Respiratory Depression in Non-Operating Room Anesthesia: An Overview
Abstract
1. Introduction
2. Adverse Respiratory Events
3. Standards and Recommendations for NORA
3.1. Pre-Procedural Standards
3.2. Intra-Procedural Standards
3.3. Post-Procedural Standards
4. Patient Population Considerations
4.1. Patient Selection
4.2. Considerations for Complex Patients in NORA Care
4.2.1. Geriatric Population
4.2.2. Obese Population
4.2.3. Obstructive Sleep Apnea
5. Monitoring in Non-Operating Room Anesthesia
5.1. Current Practices and Relevance
5.2. Oxygenation Monitoring
5.3. Ventilation Monitoring
5.4. Modalities for Reduction in Airway Obstruction
5.5. Future Direction
6. Cultural Considerations in NORA
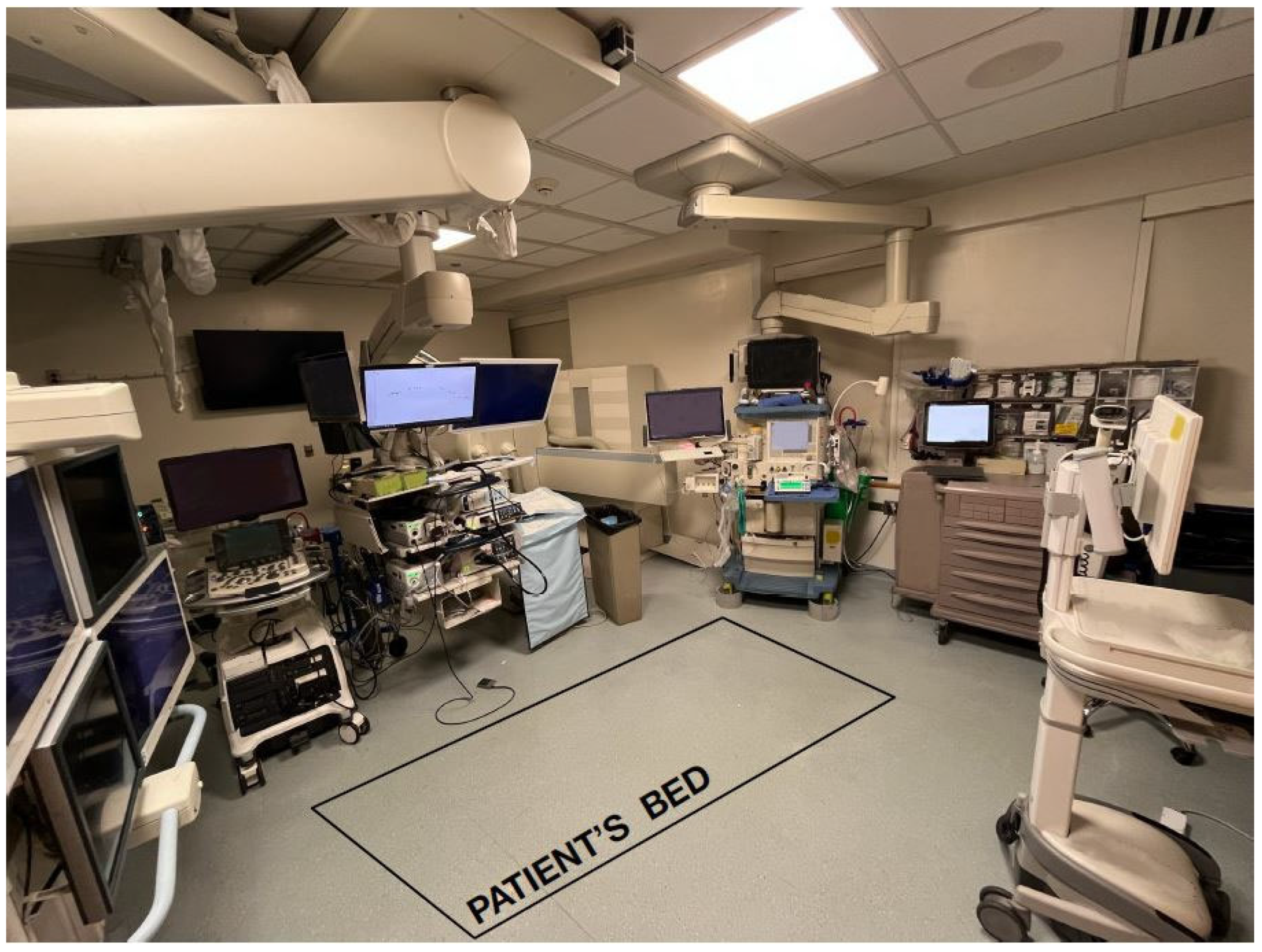
6.1. Physical Constraints
6.2. Team Familiarity
7. Post-Operative Care Considerations
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ABW | Actual Body Weight |
| APSF | Anesthesia Patient Safety Foundation |
| ASA | American Society of Anesthesia |
| BMI | Body Mass Index |
| CO2 | Carbon Dioxide |
| CPAP | Continuous Positive Airway Pressure |
| GA | General Anesthesia |
| GI | Gastrointestinal/Gastroenterology |
| HFNC | High Flow Nasal Cannula |
| LBW | Lean Body Weight |
| MAC | Monitored Anesthesia Care |
| NORA | Non-Operating Room Anesthesia |
| OR | Operating Room |
| OSA | Obstructive Sleep Apnea |
| PACU | Post Anesthesia Care Unit |
| PADS | Post-Anesthetic Discharge Score |
| PARS | Post-Anesthetic Recovery Score |
| SpO2 | Oxygen Saturation |
References
- Nagrebetsky, A.; Gabriel, R.A.; Dutton, R.P.; Urman, R.D. Growth of Nonoperating Room Anesthesia Care in the United States: A Contemporary Trends Analysis. Anesth. Analg. 2017, 124, 1261–1267. [Google Scholar] [CrossRef] [PubMed]
- Georgiadis, P.L.; Tsai, M.H.; Routman, J.S. Patient selection for nonoperating room anesthesia. Curr. Opin. Anaesthesiol. 2024, 37, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Boggs, S.D.; Barnett, S.R.; Urman, R.D. The future of nonoperating room anesthesia in the 21st century: Emphasis on quality and safety. Curr. Opin. Anaesthesiol. 2017, 30, 644–651. [Google Scholar] [CrossRef] [PubMed]
