Innovative Aesthetic and Functional Orthodontic Planning with Hard and Soft Tissue Analyses
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedure Methodology
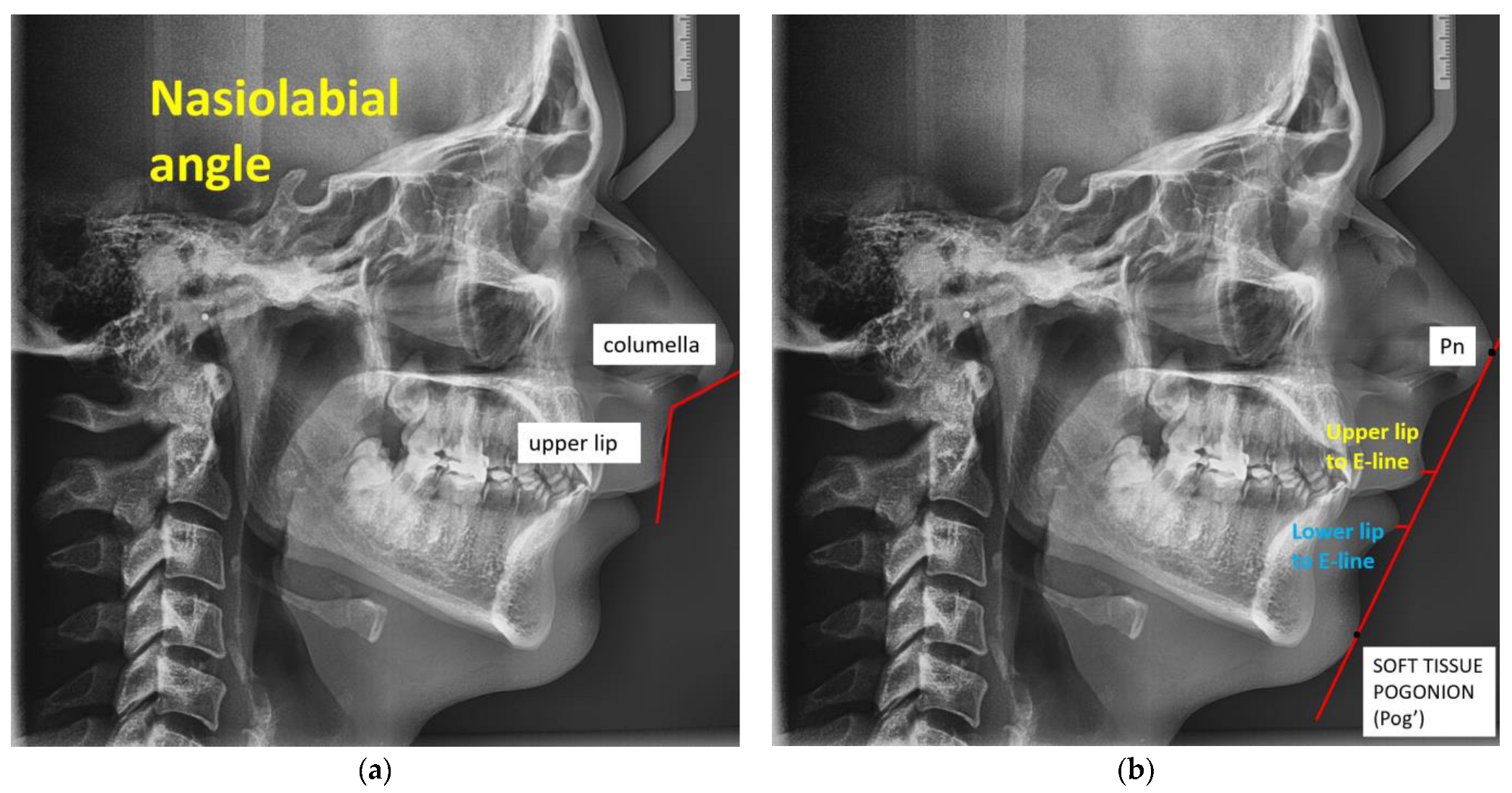
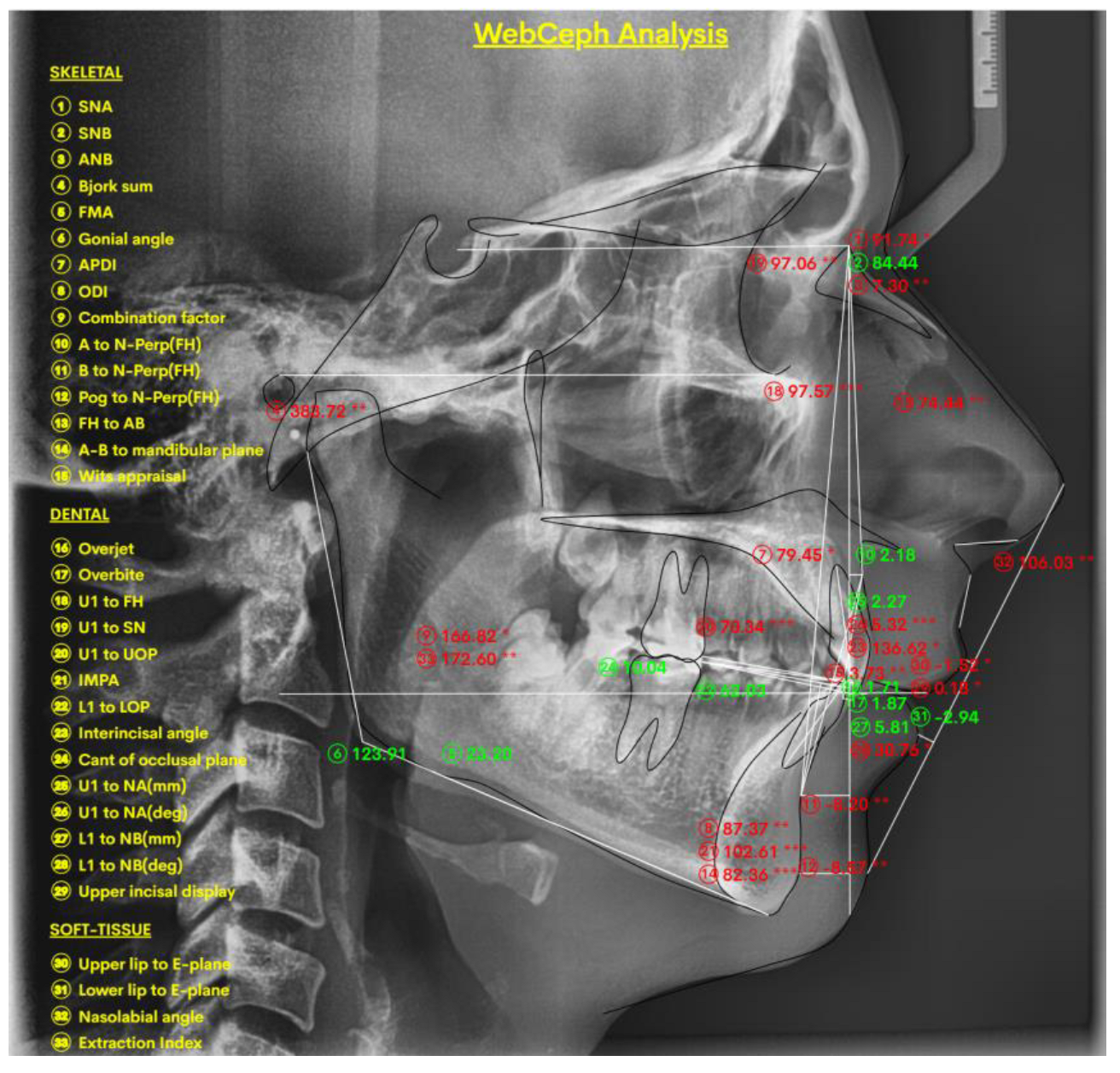
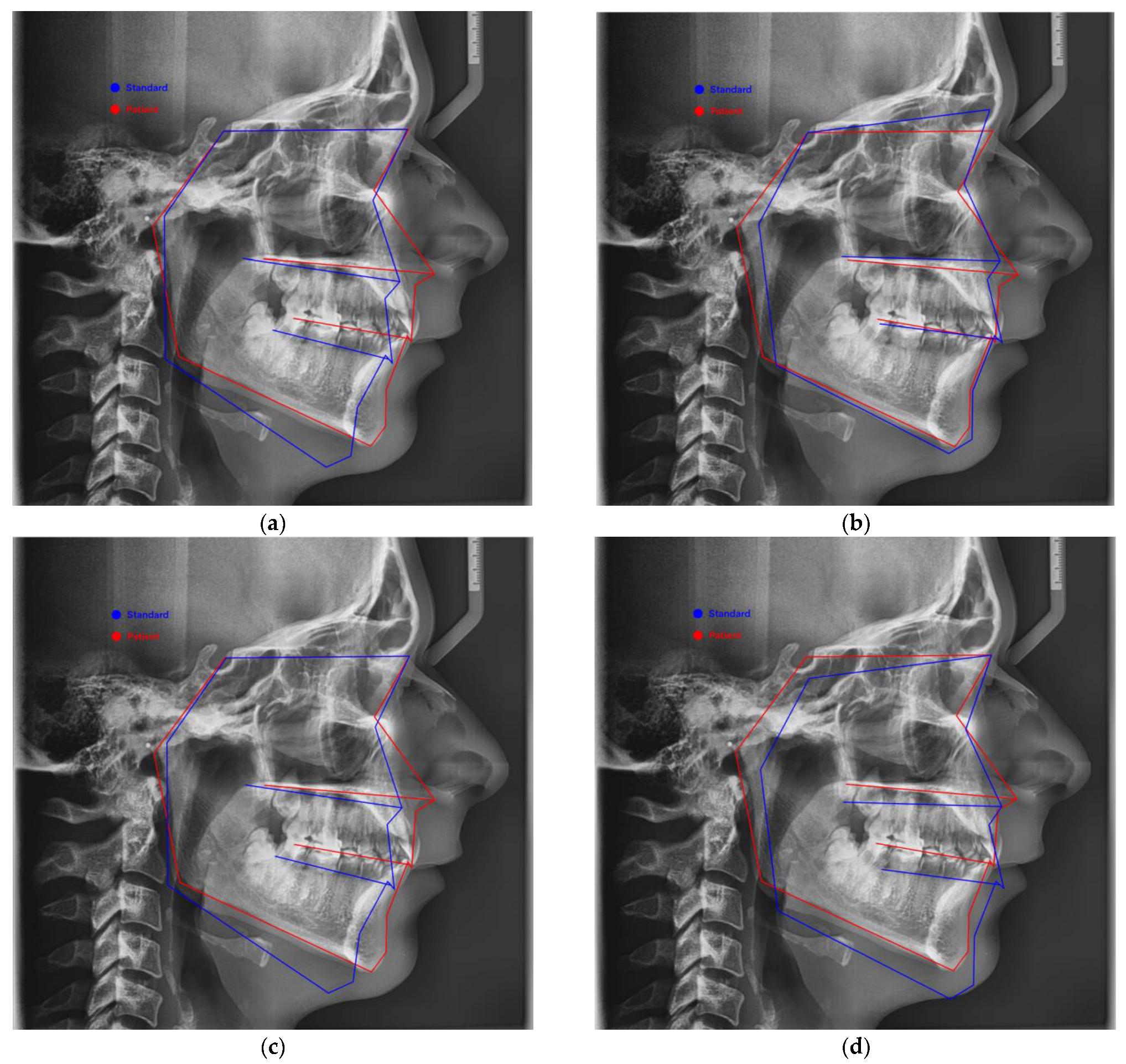
2.1.1. Digital Lateral Cephalometric Measurements and Protocol
2.1.2. Statistical Analysis
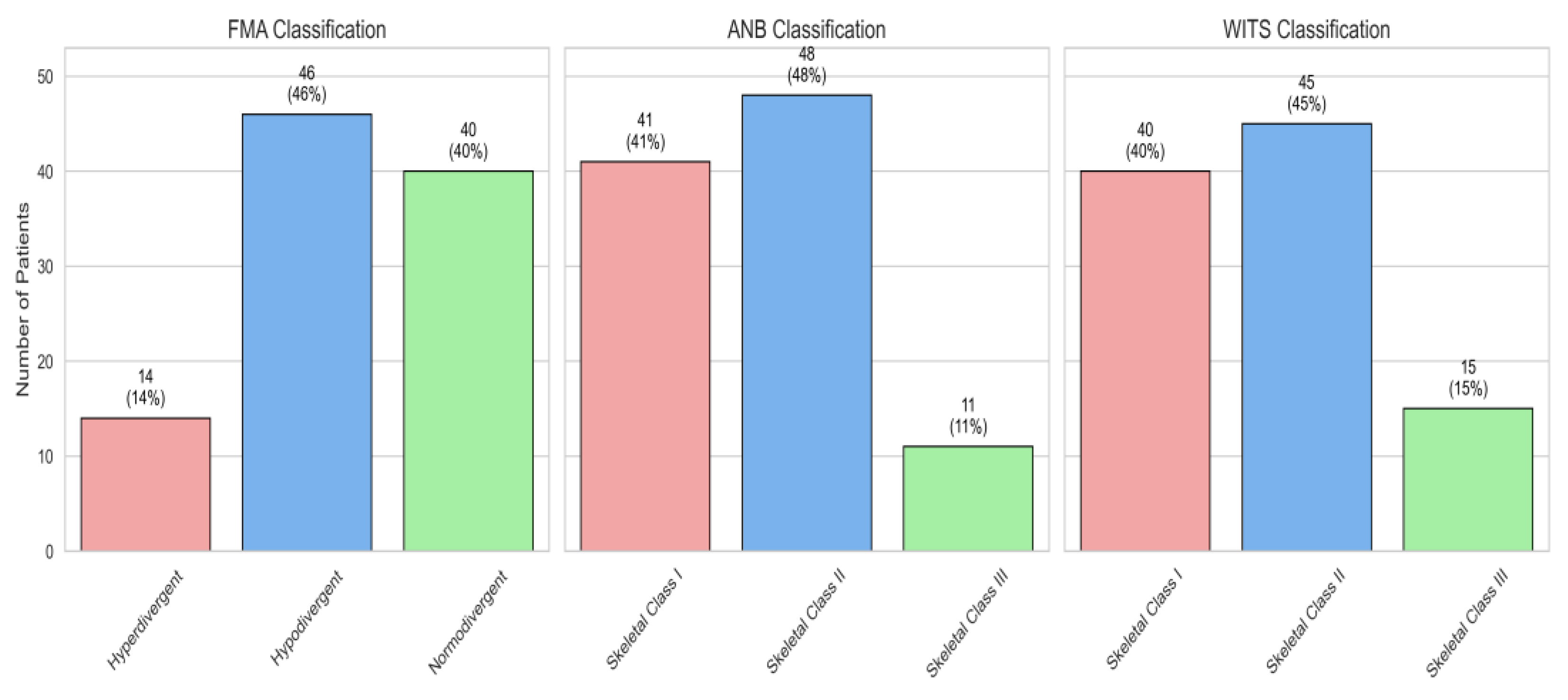
3. Results
4. Discussion
Study Limitations and Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ackerman, J.L.; Ackerman, M.B.; Kean, R.M. A Philadelphia Fable: How Ideal Occlusion Became the Philosopher’s Stone of Orthodontics. Angle Orthod. 2007, 77, 192–194. [Google Scholar] [CrossRef] [PubMed]
- Alhazmi, N.; Alrasheed, F.; Alshayea, K.; Almubarak, T.; Alzeer, B.; Alorf, M.S.; Alorf, M. Facial Soft Tissue Characteristics Among Sagittal and Vertical Skeletal Patterns: A Cone-Beam Computed Tomography Study. Cureus 2023, 15, e44428. [Google Scholar] [CrossRef] [PubMed]
- Siécola, G.S.; Capelozza, L.; Lorenzoni, D.C.; Janson, G.; Henriques, J.F.C. Subjective Facial Analysis and Its Correlation with Dental Relationships. Dental Press J. Orthod. 2017, 22, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Kochel, J.; Meyer-Marcotty, P.; Kochel, M.; Schneck, S.; Stellzig-Eisenhauer, A. 3D Soft Tissue Analysis—Part 2: Vertical Parameters. J. Orofac. Orthop. 2010, 71, 207–220. [Google Scholar] [CrossRef]
- Tucci, I.; Sferra, S.; Giuliante, L.; Scribante, A.; Mannocci, A.; Grippaudo, C. Relationship Between Vertical Facial Patterns and Palatal Morphology in Class I and Class II Malocclusion. Appl. Sci. 2025, 15, 604. [Google Scholar] [CrossRef]
- Dimaggio, F.R.; Ciusa, V.; Sforza, C.; Ferrario, V.F. Photographic Soft-Tissue Profile Analysis in Children at 6 Years of Age. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 475–480. [Google Scholar] [CrossRef]
