 60.2 ± 6.2 |
| Fujiwara [48] | 12 dogs, 2 implant site preparation each | Mandible | -Piezoelectric device -Drill | 4 and 8 weeks | In both groups, new bone, osteoid tissue and marrow structures were present after 4 and 8 weeks. After 4 weeks, bone remnants were present in the drill group. | After 4 weeks piezoelectric: 54.9 ± 6.7 drill: 49.5 ± 14.4 After 8 weeks: piezoelectric: 67.4 ± 6.7 drill: 62.9 ± 12.5 |
| Semez [62] | 6 sheep (female), 108 implants (18 implants per sheep, 9 implants in each side of the pelvis) | Iliac bones of the pelvis | Er:YAG laser osteotomy Piezoelectric Drill | 4, 6 and 8 weeks | No signs of peri-implant hard and soft tissue inflammation or infection were found in any technique. Laser and piezoelectric technique is comparable to drill osteotomy concerning early osseointegration. | After 4 weeks: Laser = 74.51 (4.03) Piezoelectric = 75.14 (13.59) Drill = 72.92 (14.28) After 6 weeks: Laser = 52.85 (13.45) Piezoelectric = 52.92 (19.84) Drill = 75.97 (10.73) |
| Schierano [42] | 15 male Wistar rats, 2 implant sites each | Tibia | Piezoelectric osteotomy Drill | 30 days | Newly formed bone had similar characteristics to the original bone in both groups. Some areas of fibrosis were observed around all implants. Some areas exhibited mature Haversian matrix deposition constituting cortical and cancellous bone. Piezosurgery had higher values for bone area with the threads and proportion of mineralized tissue. | Drill = 80.42 ± 10.88 Piezo = 70.25 ± 16.93 |
| Cesaretti [51] | 6 Labradors × 4 implants | Mandibule, premolar and molar area | - Drill 3 mm (control) - Drill 2.8 mm Implant size 3.75 × 8.5 mm | 4 months | Premolar: 59 (14.7) Premolar control: 48.6 (8.8) Molar: 51.7 (16.2) Molar control: 54.1 (15.1) | |
| Zizzari [59] | 10 pigs × 6 implants | Mandible | - Drill 3 mm (G1) - Drill 3.3 mm (G2) - Drill 3.5 mm (G3) Implant size 3.5 × 8.5 mm | 0, 1, 3 or 5 weeks | In G1 and G2 there was a collagen deformation and microcracks. | Immediately: G1 = 85.5 ± 2.6 G2 = 56.0 ± 7.4 G3 = 0 ± 0 At week 5: G1 = 80.0 ± 11.6 G2 = 73.2 ± 18.1 G3 = 66.6 ± 14.9 |
| Zeitouni [60] | 12 Beagle dogs × 4 implants | Mandible | - Drill 3.8 mm (G1) - Drill 3.3 mm (G2) Implant size 4.1 × 8.5 mm | 3 months | In 50% of implants from G1 the first screw-thread was not covered with the bone. | G1 = 47.5 (11.7) G2 = 60.6 (14.2) |
| Yi [49] | 5 male sheep, 12 implant sites per each | Mandible | Control group (sequential protocol) Group A (modified protocol) Group B (one-drill protocol) | 3 weeks | Control group—irreversible tissue damage with immediate cell death. | No numeric data |
| Semez [41] | 4 Beagle dogs, 6 implant sites per animal | Mandible | Er:YAG laser osteotomy or drill | 2 or 12 weeks | The Er:YAG laser osteotomy resulted in wider peri-implant gaps. No signs of thermal side effects in either group. At 12 weeks: Ongoing undisturbed formation of new bone in both groups, with implants surrounded by mature lamellar bone. | No numeric data |
| Trisi [56] | 100 human | Mandible at the first molar site | Drill system | No data | All groups showed a low level of bone viability. Group: 1500 rpm, 13 mm significantly reduced the percentage of viable cells compared to all other groups. | No data |
| Stelzle [40] | 3 male adult minipigs, 4 implant sites per animal | Tibia | Magneto-dynamic mallet Drill | 0 or 14 days | In mallet sites compared to drill sites: Increase in newly formed bone, increase in bone percentage, increase in osteoblast number, smaller amount of fibrous tissue, lateral bone condensation (osseocondensation). | No data |
| Scarano [61] | 10 bovine bone, 100 implant site preparations | Rib | - Piezoelectric system - Drill (2 × 13 mm) | No data | Drill method: Bone chips; irregular bone surface; microcracks, osteocytes with damage Piezoelectric method: No microcracks; bone structure has greater regularity; osteocytes without damage | No data |
