Preoperative Low Lumbar Hounsfield Units and Global Alignment Predict Postoperative Mechanical Complications After Adult Spinal Deformity Surgery: A Multicenter Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
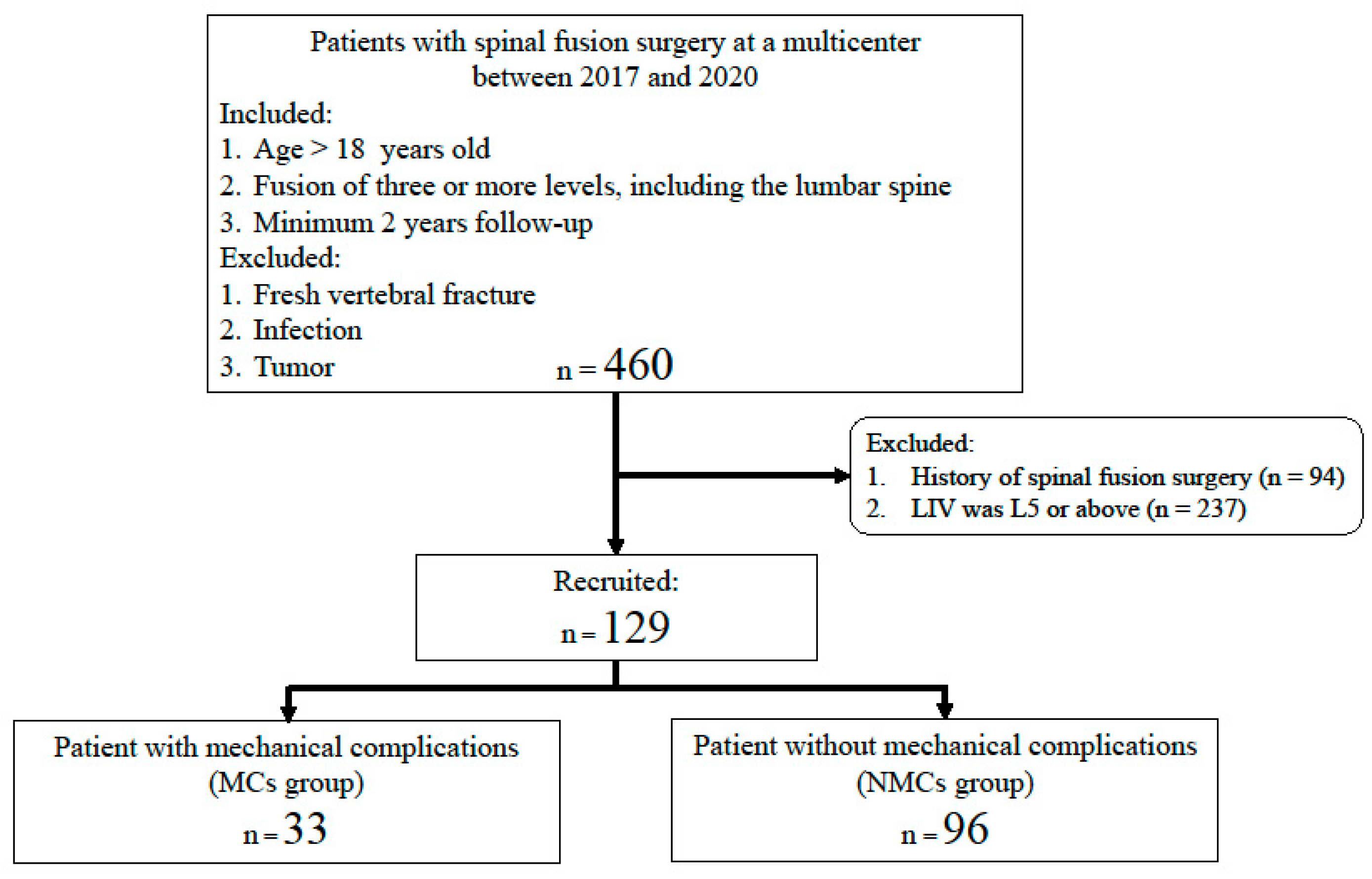
2.1. Patients
2.2. Radiographic Measurements
- Thoracic kyphosis (TK: T1–12);
- Lumbar lordosis (LL: L1–S1);
- Lower lumbar lordosis (LLL: L4–S1);
- Pelvic incidence;
- Pelvic tilt;
- Sacral slope;
- C7 sagittal vertical axis (SVA);
- Global tilt (GT).