- Denadai, R.; Chou, P.Y.; Su, Y.Y.; Lin, H.H.; Ho, C.T.; Lo, L.J. The Impacts of Orthognathic Surgery on the Facial Appearance and Age Perception of Patients Presenting Skeletal Class III Deformity: An Outcome Study Using the FACE-Q Report and Surgical Professional–Based Panel Assessment. Plast. Reconstr. Surg. 2020, 145, 1035–1046. [Google Scholar] [CrossRef]
- Cenzato, N.; Farronato, M.; Tartaglia, F.C.; Giannini, L.; Inchingolo, A.M.; Dipalma, G.; Inchingolo, F. Soft Tissue Facial Morphology in Growing Patients with Different Occlusal Classes. J. Pers. Med. 2024, 14, 1042. [Google Scholar] [CrossRef]
- Mahto, R.K.; Kafle, D.; Giri, A.; Luintel, S.; Karki, A. Evaluation of Fully Automated Cephalometric Measurements Obtained from Web-Based Artificial Intelligence Driven Platform. BMC Oral Health 2022, 22, 132. [Google Scholar] [CrossRef]
- Naoumova, J.; Lindman, R. A Comparison of Manual Traced Images and Corresponding Scanned Radiographs Digitally Traced. Eur. J. Orthod. 2009, 31, 247–253. [Google Scholar] [CrossRef]
- Huja, S.S.; Grubaugh, E.L.; Rummel, A.M.; Fields, H.W.; Beck, F.M. Comparison of Hand-Traced and Computer-Based Cephalometric Superimpositions. Angle Orthod. 2009, 79, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Thakur, V.K.; Chaudhary, D.C.; Jayan, B.; Jain, V.; Mathur, P. Soft-Tissue Paradigm: A Review. J. Glob. Oral Health 2023, 6, 107–113. [Google Scholar] [CrossRef]
- Abdulal, G.; Osman, A.; Abyad, A. Evaluation of Facial Soft-Tissue Morphology among Different Vertical Skeletal Profiles. Eur. J. Orthod. 2022, 18, 117–134. [Google Scholar] [CrossRef]
- Ahn, J.H.; Bae, K.H.; Park, Y.J.; Hong, R.K.; Nam, J.H.; Kim, M.J. Assessment of Antero-Posterior Skeletal Relationships in Adult Korean Patients in the Natural Head Position and Centric Relation. Korean J. Orthod. 2010, 40, 421–431. [Google Scholar] [CrossRef][Green Version]
