Carotid Intima–Media Thickness Is Associated with Long-Term Mortality in Patients with Non-ST Segment Elevation Myocardial Infarction
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Demographic, Clinical, and Laboratory Analysis
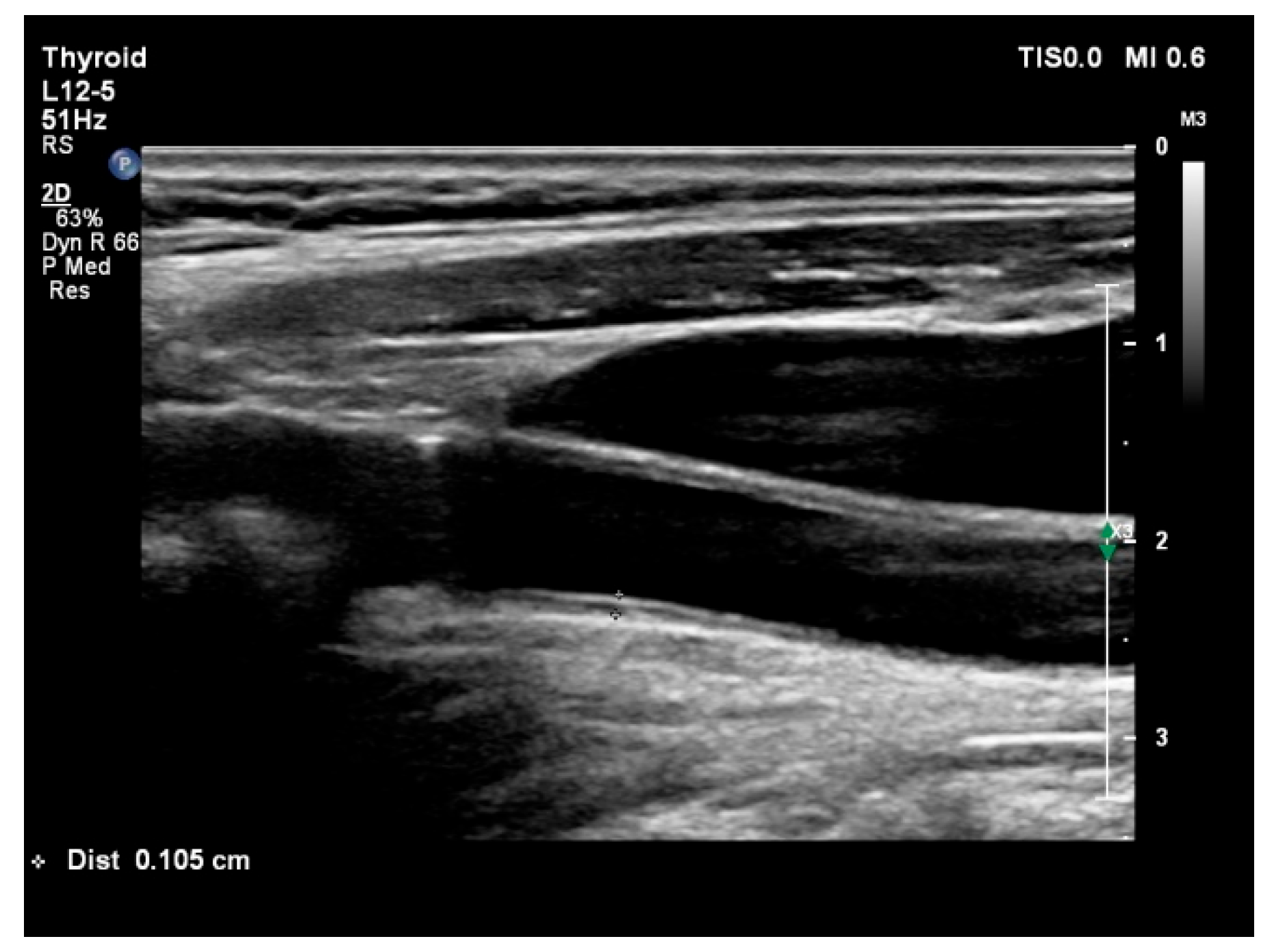
2.3. Coronary Angiography and B-Mode Ultrasound Examination
2.4. Statistical Analysis
3. Results
3.1. Demographic and Clinical Data of Patients with and Without Cardiovascular Mortality
3.2. Laboratory Data of Patients with and Without Cardiovascular Mortality
3.3. Angiographic, Echocardiographic, and Ultrasound Findings in Patients with and Without Cardiovascular Mortality
3.4. Identification of Parameters That Independently Identify Patients with Cardiovascular Mortality
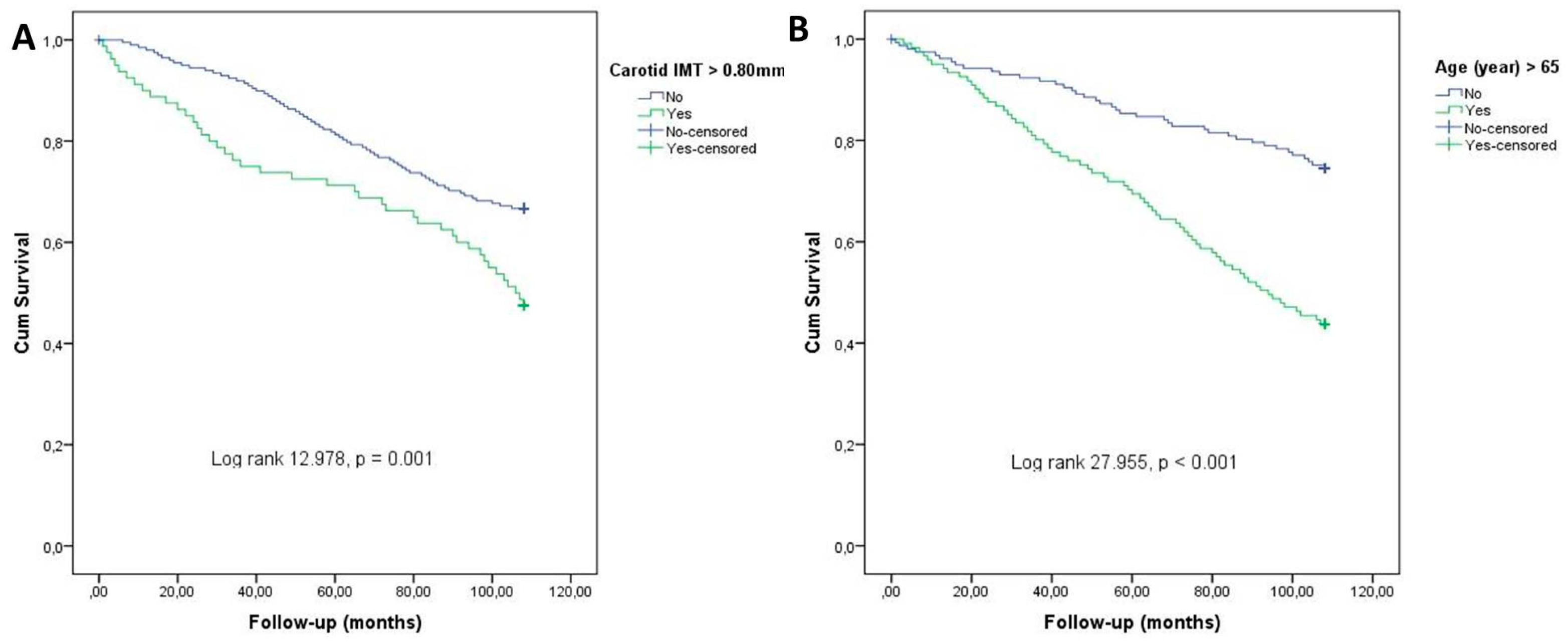
3.5. ROC Curve Analysis for Parameters That Independently Identify Patients with Cardiovascular Mortality
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rao, S.V.; O’Donoghue, M.L.; Ruel, M.; Rab, T.; Tamis-Holland, J.E.; Alexander, J.H.; Baber, U.; Baker, H.; Cohen, M.G.; Cruz-Ruiz, M.; et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI Guideline for the Management of Patients with Acute Coronary Syndromes: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2025, 151, e771–e862. [Google Scholar] [CrossRef] [PubMed]
- Bouisset, F.; Ruidavets, J.B.; Dallongeville, J.; Moitry, M.; Montaye, M.; Biasch, K.; Ferrières, J. Comparison of Short- and Long-Term Prognosis between ST-Elevation and Non-ST-Elevation Myocardial Infarction. J. Clin. Med. 2021, 10, 180. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Icen, Y.K.; Koc, A.S.; Sumbul, H.E. Coronary Artery Disease Severity Is Associated with Abdominal Aortic Intima-Media Thickness in Patients with Non-ST-Segment Elevation Myocardial Infarction. Angiology 2019, 70, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Simon, A.; Gariepy, J.; Chironi, G.; Megnien, J.L.; Levenson, J. Intima-media thickness: A new tool for diagnosis and treatment of cardiovascular risk. J. Hypertens. 