2.3. MCs
2.4. HU Values Measurement
2.5. Statistical Analysis
3. Results
3.1. Baseline Patient Characteristics and Clinical Outcomes
3.2. Comparison Radiographic Measurements Between MC and NMC Groups
3.3. BMD Measurements Using HUs
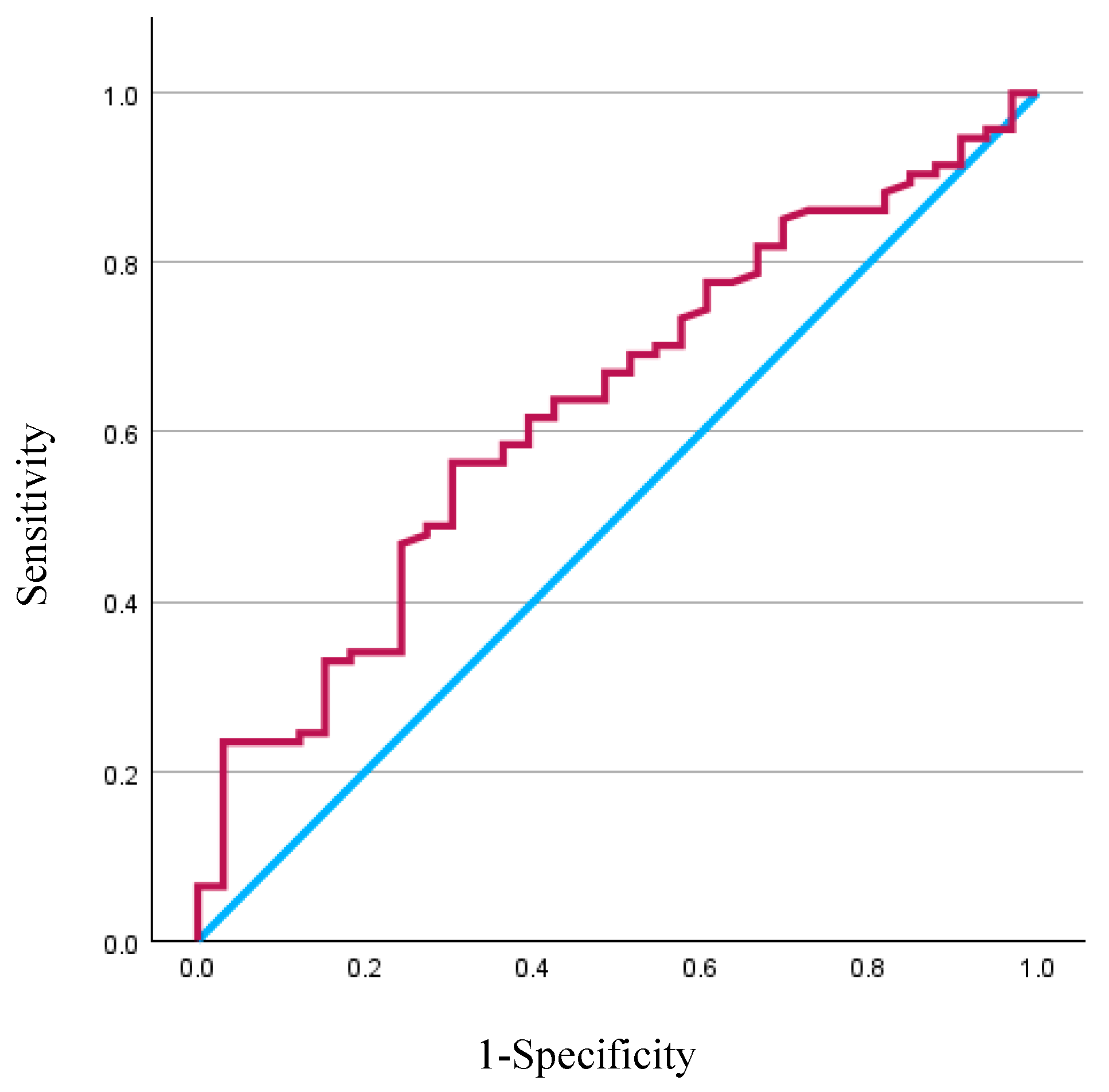
3.4. Multivariate Predictor of MCs
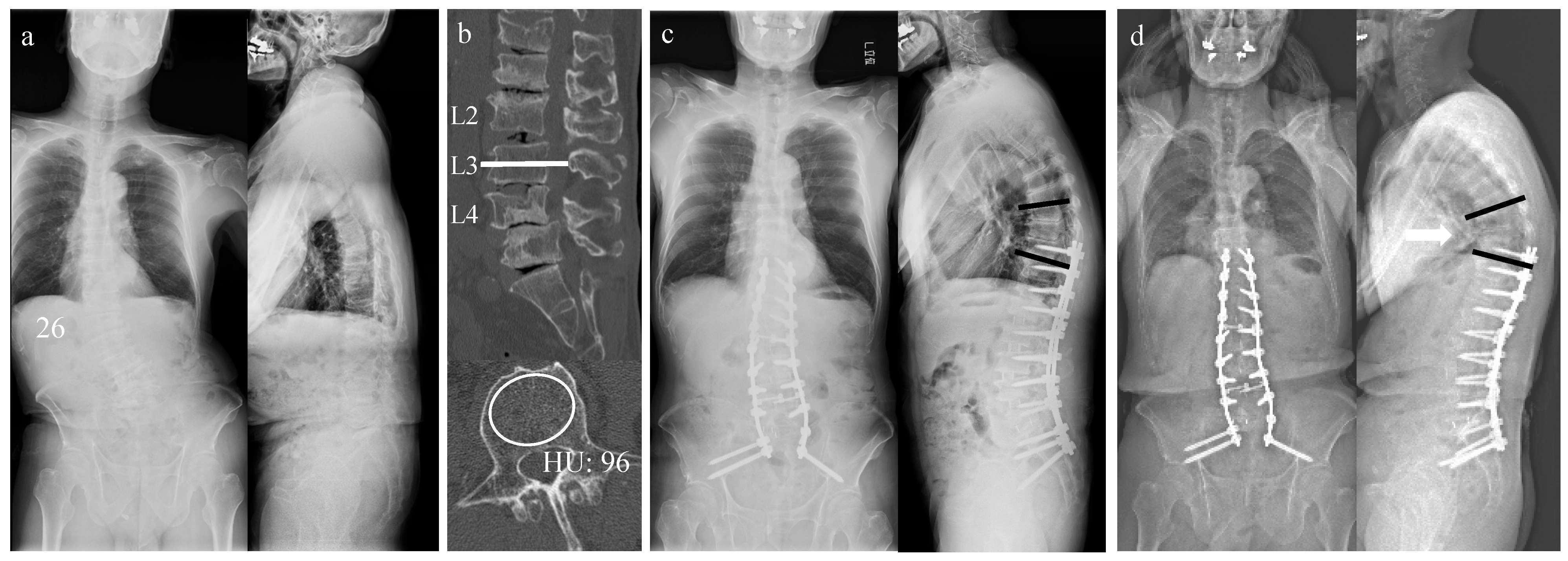
3.5. Case Presentation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ASD | Adult spinal deformity |
| AUC | Area under the curve |
| BMD | Bone mineral density |
| BMI | Body mass index |
| CI | Confidence interval |
| CT | Computed tomography |
| DEXA | Dual-energy X-ray absorptiometry |
| DJF | Distal junctional failure |
| GAP | Global alignment and proportion |
| GT | Global tilt |
| HU | Hounsfield unit |
| MC | Mechanical complications |
| PJF | Proximal junctional failure |
| PJK | Proximal junctional kyphosis |
| ROI | Region of interest |
| SVA | Sagittal vertical axis |
| UIV | Upper instrumented vertebra |
References
- Kebaish, K.M.; Neubauer, P.R.; Voros, G.D.; Khoshnevisan, M.A.; Skolasky, R.L. Scoliosis in adults aged forty years and older: Prevalence and relationship to age, race, and gender. Spine 2011, 36, 731–736. [Google Scholar] [CrossRef]
- Berven, S.; Deviren, V.; Demir-Deviren, S.; Hu, S.S.; Bradford, D.S. Studies in the modified Scoliosis Research Society Outcomes Instrument in adults: Validation, reliability, and discriminatory capacity. Spine 2003, 28, 2164–2169. [Google Scholar] [CrossRef]
- Glassman, S.D.; Bridwell, K.; Dimar, J.R.; Horton, W.; Berven, S.; Schwab, F. The impact of positive sagittal balance in adult spinal deformity. Spine 2005, 30, 2024–2029. [Google Scholar] [CrossRef]
- Yamato, Y.; Matsuyama, Y.; Hasegawa, K.; Aota, Y.; Akazawa, T.; Iida, T.; Ueyama, K.; Uno, K.; Kanemura, T.; Kawakami, N.; et al. A Japanese nationwide multicenter survey on perioperative complications of corrective fusion for elderly patients with adult spinal deformity. J. Orthop. Sci. 2017, 22, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Bridwell, K.H.; Lenke, L.G.; Cho, S.K.; Pahys, J.M.; Zebala, L.P.; Dorward, I.G.; Cho, W.; Baldus, C.; Hill, B.W.; Kang, M.M. Proximal junctional kyphosis in primary adult deformity surgery: Evaluation of 20 degrees as a critical angle. Neurosurgery 2013, 72, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Yagi, M.; King, A.B.; Boachie-Adjei, O. Incidence, risk factors, and natural course of proximal junctional kyphosis: Surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine 2012, 37, 1479–1489. [Google Scholar] [CrossRef] [PubMed]