- Verma, P.; Verma, K.G.; Kumaraswam, K.L.; Basavaraju, S.; Sachdeva, S.K.; Juneja, S. Correlation of Morphological Variants of the Soft Palate and Need’s Ratio in Normal Individuals: A Digital Cephalometric Study. Imaging Sci. Dent. 2014, 44, 193–198. [Google Scholar] [CrossRef]
- Lala, S.; McGann, D.; Dorrego, D. The Effect of Different Head Positions in Cephalometric Radiographic Analysis—A Pilot Study. Dent. Open J. Med. Res. 2021, 8, DOMR.1000396. [Google Scholar] [CrossRef]
- Yoon, Y.J.; Kim, K.S.; Hwang, M.S.; Kim, H.J.; Choi, E.H.; Kim, K.W. Effect of head rotation on lateral cephalometric radiographs. Angle Orthod. 2001, 71, 396–403. [Google Scholar]
- Kim, Y.H.; Park, J.B.; Chang, M.S.; Ryu, J.J.; Lim, W.H.; Jung, S.K. Influence of the Depth of the Convolutional Neural Networks on an Artificial Intelligence Model for Diagnosis of Orthognathic Surgery. J. Pers. Med. 2021, 11, 356. [Google Scholar] [CrossRef]
- Yassir, Y.A.; Salman, A.R.; Nabbat, S.A. The Accuracy and Reliability of WebCeph for Cephalometric Analysis. J. Taibah Univ. Med. Sci. 2022, 17, 57–66. [Google Scholar] [CrossRef]
- Katyal, D.; Balakrishnan, N. Evaluation of the Accuracy and Reliability of WebCeph–An Artificial Intelligence-Based Online Software. APOS Trends Orthod. 2022, 12, 271–276. [Google Scholar] [CrossRef]
- Natrajan, K.; Selvarajan, K.; Geevee, A.; Elango, E.; Sankar, H.; Krishnan, P. Accuracy and Reliability of WebCeph on Posteroanterior Cephalogram—A Retrospective Study. J. Contemp. Orthod. 2024, 8, 491–495. [Google Scholar]
- Alam, M.K.; Alfawzan, A.A. Dental Characteristics of Different Types of Cleft and Non-Cleft Individuals. Front. Cell Dev. Biol. 2020, 8, 789. [Google Scholar] [CrossRef]
- Szuhanek, C.; Schiller, A.; Grigore, A.; Popa, L. A Guide to Orthodontics; Editura Victor Babeș: Timisoara, Romania, 2019. [Google Scholar]
- Ghodasra, R.; Brizuela, M. Orthodontics, Cephalometric Analysis. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK594272/ (accessed on 24 February 2025).