- Beard, J.; Methangkool, E.; Angus, S.; Urman, R.D.; Cole, D.J. Consensus Recommendations for the Safe Conduct of Nonoperating Room Anesthesia: A Meeting Report From the 2022 Stoelting Conference of the Anesthesia Patient Safety Foundation. Anesth. Analg. 2023, 137, e8–e11. [Google Scholar] [CrossRef]
- Herman, A.D.; Jaruzel, C.B.; Lawton, S.; Tobin, C.D.; Reves, J.G.; Catchpole, K.R.; Alfred, M.C. Morbidity, mortality, and systems safety in non-operating room anaesthesia: A narrative review. Br. J. Anaesth. 2021, 127, 729–744. [Google Scholar] [CrossRef]
- Lebak, K.; Lane, J.; Taus, R.; Kim, H.; Stecker, M.S.; Hall, M.; Lane-Fall, M.B.; Weiss, M.S. Building and Maintaining Organizational Infrastructure to Attain Clinical Excellence. Anesthesiol. Clin. 2017, 35, 559–568. [Google Scholar] [CrossRef]
- Stone, A.B.; Brovman, E.Y.; Greenberg, P.; Urman, R.D. A medicolegal analysis of malpractice claims involving anesthesiologists in the gastrointestinal endoscopy suite (2007–2016). J. Clin. Anesth. 2018, 48, 15–20. [Google Scholar] [CrossRef]
- Clergue, F. The challenges of anaesthesia for the next decade: The Sir Robert Macintosh Lecture 2014. Eur. J. Anaesthesiol. EJA 2015, 32, 223–229. [Google Scholar] [CrossRef]
- Abdelmalak, B.; Burkle, C.M.; Marco, A.P.; Mathews, D.M. Non-Operating Room Anesthesia: Patient Safety, Scheduling, Efficiency and Effective Leadership. SAMBA 2019, e18. [Google Scholar]
- American Society of Anesthesiologists. Statement on Granting Privileges for Administration of Moderate Sedation to Practitioners Who Are Not Anesthesia Professionals. 2021. Available online: https://www.asahq.org/standards-and-practice-parameters/statement-on-granting-privileges-for-administration-of-moderate-sedation-to-practitioners-who-are-not-anesthesia-professionals (accessed on 24 April 2025).