- Williamson, T.K.; Passfall, L.; Ihejirika-Lomedico, R.; Espinosa, A.; Owusu-Sarpong, S.; Lanre-Amos, T.; Schoenfeld, A.J.; Passias, P.G. Assessing the influence of modifiable patient-related factors on complication rates after adult spinal deformity surgery. Bone Jt. J. 2022, 104, 1249–1255. [Google Scholar] [CrossRef]
- Masud, T.; Langley, S.; Wiltshire, P.; Doyle, D.V.; Spector, T.D. Effect of spinal osteophytosis on bone mineral density measurements in vertebral osteoporosis. Br. Med. J. 1993, 307, 172–173. [Google Scholar] [CrossRef]
- Svendsen, O.L.; Hassager, C.; Skodt, V.; Christiansen, C. Impact of soft tissue on in vivo accuracy of bone mineral measurements in the spine, hip, and forearm: A human cadaver study. J. Bone Miner. Res. 1995, 10, 868–873. [Google Scholar] [CrossRef]
- Anderson, P.A.; Polly, D.W.; Binkley, N.C.; Pickhardt, P.J. Clinical Use of Opportunistic Computed Tomography Screening for Osteoporosis. J. Bone Jt. Surg. Am. 2018, 100, 2073–2081. [Google Scholar] [CrossRef]
- Hiyama, A.; Sakai, D.; Katoh, H.; Sato, M.; Watanabe, M. Relationship Between Hounsfield Units of Upper Instrumented Vertebrae, Proximal Junctional Failure, and Global Alignment and Proportion Score in Female Patients with Adult Spinal Deformity. World Neurosurg. 2022, 164, e706–e717. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, N.; Hadi, M.S.; Lillard, J.C.; Passias, P.G.; Linzey, J.R.; Saadeh, Y.S.; LaBagnara, M.; Park, P. Alternatives to DEXA for the assessment of bone density: A systematic review of the literature and future recommendations. J. Neurosurg. Spine 2023, 38, 436–445. [Google Scholar] [CrossRef]
- Choi, M.K.; Kim, S.M.; Lim, J.K. Diagnostic efficacy of Hounsfield units in spine CT for the assessment of real bone mineral density of degenerative spine: Correlation study between T-scores determined by DEXA scan and Hounsfield units from CT. Acta Neurochir. 2016, 158, 1421–1427. [Google Scholar] [CrossRef]