- Ahmed, M.; Shaikh, A.; Fida, M. Diagnostic validity of different cephalometric analyses for assessment of the sagittal skeletal pattern. Dental Press J. Orthod. 2018, 23, 75–81. [Google Scholar] [CrossRef]
- Singh, K.; Chaudhary, R. Assessment of Average Frankfort Mandibular Plane Angle. J. Adv. Med. Dent. Sci. Res. 2022, 10, 109–111. [Google Scholar]
- Björk, A. Prediction of Mandibular Growth Rotation. Am. J. Orthod. 1969, 55, 585–599. [Google Scholar] [CrossRef] [PubMed]
- Jarabak, J.R.; Fizzell, J.A. Technique and Treatment with the Light-Wire Appliance, 2nd ed.; C.V. Mosby: St. Louis, MO, USA, 1972. [Google Scholar]
- Farha, P.; Arqub, S.A.; Ghoussoub, M.S. Correlation Between Cephalometric Values and Soft Tissue Profile in Class I and Class II Adult Patients Based on Vertical Patterns. Turk. J. Orthod. 2024, 37, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Jeelani, W.; Fida, M.; Shaikh, A. Facial Soft Tissue Analysis among Various Vertical Facial Patterns. J. Ayub Med. Coll. Abbottabad 2016, 28, 29–34. [Google Scholar] [PubMed]
- Da Vinci, P.C.L. Notebook of a Genius; Powerhouse Publishing: Milan, Italy, 2001. [Google Scholar]
- Abdul–Qadir, M.Y.; Ne’am, R.S.; Al–Sayagh, N.M. Analysis of Soft Tissue Facial Profile in Different Vertical Growth Patterns. Al-Rafidain Dent. J. 2011, 11, 346–356. [Google Scholar]
- Feres, M.F.N.; Hitos, S.F.; Sousa, H.I.P.D.; Matsumoto, M.A.N. Comparison of Soft Tissue Size Between Different Facial Patterns. Dent. Press J. Orthod. 2010, 15, 84–93. [Google Scholar] [CrossRef]
- Perović, T.; Blažej, Z. Male and Female Characteristics of Facial Soft Tissue Thickness in Different Orthodontic Malocclusions Evaluated by Cephalometric Radiography. Med. Sci. Monit. 2018, 24, 3415–3424. [Google Scholar] [CrossRef]
- Batool, M.; Ashraf, A.; Mirza, S.M.; Ashraf, F.; Azeem, M.; Imtiaz, M. Correlation between Facial Soft Tissues and Vertical Facial Pattern in 12–16 Years Old Untreated Patients. Pak. J. Med. Health Sci. 2022, 16, 118. [Google Scholar] [CrossRef]
- Kilic, N.; Catal, G.; Kiki, A.; Oktay, H. Soft Tissue Profile Changes Following Maxillary Protraction in Class III Subjects. Eur. J. Orthod. 2010, 32, 419–424. [Google Scholar] [CrossRef]
- Ghorbanyjavadpour, F.; Rakhshan, V. Factors Associated with the Beauty of Soft-Tissue Profile. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 832–843. [Google Scholar] [CrossRef] [PubMed]
- Rakhshan, V.; Ghorbanyjavadpour, F. Anteroposterior and Vertical Soft Tissue Cephalometric Norms of Iranians, Interethnic Comparisons, Sex Dimorphism, and the Effect of Age on Cephalometric Variables. Oral Maxillofac. Surg. 2019, 23, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Amini, F.; Razavian, Z.S.; Rakhshan, V. Soft Tissue Cephalometric Norms of Iranian Class I Adults with Good Occlusions and Balanced Faces. Int. Orthod. 2016, 14, 108–122. [Google Scholar] [CrossRef]
- Erbay, E.F.; Caniklioğlu, C.M. Soft Tissue Profile in Anatolian Turkish Adults: Part II. Comparison of Different Soft Tissue Analyses in the Evaluation of Beauty. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 65–72. [Google Scholar] [CrossRef]
- Khan, S.Q.; Ashraf, B.; Abbas, I.G.; Mahmood, S. Soft Tissue Analysis of Aesthetically Pleasing Faces. Pak. Oral Dent. J. 2015, 35, 424–428. [Google Scholar]
- Arnett, G.W.; Gunson, M.J. Facial Planning for Orthodontists and Oral Surgeons. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 290–295. [Google Scholar] [CrossRef]