- Chang, B.; Kaye, A.D.; Diaz, J.H.; Westlake, B.; Dutton, R.P.; Urman, R.D. Interventional Procedures Outside of the Operating Room: Results From the National Anesthesia Clinical Outcomes Registry. J. Patient Saf. 2018, 14, 9–16. [Google Scholar] [CrossRef]
- Chang, B.; Urman, R.D. Non-operating Room Anesthesia: The Principles of Patient Assessment and Preparation. Anesthesiol. Clin. 2016, 34, 223–240. [Google Scholar] [CrossRef] [PubMed]
- Eichhorn, V.; Henzler, D.; Murphy, M.F. Standardizing care and monitoring for anesthesia or procedural sedation delivered outside the operating room. Curr. Opin. Anaesthesiol. 2010, 23, 494–499. [Google Scholar] [CrossRef]
- Youn, A.M.; Ko, Y.K.; Kim, Y.H. Anesthesia and sedation outside of the operating room. Korean J. Anesthesiol. 2015, 68, 323–331. [Google Scholar] [CrossRef]
- Yeh, T.; Beutler, S.S.; Urman, R.D. What we can learn from nonoperating room anesthesia registries: Analysis of clinical outcomes and closed claims data. Curr. Opin. Anaesthesiol. 2020, 33, 527–532. [Google Scholar] [CrossRef]
- American Society of Anesthesiologists. Statement on Safe Use of Propofol. 2024. Available online: https://www.asahq.org/standards-and-practice-parameters/statement-on-safe-use-of-propofol (accessed on 24 April 2025).
- Robbertze, R.; Posner, K.L.; Domino, K.B. Closed claims review of anesthesia for procedures outside the operating room. Curr. Opin. Anaesthesiol. 2006, 19, 436–442. [Google Scholar] [CrossRef]
- Metzner, J.; Posner, K.L.; Domino, K.B. The risk and safety of anesthesia at remote locations: The US closed claims analysis. Curr. Opin. Anaesthesiol. 2009, 22, 502–508. [Google Scholar] [CrossRef]
- Walls, J.D.; Weiss, M.S. Safety in Non-Operating Room Anesthesia (NORA). APSF Newsletter 2019, 34, 3–4. Available online: https://www.apsf.org/article/safety-in-non-operating-room-anesthesia-nora/ (accessed on 24 April 2025).
- Lai, Y.C.; Manninen, P.H. Anesthesia for cerebral aneurysms: A comparison between interventional neuroradiology and surgery. Can. J. Anaesth. 2001, 48, 391–395. [Google Scholar] [CrossRef]
- Melloni, C. Anesthesia and sedation outside the operating room: How to prevent risk and maintain good quality. Curr. Opin. Anaesthesiol. 2007, 20, 513–519. [Google Scholar] [CrossRef]
- Woodward, Z.G.; Urman, R.D.; Domino, K.B. Safety of Non-Operating Room Anesthesia: A Closed Claims Update. Anesthesiol. Clin. 2017, 35, 569–581. [Google Scholar] [CrossRef]
- Bhananker, S.M.; Posner, K.L.; Cheney, F.W.; Caplan, R.A.; Lee, L.A.; Domino, K.B. Injury and liability associated with monitored anesthesia care: A closed claims analysis. Anesthesiology 2006, 104, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Du, A.L.; Robbins, K.; Waterman, R.S.; Urman, R.D.; Gabriel, R.A. National trends in nonoperating room anesthesia: Procedures, facilities, and patient characteristics. Curr. Opin. Anaesthesiol. 2021, 34, 464–469. [Google Scholar] [CrossRef] [PubMed]
- Shah, D.; Sen, J.; Bawiskar, D. Non-operating Room Anesthesia (NORA): A Comprehensive Review of Monitored Anesthesia Care. Cureus 2024, 16, e68024. [Google Scholar] [CrossRef] [PubMed]
- Muir, A.; Hart, R. Non-operating room anaesthesia: General considerations. Anaesth. Intensive Care Med. 2023, 24, 412–415. [Google Scholar] [CrossRef]
- Metzner, J.; Domino, K.B. Risks of anesthesia or sedation outside the operating room: The role of the anesthesia care provider. Curr. Opin. Anaesthesiol. 2010, 23, 523–531. [Google Scholar] [CrossRef]
- Borshoff, D.C.; Sadleir, P. Nonoperating room anaesthesia: Safety, monitoring, cognitive aids and severe acute respiratory syndrome coronavirus 2. Curr. Opin. Anaesthesiol. 2020, 33, 554–560. [Google Scholar] [CrossRef]
- Choi, J.W.; Kim, D.K.; Lee, S.H.; Shin, H.S.; Seong, B.G. Comparison of Safety Profiles between Non-operating Room Anesthesia and Operating Room Anesthesia: A Study of 199,764 Cases at a Korean Tertiary Hospital. J. Korean Med. Sci. 2018, 33, e183. [Google Scholar] [CrossRef]
- American Society of Anesthesiologists. Statement on Distinguishing Monitored Anesthesia Care (“MAC”) from Moderate Sedation/Analgesia (Conscious Sedation). 2023. Available online: https://www.asahq.org/standards-and-practice-parameters/statement-on-distinguishing-monitored-anesthesia-care-from-moderate-sedation-analgesia (accessed on 24 April 2025).