2002, 20, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Burke, G.L.; Evans, G.W.; Riley, W.A.; Sharrett, A.R.; Howard, G.; Barnes, R.W.; Rosamond, W.; Crow, R.S.; Rautaharju, P.M.; Heiss, G. Arterial wall thickness is associated with prevalent cardiovascular disease in middle-aged adults: The Atherosclerosis Risk in Communities (ARIC) Study. Stroke 1995, 26, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Bots, M.L.; Grobbee, D.E.; Hofman, A.; Witteman, J.C. Common carotid intima-media thickness and risk of acute myocardial infarction: The role of lumen diameter. Stroke 2005, 36, 762–767. [Google Scholar] [CrossRef] [PubMed]
- Kato, M.; Dote, K.; Habara, S.; Takemoto, H.; Goto, K.; Nakaoka, K. Clinical implications of carotid artery remodeling in acute coronary syndrome: Ultrasonographic assessment of positive remodeling. J. Am. Coll. Cardiol. 2003, 42, 1026–1032. [Google Scholar] [CrossRef] [PubMed]
- Demircan, S.; Tekin, A.; Tekin, G.; Topçu, S.; Yiğit, F.; Erol, T.; Katircibaşi, T.; Sezgin, A.T.; Baltali, M.; Ozin, B.; et al. Comparison of carotid intima-media thickness in patients with stable angina pectoris versus patients with acute coronary syndrome. Am. J. Cardiol. 2005, 96, 643–644. [Google Scholar] [CrossRef] [PubMed]
- Tello-Montoliu, A.; Moltó, J.M.; López-Hernández, N.; García-Medina, A.; Roldán, V.; Sogorb, F.; Lip, G.Y.; Marín, F. Common carotid artery intima-media thickness and intracranial pulsatility index in non-ST-elevation acute coronary syndromes. Cerebrovasc. Dis. 2007, 24, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Cho, G.Y.; Kim, H.S.; Yoon, Y.E.; Lee, S.P.; Kim, H.K.; Kim, Y.J.; Sohn, D.W. Common carotid intima-media thickness as a risk factor for outcomes in Asian patients with acute ST-elevation myocardial infarction. Can. J. Cardiol. 2014, 30, 1620–1626. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Bierig, M.; Devereux, R.B.; Flachskampf, F.A.; Foster, E.; Pellikka, P.A.; Picard, M.H.; Roman, M.J.; Seward, J.; Shanewise, J.S.; et al. Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J. Am. Soc. Echocardiogr. 2005, 18, 1440–1463. [Google Scholar] [CrossRef] [PubMed]
- Lorenz, M.W.; Schaefer, C.; Steinmetz, H.; Sitzer, M. Is carotid intima media thickness useful for individual prediction of cardiovascular risk? Ten-year results from the Carotid Atherosclerosis Progression Study (CAPS). Eur. Heart J. 2010, 31, 2041–2048. [Google Scholar] [CrossRef] [PubMed]