- Zecca, P.A.; Fastuca, R.; Beretta, M.; Caprioglio, A.; Macchi, A. Correlation Assessment between Three-Dimensional Facial Soft Tissue Scan and Lateral Cephalometric Radiography in Orthodontic Diagnosis. Int. J. Dent. 2016, 2016, 1473918. [Google Scholar] [CrossRef]
- Çelikoğlu, M.; Büyük, S.K.; Ekizer, A.; Sekerci, A.E.; Şişman, Y. Assessment of the Soft Tissue Thickness at the Lower Anterior Face in Adult Patients with Different Skeletal Vertical Patterns Using Cone-Beam Computed Tomography. Angle Orthod. 2015, 85, 211–217. [Google Scholar] [CrossRef]
- Jo, S.Y.; Bayome, M.; Park, J.; Lim, H.J.; Kook, Y.A.; Han, S.H. Comparison of Treatment Effects between Four Premolar Extraction and Total Arch Distalization Using the Modified C-Palatal Plate. Korean J. Orthod. 2018, 48, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, K.; Kulshrestha, R.; Azam, A.; Shabir, S.; Kaur, H. Soft Tissue Analysis of Chin, Upper Lip Length and Thickness in Patients with Different Mandibular Divergent Patterns—A Cephalometric Study. IP Indian J. Orthod. Dentofac. Res. 2018, 4, 88–93. [Google Scholar]
- Halazonetis, D.J. Morphometric Correlation between Facial Soft-Tissue Profile Shape and Skeletal Pattern in Children and Adolescents. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 450–457. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Sforza, C.; Schmitz, J.H.; Ciusa, V.; Colombo, A. Normal Growth and Development of the Lips: A 3-Dimensional Study from 6 Years to Adulthood Using a Geometric Model. J. Anat. 2000, 196, 415–423. [Google Scholar] [CrossRef]
- Shamlan, M.A.; Aldrees, A.M. Hard and Soft Tissue Correlations in Facial Profiles: A Canonical Correlation Study. Clin. Cosmet. Investig. Dent. 2015, 7, 9–15. [Google Scholar] [PubMed]
- Santiago, R.C.; da Silva Campos, M.J.; Vitral, R.W.F.; de Almeida Campos, J.D.F.; de Faria, F.R.; Nojima, L.I.; Sant’Anna, E.F. Correlations between ANB, Wits and Soft-Tissue Facial Profile in a Brazilian Population Sample. HU Rev. 2024, 50, 1–7. [Google Scholar] [CrossRef]
- Park, E.; Chang, J.; Park, J. Facial Soft Tissue Thickness Differences among Three Skeletal Classes in Korean Population Using CBCT. Int. J. Environ. Res. Public Health 2023, 20, 2658. [Google Scholar] [CrossRef]
- Shrestha, R.; Halwai, H.K.; Yadav, S.K.; Gupta, S.K. Skeletal, dentoalveolar and soft tissue components of skeletal class II malocclusion among Nepalese orthodontic patients: A cephalometric study. Orthod. J. Nepal 2022, 12, 2–8. [Google Scholar] [CrossRef]
- Jazmati, H.M.; Ajaj, M.A.; Hajeer, M.Y. Assessment of Facial Soft Tissue Dimensions in Adult Patients with Different Sagittal Skeletal Classes Using Cone Beam Computed Tomography. Diagnostics 2022, 12, 1497. [Google Scholar]
- Kale, B.; Buyukcavus, M.H. Comparison of Three-Dimensional Soft-Tissue Evaluations between Skeletal and Pseudo-Class III Malocclusions. Sci. Rep. 2020, 10, 14717. [Google Scholar] [CrossRef]
- Nanda, R. Esthetics and Biomechanics in Orthodontics; W.B. Saunders: Philadelphia, PA, USA, 1990. [Google Scholar]
- Tweed, C.H. The Frankfort–mandibular incisor angle in orthodontic diagnosis, treatment planning, and prognosis. Am. J. Orthod. Oral Surg. 1946, 32, 175–230. [Google Scholar] [CrossRef] [PubMed]
- Arnett, G.W.; Bergman, R.T. Facial soft tissue cephalometric norms for orthodontic diagnosis and treatment planning. Am. J. Orthod. Dentofac. Orthop. 1993, 103, 299–312. [Google Scholar] [CrossRef] [PubMed]