- Benzoni, T.; Agarwal, A.; Cascella, M. Procedural Sedation. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2025. [Google Scholar]
- Janik, L.S.; Stamper, S.; Vender, J.S.; Troianos, C.A. Pro-Con Debate: Monitored Anesthesia Care Versus General Endotracheal Anesthesia for Endoscopic Retrograde Cholangiopancreatography. Anesth. Analg. 2022, 134, 1192–1200. [Google Scholar] [CrossRef]
- Das, S.; Ghosh, S. Monitored anesthesia care: An overview. J. Anaesthesiol. Clin. Pharmacol. 2015, 31, 27–29. [Google Scholar] [CrossRef]
- Van De Velde, M.; Kuypers, M.; Teunkens, A.; Devroe, S. Risk and safety of anesthesia outside the operating room. Minerva Anestesiol. 2009, 75, 345–348. [Google Scholar]
- Urdaneta, F.; Wardhan, R.; Wells, G.; White, J.D. Prevention of pulmonary complications in sedated patients undergoing interventional procedures in the nonoperating room anesthesia setting. Curr. Opin. Anaesthesiol. 2022, 35, 493–501. [Google Scholar] [CrossRef] [PubMed]
- American Society of Anesthesiologists. Statement on Nonoperating Room Anesthesia Services. 2023. Available online: https://www.asahq.org/standards-and-practice-parameters/statement-on-nonoperating-room-anesthesia-services (accessed on 10 February 2025).
- American Society of Anesthesiologists. Standards for Postanesthesia Care. 2024. Available online: https://www.asahq.org/standards-and-practice-parameters/standards-for-postanesthesia-care (accessed on 10 February 2025).
- American Society of Anesthesiologists. Standards for Basic Anesthetic Monitoring. 2020. Available online: https://www.asahq.org/standards-and-practice-parameters/standards-for-basic-anesthetic-monitoring (accessed on 11 March 2025).
- American Society of Anesthesiologists. Basic Standards for Preanesthesia Care. 2020. Available online: https://www.asahq.org/standards-and-practice-parameters/basic-standards-for-preanesthesia-care (accessed on 1 April 2025).
- Lagina, M.; Valley, T.S. Diagnosis and Management of Acute Respiratory Failure. Crit. Care Clin. 2024, 40, 235–253. [Google Scholar] [CrossRef]
- Lefebvre, P.A. Non-Operating Room Anesthesia: Closed Claim Review and Analysis. APSF Newsl. 2023, 38, 13–14. Available online: https://www.apsf.org/article/non-operating-room-anesthesia-closed-claim-review-and-analysis/ (accessed on 1 April 2025).
- Association of periOperative Registered, N. AORN Guidance Statement: Postoperative patient care in the ambulatory surgery setting. AORN J. 2005, 81, 881–888. [Google Scholar] [CrossRef]
- Sohn, H.M.; Ryu, J.H. Monitored anesthesia care in and outside the operating room. Korean J. Anesthesiol. 2016, 69, 319–326. [Google Scholar] [CrossRef]
- American Society of Anesthesiologists. Statement on ASA Physical Status Classification System. 2020. Available online: https://www.asahq.org/standards-and-practice-parameters/statement-on-asa-physical-status-classification-system#:~:text=ASA%20IV,not%20undergoing%20regularly%20scheduled%20dialysis (accessed on 25 April 2025).