- Zou, D.; Sun, Z.; Zhou, S.; Zhong, W.; Li, W. Hounsfield units value is a better predictor of pedicle screw loosening than the T-score of DXA in patients with lumbar degenerative diseases. Eur. Spine J. 2020, 29, 1105–1111. [Google Scholar] [CrossRef]
- Glattes, R.C.; Bridwell, K.H.; Lenke, L.G.; Kim, Y.J.; Rinella, A.; Edwards, C., 2nd. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: Incidence, outcomes, and risk factor analysis. Spine 2005, 30, 1643–1649. [Google Scholar] [CrossRef] [PubMed]
- Banno, T.; Togawa, D.; Arima, H.; Hasegawa, T.; Yamato, Y.; Kobayashi, S.; Yasuda, T.; Oe, S.; Hoshino, H.; Matsuyama, Y. The cohort study for the determination of reference values for spinopelvic parameters (T1 pelvic angle and global tilt) in elderly volunteers. Eur. Spine J. 2016, 25, 3687–3693. [Google Scholar] [CrossRef] [PubMed]
- Kawabata, A.; Yoshii, T.; Sakai, K.; Hirai, T.; Yuasa, M.; Inose, H.; Utagawa, K.; Hashimoto, J.; Matsukura, Y.; Tomori, M.; et al. Identification of Predictive Factors for Mechanical Complications After Adult Spinal Deformity Surgery: A Multi-Institutional Retrospective Study. Spine 2020, 45, 1185–1192. [Google Scholar] [CrossRef]
- Noh, S.H.; Ha, Y.; Obeid, I.; Park, J.Y.; Kuh, S.U.; Chin, D.K.; Kim, K.S.; Cho, Y.E.; Lee, H.S.; Kim, K.H. Modified global alignment and proportion scoring with body mass index and bone mineral density (GAPB) for improving predictions of mechanical complications after adult spinal deformity surgery. Spine J. 2020, 20, 776–784. [Google Scholar] [CrossRef]
- Teles, A.R.; Aldebeyan, S.; Aoude, A.; Swamy, G.; Nicholls, F.H.; Thomas, K.C.; Jacobs, W.B. Mechanical Complications in Adult Spinal Deformity Surgery: Can Spinal Alignment Explain Everything? Spine 2022, 47, E1–E9. [Google Scholar] [CrossRef]
- Glassman, S.D.; Berven, S.; Bridwell, K.; Horton, W.; Dimar, J.R. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 2005, 30, 682–688. [Google Scholar] [CrossRef]
- Zanirato, A.; Damilano, M.; Formica, M.; Piazzolla, A.; Lovi, A.; Villafane, J.H.; Berjano, P. Complications in adult spine deformity surgery: A systematic review of the recent literature with reporting of aggregated incidences. Eur. Spine J. 2018, 27, 2272–2284. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Ungar, B.; Blondel, B.; Buchowski, J.; Coe, J.; Deinlein, D.; DeWald, C.; Mehdian, H.; Shaffrey, C.; Tribus, C.; et al. Scoliosis Research Society-Schwab adult spinal deformity classification: A validation study. Spine 2012, 37, 1077–1082. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F.; Patel, A.; Ungar, B.; Farcy, J.P.; Lafage, V. Adult spinal deformity-postoperative standing imbalance: How much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine 2010, 35, 2224–2231. [Google Scholar] [CrossRef]
- Yilgor, C.; Sogunmez, N.; Boissiere, L.; Yavuz, Y.; Obeid, I.; Kleinstuck, F.; Perez-Grueso, F.J.S.; Acaroglu, E.; Haddad, S.; Mannion, A.F.; et al. Global Alignment and Proportion (GAP) Score: Development and Validation of a New Method of Analyzing Spinopelvic Alignment to Predict Mechanical Complications After Adult Spinal Deformity Surgery. J. Bone Jt. Surg. Am. 2017, 99, 1661–1672. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Kim, J.J.; Jang, I.G. Patient-specific phantomless estimation of bone mineral density and its effects on finite element analysis results: A feasibility study. Comput. Math. Methods Med. 2019, 2019, 4102410. [Google Scholar] [CrossRef]
- Schreiber, J.J.; Anderson, P.A.; Hsu, W.K. Use of computed tomography for assessing bone mineral density. Neurosurg. Focus 2014, 37, E4. [Google Scholar] [CrossRef]
- Ishikawa, Y.; Katsumi, K.; Mizouchi, T.; Sato, M.; Yamazaki, A. Importance of computed tomography Hounsfield units in predicting S1 screw loosening after lumbosacral fusion. J. Clin. Neurosci. 2023, 113, 1–6. [Google Scholar] [CrossRef]
- Uei, H.; Tokuhashi, Y.; Maseda, M.; Nakahashi, M.; Sawada, H.; Matsumoto, K.; Miyakata, H. Exploratory analysis of predictors of revision surgery for proximal junctional kyphosis or additional postoperative vertebral fracture following adult spinal deformity surgery in elderly patients: A retrospective cohort study. J. Orthop. Surg. Res. 2018, 13, 252. [Google Scholar] [CrossRef]
| Total | MC Group | NMC Group | p-Value | ||
|---|---|---|---|---|---|
| Age (years) | 68.0 ± 10.9 | 69.6 ± 7.8 | 67.4 ± 11.7 | NS | |
| Sex (female, %) | 82.2 | 84.8 | 81.3 | NS | |
| Height (cm) | 152.4 ± 8.2 | 150.5 ± 7.0 | 153.1 ± 8.4 | NS | |
| Weight (kg) | 55.8 ± 11.7 | 54.1 ± 11.2 | 56.4 ± 11.9 | NS | |
| BMI (kg/cm2) | 23.9 ± 4.0 | 23.8 ± 4.2 | 23.9 ± 4.0 | NS | |
| Osteoporosis treatment PTH Bisphosphonate RANKL inhibitor | 12 10 1 | 6 6 0 | 6 4 1 | 0.02 | |