- Murakami, S.; Otsuka, K.; Hotta, N.; Yamanaka, G.; Kubo, Y.; Matsuoka, O.; Yamanaka, T.; Shinagawa, M.; Nunoda, S.; Nishimura, Y.; et al. Common carotid intima-media thickness is predictive of all-cause and cardiovascular mortality in elderly community-dwelling people: Longitudinal Investigation for the Longevity and Aging in Hokkaido County (LILAC) study. Biomed. Pharmacother. 2005, 59 (Suppl. S1), S49–S53. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zielinski, T.; Dzielinska, Z.; Januszewicz, A.; Rynkun, D.; Makowiecka Ciesla, M.; Tyczynski, P.; Prejbisz, A.; Demkow, M.; Kadziela, J.; Naruszewicz, M.; et al. Carotid intima-media thickness as a marker of cardiovascular risk in hypertensive patients with coronary artery disease. Am. J. Hypertens. 2007, 20, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Keo, H.H.; Baumgartner, I.; Hirsch, A.T.; Duval, S.; Steg, P.G.; Pasquet, B.; Bhatt, D.L.; Roether, J.; REACH Registry Investigators. Carotid plaque and intima-media thickness and the incidence of ischemic events in patients with atherosclerotic vascular disease. Vasc. Med. 2011, 16, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Katakami, N.; Yamasaki, Y.; Kosugi, K.; Waki, H.; Matsuhisa, M.; Kajimoto, Y.; Masuyama, T.; Hori, M. Tissue characterization identifies subjects with high risk of cardiovascular diseases. Diabetes Res. Clin. Pract. 2004, 63, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Dijk, J.M.; van der Graaf, Y.; Bots, M.L.; Grobbee, D.E.; Algra, A. Carotid intima-media thickness and the risk of new vascular events in patients with manifest atherosclerotic disease: The SMART study. Eur. Heart J. 2006, 27, 1971–1978. [Google Scholar] [CrossRef] [PubMed]
- Inaba, Y.; Chen, J.A.; BMazzolai, L.; Teixido-Tura, G.; Lanzi, S.; Boc, V.; Bossone, E.; Brodmann, M.; Bura-Rivière, A.; De Backer, J.; et al. 2024 ESC Guidelines for the management of peripheral arterial and aortic diseases. Eur. Heart J. 2024, 45, 3538–3700. [Google Scholar] [CrossRef] [PubMed]
- Touboul, P.J.; Hennerici, M.G.; Meairs, S.; Adams, H.; Amarenco, P.; Bornstein, N.; Csiba, L.; Desvarieux, M.; Ebrahim, S.; Hernandez Hernandez, R.; et al. Mannheim carotid intima-media thickness and plaque consensus (2004–2006–2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc. Dis. 2012, 34, 290–296. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yuk, H.B.; Park, H.W.; Jung, I.J.; Kim, W.H.; Kim, K.H.; Kim, K.H.; Yang, D.J.; Park, Y.H.; Kim, Y.K.; Song, I.G.; et al. Analysis of Carotid Ultrasound Findings on Cardiovascular Events in Patients with Coronary Artery Disease during Seven-Year Follow-Up. Korean Circ. J. 2015, 45, 28–37. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Park, H.W.; Kim, W.H.; Kim, K.H.; Yang, D.J.; Kim, J.H.; Song, I.G.; Kwon, T.G.; Bae, J.H. Carotid plaque is associated with increased cardiac mortality in patients with coronary artery disease. Int. J. Cardiol. 2013, 166, 658–663. [Google Scholar] [CrossRef] [PubMed]
- Karakasis, P.; Patoulias, D.; Kassimis, G.; Koufakis, T.; Klisic, A.; Doumas, M.; Fragakis, N.; Rizzo, M. Therapeutic Potential of Sodium-glucose Co-transporter-2 Inhibitors and Glucagon-like Peptide-1 Receptor Agonists for Patients with Acute Coronary Syndrome: A Review of Clinical Evidence. Curr. Pharm. Des. 2024, 30, 2109–2119. [Google Scholar] [CrossRef] [PubMed]

| Variables | Mortality (+) n = 77 | Mortality (−) n = 202 | p |
|---|---|---|---|
| Age (year) | 59.1 ± 10.7 | 70.3 ± 11.5 | <0.001 |
| Gender (female/male), n | 38/39 | 95/107 | 0.337 |
| Hypertension, n (%) | 44 (57%) | 105 (52%) | 0.260 |
| Diabetes mellitus, n (%) | 42 (54%) | 103 (51%) | 0.895 |
| Smoking, n (%) | 35 (45%) | 89 (44%) | 0.809 |
| Hypercholesterolemia, n (%) | 40 (48%) | 101 (50%) | 0.808 |
| Systolic blood pressure (mmHg) | 117 ± 17 | 111 ± 16 | 0.502 |
| Diastolic blood pressure (mmHg) | 76 ± 7.8 | 77 ± 7.7 | 0.302 |
| Heart rate (beats/minute) | 84 ± 16 | 83 ± 17 | 0.770 |
| Variables | Mortality (+) n = 77 | Mortality (−) n = 202 | p |
|---|---|---|---|
| White blood cell (103/µL) | 10.1 ± 3.7 | 9.5 ± 3.2 | 0.209 |
| Hemoglobin (g/dL) | 12.8 ± 2.9 | 13.5 ± 1.7 | 0.023 |
| Creatinine (mg/dL) | 1.11 ± 0.98 | 0.85 ± 0.51 | 0.012 |
| Blood urea nitrogen (mg/dL) | 42.7 ± 21.8 | 32.1 ± 11.7 | 0.001 |
| Sodium (mmol/L) | 139 ± 3.9 | 137 ± 4.9 | 0.182 |
| Potassium (mmol/L) | 4.44 ± 0.52 | 4.34 ± 0.47 | 0.085 |
| Total cholesterol (mg/dL) | 167 ± 46 | 189 ± 49 | 0.001 |
| Low-density lipoprotein cholesterol (mg/dL) | 102 ± 32 | 112 ± 43 | 0.033 |
| High-density lipoprotein cholesterol (mg/dL) | 41 ± 13 | 41 ± 11 | 0.923 |
| Triglycerides (mg/dL) | 149 ± 101 | 183 ± 89 | 0.032 |
| Hs troponin T level (ng/mL) | 993 ± 1946 | 447 ± 1246 | 0.024 |
| Creatine kinase–myocardial band (U/L) | 17.2 ± 35.2 | 15.3 ± 38.3 | 0.703 |