- Committee on Standards and Practice Parameters; Apfelbaum, J.L.; Connis, R.T.; Nickinovich, D.G.; American Society of Anesthesiologists Task Force on Preanesthesia Evaluation; Pasternak, L.R.; Arens, J.F.; Caplan, R.A.; Connis, R.T.; Fleisher, L.A.; et al. Practice advisory for preanesthesia evaluation: An updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology 2012, 116, 522–538. [Google Scholar] [CrossRef]
- Tolep, K.; Higgins, N.; Muza, S.; Criner, G.; Kelsen, S.G. Comparison of diaphragm strength between healthy adult elderly and young men. Am. J. Respir. Crit. Care Med. 1995, 152, 677–682. [Google Scholar] [CrossRef]
- Mittman, C.; Edelman, N.H.; Norris, A.H.; Shock, N.W. Relationship Between Chest Wall and Pulmonary Compliance and Age. J. Appl. Physiol. 1965, 20, 1211–1216. [Google Scholar] [CrossRef]
- Kim, J.; Heise, R.L.; Reynolds, A.M.; Pidaparti, R.M. Aging effects on airflow dynamics and lung function in human bronchioles. PLoS ONE 2017, 12, e0183654. [Google Scholar] [CrossRef]
- Sharma, G.; Goodwin, J. Effect of aging on respiratory system physiology and immunology. Clin. Interv. Aging 2006, 1, 253–260. [Google Scholar] [CrossRef]
- Turnheim, K. When drug therapy gets old: Pharmacokinetics and pharmacodynamics in the elderly. Exp. Gerontol. 2003, 38, 843–853. [Google Scholar] [CrossRef] [PubMed]
- Mangoni, A.A.; Jackson, S.H. Age-related changes in pharmacokinetics and pharmacodynamics: Basic principles and practical applications. Br. J. Clin. Pharmacol. 2004, 57, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Mercadante, S.; Arcuri, E. Opioids and renal function. J. Pain. 2004, 5, 2–19. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; Cao, Q.; Hong, A.; Gu, Z.; Jian, J.; Liang, X. Incidence of respiratory depression between ciprofol and propofol after anesthesia: A systematic review and meta-analysis. Medicine 2024, 103, e40037. [Google Scholar] [CrossRef]
- World Health Organization. Obesity and Overweight [Fact Sheet]; World Health Organization: Geneva, Switzerland, 2024. [Google Scholar]
- Pouwels, S.; Smeenk, F.W.; Manschot, L.; Lascaris, B.; Nienhuijs, S.; Bouwman, R.A.; Buise, M.P. Perioperative respiratory care in obese patients undergoing bariatric surgery: Implications for clinical practice. Respir. Med. 2016, 117, 73–80. [Google Scholar] [CrossRef]
- Pelosi, P.; Croci, M.; Ravagnan, I.; Tredici, S.; Pedoto, A.; Lissoni, A.; Gattinoni, L. The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth. Analg. 1998, 87, 654–660. [Google Scholar] [CrossRef]
- Urdaneta, F. NORA Airway Management. In Anesthesiology News; McMahon Publishing: New York, NY, USA, 2020; pp. 7–12. [Google Scholar]
- Ingrande, J.; Lemmens, H.J. Dose adjustment of anaesthetics in the morbidly obese. Br. J. Anaesth. 2010, 105 (Suppl. 1), i16–i23. [Google Scholar] [CrossRef]
- Janmahasatian, S.; Duffull, S.B.; Ash, S.; Ward, L.C.; Byrne, N.M.; Green, B. Quantification of lean bodyweight. Clin. Pharmacokinet. 2005, 44, 1051–1065. [Google Scholar] [CrossRef]
- MacDonald, J.J.; Moore, J.; Davey, V.; Pickering, S.; Dunne, T. The weight debate. J. Intensive Care Soc. 2015, 16, 234–238. [Google Scholar] [CrossRef]
- Emmerich, S.D.; Fryar, C.D.; Stierman, B.; Ogden, C.L. Obesity and Severe Obesity Prevalence in Adults: United States, August 2021–August 2023; NCHS Data Brief, no 508; National Center for Health Statistics: Hyattsville, MD, USA, 2024. [CrossRef]
- American Society of Anesthesiologists Task Force. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: An updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology 2014, 120, 268–286. [Google Scholar] [CrossRef]
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pepin, J.L.; et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef] [PubMed]
- Eastwood, P.R.; Platt, P.R.; Shepherd, K.; Maddison, K.; Hillman, D.R. Collapsibility of the upper airway at different concentrations of propofol anesthesia. Anesthesiology 2005, 103, 470–477. [Google Scholar] [CrossRef]
- Walls, J.D.; Bramble, W.J., Jr.; Weiss, M.S. Safety in the nonoperating room anesthesia suite is not an accident: Lessons from the National Transportation Safety Board. Curr. Opin. Anaesthesiol. 2019, 32, 504–510. [Google Scholar] [CrossRef]
- American Lung Association. Pulse Oximetry. American Lung Association. 2024. Available online: https://www.lung.org/lung-health-diseases/lung-procedures-and-tests/pulse-oximetry (accessed on 11 March 2025).