| Stubinger [57] | 6 Beagle dogs 12 implant site preparations | Mandible | Dill or piezo | 8 weeks | When the original position of the bony crest was taken into account, a higher bone loss and a more apical position of the peri-implant mucosa resulted at the test sites. | No data |
| Tabrizi [38] | 6 sheep 24 implant site preparation | Illac crest | Piezo or drill | 15 or 30 days | Piezoelectric—more rapid healing, more organized newly formed bone. | No data |
| Schierano [43] | Sheep | Femoral heads | Laser Er:YAG Drill 3 mm | 0 | Laser cutting preserves the trabecular structure at the margin cuts unlike conventional drilling. | No data |
| Schwarz [50] | 6 rabbits 36 implant site preparation | Tibia | Drill: 1.5 mm, 2.0 mm, 2.5 mm, 3.5 mm Low speed 50 rpm without irrigation vs. 800 rpm with irrigation | 0 | No histological differences between the two surgical drill technique in optical microscope. | No data |
| Sirolli [64] | 18 rats | Maxillary | Drill (1, 1.3 or 1.6 mm) New type of drill (1.0 or 1.6 mm) | 0.5/3/7 days | Less heat damage caused by new type of drill. Higher osteoclast marker TRAP after using conventional drill. | No data |
| Rugova and Abboud [58] | Pigs 27 boreholes | Porcine ribs | Drill (systems: Osstem 3.0 mm, Straumann 3.3 mm, S-wide 5.5 mm) | 0 | Osstem—smooth surface, no damage to surrounding tissues, bone structure unchanged, small chips, partial compression of the bone, signs of mild carbonization. Straumann—smooth surface, uneven drill holes, no signs of carbonization. Adjacent tissue without damage. S -wide—uneven but smooth surface without damage to adjacent tissues. | No data |
| Gaspar [63] | 4 pigs × 10 implants | Tibia | - Drill 3 mm - Piezoelectric system (Piezosonic Driller®) Drills: ESO 18D, ESO 19D, ESO 40A, ESO 40B, oscillating 27–31 Khz, power 50 W | 2, 7, 14 or 28 days | At 2 days: In rotary group smooth surface, in piezoelectric group irregular pattern. At 7 days: Greater osteogenesis in the rotary group. At 14 days: In piezoelectric group diffuse new bone formation, in rotary group intense bone formation with greater quantity and better organization. At 28 days: Mature bone in both groups. | No data |
| Technique | Osseointegration Rate/Earliest Observed Signs of Healing | Bone Structure After Healing | Technique Sensitivity | Advantages | References |
|---|---|---|---|---|---|
| Rotary Drill | Moderate—slower integration/after 3–4 weeks | Moderate new bone formation, but often with more irregularities and delayed organization | Low | Versatile and easy to control | [38,41,44,45,47,48,49,52,53,55,61,63,65,66] |
| Piezoelectric Surgery | Good, especially in cancellous bone/14–30 days | High osteoblast activity, early bone matrix formation, smooth osteotomy surfaces | High | Minimally invasive, supports osteogenesis | [40,42,46,48,51,57,59,61,64] |
| Er:YAG Laser | Variable/ 14–21 days | Early woven bone formation with minimal thermal effects and preserved bone structure | High | Minimal necrosis, no thermal damage | [40,41,50,57,60,62,66] |
| Osteotome | Fast during early healing/within 1 month | Dense and well-adapted Higher BIC in first 1–3 months, denser bone near implant threads | Moderate | Improved stability in soft bone | [39] |
| Magneto-dynamic Mallet | Very rapid/ 14 days (T14) | High osteoblast activity Significantly more newly formed bone, higher osteoblast count, less fibrous tissue | High | Accelerated healing, less fibrous tissue | [43] |
| Osseodensification | Moderate/by 60 days | Dense, granular microstructure Granular new bone formation, higher bone density despite similar BIC compared to drilling | Moderate | Increased density and primary stability | [56] |