| Operative parameters | |||||
| Time (minutes) | 268.9 ± 111.2 | 257.2 ± 106.0 | 273.0 ± 113.2 | NS | |
| Blood loss (g) | 1057.1 ± 1388.4 | 896.4 ± 1127.1 | 1112.4 ± 1468.8 | NS | |
| Fusion level (n) | 6.5 ± 2.9 | 6.5 ± 3.3 | 6.5 ± 2.8 | NS | |
| UIV T2-5 T10-L3 | 10 119 | 3 30 | 7 89 | NS | |
| LIV Sacrum Ilium | 18 111 | 6 27 | 12 84 | NS | |
| Duration of hospital stay (day) | 52.8 ± 37.3 | 46.4 ± 32.2 | 55.1 ± 38.9 | NS | |
| JOA score | |||||
| Pre | 15.4 ± 5.0 | 14.6 ± 4.8 | 15.7 ± 5.1 | NS | |
| 2 years postoperatively | 22.6 ± 3.9 | 20.7 ± 3.9 | 23.3 ± 3.7 | <0.01 | |
| MCs | PJK/PJF | 22 | |||
| DJF | 2 | ||||
| Rod fracture | 5 | ||||
| Re-operation | 9 | ||||
| Degrees | Total | MC Group | NMC Group | p-Value |
|---|---|---|---|---|
| TK | ||||
| Pre | 23.6 ± 15.9 | 25.1 ± 16.9 | 23.0 ± 15.6 | NS |
| Post-op | 30.2 ± 12.0 | 29.4 ± 13.6 | 30.5 ± 11.4 | NS |
| 2 years post-op | 35.6 ± 13.0 | 37.5 ± 17.8 | 34.9 ± 11.1 | NS |
| LL | ||||
| Pre | 23.6 ± 31.3 | 20.4 ± 18.7 | 24.7 ± 34.6 | NS |
| Post-op | 42.4 ± 11.8 | 42.0 ± 12.4 | 42.5 ± 11.6 | NS |
| 2 years post-op | 38.8 ± 13.5 | 35.7 ± 14.2 | 40.0 ± 13.2 | NS |
| LLL | ||||
| Pre | 18.1 ± 13.8 | 15.0 ± 12.1 | 19.1 ± 14.3 | NS |
| Post-op | 26.4 ± 7.6 | 24.8 ± 9.7 | 27.0 ± 6.8 | NS |
| 2 years post-op | 27.2 ± 18.9 | 24.7 ± 7.7 | 28.1 ± 21.5 | NS |
| PI | ||||
| Pre | 52.4 ± 12.3 | 53.2 ± 10.7 | 52.1 ± 12.9 | NS |
| Post-op | 49.9 ± 12.1 | 49.1 ± 14.1 | 50.2 ± 11.4 | NS |
| 2 years post-op | 52.6 ± 13.4 | 53.1 ± 13.6 | 52.4 ± 13.4 | NS |
| PT | ||||
| Pre | 29.9 ± 12.1 | 33.0 ± 11.8 | 28.9 ± 12.1 | NS |
| Post-op | 20.5 ± 8.5 | 20.4 ± 8.3 | 20.5 ± 8.6 | NS |
| 2 years post-op | 25.0 ± 9.5 | 27.3 ± 9.5 | 24.2 ± 9.4 | NS |
| SS | ||||
| Pre | 22.5 ± 13.3 | 20.2 ± 14.1 | 23.2 ± 13.0 | NS |
| Post-op | 29.4 ± 10.2 | 28.7 ± 11.5 | 29.7 ± 9.8 | NS |
| 2 years post-op | 27.6 ± 13.5 | 25.7 ± 14.9 | 28.2 ± 12.9 | NS |
| PI-LL | ||||
| Pre | 30.9 ± 19.9 | 32.8 ± 17.5 | 30.3 ± 20.7 | NS |
| Post-op | 7.5 ± 77.7 | 7.1 ± 13.4 | 7.6 ± 11.2 | NS |
| 2 years post-op | 14.0 ± 14.7 | 17.3 ± 17.3 | 12.8 ± 13.6 | NS |
| SVA | ||||
| Pre | 85.5 ± 55.7 | 101.3 ± 49.5 | 79.8 ± 56.9 | 0.03 |
| Post-op | 32.9 ± 33.7 | 43.7 ± 37.2 | 29.1 ± 31.8 | 0.04 |
| 2 years post-op | 51.7 ± 49.0 | 71.2 ± 53.9 | 45.2 ± 45.8 | 0.01 |
| GT | ||||