- Maisel, W. FDA in Brief: FDA Warns About Limitations and Accuracy of Pulse Oximeters; U.S. Food and Drug Administration: Silver Spring, MD, USA, 2021.
- Singh, S.; Bennett, M.R.; Chen, C.; Shin, S.; Ghanbari, H.; Nelson, B.W. Impact of Skin Pigmentation on Pulse Oximetry Blood Oxygenation and Wearable Pulse Rate Accuracy: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2024, 26, e62769. [Google Scholar] [CrossRef]
- Al-Halawani, R.; Charlton, P.H.; Qassem, M.; Kyriacou, P.A. A review of the effect of skin pigmentation on pulse oximeter accuracy. Physiol. Meas. 2023, 44, 05TR01. [Google Scholar] [CrossRef]
- Soto, R.G.; Fu, E.S.; Vila, H., Jr.; Miguel, R.V. Capnography accurately detects apnea during monitored anesthesia care. Anesth. Analg. 2004, 99, 379–382. [Google Scholar] [CrossRef]
- Downs, J.B. Prevention of Hypoxemia: The Simple, Logical, but Incorrect Solution. J. Clin. Anesth. 1994, 6, 180–181. [Google Scholar] [CrossRef]
- Fu, E.S.; Downs, J.B.; Schweiger, J.W.; Miguel, R.V.; Smith, R.A. Supplemental oxygen impairs detection of hypoventilation by pulse oximetry. Chest 2004, 126, 1552–1558. [Google Scholar] [CrossRef]
- McGrath, S.P.; Perreard, I.M.; McGovern, K.M.; Blike, G.T. Understanding the “alarm problem” associated with continuous physiologic monitoring of general care patients. Resusc. Plus 2022, 11, 100295. [Google Scholar] [CrossRef]
- Harskamp, R.E.; Bekker, L.; Himmelreich, J.C.L.; De Clercq, L.; Karregat, E.P.M.; Sleeswijk, M.E.; Lucassen, W.A.M. Performance of popular pulse oximeters compared with simultaneous arterial oxygen saturation or clinical-grade pulse oximetry: A cross-sectional validation study in intensive care patients. BMJ Open Respir. Res. 2021, 8, e000939. [Google Scholar] [CrossRef]
- Arthur, J.; Hui, D. Safe Opioid Use: Management of Opioid-Related Adverse Effects and Aberrant Behaviors. Hematol. Oncol. Clin. North. Am. 2018, 32, 387–403. [Google Scholar] [CrossRef] [PubMed]
- Conway, A.; Douglas, C.; Sutherland, J. Capnography monitoring during procedural sedation and analgesia: A systematic review protocol. Syst. Rev. 2015, 4, 92. [Google Scholar] [CrossRef] [PubMed]
- Cacho, G.; Perez-Calle, J.L.; Barbado, A.; Lledo, J.L.; Ojea, R.; Fernandez-Rodriguez, C.M. Capnography is superior to pulse oximetry for the detection of respiratory depression during colonoscopy. Rev. Esp. Enferm. Dig. 2010, 102, 86–89. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Qadeer, M.A.; Vargo, J.J.; Dumot, J.A.; Lopez, R.; Trolli, P.A.; Stevens, T.; Parsi, M.A.; Sanaka, M.R.; Zuccaro, G. Capnographic monitoring of respiratory activity improves safety of sedation for endoscopic cholangiopancreatography and ultrasonography. Gastroenterology 2009, 136, 1568–1576; quiz 1819–1820. [Google Scholar] [CrossRef]
- Berry, J. Carbon Dioxide Used as Insufflating Gas May Raise ETCO2 During GI Endoscopy; Anesthesia Patient Safety Foundation: Rochester, MN, USA, 2018. [Google Scholar]
- Blonder, Y.; Mazor, E.; Jew, K. Advanced Capnography Sampling Lines May Improve Patient Comfort and Compliance. Med. Devices 2021, 14, 37–42. [Google Scholar] [CrossRef]
- Mirunalini, G.; Anand, K.; Pushparani, A.; Kadirvelu, G. Comparison of High Flow Nasal Cannula and Continuous Positive Airway Pressure in COVID-19 Patients With Acute Respiratory Distress Syndrome in Critical Care Unit: A Randomized Control Study. Cureus 2023, 15, e45798. [Google Scholar] [CrossRef]
- Pinto, V.L.; Sankari, A.; Sharma, S. Continuous Positive Airway Pressure. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2025. [Google Scholar]