| Variables | Short Form | Details |
|---|---|---|
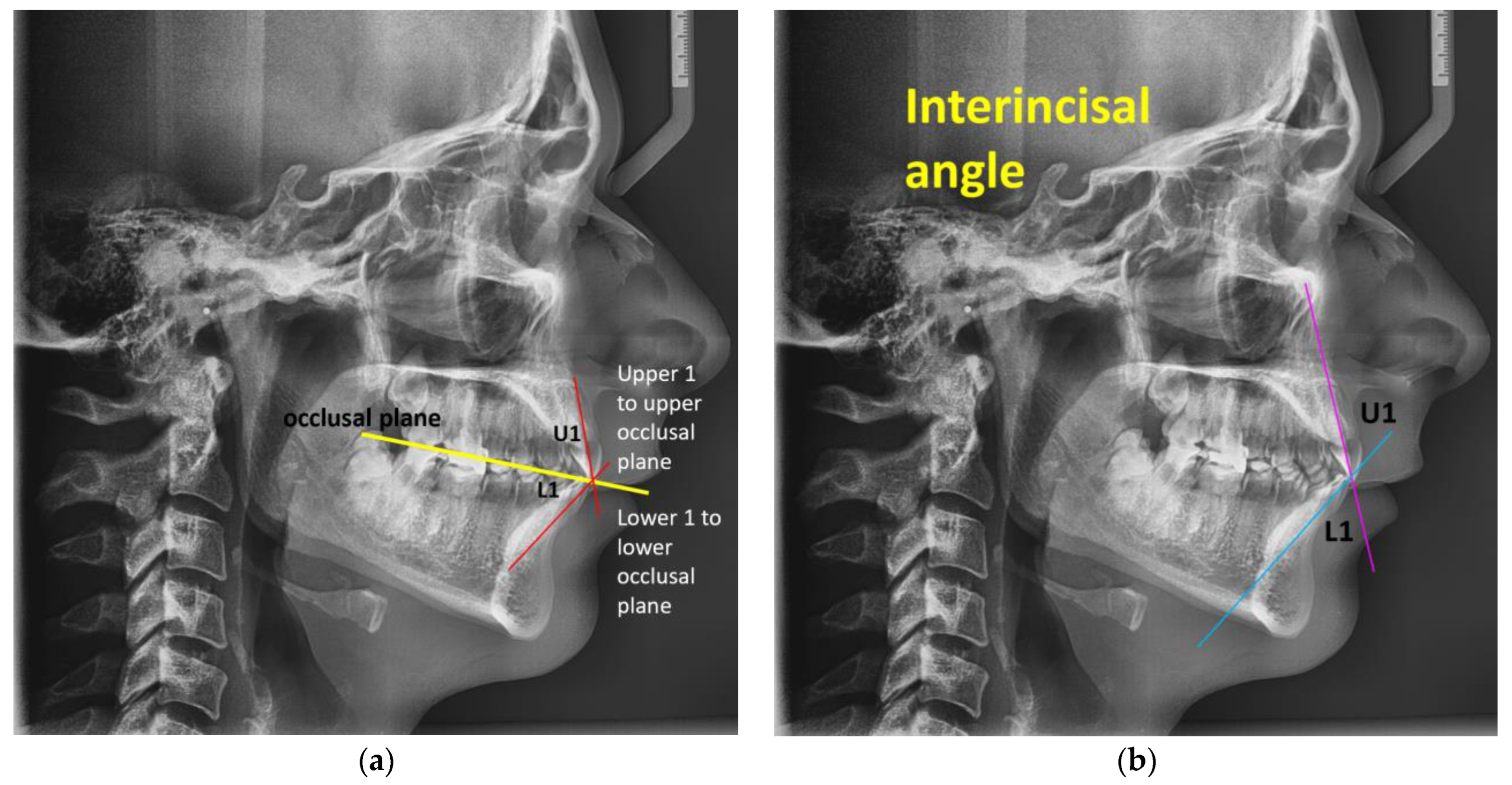
| Upper 1 to upper occlusal plane | U1 to UOP | Angle between the upper occlusal plane and the upper incisor’s long axis [22]. Mean values from the WEBCEPH digital program: 55°, S.D. 4.0. |
| Lower 1 to lower occlusal plane | L1 to LOP | Angle between the lower occlusal plane and the lower incisor’s long axis [22]. Mean values from the WEBCEPH digital program: 66°, S.D. 5.0. |
| Interincisal angle | IIA | Angle formed by the upper and lower incisors’ long axes [22]. The mutual angulation between the incisors is expressed by the interincisal angle, which is independent of the bone bases. Value normal: 130 ± 5°. When the value exceeds 135°, the incisors are retroclined. When the value is less than 125°, the incisors are proclined [23]. Mean values from the WEBCEPH digital program: 130°, S.D. 5.8. |
| Occlusal plane | OP | Occlusal plane: the line that, in the event of open frontal occlusion, crosses the space between the central incisors or the midway point of the overbite to split the occlusion of the first molars; following Ricketts, a line that passes across the greatest number of points of contact between the superior and inferior ocular bones represents linear deformation caused by Spee [23]. |
| Characteristic | Value |
|---|---|
| Age (years) | 26 (19, 32) |
| Gender | |
| Female | 52 (52%) |
| Male | 48 (48%) |
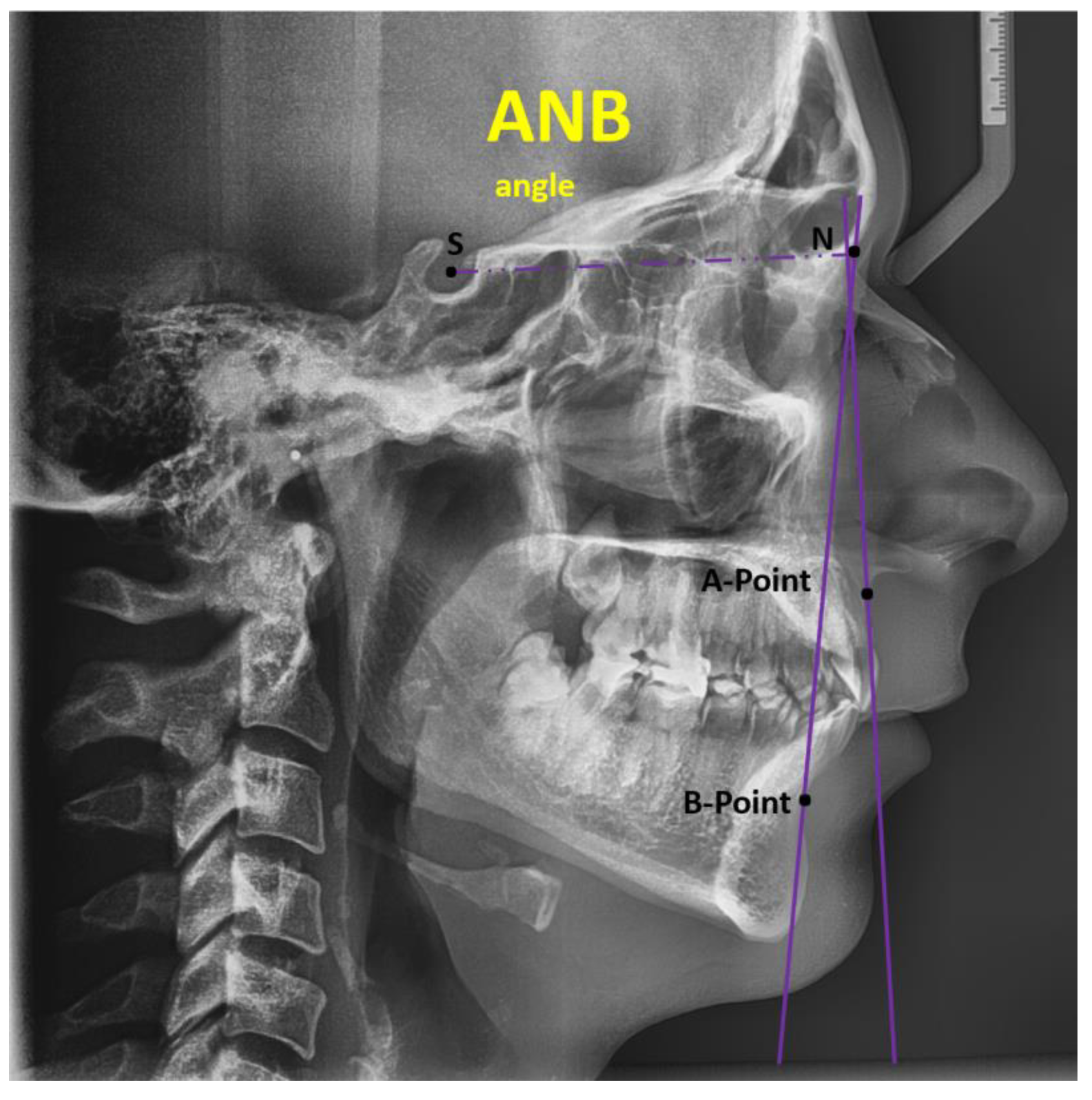
| ANB (degrees) | 4.53 (2.65, 7.00) |
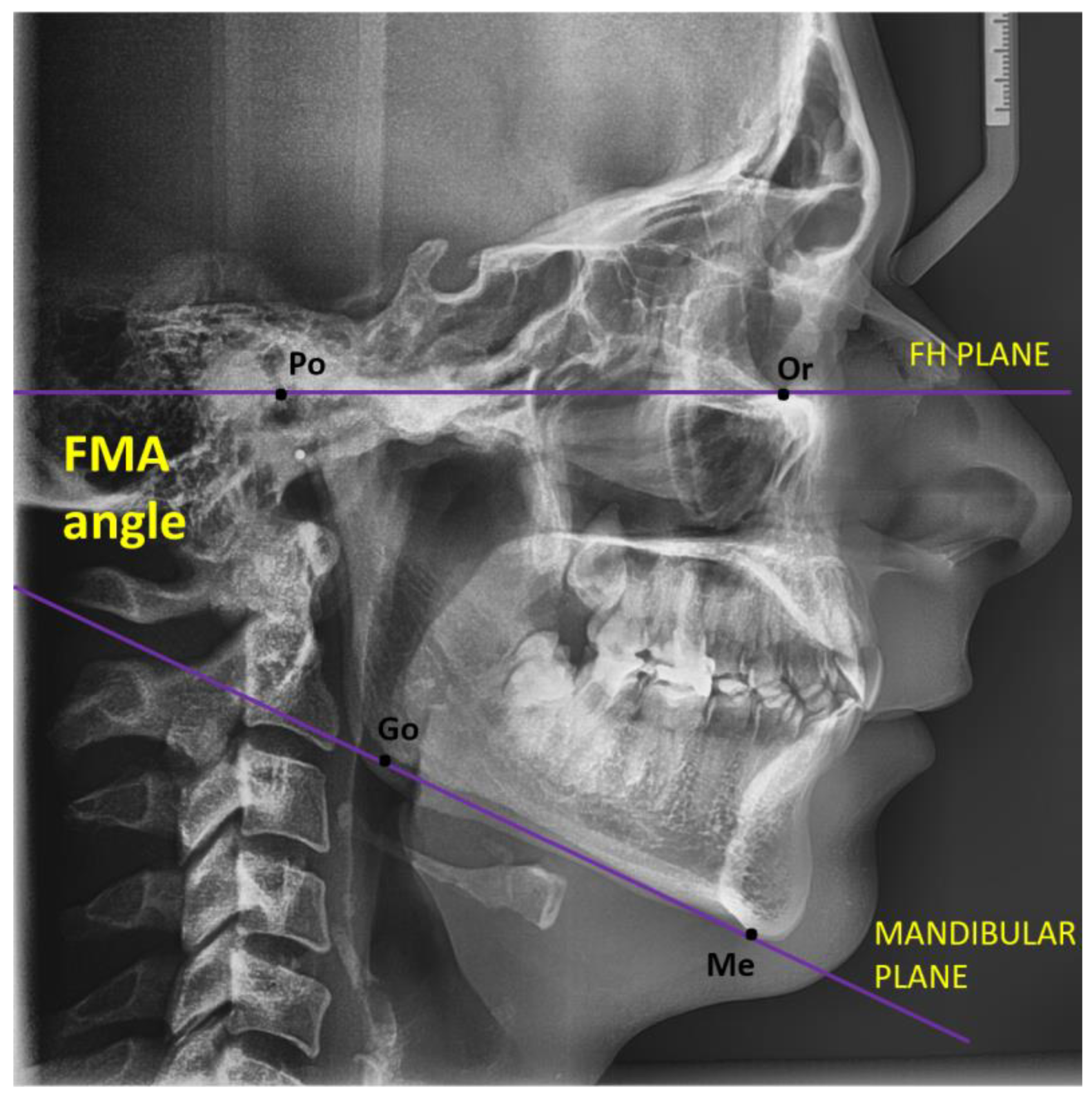
| FMA (degrees) | 22 (16, 26) |
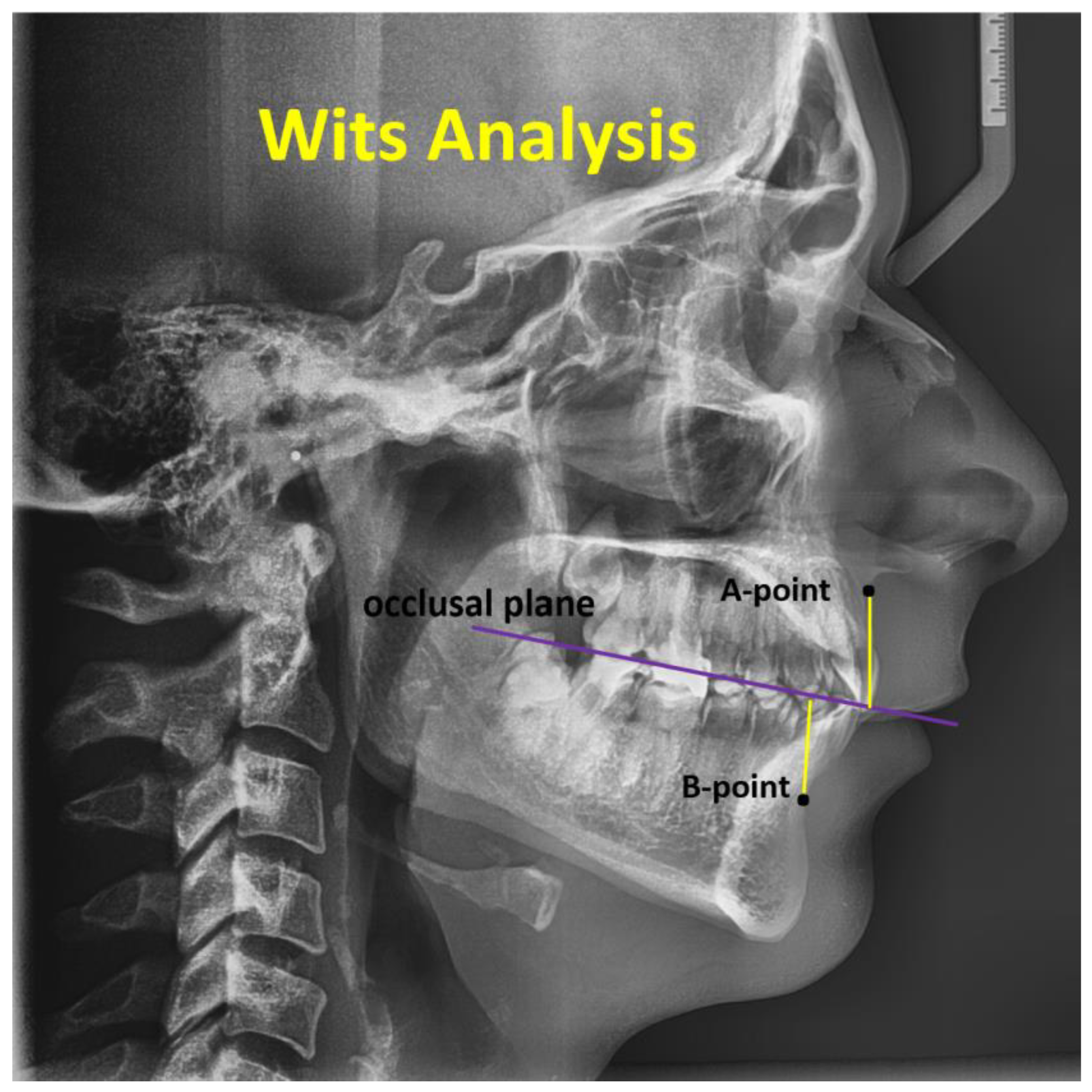
| Wits (mm) | 2.1 (0.0, 4.3) |
| Upper lip to E-plane (mm) | −2.75 (−4.86, −1.30) |
| Lower lip to E-plane (mm) | −2.3 (−3.9, −0.6) |
| Nasolabial angle (degrees) | 101 (97, 110) |
| U1 to UOP (upper incisors to upper occlusal plane) | 59 (55, 64) |
| L1 to LOP (lower incisors to lower occlusal plane) | 65 (60, 69) |
| Interincisal angle (degrees) | 128 (122, 137) |
| Dependent: Gender | Female | Male | Total | p | |
|---|---|---|---|---|---|
| Total N (%) | 52 (52.0) | 48 (48.0) | 100 | ||
| Age (years) | Median (IQR) | 26.0 (20.5 to 32.0) | 26.0 (18.8 to 32.2) | 26.0 (19.0 to 32.0) | 0.671 |
| ANB degrees | Median (IQR) | 4.3 (2.6 to 6.9) | 4.6 (3.2 to 6.9) | 4.5 (2.6 to 6.9) | 0.858 |
| FMA degrees | Median (IQR) | 21.1 (15.8 to 26.0) | 22.7 (19.0 to 25.6) | 22.2 (16.5 to 25.7) | 0.572 |
| Wits (mm) | Median (IQR) | 2.1 (−0.1 to 4.3) | 2.1 (0.1 to 4.2) | 2.1 (0.0 to 4.3) | 0.994 |
| Upper lip to E-plane (mm) | Median (IQR) | −3.0 (−4.8 to −1.6) | −2.7 (−4.9 to −1.0) | −2.8 (−4.8 to −1.3) | 0.424 |
| Lower lip to E-plane (mm) | Median (IQR) | −2.3 (−3.5 to −1.1) | −2.3 (−4.1 to −0.1) | −2.3 (−3.8 to −0.6) | 0.586 |
| Nasolabial angle | Median (IQR) | 102.6 (96.6 to 109.8) | 101.1 (96.4 to 109.7) | 101.5 (96.5 to 109.7) | 0.406 |
| U1 to UOP | Median (IQR) | 59.5 (56.6 to 63.9) | 58.1 (53.8 to 62.5) | 58.8 (54.9 to 63.8) | 0.361 |
| L1 to LOP | Median (IQR) | 63.8 (59.0 to 68.0) | 66.4 (61.2 to 69.7) | 65.2 (60.5 to 69.4) | 0.183 |
| Interincisal angle | Median (IQR) | 129.0 (123.0 to 137.9) | 127.7 (121.0 to 135.7) | 128.2 (121.6 to 136.8) | 0.422 |
| Meaning results of FMA | Hyperdivergent | 8 (15.4) | 6 (12.5) | 14 (14.0) | 0.298 |
| Hypodivergent | 27 (51.9) | 19 (39.6) | 46 (46.0) | ||
| Normodivergent | 17 (32.7) | 23 (47.9) | 40 (40.0) | ||