| Authors | 1. Is It Clear in the Study What Is the “Cause” and What Is the “Effect”? | 2. Were the Participants Included in Any Comparisons Similar? | 3. Were the Participants Included in Any Comparisons Receiving Similar Treatment/Care, Other than the Exposure or Intervention of Interest? | 4. Was There a Control Group? | 5. Were There Multiple Measurements of the Outcome Both Pre and Post the Intervention/Exposure? | 6. Was a Follow up Completed, and If Not, Were the Differences Between Groups in Terms of Their Follow up Adequately Described and Analyzed? | 7. Were the Outcomes of the Participants Included in Any Comparisons Measured in the Same Way? | 8. Were the Outcomes Measured in a Reliable Way? | 9. Was Appropriate Statistical Analysis Used? |
|---|---|---|---|---|---|---|---|---|---|
| Nkenke [39] | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Scarano [61] | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Trisi [54] | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Trisi [55] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Kesler [66] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Fujiwara [47] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Fujiwara [48] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Semez [62] | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No |
| Trisi [56] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Stelzle [40] | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Semez [41] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Schierano [42] | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Yi [49] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Stubinger [57] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Tabrizi [38] | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes |
| Schierano [43] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Schwarz [50] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Sirolli [64] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Rugova and Abboud [58] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Cesaretti [51] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Zizzari [59] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Zeitouni [60] | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Gaspar [63] | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Chen [65] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Kosior [44] | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Pantani [52] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Eom [45] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Al-Marshood [53] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Sakita [46] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kosior, P.; Kiryk, S.; Kotela, A.; Kiryk, J.; Kensy, J.; Laszczyńska, M.; Michalak, M.; Matys, J.; Dobrzyński, M. Histological and Histomorphometric Insights into Implant Bed Preparation: A Systematic Review. J. Clin. Med. 2025, 14, 4538. https://doi.org/10.3390/jcm14134538
Kosior P, Kiryk S, Kotela A, Kiryk J, Kensy J, Laszczyńska M, Michalak M, Matys J, Dobrzyński M. Histological and Histomorphometric Insights into Implant Bed Preparation: A Systematic Review. Journal of Clinical Medicine. 2025; 14(13):4538. https://doi.org/10.3390/jcm14134538
Chicago/Turabian StyleKosior, Piotr, Sylwia Kiryk, Agnieszka Kotela, Jan Kiryk, Julia Kensy, Marzena Laszczyńska, Mateusz Michalak, Jacek Matys, and Maciej Dobrzyński. 2025. "Histological and Histomorphometric Insights into Implant Bed Preparation: A Systematic Review" Journal of Clinical Medicine 14, no. 13: 4538. https://doi.org/10.3390/jcm14134538
APA StyleKosior, P., Kiryk, S., Kotela, A., Kiryk, J., Kensy, J., Laszczyńska, M., Michalak, M., Matys, J., & Dobrzyński, M. (2025). Histological and Histomorphometric Insights into Implant Bed Preparation: A Systematic Review. Journal of Clinical Medicine, 14(13), 4538. https://doi.org/10.3390/jcm14134538