| Pre | 34.4 ± 20.6 | 42.5 ± 23.1 | 31.5 ± 18.9 | 0.03 |
| Post-op | 20.3 ± 15.1 | 24.6 ± 18.2 | 18.9 ± 13.6 | NS |
| 2 years post-op | 25.1 ± 17.8 | 33.3 ± 18.4 | 22.2 ± 16.7 | <0.01 |
| Predictors | Odds Ratio | Standard Error | p | 95% CI |
|---|---|---|---|---|
| Age | 0.997 | 0.027 | 0.926 | 0.946–1.052 |
| Sex | 0.933 | 0.593 | 0.906 | 0.291–2.985 |
| SVA | 1.007 | 0.004 | 0.097 | 0.999–1.014 |
| HU value | 0.989 | 0.005 | 0.046 | 0.979–1.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamauchi, I.; Nakashima, H.; Ito, S.; Segi, N.; Ouchida, J.; Morita, Y.; Ode, Y.; Nagatani, Y.; Okada, Y.; Takeichi, Y.; et al. Preoperative Low Lumbar Hounsfield Units and Global Alignment Predict Postoperative Mechanical Complications After Adult Spinal Deformity Surgery: A Multicenter Retrospective Study. J. Clin. Med. 2025, 14, 4267. https://doi.org/10.3390/jcm14124267
Yamauchi I, Nakashima H, Ito S, Segi N, Ouchida J, Morita Y, Ode Y, Nagatani Y, Okada Y, Takeichi Y, et al. Preoperative Low Lumbar Hounsfield Units and Global Alignment Predict Postoperative Mechanical Complications After Adult Spinal Deformity Surgery: A Multicenter Retrospective Study. Journal of Clinical Medicine. 2025; 14(12):4267. https://doi.org/10.3390/jcm14124267
Chicago/Turabian StyleYamauchi, Ippei, Hiroaki Nakashima, Sadayuki Ito, Naoki Segi, Jun Ouchida, Yoshinori Morita, Yukihito Ode, Yasuhiro Nagatani, Yuya Okada, Yosuke Takeichi, and et al. 2025. "Preoperative Low Lumbar Hounsfield Units and Global Alignment Predict Postoperative Mechanical Complications After Adult Spinal Deformity Surgery: A Multicenter Retrospective Study" Journal of Clinical Medicine 14, no. 12: 4267. https://doi.org/10.3390/jcm14124267
APA StyleYamauchi, I., Nakashima, H., Ito, S., Segi, N., Ouchida, J., Morita, Y., Ode, Y., Nagatani, Y., Okada, Y., Takeichi, Y., Kagami, Y., Tachi, H., Ohshima, K., Oyama, H., Ogura, K., Miyairi, Y., Oishi, R., Morishita, K., Shinjo, R., ... Imagama, S., on behalf of the Adult Spinal Deformity Study Group of the Nagoya Spine Group. (2025). Preoperative Low Lumbar Hounsfield Units and Global Alignment Predict Postoperative Mechanical Complications After Adult Spinal Deformity Surgery: A Multicenter Retrospective Study. Journal of Clinical Medicine, 14(12), 4267. https://doi.org/10.3390/jcm14124267