- Vetrugno, L.; Deana, C.; Colaianni-Alfonso, N.; Tritapepe, F.; Fierro, C.; Maggiore, S.M. Noninvasive respiratory support in the perioperative setting: A narrative review. Front Med. 2024, 11, 1364475. [Google Scholar] [CrossRef]
- Sharma, S.; Danckers, M.; Sanghavi, D.K.; Chakraborty, R.K. High-Flow Nasal Cannula. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2025. [Google Scholar]
- Tao, Y.; Sun, M.; Miao, M.; Han, Y.; Yang, Y.; Cong, X.; Zhang, J. High flow nasal cannula for patients undergoing bronchoscopy and gastrointestinal endoscopy: A systematic review and meta-analysis. Front. Surg. 2022, 9, 949614. [Google Scholar] [CrossRef]
- Syversen, A.; Dosis, A.; Jayne, D.; Zhang, Z. Wearable Sensors as a Preoperative Assessment Tool: A Review. Sensors 2024, 24, 482. [Google Scholar] [CrossRef]
- Hussain, T.; Ullah, S.; Fernandez-Garcia, R.; Gil, I. Wearable Sensors for Respiration Monitoring: A Review. Sensors 2023, 23, 7518. [Google Scholar] [CrossRef]
- Al-Khalidi, F.Q.; Saatchi, R.; Burke, D.; Elphick, H.; Tan, S. Respiration rate monitoring methods: A review. Pediatr. Pulmonol. 2011, 46, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Vitazkova, D.; Foltan, E.; Kosnacova, H.; Micjan, M.; Donoval, M.; Kuzma, A.; Kopani, M.; Vavrinsky, E. Advances in Respiratory Monitoring: A Comprehensive Review of Wearable and Remote Technologies. Biosensors 2024, 14, 90. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.K.; Yang, H.L.; Jung, C.W.; Lee, H.C. Artificial intelligence in perioperative medicine: A narrative review. Korean J. Anesthesiol. 2022, 75, 202–215. [Google Scholar] [CrossRef] [PubMed]
- Khanna, A.K.; Bergese, S.D.; Jungquist, C.R.; Morimatsu, H.; Uezono, S.; Lee, S.; Ti, L.K.; Urman, R.D.; McIntyre, R., Jr.; Tornero, C.; et al. Prediction of Opioid-Induced Respiratory Depression on Inpatient Wards Using Continuous Capnography and Oximetry: An International Prospective, Observational Trial. Anesth. Analg. 2020, 131, 1012–1024. [Google Scholar] [CrossRef]
- Schroeck, H.; Whitty, M.A.; Martinez-Camblor, P.; Voicu, S.; Burian, B.K.; Taenzer, A.H. Anaesthesia clinicians’ perception of safety, workload, anxiety, and stress in a remote hybrid suite compared with the operating room. Br. J. Anaesth. 2023, 131, 598–606. [Google Scholar] [CrossRef]
- Bouhenguel, J.T.; Preiss, D.A.; Urman, R.D. Implementation and Use of Anesthesia Information Management Systems for Non-operating Room Locations. Anesthesiol. Clin. 2017, 35, 583–590. [Google Scholar] [CrossRef]
- Chang, C.; Tan, J.; Mack, P.F.; Anca, D. Clinician Safety in NORA. APSF Newsl. 2023, 38, 84–86. Available online: https://www.apsf.org/article/clinician-safety-in-nora/ (accessed on 13 May 2025).
- Frankel, A. Patient safety: Anesthesia in remote locations. Anesthesiol. Clin. 2009, 27, 127–139. [Google Scholar] [CrossRef]
- O’Daniel, M.; Rosenstein, A.H. Professional Communication and Team Collaboration. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Hughes, R.G., Ed.; Advances in Patient Safety, Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2008. [Google Scholar]
- Salik, I.; Ashurst, J.V. Closed Loop Communication Training in Medical Simulation. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2025. [Google Scholar]
- Chang, C.; Dudley, R. Time-Out Checklists Promote Safety in Nonoperating Room Anesthesia. APSF Newsl. 2021, 36, 120–122. Available online: https://www.apsf.org/article/time-out-checklists-promote-safety-in-nonoperating-room-anesthesia-nora/ (accessed on 1 April 2025).