| Meaning results of ANB | Skeletal Class I | 21 (40.4) | 20 (41.7) | 41 (41.0) | 0.981 |
| Skeletal Class II | 25 (48.1) | 23 (47.9) | 48 (48.0) | ||
| Skeletal Class III | 6 (11.5) | 5 (10.4) | 11 (11.0) | ||
| Meaning results WITS | Skeletal Class I | 21 (40.4) | 19 (39.6) | 40 (40.0) | 0.986 |
| Skeletal Class II | 23 (44.2) | 22 (45.8) | 45 (45.0) | ||
| Skeletal Class III | 8 (15.4) | 7 (14.6) | 15 (15.0) |
| Parameter | Meaning Results WITS Skeletal Class I | Meaning Results WITS Skeletal Class II | Meaning Results WITS Skeletal Class III | Total | p-Value |
|---|---|---|---|---|---|
| Total N (%) | 40 (40.0) | 45 (45.0) | 15 (15.0) | 100 | |
| Interincisal angle (degrees) | 128.8 (122.7 to 134.7) | 125.8 (119.8 to 133.6) | 137.4 (129.1 to 146.1) | 128.2 (121.6 to 136.8) | 0.01 |
| L1 to LOP (degrees) | 66.3 (64.1 to 69.5) | 61.3 (57.0 to 64.4) | 76.6 (71.8 to 79.3) | 65.2 (60.5 to 69.4) | <0.001 |
| U1 to UOP (degrees) | 58.8 (54.5 to 60.8) | 59.6 (55.7 to 64.5) | 57.2 (52.2 to 65.5) | 58.8 (54.9 to 63.8) | 0.507 |
| Nasolabial angle (degrees) | 100.7 (92.4 to 104.1) | 104.1 (98.8 to 114.0) | 99.4 (92.0 to 102.7) | 101.5 (96.5 to 109.7) | 0.01 |
| Lower lip to E-plane (mm) | −1.9 (−3.2 to −0.7) | −2.2 (−3.5 to −0.1) | −3.5 (−7.8 to −2.3) | −2.3 (−3.8 to −0.6) | 0.039 |
| Upper lip to E-plane (mm) | −2.7 (−4.4 to −1.6) | −1.9 (−4.0 to −1.0) | −5.5 (−7.6 to −4.4) | −2.8 (−4.8 to −1.3) | 0.001 |
| Wits (mm) | 1.0 (0.0 to 2.0) | 4.5 (3.5 to 7.0) | −3.8 (−4.4 to −2.6) | 2.1 (0.0 to 4.3) | <0.001 |
| FMA (degrees) | 23.4 (15.8 to 27.4) | 21.6 (16.3 to 24.4) | 22.9 (18.8 to 24.8) | 22.2 (16.5 to 25.7) | 0.416 |
| ANB (degrees) | 3.9 (2.6 to 4.7) | 6.8 (5.4 to 8.1) | −0.2 (−0.9 to 1.7) | 4.5 (2.6 to 6.9) | <0.001 |
| Meaning results of FMA | 0.558 | ||||
| Hyperdivergent | 8 (20.0) | 5 (11.1) | 1 (6.7) | 14 (14.0) | |
| Hypodivergent | 18 (45.0) | 22 (48.9) | 6 (40.0) | 46 (46.0) | |
| Normodivergent | 14 (35.0) | 18 (40.0) | 8 (53.3) | 40 (40.0) | |
| Meaning results of ANB | <0.001 | ||||
| Skeletal Class I | 28 (70.0) | 8 (17.8) | 5 (33.3) | 41 (41.0) | |
| Skeletal Class II | 11 (27.5) | 36 (80.0) | 1 (6.7) | 48 (48.0) | |
| Skeletal Class III | 1 (2.5) | 1 (2.2) | 9 (60.0) | 11 (11.0) |
| Parameter | Hyperdivergent | Hypodivergent | Normodivergent | Total | p-Value |
|---|---|---|---|---|---|
| Total N (%) | 14 (14.0) | 46 (46.0) | 40 (40.0) | 100 | |
| Interincisal angle (°) | 127.9 (121.6 to 133.5) | 128.0 (120.1 to 136.8) | 128.7 (123.0 to 137.9) | 128.2 (121.6 to 136.8) | 0.655 |
| L1 to LOP (°) | 63.8 (60.8 to 69.0) | 64.7 (58.8 to 67.9) | 66.1 (62.8 to 72.0) | 65.2 (60.5 to 69.4) | 0.230 |
| U1 to UOP (°) | 59.9 (57.0 to 61.8) | 58.5 (53.2 to 61.8) | 58.8 (55.6 to 64.6) | 58.8 (54.9 to 63.8) | 0.478 |
| Nasolabial angle (°) | 103.8 (100.3 to 109.4) | 100.1 (94.5 to 108.8) | 101.6 (97.0 to 109.7) | 101.5 (96.5 to 109.7) | 0.423 |
| Lower lip to E-plane (mm) | −1.1 (−1.3 to 0.3) | −2.5 (−3.5 to −1.4) | −2.1 (−4.5 to −0.2) | −2.3 (−3.8 to −0.6) | 0.147 |
| Upper lip to E-plane (mm) | −2.4 (−3.3 to −0.8) | −3.0 (−4.6 to −1.6) | −2.7 (−5.4 to −1.3) | −2.8 (−4.8 to −1.3) | 0.713 |
| WITS (mm) | 1.7 (0.1 to 5.1) | 2.4 (0.5 to 4.3) | 2.1 (−1.1 to 4.2) | 2.1 (0.0 to 4.3) | 0.708 |
| FMA (°) | 32.1 (30.9 to 34.7) | 15.9 (14.5 to 19.0) | 24.5 (23.4 to 26.1) | 22.2 (16.5 to 25.7) | <0.001 |
| ANB (°) | 6.0 (3.6 to 7.9) | 4.2 (2.5 to 5.8) | 5.0 (2.3 to 7.3) | 4.5 (2.6 to 6.9) | 0.123 |