| Variables | Mortality (+) n = 77 | Mortality (−) n = 202 | p |
|---|---|---|---|
| LVEF (%) | 51.7 ± 8.7 | 54.1 ± 7.8 | 0.026 |
| Carotid IMT (mm) | 0.81 ± 0.21 | 0.71 ± 0.17 | <0.001 |
| Aortic IMT (mm) | 1.69 ± 0.84 | 1.29 ± 0.71 | <0.001 |
| Femoral IMT (mm) | 0.96 ± 0.29 | 0.81 ± 0.25 | <0.001 |
| SYNTAX score | 17.3 ± 9.8 | 12.3 ± 8.5 | <0.001 |
| Odds | 95% CI | p | |
|---|---|---|---|
| Carotid IMT (each 0.1 mm) | 1.465 | 1.224–1.750 | <0.001 |
| Age (each year) | 1.080 | 1.051–1.110 | 0.001 |
| Creatinine (each 0.1 mg/L) | 1.126 | 1.034–1.226 | 0.008 |
| LVEF (%) | 0.982 | 0.949–1.017 | 0.308 |
| SYNTAX score | 1.012 | 0.917–1.081 | 0.235 |
| Hs troponin T level (each 10 ng/mL) | 1.015 | 0.996–1.034 | 0.126 |
| Variable | AUROC Curve | p | Cut-Off | Sensitivity | Specificity |
|---|---|---|---|---|---|
| Carotid IMT | 0.769 (0.712–0.827) | <0.001 | 0.80 mm | 79.8% | 75.1% |
| Age | 0.751 (0.693–0.810) | <0.001 | 65 year | 72.0% | 71.3% |
| Creatinine | 0.622 (0.555–0.690) | 0.001 | 0.90 mg/L | 65.8% | 65.1% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koc, A.S.; Cetin, A.E.; Icen, Y.K.; Sumbul, H.E.; Ugurlu, M.; Izlimek, U.C.; Koc, M. Carotid Intima–Media Thickness Is Associated with Long-Term Mortality in Patients with Non-ST Segment Elevation Myocardial Infarction. J. Clin. Med. 2025, 14, 4461. https://doi.org/10.3390/jcm14134461
Koc AS, Cetin AE, Icen YK, Sumbul HE, Ugurlu M, Izlimek UC, Koc M. Carotid Intima–Media Thickness Is Associated with Long-Term Mortality in Patients with Non-ST Segment Elevation Myocardial Infarction. Journal of Clinical Medicine. 2025; 14(13):4461. https://doi.org/10.3390/jcm14134461
Chicago/Turabian StyleKoc, Ayse Selcan, Abdullah Eren Cetin, Yahya Kemal Icen, Hilmi Erdem Sumbul, Mehmet Ugurlu, Ugur Can Izlimek, and Mevlut Koc. 2025. "Carotid Intima–Media Thickness Is Associated with Long-Term Mortality in Patients with Non-ST Segment Elevation Myocardial Infarction" Journal of Clinical Medicine 14, no. 13: 4461. https://doi.org/10.3390/jcm14134461
APA StyleKoc, A. S., Cetin, A. E., Icen, Y. K., Sumbul, H. E., Ugurlu, M., Izlimek, U. C., & Koc, M. (2025). Carotid Intima–Media Thickness Is Associated with Long-Term Mortality in Patients with Non-ST Segment Elevation Myocardial Infarction. Journal of Clinical Medicine, 14(13), 4461. https://doi.org/10.3390/jcm14134461