- Latzman, J.A.; Castellanos, J.G.; Anca, D. Using checklists to improve care in the nonoperating room environment. Curr. Opin. Anaesthesiol. 2022, 35, 479–484. [Google Scholar] [CrossRef]
- Gawande, A. The Checklist Manifesto: How to Get Things Right; Henry Holt and Company, LLC: New York City, NY, USA, 2009. [Google Scholar]
- Grigg, E. Smarter Clinical Checklists: How to Minimize Checklist Fatigue and Maximize Clinician Performance. Anesth. Analg. 2015, 121, 570–573. [Google Scholar] [CrossRef] [PubMed]
- Awad, I.T.; Chung, F. Factors affecting recovery and discharge following ambulatory surgery. Can. J. Anaesth. 2006, 53, 858–872. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.; Georgiadis, P.L.; Urman, R.D.; Tsai, M.H. Non-Operating Room Anesthesia: Patient Selection and Special Considerations. Local. Reg. Anesth. 2020, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- White, P.F.; Song, D. New criteria for fast-tracking after outpatient anesthesia: A comparison with the modified Aldrete’s scoring system. Anesth. Analg. 1999, 88, 1069–1072. [Google Scholar] [CrossRef]
- Chung, F.; Chan, V.W.; Ong, D. A post-anesthetic discharge scoring system for home readiness after ambulatory surgery. J. Clin. Anesth. 1995, 7, 500–506. [Google Scholar] [CrossRef]
- American Society of PeriAnesthesia Nurses. Clinical Practice: Frequently Asked Question; ASPAN: Dallas, TX, USA, 2024; Available online: https://www.aspan.org/Portals/88/Clinical%20Practice/FAQs/FAQ%20Vital%20Signs.pdf?ver=D58MtPrg1_l4xLCZYftd6g%3D%3D (accessed on 13 May 2025).
- Apfelbaum, J.L.; Silverstein, J.H.; Chung, F.F.; Connis, R.T.; Fillmore, R.B.; Hunt, S.E.; Nickinovich, D.G.; Schreiner, M.S.; Silverstein, J.H.; Apfelbaum, J.L.; et al. Practice guidelines for postanesthetic care: An updated report by the American Society of Anesthesiologists Task Force on Postanesthetic Care. Anesthesiology 2013, 118, 291–307. [Google Scholar] [CrossRef]
- Clifford, T.L. Phase I and Phase II Recovery; Jones & Bartlett Learning: Burlington, MA, USA, 2018. [Google Scholar]
| Key Referenced Documents |
|---|
|
|
|
|
|
|
| Aspects of the Pre-Anesthesia Assessment | |
|
|
|
|
|
|
| Additional Perspectives from the APSF | |
|
|
| Aspects of Intra-Operative Anesthesia Management | |
|---|---|
|
|
|
|
| Aspects of Post-Operative Anesthesia Management | |
|---|---|
|
|
|
|
| NORA Challenges for Anesthesia Professionals | |
|---|---|
| Remote location | After-hour case starts |
| Limited anesthesia workspace | Rooms with inadequate lighting |
| Shared airway | Patient positioning |
| Imaging machinery | Lack of access to equipment, medications, and anesthesia trained personnel |
| Unfamiliar healthcare team | Lack of standardized time-out checklist |
| Phase I Recovery Criteria | |
| Hemodynamic Stability | Level of Consciousness |
| Voluntary Physical Activity | Respiratory Stability |
| Maintaining Oxygen Saturation | Minimal Post-Operative Nausea/Vomiting/Pain |
| Phase II Recovery Criteria | |
| Stable Vital Signs | Ambulating at Baseline without Dizziness |
| Minimal-No Nausea/Vomiting/Pain | Minimal Post-Operative Bleeding |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Royz, I.E.; Clevenger, N.B.; Bochenek, A.; Locke, A.R.; Greenberg, S.B. Respiratory Depression in Non-Operating Room Anesthesia: An Overview. J. Clin. Med. 2025, 14, 4528. https://doi.org/10.3390/jcm14134528
Royz IE, Clevenger NB, Bochenek A, Locke AR, Greenberg SB. Respiratory Depression in Non-Operating Room Anesthesia: An Overview. Journal of Clinical Medicine. 2025; 14(13):4528. https://doi.org/10.3390/jcm14134528
Chicago/Turabian StyleRoyz, Isabel E., Nicholas B. Clevenger, Andrew Bochenek, Andrew R. Locke, and Steven B. Greenberg. 2025. "Respiratory Depression in Non-Operating Room Anesthesia: An Overview" Journal of Clinical Medicine 14, no. 13: 4528. https://doi.org/10.3390/jcm14134528
APA StyleRoyz, I. E., Clevenger, N. B., Bochenek, A., Locke, A. R., & Greenberg, S. B. (2025). Respiratory Depression in Non-Operating Room Anesthesia: An Overview. Journal of Clinical Medicine, 14(13), 4528. https://doi.org/10.3390/jcm14134528