| Meaning results of ANB | 0.042 | ||||
| Skeletal Class I | 4 (28.6) | 26 (56.5) | 11 (27.5) | 41 (41.0) | |
| Skeletal Class II | 9 (64.3) | 17 (37.0) | 22 (55.0) | 48 (48.0) | |
| Skeletal Class III | 1 (7.1) | 3 (6.5) | 7 (17.5) | 11 (11.0) | |
| Meaning results of WITS | 0.558 | ||||
| Skeletal Class I | 8 (57.1) | 18 (39.1) | 14 (35.0) | 40 (40.0) | |
| Skeletal Class II | 5 (35.7) | 22 (47.8) | 18 (45.0) | 45 (45.0) | |
| Skeletal Class III | 1 (7.1) | 6 (13.0) | 8 (20.0) | 15 (15.0) |
| Parameter | ANB Skeletal Class I (41, 41.0%) | ANB Skeletal Class II (48, 48.0%) | ANB Skeletal Class III (11, 11.0%) | Total | p-Value |
|---|---|---|---|---|---|
| Interincisal angle (°) | 129.6 (123.2 to 137.8) | 125.7 (120.7 to 132.8) | 130.0 (126.0 to 146.1) | 128.2 (121.6 to 136.8) | 0.047 |
| L1 to LOP (°) | 66.3 (63.8 to 70.3) | 61.4 (57.3 to 65.3) | 73.5 (69.9 to 78.0) | 65.2 (60.5 to 69.4) | <0.001 |
| U1 to UOP (°) | 59.0 (55.3 to 61.6) | 58.9 (55.5 to 64.5) | 57.2 (52.2 to 64.5) | 58.8 (54.9 to 63.8) | 0.873 |
| Nasolabial angle (°) | 101.5 (96.5 to 107.0) | 102.6 (96.9 to 114.0) | 99.0 (92.0 to 100.6) | 101.5 (96.5 to 109.7) | 0.202 |
| Lower lip to E-plane (mm) | −2.9 (−4.1 to −1.6) | −1.3 (−2.7 to 0.6) | −3.3 (−7.1 to −0.4) | −2.3 (−3.8 to −0.6) | 0.009 |
| Upper lip to E-plane (mm) | −4.0 (−5.4 to −2.1) | −1.8 (−3.1 to −0.5) | −5.4 (−7.6 to −2.6) | −2.8 (−4.8 to −1.3) | <0.001 |
| WITS (mm) | 1.0 (−0.1 to 2.2) | 4.0 (2.8 to 6.7) | −2.7 (−4.2 to −2.3) | 2.1 (0.0 to 4.3) | <0.001 |
| FMA (°) | 19.0 (15.2 to 24.5) | 24.2 (18.9 to 27.3) | 22.9 (22.0 to 25.9) | 22.2 (16.5 to 25.7) | 0.020 |
| ANB (°) | 3.3 (2.2 to 4.2) | 7.0 (5.7 to 8.1) | −0.3 (−0.9 to 0.1) | 4.5 (2.6 to 6.9) | <0.001 |
| Meaning results of WITS | <0.001 | ||||
| Skeletal Class I | 28 (68.3) | 11 (22.9) | 1 (9.1) | 40 (40.0) | |
| Skeletal Class II | 8 (19.5) | 36 (75.0) | 1 (9.1) | 45 (45.0) | |
| Skeletal Class III | 5 (12.2) | 1 (2.1) | 9 (81.8) | 15 (15.0) | |
| Meaning results of FMA | 0.042 | ||||
| Hyperdivergent | 4 (9.8) | 9 (18.8) | 1 (9.1) | 14 (14.0) | |
| Hypodivergent | 26 (63.4) | 17 (35.4) | 3 (27.3) | 46 (46.0) | |
| Normodivergent | 11 (26.8) | 22 (45.8) | 7 (63.6) | 40 (40.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stăncioiu, A.-A.; Motofelea, A.C.; Hușanu, A.A.; Vasica, L.; Popa, A.; Nagib, R.; Szuhanek, C. Innovative Aesthetic and Functional Orthodontic Planning with Hard and Soft Tissue Analyses. J. Clin. Med. 2025, 14, 4458. https://doi.org/10.3390/jcm14134458
Stăncioiu A-A, Motofelea AC, Hușanu AA, Vasica L, Popa A, Nagib R, Szuhanek C. Innovative Aesthetic and Functional Orthodontic Planning with Hard and Soft Tissue Analyses. Journal of Clinical Medicine. 2025; 14(13):4458. https://doi.org/10.3390/jcm14134458
Chicago/Turabian StyleStăncioiu, Andra-Alexandra, Alexandru Cătălin Motofelea, Anca Adriana Hușanu, Lorena Vasica, Adelina Popa, Riham Nagib, and Camelia Szuhanek. 2025. "Innovative Aesthetic and Functional Orthodontic Planning with Hard and Soft Tissue Analyses" Journal of Clinical Medicine 14, no. 13: 4458. https://doi.org/10.3390/jcm14134458
APA StyleStăncioiu, A.-A., Motofelea, A. C., Hușanu, A. A., Vasica, L., Popa, A., Nagib, R., & Szuhanek, C. (2025). Innovative Aesthetic and Functional Orthodontic Planning with Hard and Soft Tissue Analyses. Journal of Clinical Medicine, 14(13), 4458. https://doi.org/10.3390/jcm14134458






